Environmental and Genetic Determinants of Ankylosing Spondylitis
Abstract
:1. Introduction
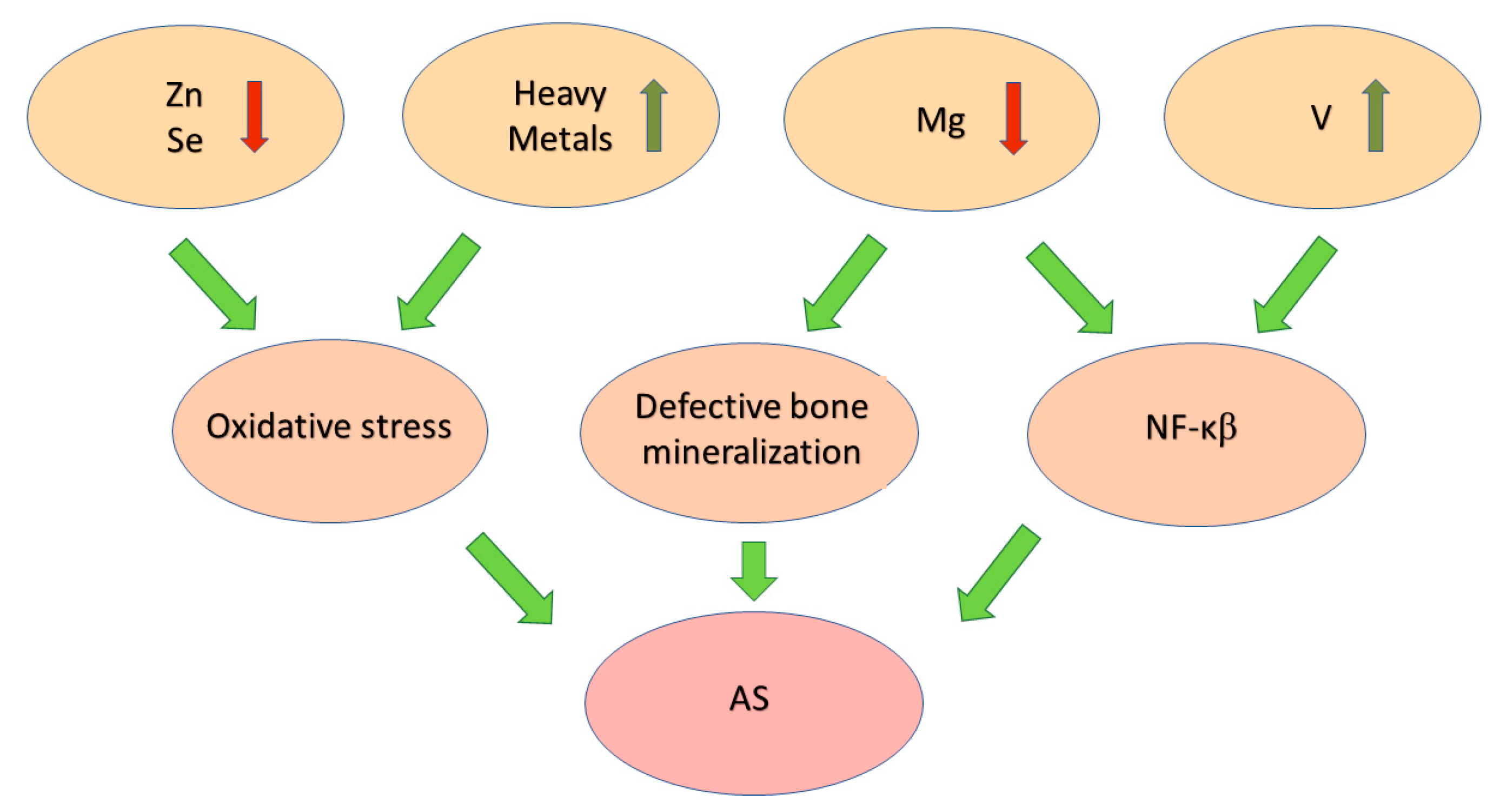
2. The Participation of Oxidative Stress in Pathogenesis of AS
3. The Participation of Elements as Environmental Factors in AS Development
4. Lifestyle as an Environmental Factor in AS Development
5. Infection in AS
6. Microbiota in AS
7. Genetic Polymorphism in HLA System
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sharip, A.; Kunz, J. Understanding the Pathogenesis of Spondyloarthritis. Biomolecules 2020, 10, 1461. [Google Scholar] [CrossRef]
- Akhondi, H.; Varacallo, M. Rheumatoid Arthritis And Ankylosing Spondylitis; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Hwang, M.C.; Ridley, L.; Reveille, J.D. Ankylosing spondylitis risk factors: A systematic literature review. Clin. Rheumatol 2021, 40, 3079–3093. [Google Scholar] [CrossRef]
- Liao, H.-T.; Tsai, C.-Y.; Lai, C.-C.; Hsieh, S.-C.; Sun, Y.-S.; Li, K.-J.; Shen, C.-Y.; Wu, C.-H.; Lu, C.-H.; Kuo, Y.-M.; et al. The Potential Role of Genetics, Environmental Factors, and Gut Dysbiosis in the Aberrant Non-Coding RNA Expression to Mediate Inflammation and Osteoclastogenic/Osteogenic Differentiation in Ankylosing Spondylitis. Front. Cell Dev. Biol. 2022, 9, 748063. [Google Scholar] [CrossRef]
- Wordsworth, B.P.; Cohen, C.J.; Davidson, C.; Vecellio, M. Perspectives on the Genetic Associations of Ankylosing Spondylitis. Front. Immunol. 2021, 12, 603726. [Google Scholar] [CrossRef]
- Voruganti, A.; Bowness, P. New developments in our understanding of ankylosing spondylitis pathogenesis. Immunology 2020, 161, 94–102. [Google Scholar] [CrossRef]
- Poddubnyy, D.; Haibel, H.; Listing, J.; Märker-Hermann, E.; Zeidler, H.; Braun, J.; Sieper, J.; Rudwaleit, M. Baseline radiographic damage, elevated acute-phase reactant levels, and cigarette smoking status predict spinal radiographic progression in early axial spondylarthritis. Arthritis Rheum. 2012, 64, 1388–1398. [Google Scholar] [CrossRef]
- de Bruin, F.; de Koning, A.; van den Berg, R.; Baraliakos, X.; Braun, J.; Ramiro, S.; van Gaalen, F.A.; Reijnierse, M.; van der Heijde, D. Development of the CT Syndesmophyte Score (CTSS) in patients with ankylosing spondylitis: Data from the SIAS cohort. Ann. Rheum. Dis. 2018, 77, 371–377. [Google Scholar] [CrossRef]
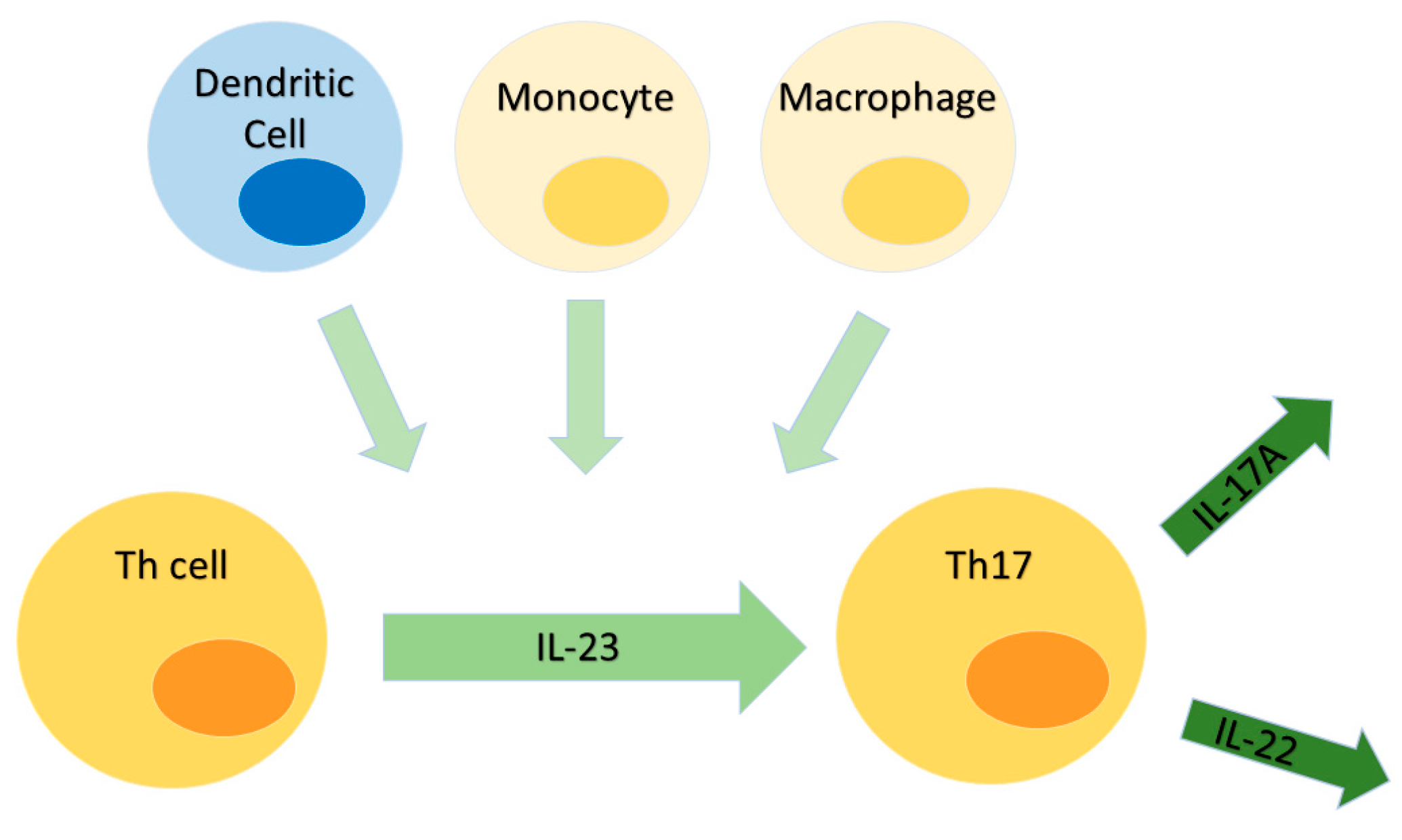
- Tsukazaki, H.; Kaito, T. The Role of the IL-23/IL-17 Pathway in the Pathogenesis of Spondyloarthritis. Int. J. Mol. Sci. 2020, 21, 6401. [Google Scholar] [CrossRef]
- Baeten, D.; Adamopoulos, I.E. IL-23 Inhibition in Ankylosing Spondylitis: Where Did It Go Wrong? Front. Immunol. 2021, 11, 623874. [Google Scholar] [CrossRef]
- Gravallese, E.M.; Schett, G. Effects of the IL-23-IL-17 pathway on bone in spondyloarthritis. Nat. Rev. Rheumatol. 2018, 14, 631–640. [Google Scholar] [CrossRef]
- Tang, M.; Lu, L.; Yu, X. Interleukin-17A Interweaves the Skeletal and Immune Systems. Front. Immunol. 2021, 11, 625034. [Google Scholar] [CrossRef]
- Vebr, M.; Pomahačová, R.; Sýkora, J.; Schwarz, J. A Narrative Review of Cytokine Networks: Pathophysiological and Therapeutic Implications for Inflammatory Bowel Disease Pathogenesis. Biomedicines 2023, 11, 3229. [Google Scholar] [CrossRef]
- Klasen, C.; Meyer, A.; Wittekind, P.S.; Waqué, I.; Nabhani, S.; Kofler, D.M. Prostaglandin receptor EP4 expression by Th17 cells is associated with high disease activity in ankylosing spondylitis. Arthritis Res. Ther. 2019, 21, 159. [Google Scholar] [CrossRef]
- Verstrepen, L.; Bekaert, T.; Chau, T.L.; Tavernier, J.; Chariot, A.; Beyaert, R. TLR-4, IL-1R and TNF-R signaling to NF-κB: Variations on a common theme. Cell. Mol. Life Sci. 2008, 65, 2964–2978. [Google Scholar] [CrossRef]
- Li, Z.; Guo, J.; Bi, L. Role of the NLRP3 inflammasome in autoimmune diseases. Biomed. Pharmacother. 2020, 130, 110542. [Google Scholar] [CrossRef]
- Coll, R.C.; Schroder, K.; Pelegrín, P. NLRP3 and pyroptosis blockers for treating inflammatory diseases. Trends Pharmacol. Sci. 2022, 43, 653–668. [Google Scholar] [CrossRef]
- Fu, R.; Guo, X.; Pan, Z.; Wang, Y.; Xu, J.; Zhang, L.; Li, J. Molecular mechanisms of AMPK/YAP/NLRP3 signaling pathway affecting the occurrence and development of ankylosing spondylitis. J. Orthop. Surg. Res. 2023, 18, 831. [Google Scholar] [CrossRef]
- Kwon, S.R.; Lim, M.J.; Suh, C.H.; Park, S.G.; Hong, Y.S.; Yoon, B.Y.; Kim, H.A.; Choi, H.J.; Park, W. Dickkopf-1 level is lower in patients with ankylosing spondylitis than in healthy people and is not influenced by anti-tumor necrosis factor therapy. Rheumatol. Int. 2012, 32, 2523–2527. [Google Scholar] [CrossRef]
- Qin, X.; Zhu, B.; Jiang, T.; Tan, J.; Wu, Z.; Yuan, Z.; Zheng, L.; Zhao, J. miR-17-5p Regulates Heterotopic Ossification by Targeting ANKH in Ankylosing Spondylitis. Mol. Ther. Nucleic Acids 2019, 18, 696–707. [Google Scholar] [CrossRef]
- Solmaz, D.; Uslu, S.; Kozacı, D.; Karaca, N.; Bulbul, H.; Tarhan, E.F.; Ozmen, M.; Can, G.; Akar, S. Evaluation of periostin and factors associated with new bone formation in ankylosing spondylitis: Periostin may be associated with the Wnt pathway. Int. J. Rheum. Dis. 2018, 21, 502–509. [Google Scholar] [CrossRef]
- Ramiro, S.; van der Heijde, D.; van Tubergen, A.; Stolwijk, C.; Dougados, M.; van den Bosch, F.; Landewé, R. Higher disease activity leads to more structural damage in the spine in ankylosing spondylitis: 12-year longitudinal data from the OASIS cohort. Ann. Rheum. Dis. 2014, 73, 1455–1461. [Google Scholar] [CrossRef]
- Łosińska, K.; Korkosz, M.; Kwaśny-Krochin, B. Endothelial Dysfunction in Patients with Ankylosing Spondylitis. Rheumatology 2019, 57, 100–105. [Google Scholar] [CrossRef]
- Le, T.H.V.; Kwon, S.-M. Vascular Endothelial Growth Factor Biology and Its Potential as a Therapeutic Target in Rheumatic Diseases. Int. J. Mol. Sci. 2021, 22, 5387. [Google Scholar] [CrossRef]
- Yamamoto, T. Angiogenic and Inflammatory Properties of Psoriatic Arthritis. Int. Sch. Res. Not. 2013, 2013, 630620. [Google Scholar] [CrossRef]
- Fearon, U.; Griosios, K.; Fraser, A.; Reece, R.; Emery, P.; Jones, P.F.; Veale, D.J. Angiopoietins, growth factors, and vascular morphology in early arthritis. J. Rheumatol. 2003, 30, 260–268. [Google Scholar]
- Liu, K.G.; He, Q.H.; Tan, J.W.; Liao, G.J. Expression of TNF-α, VEGF, and MMP-3 mRNAs in Synovial Tissues and Their Roles in Fibroblast-Mediated Osteogenesis in Ankylosing Spondylitis. Genet. Mol. Res. 2015, 14, 6852–6858. [Google Scholar] [CrossRef]
- Kawashima, M.; Fujikawa, Y.; Itonaga, I.; Takita, C.; Tsumura, H. The Effect of Selective Cyclooxygenase-2 Inhibitor on Human Osteoclast Precursors to Influence Osteoclastogenesis In Vitro. Mod. Rheumatol. 2009, 19, 192–198. [Google Scholar] [CrossRef]
- Drouart, M.; Saas, P.; Billot, M.; Cedoz, J.-P.; Tiberghien, P.; Wendling, D.; Toussirot, É. High Serum Vascular Endothelial Growth Factor Correlates with Disease Activity of Spondylarthropathies. Clin. Exp. Immunol. 2003, 132, 158–162. [Google Scholar] [CrossRef]
- Liu, Z.; Cai, M.; Ke, H.; Deng, H.; Ye, W.; Wang, T.; Chen, Q.; Cen, S. Fibroblast Insights into the Pathogenesis of An-kylosing Spondylitis. J. Inflamm. Res. 2023, 16, 6301–6317. [Google Scholar] [CrossRef]
- Sies, H. Oxidative Stress: Concept and Some Practical Aspects. Antioxidants 2020, 9, 852. [Google Scholar] [CrossRef]
- Betteridge, D.J. What Is Oxidative Stress? Metab. Clin. Exp. 2000, 49, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Kiranatlioglu-Firat, F.; Demir, H.; Cuce, I.; Altın-Celik, P.; Eciroglu, H.; Bayram, F.; Donmez-Altuntas, H. Increased Oxidative and Chromosomal DNA Damage in Patients with Ankylosing Spondylitis: Its Role in Pathogenesis. Clin. Exp. Med. 2023, 23, 1721–1728. [Google Scholar] [CrossRef] [PubMed]
- Kozaci, L.D.; Sari, I.; Alacacioglu, A.; Akar, S.; Akkoc, N. Evaluation of inflammation and oxidative stress in ankylosing spondylitis: A role for macrophage migration inhibitory factor. Mod. Rheumatol. 2010, 20, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Solmaz, D.; Kozacı, D.; Sarı, İ.; Taylan, A.; Önen, F.; Akkoç, N.; Akar, S. Oxidative stress and related factors in patients with ankylosing spondylitis. Eur. J. Rheumatol. 2016, 3, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Alfadda, A.A.; Sallam, R.M. Reactive oxygen species in health and disease. J. Biotechnol. Biomed. 2012, 2012, 936486. [Google Scholar] [CrossRef] [PubMed]
- Belenguer-Varea, Á.; Tarazona-Santabalbina, F.J.; Avellana-Zaragoza, J.A.; Martínez-Reig, M.; Mas-Bargues, C.; Inglés, M. Oxidative stress and exceptional human longevity: Systematic review. Free Radic. Biol. Med. 2020, 149, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Ezzat, S.; Louka, M.L.; Zakaria, Z.M.; Nagaty, M.M.; Metwaly, R.G. Autophagy in osteoporosis: Relation to oxidative stress. J. Cell. Biochem. 2018, 120, 2560–2568. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.Y.; Ahmad, N.; Haqqi, T.M. Oxidative stress and inflammation in osteoarthritis pathogenesis: Role of polyphenols. Biomed. Pharmacother. 2020, 129, 110452. [Google Scholar] [CrossRef] [PubMed]
- Veen, L.; Hantikainen, E.; Bellocco, R.; Ye, W.; Serafini, M.; Ponzano, M.; Grotta, A.; Trolle Lagerros, Y. Dietary antioxidants, non-enzymatic antioxidant capacity and the risk of osteoarthritis in the Swedish National March Cohort. Eur. J. Nutr. 2021, 60, 169–178. [Google Scholar] [CrossRef]
- Wang, Y.N.; Miao, H.; Yu, X.Y.; Guo, Y.; Su, W.; Liu, F.; Cao, G.; Zhao, Y.Y. Oxidative stress and inflammation are mediated via aryl hydrocarbon receptor signalling in idiopathic membranous nephropathy. Free Radic. Biol. Med. 2023, 207, 89–106. [Google Scholar] [CrossRef]
- Mussbacher, M.; Salzmann, M.; Brostjan, C.; Hoesel, B.; Schoergenhofer, C.; Datler, H.; Hohensinner, P.; Basílio, J.; Petzelbauer, P.; Assinger, A.; et al. Cell Type-Specific Roles of NF-κB Linking Inflammation and Thrombosis. Front. Immunol. 2019, 10, 85. [Google Scholar] [CrossRef]
- Vatner, S.F.; Zhang, J.; Oydanich, M.; Berkman, T.; Naftalovich, R.; Vatner, D.E. Healthful aging mediated by inhibition of oxidative stress. Ageing Res. Rev. 2020, 64, 101194. [Google Scholar] [CrossRef] [PubMed]
- Henrotin, Y.; Kurz, B.; Aigner, T. Oxygen and reactive oxygen species in cartilage degradation: Friends or foes? Osteoarthr. Cartil. 2005, 13, 643–654. [Google Scholar] [CrossRef]
- Karakoc, M.; Altindag, O.; Keles, H.; Soran, N.; Selek, S. Serum oxidative-antioxidative status in patients with ankylosing spondilitis. Rheumatol. Int. 2007, 27, 1131–1134. [Google Scholar] [CrossRef]
- Łuszczewski, A.; Matyska-Piekarska, E.; Trefler, J.; Wawer, I.; Łącki, J.; Śliwińska-Stańczyk, P. Review article Reactive oxygen species—Physiological and pathological function in the human body. Rheumatology 2007, 45, 284–289. [Google Scholar]
- Kabuyama, Y.; Kitamura, T.; Yamaki, J.; Homma, M.K.; Kikuchi, S.; Homma, Y. Involvement of thioredoxin reductase 1 in the regulation of redox balance and viability of rheumatoid synovial cells. Biochem. Biophys. Res. 2008, 367, 491–496. [Google Scholar] [CrossRef]
- Farsi, F.; Heshmati, J.; Keshtkar, A.; Irandoost, P.; Alamdari, N.M.; Akbari, A.; Janani, L.; Morshedzadeh, N.; Vafa, M. Can coenzyme Q10 supplementation effectively reduce human tumor necrosis factor-α and interleukin-6 levels in chronic inflammatory diseases? A systematic review and meta-analysis of randomized controlled trials. Pharmacol. Res. 2019, 148, 104290. [Google Scholar] [CrossRef] [PubMed]
- Bushnell, G.W.; Louie, G.V.; Brayer, G.D. High-resolution three-dimensional structure of horse heart cytochrome c. J. Mol. Biol. 1990, 214, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Patriarca, A.; Eliseo, T.; Sinibaldi, F.; Piro, M.C.; Melis, R.; Paci, M.; Cicero, D.O.; Polticelli, F.; Santucci, R.; Fiorucci, L. ATP acts as a regulatory effector in modulating structural transitions of cytochrome c: Implications for apoptotic activity. Biochemistry 2009, 48, 3279–3287. [Google Scholar] [CrossRef]
- Yadav, N.; Gogada, R.; O’Malley, J.; Gundampati, R.K.; Jayanthi, S.; Hashmi, S.; Lella, R.; Zhang, D.; Wang, J.; Kumar, R.; et al. Molecular insights on cytochrome c and nucleotide regulation of apoptosome function and its implication in cancer. Biochim. Biophys. Acta (BBA)-Mol. Cell Res. 2020, 1867, 118573. [Google Scholar] [CrossRef]
- Hannibal, L.; Tomasina, F.; Capdevila, D.A.; Demicheli, V.; Tórtora, V.; Alvarez-Paggi, D.; Jemmerson, R.; Murgida, D.H.; Radi, R. Alternative Conformations of Cytochrome c: Structure, Function, and Detection. Biochemistry 2016, 55, 407–428. [Google Scholar] [CrossRef]
- Santucci, R.; Sinibaldi, F.; Polticelli, F.; Fiorucci, L. Role of cardiolipin in mitochondrial diseases and apoptosis. Curr. Med. Chem. 2014, 21, 2702–2714. [Google Scholar] [CrossRef] [PubMed]
- Jemmerson, R.; Staskus, K.; Higgins, L.; Conklin, K.; Kelekar, A. Intracellular leucine-rich alpha-2-glycoprotein-1 competes with Apaf-1 for binding cytochrome c in protecting MCF-7 breast cancer cells from apoptosis. Apoptosis 2021, 26, 71–82. [Google Scholar] [CrossRef]
- Tang, M.; Li, G.; Chen, L.; Tu, J. Application of Cytochrome C-Related Genes in Prognosis and Treatment Prediction of Lung Adenocarcinoma. Dis. Markers 2022, 2022, 8809956. [Google Scholar] [CrossRef]
- Patriarca, A.; Polticelli, F.; Piro, M.C.; Sinibaldi, F.; Mei, G.; Bari, M.; Santucci, R.; Fiorucci, L. Conversion of cytochrome c into a peroxidase: Inhibitory mechanisms and implication for neurodegenerative diseases. Arch. Biochem. Biophys. 2012, 522, 62–69. [Google Scholar] [CrossRef]
- Hamanaka, R.B.; Chandel, N.S. Mitochondrial reactive oxygen species regulate hypoxic signaling. Curr. Opin. Cell Biol. 2009, 21, 894–899. [Google Scholar] [CrossRef]
- Kretz-Rommel, A.; Rubin, R.L. Early cellular events in systemic autoimmunity driven by chromatin-reactive T cells. Cell. Immunol. 2001, 208, 125–136. [Google Scholar] [CrossRef] [PubMed]
- Omori, E.; Morioka, S.; Matsumoto, K.; Ninomiya-Tsuji, J. TAK1 regulates reactive oxygen species and cell death in keratinocytes, which is essential for skin integrity. J. Biol. Chem. 2008, 283, 26161–26168. [Google Scholar] [CrossRef]
- Shi, Q.; Yang, X.; Mattes, W.B.; Mendrick, D.L.; Harrill, A.H.; Beger, R.D. Circulating mitochondrial biomarkers for drug-induced liver injury. Biomark. Med. 2015, 9, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Rashmi, R.; Rao, K.S.; Basavaraj, K.H. A comprehensive review of biomarkers in psoriasis. Clin. Exp. Dermatol. 2009, 34, 658–663. [Google Scholar] [CrossRef]
- Gladman, D.D.; Antoni, C.; Mease, P.; Clegg, D.O.; Nash, P. Psoriatic arthritis: Epidemiology, clinical features, course, and outcome. Ann. Rheum. Dis. 2005, 64, ii14–ii17. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, O.; Dougados, M. Psoriatic arthritis: One or more diseases? Best practice & research. Clin. Rheumatol. 2006, 20, 435–450. [Google Scholar]
- Sommerhoff, C.P.; Bode, W.; Pereira, P.J.; Stubbs, M.T.; Stürzebecher, J.; Piechottka, G.P.; Matschiner, G.; Bergner, A. The structure of the human betaII-tryptase tetramer: Fo(u)r better or worse. Proc. Natl. Acad. Sci. USA 1999, 96, 10984–10991. [Google Scholar] [CrossRef] [PubMed]
- Chimenti, M.S.; Triggianese, P.; Botti, E.; Narcisi, A.; Conigliaro, P.; Giunta, A.; Teoli, M.; Perricone, R.; Costanzo, A. S100A8/A9 in psoriatic plaques from patients with psoriatic arthritis. Int. J. Med. Res. 2016, 44, 33–37. [Google Scholar] [CrossRef]
- Couto, D.; Ribeiro, D.; Freitas, M.; Gomes, A.; Lima, J.L.; Fernandes, E. Scavenging of reactive oxygen and nitrogen species by the prodrug sulfasalazine and its metabolites 5-aminosalicylic acid and sulfapyridine. Redox Rep. 2010, 15, 259–267. [Google Scholar] [CrossRef]
- Ozgocmen, S.; Sogut, S.; Ardicoglu, O.; Fadillioglu, E.; Pekkutucu, I.; Akyol, O. Serum nitric oxide, catalase, superoxide dismutase, and malondialdehyde status in patients with ankylosing spondylitis. Rheumatol. Int. 2004, 24, 80–83. [Google Scholar] [CrossRef]
- Yazici, C.; Köse, K.; Calis, M.; Kuzugüden, S.; Kirnap, M. Protein oxidation status in patients with ankylosing spondylitis. Rheumatology 2004, 43, 1235–1239. [Google Scholar] [CrossRef] [PubMed]
- Hassan, S.Z.; Gheita, T.A.; Kenawy, S.A.; Fahim, A.T.; El-Sorougy, I.M.; Abdou, M.S. Oxidative stress in systemic lupus erythematosus and rheumatoid arthritis patients: Relationship to disease manifestations and activity. Int. J. Rheum. Dis. 2011, 14, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Ye, G.; Xie, Z.; Zeng, H.; Wang, P.; Li, J.; Zheng, G.; Wang, S.; Cao, Q.; Li, M.; Liu, W.; et al. Oxidative stress-mediated mitochondrial dysfunction facilitates mesenchymal stem cell senescence in ankylosing spondylitis. Cell Death Dis. 2020, 11, 775. [Google Scholar] [CrossRef]
- Phaniendra, A.; Jestadi, D.B.; Periyasamy, L. Free radicals: Properties, sources, targets, and their implication in various diseases. Indian J. Clin. Biochem. 2015, 30, 11–26. [Google Scholar] [CrossRef]
- Ryter, S.W.; Kim, H.P.; Hoetzel, A.; Park, J.W.; Nakahira, K.; Wang, X.; Choi, A.M. Mechanisms of cell death in oxidative stress. Antioxid. Redox Signal. 2007, 9, 49–89. [Google Scholar] [CrossRef] [PubMed]
- Sardesai, V.M. Role of antioxidants in health maintenance. Nutr. Clin. Pract. 1995, 10, 19–25. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, S.; Cui, Y. Oxidative and Antioxidative Stress Linked Biomarkers in Ankylosing Spondylitis: A Systematic Review and Meta-analysis. Oxidative Med. Cell. Longev. 2020, 2020, 4759451. [Google Scholar] [CrossRef]
- Surh, Y.J.; Kundu, J.K.; Na, H.K.; Lee, J.S. Redox-sensitive transcription factors as prime targets for chemoprevention with anti-inflammatory and antioxidative phytochemicals. J. Nutr. 2005, 135, 2993–3001. [Google Scholar] [CrossRef] [PubMed]
- Stanek, A.; Cieślar, G.; Romuk, E.; Kasperczyk, S.; Sieroń-Stołtny, K.; Birkner, E.; Sieroń, A. Decrease in antioxidant status of plasma and erythrocytes from patients with ankylosing spondylitis. Clin. Biochem. 2010, 43, 566–570. [Google Scholar] [CrossRef] [PubMed]
- Pishgahi, A.; Abolhasan, R.; Danaii, S.; Amanifar, B.; Soltani-Zangbar, M.S.; Zamani, M.; Kamrani, A.; Ghorbani, F.; Mehdizadeh, A.; Kafil, H.S.; et al. Immunological and oxidative stress biomarkers in Ankylosing Spondylitis patients with or without metabolic syndrome. Cytokine 2020, 128, 155002. [Google Scholar] [CrossRef] [PubMed]
- Danaii, S.; Abolhasani, R.; Soltani-Zangbar, M.S.; Zamani, M.; Mehdizadeh, A.; Amanifar, B.; Yousefi, B.; Nazari, M.; Pourlak, T.; Hajialiloo, M.; et al. Oxidative stress and immunological biomarkers in Ankylosing spondylitis patients. Gene Rep. 2020, 18, 100574. [Google Scholar] [CrossRef]
- Adıgüzel, T.K.; Yurdakul, F.G.; Kürklü, N.S.; Yaşar, E.; Bodur, H. Relationship between diet, oxidative stress, and inflammation in ankylosing spondylitis. Arch. Rheumatol. 2021, 37, 1–10. [Google Scholar] [CrossRef]
- Jayson, M.I.; Davis, P.; Whicher, J.T.; Walters, G. Serum copper and caeruloplasmin in ankylosing spondylitis, systemic sclerosis, and morphea. Ann. Rheum. Dis. 1975, 35, 443–445. [Google Scholar] [CrossRef]
- Aiginger, P.; Kolarz, G.; Willvonseder, R. Copper in ankylosing spondylitis and rheumatoid arthritis. Scand. J. Rheumatol. 1978, 7, 75–78. [Google Scholar] [CrossRef]
- Li, T.; Huang, Z.; Zheng, B.; Liao, Z.; Zhao, L.; Gu, J. Serum disease-associated proteins of ankylosing spondylitis: Results of a preliminary study by comparative proteomics. Clin. Exp. Rheumatol. 2010, 28, 201–207. [Google Scholar]
- Salmón, P.; Watson, H.; Nord, A.; Isaksson, C. Effects of the Urban Environment on Oxidative Stress in Early Life: Insights from a Cross-fostering Experiment. Integr. Comp. Biol. 2018, 58, 986–994. [Google Scholar] [CrossRef] [PubMed]
- Damavandi, D.R.; Mousavi, S.N.; Shidfar, F.; Mohammadi, V.; Rajab, A.; Hosseini, S.; Heshmati, J. Effects of Daily Consumption of Cashews on Oxidative Stress and Atherogenic Indices in Patients with Type 2 Diabetes: A Randomized, Controlled-Feeding Trial. Int. J. Endocrinol. Metab. 2019, 17, e70744. [Google Scholar] [CrossRef] [PubMed]
- Vanaki, N.; Aslani, S.; Jamshidi, A.; Mahmoudi, M. Role of innate immune system in the pathogenesis of ankylosing spondylitis. Biomed. Pharmacother. 2018, 105, 130–143. [Google Scholar] [CrossRef] [PubMed]
- Ayala, M.; Muroz, F.; Arguelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxidative Med. Cell. Longev. 2014, 2014, 360438. [Google Scholar] [CrossRef]
- Türkön, H.; Gökmen, F.; Çakir, D.Ü.; Sehitoğlu, M.H.; Reşorlu, H.; Döner, D.; Eşsizoğlu, E.; Akbal, A.; Kizilkaya, B.; Uysal, S. Increased Levels of Serum Ischemia Modified Albumin in Patients with Ankylosing Spondylitis. Clin. Lab. 2016, 62, 645–649. [Google Scholar] [CrossRef]
- Nazıroğlu, M.; Akkuş, S.; Celik, H. Levels of lipid peroxidation and antioxidant vitamins in plasma and erythrocytes of patients with ankylosing spondylitis. Clin. Biochem. 2011, 44, 1412–1415. [Google Scholar] [CrossRef]
- Feng, X.; Yang, Q.; Wang, C.; Tong, W.; Xu, W. Punicalagin Exerts Protective Effects against Ankylosing Spondylitis by Regulating NF-κB-TH17/JAK2/STAT3 Signaling and Oxidative Stress. BioMed Res. 2020, 2020, 4918239. [Google Scholar] [CrossRef]
- Ruef, J.; Hu, Z.Y.; Yin, L.-Y.; Wu, Y.; Hanson, S.R.; Kelly, A.B.; Harker, L.A.; Rao, G.N.; Runge, M.S.; Patterson, C. Induction of Vascular Endothelial Growth Factor in Balloon-Injured Baboon Arteries. Circ. Res. 1997, 81, 24–33. [Google Scholar] [CrossRef]
- Knighton, D.R.; Hunt, T.K.; Scheuenstuhl, H.; Halliday, B.J.; Werb, Z.; Banda, M.J. Oxygen Tension Regulates the Expression of Angiogenesis Factor by Macrophages. Science 1983, 221, 1283–1285. [Google Scholar] [CrossRef]
- Chua, C.C.; Hamdy, R.C.; Chua, B.H.L. Upregulation of Vascular Endothelial Growth Factor by H2O2 in Rat Heart Endothelial Cells. Free Radic. Biol. Med. 1998, 25, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zang, Q.S.; Liu, Z.; Wu, Q.; Maass, D.; Dulan, G.; Shaul, P.W.; Melito, L.; Frantz, D.E.; Kilgore, J.A.; et al. Regulation of VEGF-Induced Endothelial Cell Migration by Mitochondrial Reactive Oxygen Species. Am. J. Physiol. Cell Physiol. 2011, 301, C695–C704. [Google Scholar] [CrossRef] [PubMed]
- Balbir-Gurman, A.; Fuhrman, B.; Braun-Moscovici, Y.; Markovits, D.; Aviram, M. Consumption of pomegranate decreases serum oxidative stress and reduces disease activity in patients with active rheumatoid arthritis: A pilot study. Isr. Med. Assoc. J. 2011, 13, 474–479. [Google Scholar] [PubMed]
- Balogh, E.; Veale, D.J.; McGarry, T.; Orr, C.; Szekanecz, Z.; Ng, C.-T.; Fearon, U.; Biniecka, M. Oxidative Stress Impairs Energy Metabolism in Primary Cells and Synovial Tissue of Patients with Rheumatoid Arthritis. Arthritis Res. Ther. 2018, 20, 95. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Yousaf, M.J.; Rashid, A.; Majeed, A.; Javed, A. Comparison of oxidative stress, lipid peroxidation and inflammatory markers between rheumatoid arthritis and ankylosing spondylitis patients. JPMA. J. Pak. Med. Assoc. 2024, 74, 886–890. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Gao, L.; Jin, D.; Wang, P.; Yang, B.; Deng, W.; Xie, Z.; Tang, Y.; Wu, Y.; Shen, H. The Relationship of Bone Mineral Density to Oxidant/Antioxidant Status and Inflammatory and Bone Turnover Markers in a Multicenter Cross-Sectional Study of Young Men with Ankylosing Spondylitis. Calcif. Tissue Int. 2015, 97, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Stanek, A.; Cholewka, A.; Wielkoszyński, T.; Romuk, E.; Sieroń, K.; Sieroń, A. Increased Levels of Oxidative Stress Markers, Soluble CD40 Ligand, and Carotid Intima-Media Thickness Reflect Acceleration of Atherosclerosis in Male Patients with Ankylosing Spondylitis in Active Phase and without the Classical Cardiovascular Risk Factors. Oxidative Med. Cell. Longev. 2017, 2017, 9712536. [Google Scholar] [CrossRef] [PubMed]
- Jeka, S.; Murawska, A. Ultrasonography of synovium in rheumatological diseases. Reumatologia 2009, 47, 339–343. [Google Scholar]
- Jeka, S. Soft tissue rheumatism. Reumatologia 2012, 50, 166–176. [Google Scholar]
- Kamiński, P.; Wiśniewska, A.; Jerzak, L.; Żuchowski, P.; Jeka, S.; Kavanagh, B.P.; Kozera, W.; Woźniak, A. Ecophysiological Determinants of the Human Skeletal System. Med. Res. J. 2018, 3, 47–54. [Google Scholar] [CrossRef]
- Somers, E.C.; Richardson, B.C. Environmental exposures, epigenetic changes and the risk of lupus. Lupus 2014, 23, 568–576. [Google Scholar] [CrossRef] [PubMed]
- Soleimanifar, N.; Nicknam, M.H.; Bidad, K.; Jamshidi, A.R.; Mahmoudi, M.; Mostafaei, S.; Hosseini-Khah, Z.; Nikbin, B. Effect of food intake and ambient air pollution exposure on ankylosing spondylitis disease activity. Adv. Rheumatol. 2019, 59, 9. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Fu, W.; Meng, L.; Liu, J.; Wu, L.; Peng, Y.; Li, Z. SWE and SMI ultrasound techniques for monitoring needling treatment of ankylosing spondylitis: Study protocol for a single-blinded randomized controlled trial. Trials 2021, 22, 385. [Google Scholar] [CrossRef] [PubMed]
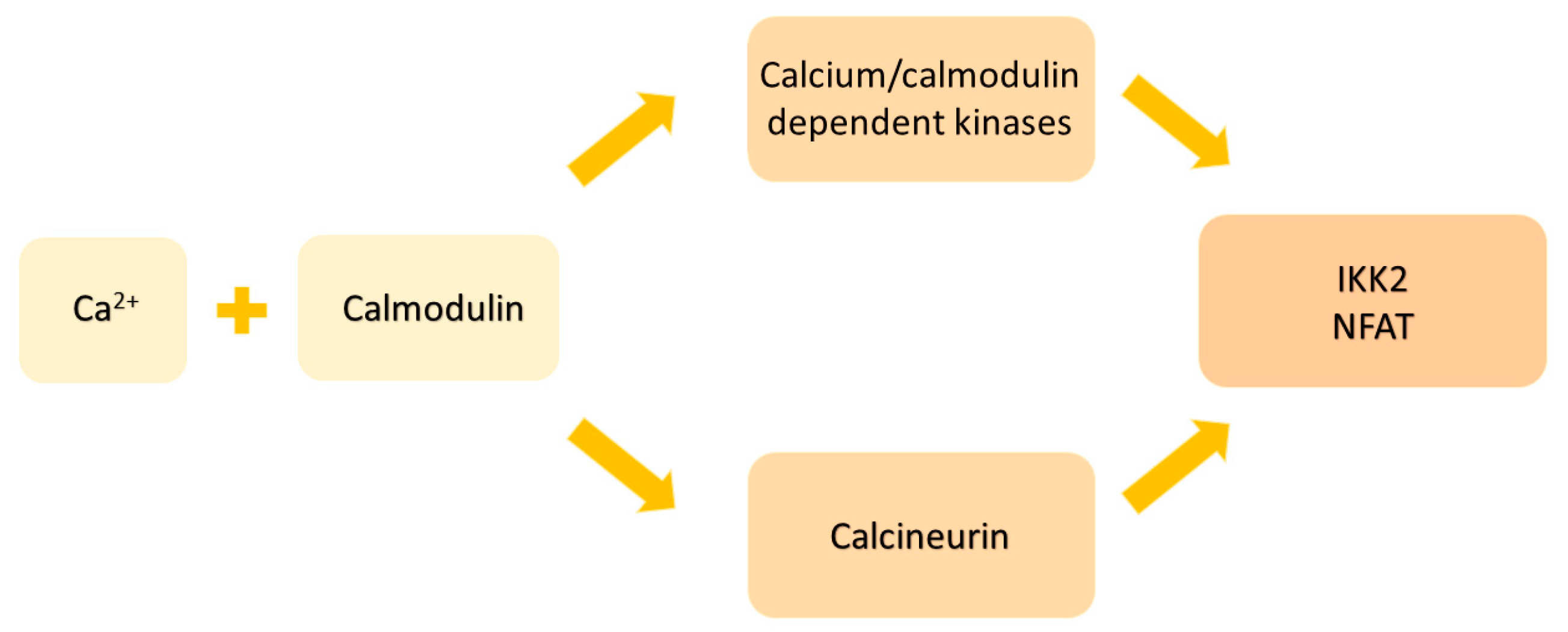
- Huybers, S.; Apostolaki, M.; van der Eerden, B.C.; Kollias, G.; Naber, T.H.; Bindels, R.J.; Hoenderop, J.G. Murine TNFΔARE Crohn’s disease model displays diminished expression of intestinal Ca2+ transporters. Inflamm. Bowel Dis. 2008, 14, 803–811. [Google Scholar] [CrossRef] [PubMed]
- Pinto, M.C.; Kihara, A.H.; Goulart, V.A.; Tonelli, F.M.; Gomes, K.N.; Ulrich, H.; Resende, R.R. Calcium signaling and cell proliferation. Cell. Signal. 2015, 27, 2139–2149. [Google Scholar] [CrossRef] [PubMed]
- Hendy, G.N.; Canaff, L. Calcium-sensing receptor, proinflammatory cytokines and calcium homeostasis. Semin. Cell Dev. Biol. 2016, 49, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Ugan, Y.; Nazıroğlu, M.; Şahin, M.; Aykur, M. Anti-tumor Necrosis Factor Alpha (Infliximab) Attenuates Apoptosis, Oxidative Stress, and Calcium Ion Entry Through Modulation of Cation Channels in Neutrophils of Patients with Ankylosing Spondylitis. J. Membr. Biol. 2016, 249, 437–447. [Google Scholar] [CrossRef] [PubMed]
- Toldi, G.; Munoz, L.; Herrmann, M.; Schett, G.; Balog, A. The effects of Kv1.3 and IKCa1 channel inhibition on cytokine production and calcium influx of T lymphocytes in rheumatoid arthritis and ankylosing spondylitis. Immunol. Res. 2016, 64, 627–631. [Google Scholar] [CrossRef] [PubMed]
- Staud, R. Vitamin D: More than Just Affecting Calcium and Bone. Curr. Rheumatol. Rep. 2005, 7, 356–364. [Google Scholar] [CrossRef]
- Chen, M.; Li, W.; Li, L.; Chai, Y.; Yang, Y.; Pu, X. Ankylosing Spondylitis Disease Activity and Serum Vitamin D Levels: A Systematic Review and Meta-Analysis. Medicine 2022, 101, e31764. [Google Scholar] [CrossRef]
- Diao, M.; Peng, J.; Wang, D.; Wang, H. Peripheral Vitamin D Levels in Ankylosing Spondylitis: A Systematic Review and Meta-Analysis. Front. Med. 2022, 9, 972586. [Google Scholar] [CrossRef] [PubMed]
- Jiang, J.; Shao, M.; Wu, X. Vitamin D and Risk of Ankylosing Spondylitis: A Two-Sample Mendelian Randomization Study. Hum. Immunol. 2022, 83, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.S.; Lee, E.J.; Lee, J.H.; Hong, S.C.; Lee, C.K.; Yoo, B.; Oh, J.S.; Lee, S.H.; Kim, T.J.; Lee, S.H.; et al. Autoantibodies against Protein Phosphatase Magnesium-Dependent 1A as a Biomarker for Predicting Radiographic Progression in Ankylosing Spondylitis Treated with Anti-Tumor Necrosis Factor Agents. J. Clin. Med. 2020, 9, 3968. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Tang, L.; Qi, H.; Zhao, Q.; Liu, Y.; Zhang, Y. Dual Function of Magnesium in Bone Biomineralization. Adv. Healthc. Mater. 2019, 8, e1901030. [Google Scholar] [CrossRef] [PubMed]
- Brenner, M.; Laragione, T.; Gulko, P.S. Short-term low-magnesium diet reduces autoimmune arthritis severity and synovial tissue gene expression. Physiol. Genom. 2017, 49, 238–242. [Google Scholar] [CrossRef] [PubMed]
- Sode, J.; Bank, S.; Vogel, U.; Andersen, P.S.; Sørensen, S.B.; Bojesen, A.B.; Andersen, M.R.; Brandslund, I.; Dessau, R.B.; Hoffmann, H.J.; et al. Genetically determined high activities of the TNF-alpha, IL23/IL17, and NFkB pathways were associated with increased risk of ankylosing spondylitis. BMC Med. Genet. 2018, 19, 165. [Google Scholar] [CrossRef] [PubMed]
- Gönüllü, E.; Bilge, N.Ş.Y.; Cansu, D.U.; Bekmez, M.; Musmul, A.; Akçar, N.; Kaşifoğlu, T.; Korkmaz, C. Risk factors for urolithiasis in patients with ankylosing spondylitis: A prospective case-control study. Urolithiasis 2017, 45, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Kabata-Pendias, A.; Szteke, B. Trace Elements in Abiotic and Biotic Environments, 1st ed.; CRC Press, Taylor & Francis LLC: Boca Raton, FL, USA, 2015; pp. 281–293. [Google Scholar]
- Rayman, M.P.; Pattison, D.J. Dietary Manipulation in Musculoskeletal Conditions. Best Pract. Res. Clin. Rheumatol. 2008, 22, 535–561. [Google Scholar] [CrossRef]
- Deyab, G.; Hokstad, I.; Aaseth, J.; Småstuen, M.C.; Whist, J.E.; Agewall, S.; Lyberg, T.; Tveiten, D.; Hjeltnes, G.; Zibara, K.; et al. Effect of anti-rheumatic treatment on selenium levels in inflammatory arthritis. J. Trace Elem. Med. Biol. 2018, 49, 91–97. [Google Scholar] [CrossRef]
- Sahebari, M.; Rezaieyazdi, Z.; Khodashahi, M. Selenium and Autoimmune Diseases: A Review Article. Curr. Rheumatol. Rev. 2019, 15, 123–134. [Google Scholar] [CrossRef]
- Qamar, N.; John, P.; Bhatti, A. Emerging role of selenium in treatment of rheumatoid arthritis: An insight on its antioxidant properties. J. Trace Elem. Med. Biol. 2021, 66, 126737. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Zhang, X.; Fan, D.; Xia, Q.; Wang, M.; Pan, F. Common Trace Metals in Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. J. Trace Elem. Med. Biol. 2019, 56, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Turrubiates-Hernández, F.J.; Márquez-Sandoval, Y.F.; González-Estevez, G.; Reyes-Castillo, Z.; Muñoz-Valle, J.F. The Relevance of Selenium Status in Rheumatoid Arthritis. Nutrients 2020, 12, 3007. [Google Scholar] [CrossRef] [PubMed]
- Tarp, U.; Overvad, K.; Thorling, E.B.; Graudal, H.; Hansen, J.C. Selenium Treatment in Rheumatoid Arthritis. Scand. J. Rheumatol. 1985, 14, 364–368. [Google Scholar] [CrossRef] [PubMed]
- Jäntti, J.; Vapaatalo, H.; Seppala, E.; Ruutsalo, H.M.; Isomaki, H. Treatment of rheumatoid arthritis with fish oil, selenium, Vitamins A and E, and placebo. Scand. J. Rheumatol. 1991, 20, 225. [Google Scholar]
- Heinlei, K.; Adam, A.; Gradl, M.; Wiseman, M.; Adam, O. Selenkonzentration in den Erythrozyten bei Patienten mit rheumatoider. Arthritis Med. Klin. 1997, 92, 29–31. [Google Scholar] [CrossRef] [PubMed]
- Peretz, A.; Siderova, V.; Nève, J. Selenium supplementation in rheumatoid arthritis investigated in a double blind, placebo-controlled trial. Scand. J. Rheumatol. 2001, 30, 208–212. [Google Scholar]
- Malhotrai, S.; Welling, M.N.; Mantri, S.B.; Desai, K. In vitro and in vivo antioxidant, cytotoxic, and anti-chronic inflammatory arthritic effect of selenium nanoparticles. J. Biomed. Mater. Res. B Appl. Biomater. 2016, 104, 993–1003. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Ma, L.; Zhou, H.; Zhu, X.; Yu, Q.; Chen, X.; Zhao, Y.; Liu, J. Polypeptide Nano-Se Targeting Inflammation and Theranostic Rheumatoid Arthritis by Anti-Angiogenic and NO Activating AMPKα Signaling Pathway. J. Mater. Chem. B 2018, 6, 3497–3514. [Google Scholar] [CrossRef]
- Ren, S.X.; Zhang, B.; Lin, Y.; Ma, D.S.; Yan, H. Selenium Nanoparticles Dispersed in Phytochemical Exert Anti-Inflammatory Activity by Modulating Catalase, GPx1, and COX-2 Gene Expression in a Rheumatoid Arthritis Rat Model. Med. Sci. Monit. 2019, 25, 991–1000. [Google Scholar] [CrossRef]
- Frangos, T.; Maret, W. Zinc and Cadmium in the Aetiology and Pathogenesis of Osteoarthritis and Rheumatoid Arthritis. Nutrients 2021, 13, 53. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Menéndez, S.; García, M.; Fernández, B.; Álvarez, L.; Fernández-Vega-Cueto, A.; Coca-Prados, M.; Pereiro, R.; González-Iglesias, H. The Zinc-Metallothionein Redox System Reduces Oxidative Stress in Retinal Pigment Epithelial Cells. Nutrients 2018, 10, 1874. [Google Scholar] [CrossRef]
- Eide, D.J. The oxidative stress of zinc deficiency. Metallomics 2011, 3, 1124–1129. [Google Scholar] [CrossRef]
- Goggs, R.; Vaughan-Thomas, A.; Clegg, P.D.; Carter, S.D.; Innes, J.F.; Mobasheri, A.; Shakibaei, M.; Schwab, W.; Bondy, C.A. Nutraceutical therapies for degenerative joint diseases: A critical review. Crit. Rev. Food Sci. Nutr. 2005, 45, 145–164. [Google Scholar] [CrossRef] [PubMed]
- Tsai, Y.L.; Ko, W.S.; Hsiao, J.L.; Pan, H.H.; Chiou, Y.L. Zinc sulfate improved the unbalanced T cell profiles in Der p-allergic asthma: An ex vivo study. Clin. Respir. J. 2018, 12, 563–571. [Google Scholar] [CrossRef]
- Higashimura, Y.; Takagi, T.; Naito, Y.; Uchiyama, K.; Mizushima, K.; Tanaka, M.; Hamaguchi, M.; Itoh, Y. Zinc Deficiency Activates the IL-23/Th17 Axis to Aggravate Experimental Colitis in Mice. J. Crohn’s Colitis 2020, 14, 856–866. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Deng, Y.; Ma, Y.; Shao, M.; Ni, M.; Zhang, T.; Wang, X.; Xu, S.; Chen, Y.; Xu, S.; et al. Common mineral nutrients in ankylosing spondylitis: A 2-sample Mendelian randomization study. Int. J. Rheum. Dis. 2022, 25, 1129–1136. [Google Scholar] [CrossRef]
- Afridi, H.I.; Kazi, T.G.; Brabazon, D.; Naher, S. Association between essential trace and toxic elements in scalp hair samples of smokers’ rheumatoid arthritis subjects. Sci. Total Environ. 2011, 412–413, 93–100. [Google Scholar] [CrossRef]
- Mierzecki, A.; Strecker, D.; Radomska, K. A pilot study on zinc levels in patients with rheumatoid arthritis. Biol. Trace Elem. Res. 2011, 143, 854–862. [Google Scholar] [CrossRef]
- Smolen, J.S.; Aletaha, D.; Bijlsma, J.W.J.; Breedveld, F.C.; Boumpas, D.; Burmester, G.; Combe, B.; Cutolo, M.; de Wit, M.; Dougados, M.; et al. Treating Rheumatoid Arthritis to Target: Recommendations of an International Task Force. Ann. Rheum. Dis. 2010, 69, 631–637. [Google Scholar] [CrossRef]
- Hall, S.C.; Knoell, D.L.; Fukada, T.; Kambe, T. Zinc signals in inflammation. In Zinc Signalling; Springer: Singapore, 2019; Volume 2019, pp. 279–304. [Google Scholar]
- Maywald, M.; Rink, L.; Fukada, T.; Kambe, T. Zinc signals in immunology. In Zinc Signalling; Springer: Singapore, 2019; pp. 243–277. [Google Scholar]
- O’Connor, J.P.; Kanjilal, D.; Teitelbaum, M.; Lin, S.S.; Cottrell, J.A. Zinc as a therapeutic agent in bone regeneration. Materials 2020, 13, 2211. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.; Sinha–Royle, E.; Bellis, K.; Harrington, C.; Hutchinson, D. Nodular Rheumatoid Arthritis (RA): A Distinct Disease Subtype, Initiated by Cadmium Inhalation Inducing Pulmonary Nodule Formation and Subsequent RA–Associated Autoantibody Generation. Med. Hypotheses 2019, 122, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Torres, J.; Zamudio-Cuevas, Y.; Martínez-Nava, G.A.; Aztatzi-Aguilar, O.G.; Sierra-Vargas, M.P.; Lozada-Pérez, C.A.; Suárez-Ahedo, C.; Landa-Solís, C.; Olivos-Meza, A.; Del Razo, L.M.; et al. Impact of Cadmium Mediated by Tobacco Use in Musculoskeletal Diseases. Biol. Trace Elem. Res. 2021, 200, 2008–2015. [Google Scholar] [CrossRef] [PubMed]
- Shiue, I. Relationship of environmental exposures and ankylosing spondylitis and spinal mobility: US NHAENS, 2009–2010. Int. J. Environ. Res. Public Health 2015, 25, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Markiewicz-Górka, I.; Chowaniec, M.; Martynowicz, H.; Wojakowska, A.; Jaremków, A.; Mazur, G.; Wiland, P.; Pawlas, K.; Poręba, R.; Gać, P. Cadmium Body Burden and Inflammatory Arthritis: A Pilot Study in Patients from Lower Silesia, Poland. Int. J. Environ. Res. Public Health 2022, 19, 3099. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Demers, L.M.; Vallyathan, V.; Ding, M.; Lu, Y.; Castranova, V.; Shi, X. Vanadate induction of NF-κB involves IκB kinase β and SAPK/ERK kinase 1 in macrophages. J. Biol. Chem. 1999, 274, 20307–20312. [Google Scholar] [CrossRef] [PubMed]
- Pessoa, J.C. Thirty years through vanadium chemistry. J. Inorg. Biochem. 2015, 147, 4–24. [Google Scholar] [CrossRef] [PubMed]
- Sparks, J.A.; Chen, C.Y.; Hiraki, L.T.; Malspeis, S.; Costenbader, K.H.; Karlson, E.W. Contributions of familial rheumatoid arthritis or lupus and environmental factors to risk of rheumatoid arthritis in women: A prospective cohort study. Arthritis Care Res. 2014, 66, 1438–1446. [Google Scholar] [CrossRef] [PubMed]
- Pfohler, C.; Muller, C.S.; Vogt, T. Psoriasis vulgaris and psoriasis pustulosa—Epidemiology, quality of life, comorbidities and treatment. Curr. Rheumatol. Rev. 2013, 9, 2–7. [Google Scholar] [CrossRef]
- Yazisiz, V.; Arslan, G.; Ozbudak, I.H.; Turker, S.; Erbasan, F.; Avci, A.B.; Ozbudak, O.; Terzioglu, E. Lung involvement in patients with primary Sjögren’s syndrome: What are the predictors? Rheumatol. Int. 2010, 30, 1317–1324. [Google Scholar] [CrossRef]
- Jiang, L.; Yin, J.; Ye, L.; Yang, J.; Hemani, G.; Liu, A.J.; Zou, H.; He, D.; Sun, L.; Zeng, X.; et al. Novel risk loci for rheumatoid arthritis in Han Chinese and congruence with risk variants in Europeans. Arthritis Rheumatol. 2014, 66, 1121–1132. [Google Scholar] [CrossRef] [PubMed]
- Saevarsdottir, S.; Rezaei, H.; Geborek, P.; Petersson, I.; Ernestam, S.; Albertsson, K.; Forslind, K.; van Vollenhoven, R.F.; SWEFOT Study Group. Current smoking status is a strong predictor of radiographic progression in early rheumatoid arthritis: Results from the SWEFOT trial. Ann. Rheum. Dis. 2015, 74, 1509–1514. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Chen, H.A.; Lu, C.L.; Liao, H.T.; Liu, C.H.; Tsai, C.Y.; Chou, C.T. Association of cigarette smoking with Chinese ankylosing spondylitis patients in Taiwan: A poor disease outcome in systemic inflammation, functional ability, and physical mobility. Clin. Rheumatol. 2013, 32, 659–663. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Li, Y.; Xu, X.; Feng, X.; Yang, D.; Lin, G. Effect of cigarette smoking and alcohol consumption on disease activity and physical functioning in ankylosing spondylitis: A cross-sectional study. Int. J. Clin. Exp. 2015, 8, 13919–13927. [Google Scholar]
- Zhao, S.; Jones, G.T.; Macfarlane, G.J.; Hughes, D.M.; Dean, L.E.; Moots, R.J.; Goodson, N.J. Associations between smoking and extra-axial manifestations and disease severity in axial spondyloarthritis: Results from the BSR Biologics Register for Ankylosing Spondylitis (BSRBR-AS). Rheumatology 2019, 58, 811–819. [Google Scholar] [CrossRef] [PubMed]
- Hu, Z.; Li, Y.; Hu, L.; Ji, X.; Wang, L.; Li, K.; Zhu, J.; Zhang, J.; Huang, F. Cigarette Smoking Increases the Prevalence of Hip Joint Involvement in Ankylosing Spondylitis: A Real-World Case-Control Study. J. Rheumatol. 2023, 50, 901–906. [Google Scholar] [CrossRef] [PubMed]
- Myllykangas-Luosujärvi, R.; Aho, K.; Lehtinen, K.; Kautiainen, H.; Hakala, M. Increased incidence of alcohol-related deaths from accidents and violence in subjects with ankylosing spondylitis. Br. J. Rheumatol. 1998, 37, 688–690. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Thong, D.; Duffield, S.J.; Hughes, D.; Goodson, N.J. Alcohol and disease activity in axial spondyloarthritis: A cross-sectional study. Rheumatol. Int. 2018, 38, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Min, H.K.; Lee, J.; Ju, J.H.; Park, S.-H.; Kwok, S.-K. Alcohol consumption as a predictor of the progression of spinal structural damage in axial spondyloarthritis: Data from the Catholic Axial Spondyloarthritis COhort (CASCO). Arthritis Res. Ther. 2019, 21, 187. [Google Scholar] [CrossRef]
- Du, K.; Zhang, C.Y.; Li, A.; Hu, J.Z.; Guo, R.; Li, S.M. Causality of occupational exposure on rheumatoid arthritis and ankylosing spondylitis: A two-sample mendelian randomization study. Front. Immunol. 2023, 14, 1223810. [Google Scholar] [CrossRef]
- Hu, S.; Xing, H.; Wang, X.; Zhang, N.; Xu, Q. Causal Relationships Between Total Physical Activity and Ankylosing Spondylitis: A Mendelian Randomization Study. Front Immunol. 2022, 13, 887326. [Google Scholar] [CrossRef] [PubMed]
- Batmaz, İ.; Sarıyıldız, M.A.; Dilek, B.; Bez, Y.; Karakoç, M.; Çevik, R. Sleep Quality and Associated Factors in Ankylosing Spondylitis: Relationship with Disease Parameters, Psychological Status and Quality of Life. Rheumatol. Int. 2012, 33, 1039–1045. [Google Scholar] [CrossRef]
- Yüce, E.; Şentürk, E.; Sağaltıcı, E.; Şentürk, İ.A.; Aytekin, E. Sleep quality and depression in patients with ankylosing spondylitis and their associations with clinical parameters: A cross-sectional, case-control study. Ankilozan spondilitli hastalarda uyku kalitesi, depresyon ve bunların klinik parametrelerle ilişkisi: Kesitsel, vaka-kontrol çalışması. AGRI 2023, 35, 1–9. [Google Scholar] [PubMed]
- Aydin, E.; Bayraktar, K.; Turan, Y.; Omurlu, I.; Tastaban, E.; Sendur, O.F. Qualidade Do Sono Em Pacientes Com Espondilite Anquilosante. Rev. Bras. Reumatol. 2015, 55, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Vergne-Salle, P.; Salle, L.; Fressinaud-Marie, A.C.; Descamps-Deplas, A.; Montestruc, F.; Bonnet, C.; Bertin, P. Diet and Disease Activity in Patients with Axial Spondyloarthritis: SpondyloArthritis and NUTrition Study (SANUT). Nutrients 2022, 14, 4730. [Google Scholar] [CrossRef] [PubMed]
- Kao, C.M.; Chen, Y.M.; Huang, W.N.; Chen, Y.H.; Chen, H.H. Association between air pollutants and initiation of biological therapy in patients with ankylosing spondylitis: A nationwide, population-based, nested case-control study. Arthritis Res. Ther. 2023, 25, 75. [Google Scholar] [CrossRef] [PubMed]
- Bartels, L.E.; Pedersen, A.B.; Kristensen, N.R.; Vilstrup, H.; Stengaard-Pedersen, K.; Dahlerup, J.F. A positive Helicobacter pylori test is associated with low spondylarthritis incidence in a Danish historical cohort study. Rheumatol. Int. 2020, 40, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, P.R.; Kragstrup, T.W.; Deleuran, B.W.; Benros, M.E. Infections as risk factor for autoimmune diseases—A nationwide study. J. Autoimmun. 2016, 74, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Stone, M.A.; Payne, U.; Schentag, C.; Rahman, P.; Pacheco-Tena, C.; Inman, R.D. Comparative immune responses to candidate arthritogenic bacteria do not confirm a dominant role for Klebsiella pneumonia in the pathogenesis of familial ankylosing spondylitis. Rheumatology 2004, 43, 148–155. [Google Scholar] [CrossRef]
- Keller, J.J.; Kang, J.H.; Lin, H.C. Association between ankylosing spondylitis and chronic periodontitis: A population-based study. Arthritis Rheumatol. 2013, 65, 167–173. [Google Scholar] [CrossRef]
- Wei, C.Y.; Lin, J.Y.; Wang, Y.T.; Huang, J.Y.; Wei, J.C.; Chiou, J.Y. Risk of ankylosing spondylitis following human papillomavirus infection: A nationwide, population-based, cohort study. J. Autoimmun. 2020, 113, 102482. [Google Scholar] [CrossRef]
- Damba, J.J.; Laskine, M.; Jin, Y.; Sinyavskaya, L.; Durand, M. Incidence of autoimmune diseases in people living with HIV compared to a matched population: A cohort study. Clin. Rheumatol. 2021, 40, 2439–2445. [Google Scholar] [CrossRef] [PubMed]
- Yen, Y.F.; Chuang, P.H.; Jen, I.A.; Chen, M.; Lan, Y.C.; Liu, Y.L.; Lee, Y.; Chen, Y.H.; Chen, Y.A. Incidence of autoimmune diseases in a nationwide HIV/AIDS patient cohort in Taiwan, 2000–2012. Ann. Rheum. Dis. 2017, 76, 661–665. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.C.; Chou, M.C.; Huang, J.Y.; Chang, R.; Hung, Y.M. The association between Candida infection and ankylosing spondylitis: A population-based matched cohort study. Curr. Med. Res. Opin. 2020, 36, 2063–2069. [Google Scholar] [CrossRef] [PubMed]
- Chu, K.A.; Chen, W.; Hung, Y.M.; Wei, J.C. Increased risk of ankylosing spondylitis after Mycoplasma pneumonia: A Nationwide population-based study. Medicine 2019, 98, e15596. [Google Scholar] [CrossRef] [PubMed]
- Feng, X.G.; Xu, X.J.; Ye, S.; Lin, Y.Y.; Chen, P.; Zhang, X.J.; Lin, G.Y.; Lin, X.Q. Recent Chlamydia pneumoniae infection is highly associated with active ankylosing spondylitis in a Chinese cohort. Scand. J. Rheumatol. 2011, 40, 289–291. [Google Scholar]
- Lindström, U.; Exarchou, S.; Lie, E.; Dehlin, M.; Forsblad-d’Elia, H.; Askling, J.; Jacobsson, L. Childhood hospitalisation with infections and later development of ankylosing spondylitis: A national case-control study. Arthritis Res. Ther. 2016, 18, 240. [Google Scholar] [CrossRef] [PubMed]
- Chao, W.C.; Lin, C.H.; Chen, Y.M.; Jiang, R.S.; Chen, H.H. Association between tonsillitis and newly diagnosed ankylosing spondylitis: A nationwide, population-based, case-control study. PLoS ONE 2019, 14, e0220721. [Google Scholar] [CrossRef] [PubMed]
- Abbood, H.M.; Pathan, E.; Cherukara, G.P. The link between ankylosing spondylitis and oral health conditions: Two nested case-control studies using data of the UK Biobank. J. Appl. Oral Sci. 2018, 27, e20180207. [Google Scholar] [CrossRef]
- Bartels, L.E.; Jepsen, P.; Christensen, L.A.; Gerdes, L.U.; Vilstrup, H.; Dahlerup, J.F. Diagnosis of Helicobacter Pylori Infection is Associated with Lower Prevalence and Subsequent Incidence of Crohn’s Disease. J. Crohn’s Colitis 2016, 10, 443–448. [Google Scholar] [CrossRef]
- Yap, T.W.; Gan, H.M.; Lee, Y.P.; Leow, A.H.; Azmi, A.N.; Francois, F.; Perez-Perez, G.I.; Loke, M.F.; Goh, K.L.; Vadivelu, J. Helicobacter pylori Eradication Causes Perturbation of the Human Gut Microbiome in Young Adults. PLoS ONE 2016, 11, e0151893. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Wang, L.; Wang, X.; Xian, C.J.; Lu, H. A Possible Role of Intestinal Microbiota in the Pathogenesis of Ankylosing Spondylitis. Int. J. Mol. Sci. 2016, 17, 2126. [Google Scholar] [CrossRef]
- Al-Katma, M.K.; Bissada, N.F.; Bordeaux, J.M.; Sue, J.; Askari, A.D. Control of periodontal infection reduces the severity of active rheumatoid arthritis. J. Clin. Rheumatol. 2007, 13, 134–137. [Google Scholar] [CrossRef]
- de Pablo, P.; Dietrich, T.; McAlindon, T.E. Association of periodontal disease and tooth loss with rheumatoid arthritis in the US population. J. Rheumatol. 2008, 35, 70–76. [Google Scholar] [PubMed]
- Pischon, N.; Pischon, T.; Kröger, J.; Gülmez, E.; Kleber, B.M.; Bernimoulin, J.P.; Landau, H.; Brinkmann, P.G.; Schlattmann, P.; Zernicke, J.; et al. Association among rheumatoid arthritis, oral hygiene, and periodontitis. J. Periodontol. 2008, 79, 979–986. [Google Scholar] [CrossRef]
- Palomares, O.; Rückert, B.; Jartti, T.; Kücüksezer, U.C.; Puhakka, T.; Gomez, E.; Fahrner, H.B.; Speiser, A.; Jung, A.; Kwok, W.W.; et al. Induction and maintenance of allergen-specific FOXP3+ Treg cells in human tonsils as potential first-line organs of oral tolerance. J. Allergy Clin. Immunol. 2012, 129, 510–520.e9. [Google Scholar] [CrossRef] [PubMed]
- Itescu, S.; Dalton, J.; Zhang, H.Z.; Winchester, R. Tissue infiltration in a CD8 lymphocytosis syndrome associated with human immunodeficiency virus-1 infection has the phenotypic appearance of an antigenically driven response. J. Clin. Investig. 1993, 91, 2216–2225. [Google Scholar] [CrossRef]
- Fife, D.J.; Waller, J.M.; Jeffes, E.W.; Koo, J.Y. Unraveling the paradoxes of HIV-associated psoriasis: A review of T-cell subsets and cytokine profiles. Dermatol. Online J. 2007, 13, 4. [Google Scholar] [CrossRef]
- Russo, S.; Lopalco, L. Is autoimmunity a component of natural immunity to HIV? Curr. HIV Res. 2006, 4, 177–190. [Google Scholar] [CrossRef]
- Zhou, C.; Zhao, H.; Xiao, X.Y.; Chen, B.D.; Guo, R.J.; Wang, Q.; Chen, H.; Zhao, L.D.; Zhang, C.C.; Jiao, Y.H.; et al. Metagenomic profiling of the pro-inflammatory gut microbiota in ankylosing spondylitis. J. Autoimmun. 2020, 107, 102360. [Google Scholar] [CrossRef]
- Liu, G.; Hao, Y.; Yang, Q.; Deng, S. The Association of Fecal Microbiota in Ankylosing Spondylitis Cases with C-Reactive Protein and Erythrocyte Sedimentation Rate. Mediat. Inflamm. 2020, 2020, 8884324. [Google Scholar] [CrossRef] [PubMed]
- Costello, M.E.; Ciccia, F.; Willner, D.; Warrington, N.; Robinson, P.C.; Gardiner, B.; Marshall, M.; Kenna, T.J.; Triolo, G.; Brown, M.A. Brief Report: Intestinal Dysbiosis in Ankylosing Spondylitis. Arthritis Rheumatol. 2015, 67, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Dai, B.; Tang, Y.; Lei, L.; Li, N.; Liu, C.; Ge, T.; Zhang, L.; Xu, Y.; Hu, Y.; et al. Altered Bacterial-Fungal Interkingdom Networks in the Guts of Ankylosing Spondylitis Patients. mSystems 2019, 4, e00176-18. [Google Scholar] [CrossRef] [PubMed]
- Ebringer, R.W.; Cawdell, D.R.; Cowling, P.; Ebringer, A. Sequential studies in ankylosing spondylitis. association of klebsiella pneumoniae with active disease. Ann. Rheum. Dis. 1978, 37, 146–151. [Google Scholar] [CrossRef] [PubMed]
- Mäki-Ikola, O.; Leirisalo-Repo, M.; Turunen, U.; Granfors, K. Association of gut inflammation with increased serum IgA class Klebsiella antibody concentrations in patients with axial ankylosing spondylitis (AS): Implication for different aetiopathogenetic mechanisms for axial and peripheral AS? Ann. Rheum. Dis. 1997, 56, 180–183. [Google Scholar] [CrossRef] [PubMed]
- Wen, C.; Zheng, Z.; Shao, T.; Liu, L.; Xie, Z.; Le Chatelier, E.; He, Z.; Zhong, W.; Fan, Y.; Zhang, L.; et al. Quantitative metagenomics reveals unique gut microbiome biomarkers in ankylosing spondylitis. Genome Biol. 2017, 18, 142. [Google Scholar]
- Laurence, M.; Asquith, M.; Rosenbaum, J.T. Spondyloarthritis, Acute Anterior Uveitis, and Fungi: Updating the Catterall-King Hypothesis. Front. Med. 2018, 5, 80. [Google Scholar] [CrossRef]
- Hammer, R.E.; Maika, S.D.; Richardson, J.A.; Tang, J.P.; Taurog, J.D. Spontaneous inflammatory disease in transgenic rats expressing HLA-B27 and human beta 2m: An animal model of HLA-B27-associated human disorders. Cell 1990, 63, 1099–1112. [Google Scholar] [CrossRef] [PubMed]
- Glatigny, S.; Fert, I.; Blaton, M.A.; Lories, R.J.; Araujo, L.M.; Chiocchia, G.; Breban, M. Proinflammatory Th17 cells are expanded and induced by dendritic cells in spondylarthritis-prone HLA-B27-transgenic rats. Arthritis Rheum. 2012, 64, 110–120. [Google Scholar] [CrossRef]
- Taurog, J.D.; Richardson, J.A.; Croft, J.T.; Simmons, W.A.; Zhou, M.; Fernández-Sueiro, J.L.; Balish, E.; Hammer, R.E. The germfree state prevents development of gut and joint inflammatory disease in HLA-B27 transgenic rats. J. Exp. Med. 1994, 180, 2359–2364. [Google Scholar] [CrossRef]
- Rath, H.C.; Herfarth, H.H.; Ikeda, J.S.; Grenther, W.B.; Hamm, T.E.; Balish, E., Jr.; Taurog, J.D.; Hammer, R.E.; Wilson, K.H.; Sartor, R.B. Normal luminal bacteria, especially Bacteroides species, mediate chronic colitis, gastritis, and arthritis in HLA-B27/human beta2 microglobulin transgenic rats. J. Clin. Investig. 1996, 98, 945–953. [Google Scholar] [CrossRef] [PubMed]
- Schlosstein, L.; Terasaki, P.I.; Bluestone, R.; Pearson, C.M. High association of an HL-A antigen, W27, with ankylosing spondylitis. N. Engl. J. Med. 1973, 288, 704–706. [Google Scholar] [CrossRef] [PubMed]
- Taurog, J.D.; Chhabra, A.; Colbert, R.A. Ankylosing Spondylitis and Axial Spondyloarthritis. N. Engl. J. Med. 2016, 374, 2563–2574. [Google Scholar] [CrossRef] [PubMed]
- Rudwaleit, M.; van der Heijde, D.; Landewé, R.; Listing, J.; Akkoc, N.; Brandt, J.; Braun, J.; Chou, C.T.; Collantes-Estevez, E.; Dougados, M.; et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): Validation and final selection. Ann. Rheum. Dis. 2009, 68, 777–783. [Google Scholar] [CrossRef] [PubMed]
- Rudwaleit, M.; van der Heijde, D.; Landewé, R.; Akkoc, N.; Brandt, J.; Chou, C.T.; Dougados, M.; Huang, F.; Gu, J.; Kirazli, Y.; et al. The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann. Rheum. Dis. 2011, 70, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Casanova, J.L.; Puel, A. Mucocutaneous IL-17 immunity in mice and humans: Host defense vs. excessive inflammation. Mucosal Immunol. 2018, 11, 581–589. [Google Scholar] [CrossRef] [PubMed]
- Fragoulis, G.E.; Liava, C.; Daoussis, D.; Akriviadis, E.; Garyfallos, A.; Dimitroulas, T. Inflammatory bowel diseases and spondyloarthropathies: From pathogenesis to treatment. World J. Gastroenterol. 2019, 25, 2162–2176. [Google Scholar] [CrossRef] [PubMed]
- DeLay, M.L.; Turner, M.J.; Klenk, E.I.; Smith, J.A.; Sowders, D.P.; Colbert, R.A. HLA-B27 misfolding and the unfolded protein response augment interleukin-23 production and are associated with Th17 activation in transgenic rats. Arthritis Rheumatol. 2009, 60, 2633–2643. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Torchinsky, M.B.; Gobert, M.; Xiong, H.; Xu, M.; Linehan, J.L.; Alonzo, F.; Ng, C.; Chen, A.; Lin, X.; et al. Focused specificity of intestinal TH17 cells towards commensal bacterial antigens. Nature 2014, 510, 152–156. [Google Scholar] [CrossRef]
- Zielinski, C.E.; Mele, F.; Aschenbrenner, D.; Jarrossay, D.; Ronchi, F.; Gattorno, M.; Monticelli, S.; Lanzavecchia, A.; Sallusto, F. Pathogen-induced human TH17 cells produce IFN-γ or IL-10 and are regulated by IL-1β. Nature 2012, 484, 514–518. [Google Scholar] [CrossRef]
- Larsen, J.M. The immune response to prevotella bacteria in chronic inflammatory disease. Immunology 2017, 151, 363–374. [Google Scholar] [CrossRef]
- Goto, Y.; Panea, C.; Nakato, G.; Cebula, A.; Lee, C.; Diez, M.G.; Laufer, T.M.; Ignatowicz, L.; Ivanov, I.I. Segmented filamentous bacteria antigens presented by intestinal dendritic cells drive mucosal Th17 cell differentiation. Immunity 2014, 40, 594–607. [Google Scholar] [CrossRef]
- Rogier, R.; Koenders, M.I.; Abdollahi-Roodsaz, S. Toll-like receptor mediated modulation of T cell response by commensal intestinal microbiota as a trigger for autoimmune arthritis. J. Immunol. Res. 2015, 2015, 527696. [Google Scholar] [CrossRef]
- Ivanov, I.I.; Frutos, R. deL.; Manel, N.; Yoshinaga, K.; Rifkin, D.B.; Sartor, R.B.; Finlay, B.B.; Littman, D.R. Specific microbiota direct the differentiation of IL-17-producing T-helper cells in the mucosa of the small intestine. Cell Host Microbe 2008, 4, 337–349. [Google Scholar] [CrossRef]
- Chambers, R.E.; MacFarlane, D.G.; Whicher, J.T.; Dieppe, P.A. Serum amyloid-A protein concentration in rheumatoid arthritis and its role in monitoring disease activity. Ann. Rheum. Dis. 1983, 42, 665–667. [Google Scholar] [CrossRef]
- Geuking, M.B.; Cahenzli, J.; Lawson, M.A.; Ng, D.C.; Slack, E.; Hapfelmeier, S.; McCoy, K.D.; Macpherson, A.J. Intestinal bacterial colonization induces mutualistic regulatory T cell responses. Immunity 2010, 34, 794–806. [Google Scholar] [CrossRef]
- Round, J.L.; Lee, S.M.; Li, J.; Tran, G.; Jabri, B.; Chatila, T.A.; Mazmanian, S.K. The Toll-like receptor 2 pathway establishes colonization by a commensal of the human microbiota. Science 2011, 332, 974–977. [Google Scholar] [CrossRef]
- Round, J.L.; Mazmanian, S.K. Inducible Foxp3+ regulatory T-cell development by a commensal bacterium of the intestinal microbiota. Proc. Natl. Acad. Sci. USA 2010, 107, 12204–12209. [Google Scholar] [CrossRef]
- Smith, P.M.; Howitt, M.R.; Panikov, N.; Michaud, M.; Gallini, C.A.; Bohlooly-Y, M.; Glickman, J.N.; Garrett, W.S. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 2013, 341, 569–573. [Google Scholar] [CrossRef] [PubMed]
- Song, Z.Y.; Yuan, D.; Zhang, S.X. Role of the microbiome and its metabolites in ankylosing spondylitis. Front. Immunol. 2022, 13, 1010572. [Google Scholar] [CrossRef] [PubMed]
- Galocha, B.; López de Castro, J.A. Mutational analysis reveals a complex interplay of peptide binding and multiple biological features of HLA-B27. J. Biol. Chem. 2010, 285, 39180–39190. [Google Scholar] [CrossRef] [PubMed]
- Madden, D.R. The three-dimensional structure of peptide-MHC complexes. Annu. Rev. Immunol. 1995, 13, 587–622. [Google Scholar] [CrossRef] [PubMed]
- Toh, H.; Savoie, C.J.; Kamikawaji, N.; Muta, S.; Sasazuki, T.; Kuhara, S. Changes at the floor of the peptide-binding groove induce a strong preference for proline at position 3 of the bound peptide: Molecular dynamics simulations of HLA-A*0217. Biopolymers 2000, 54, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.T.; Chang, S.C.; Evnouchidou, I.; York, I.A.; Zikos, C.; Rock, K.L.; Goldberg, A.L.; Stratikos, E.; Stern, L.J. Structural basis for antigenic peptide precursor processing by the endoplasmic reticulum aminopeptidase ERAP1. Nat. Struct. Mol. Biol. 2011, 18, 604–613. [Google Scholar] [CrossRef] [PubMed]
- Yewdell, J.W. DRiPs solidify: Progress in understanding endogenous MHC class I antigen processing. Trends Immunol. 2011, 32, 548–558. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Navarro, C.; López de Castro, J.A. ERAP1 structure, function and pathogenetic role in ankylosing spondylitis and other MHC-associated diseases. Mol. Immunol. 2014, 57, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Schittenhelm, R.B.; Sian, T.C.; Wilmann, P.G.; Dudek, N.L.; Purcell, A.W. Revisiting the arthritogenic peptide theory: Quantitative not qualitative changes in the peptide repertoire of HLA-B27 allotypes. Arthritis Rheumatol. 2015, 67, 702–713. [Google Scholar] [CrossRef] [PubMed]
- Australo-Anglo-American Spondyloarthritis Consortium (TASC); Reveille, J.D.; Sims, A.M.; Danoy, P.; Evans, D.M.; Leo, P.; Pointon, J.J.; Jin, R.; Zhou, X.; Bradbury, L.A.; et al. Genome-wide association study of ankylosing spondylitis identifies non-MHC susceptibility loci. Nat. Genet. 2010, 42, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Evans, D.M.; Spencer, C.C.; Pointon, J.J.; Su, Z.; Harvey, D.; Kochan, G.; Oppermann, U.; Dilthey, A.; Pirinen, M.; Stone, M.A.; et al. Interaction between ERAP1 and HLA-B27 in ankylosing spondylitis implicates peptide handling in the mechanism for HLA-B27 in disease susceptibility. Nat. Genet. 2011, 43, 761–767. [Google Scholar] [CrossRef]
- Chatzikyriakidou, A.; Voulgari, P.V.; Drosos, A.A. What is the role of HLA-B27 in spondyloarthropathies? Autoimmun. Rev. 2011, 10, 464–468. [Google Scholar] [CrossRef]
- Faham, M.; Carlton, V.; Moorhead, M.; Zheng, J.; Klinger, M.; Pepin, F.; Asbury, T.; Vignali, M.; Emerson, R.O.; Robins, H.S.; et al. Discovery of T Cell Receptor β Motifs Specific to HLA-B27-Positive Ankylosing Spondylitis by Deep Repertoire Sequence Analysis. Arthritis Rheumatol. 2017, 69, 774–784. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, A.N.; Ford, S.; Taurog, J.D.; Butcher, G.W.; Powis, S.J. Formation of HLA-B27 homodimers and their relationship to assembly kinetics. J. Biol. Chem. 2004, 279, 8895–8902. [Google Scholar] [CrossRef] [PubMed]
- Colbert, R.A.; DeLay, M.L.; Layh-Schmitt, G.; Sowders, D.P. HLA-B27 misfolding and spondyloarthropathies. Prion 2009, 3, 15–26. [Google Scholar] [CrossRef] [PubMed]
- Bowness, P.; Ridley, A.; Shaw, J.; Chan, A.T.; Wong-Baeza, I.; Fleming, M.; Cummings, F.; McMichael, A.; Kollnberger, S. Th17 cells expressing KIR3DL2+ and responsive to HLA-B27 homodimers are increased in ankylosing spondylitis. J. Immunol. 2011, 186, 2672–2680. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Wu, J.; Li, X.; Wei, Q.; Lv, Q.; Zhang, P.; Zheng, X.; Chen, Z.; Cao, S.; Tu, L.; et al. The Clinical Characteristics of Other HLA-B Types in Chinese Ankylosing Spondylitis Patients. Front. Med. 2021, 7, 568790. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.A.; Pile, K.D.; Kennedy, L.G.; Calin, A.; Darke, C.; Bell, J.; Wordsworth, B.P.; Cornélis, F. HLA class I associations of ankylosing spondylitis in the white population in the United Kingdom. Ann. Rheum. Dis. 1996, 55, 268–270. [Google Scholar] [CrossRef]
- Brown, M.A.; Kennedy, L.G.; MacGregor, A.J.; Darke, C.; Duncan, E.; Shatford, J.L.; Taylor, A.; Calin, A.; Wordsworth, P. Susceptibility to ankylosing spondylitis in twins: The role of genes, HLA, and the environment. Arthritis Rheum. 1997, 40, 1823–1828. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.C.; Tsai, W.C.; Lin, H.S.; Tsai, C.Y.; Chou, C.T. HLA-B60 and B61 are strongly associated with ankylosing spondylitis in HLA-B27-negative Taiwan Chinese patients. Rheumatology 2004, 43, 839–842. [Google Scholar] [CrossRef]
- International Genetics of Ankylosing Spondylitis Consortium (IGAS). Identification of multiple risk variants for ankylosing spondylitis through high-density genotyping of immune-related loci. Nat. Genet. 2013, 45, 730–738. [Google Scholar] [CrossRef]
- López-Larrea, C.; Mijiyawa, M.; González, S.; Fernández-Morera, J.L.; Blanco-Gelaz, M.A.; Martínez-Borra, J.; López-Vázquez, A. Association of ankylosing spondylitis with HLA-B*1403 in a West African population. Arthritis Rheum. 2002, 46, 2968–2971. [Google Scholar] [CrossRef]
- Díaz-Peña, R.; Blanco-Gelaz, M.A.; Njobvu, P.; López-Vazquez, A.; Suárez-Alvarez, B.; López-Larrea, C. Influence of HLA-B*5703 and HLA-B*1403 on susceptibility to spondyloarthropathies in the Zambian population. J. Rheumatol. 2008, 35, 2236–2240. [Google Scholar] [CrossRef] [PubMed]
- Remans, P.H.; Wijbrandts, C.A.; Sanders, M.E.; Toes, R.E.; Breedveld, F.C.; Tak, P.P.; van Laar, J.M.; Reedquist, K.A. CTLA-4IG suppresses reactive oxygen species by preventing synovial adherent cell-induced inactivation of Rap1, a Ras family GTPASE mediator of oxidative stress in rheumatoid arthritis T cells. Arthritis Rheum. 2006, 54, 3135–3143. [Google Scholar] [CrossRef] [PubMed]
- Dahmani, C.A.; Benzaoui, A.; Amroun, H.; Mecabih, F.; Sediki, F.Z.; Zemani-Fodil, F.; Fodil, M.; Boughrara, W.; Mecheti, B.; Attal, N.; et al. Association of the HLA-B27 antigen and the CTLA4 gene CT60/rs3087243 polymorphism with ankylosing spondylitis in Algerian population: A case-control study. Int. J. Immunogenet. 2018, 45, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Zhang, P.; Dong, J. Genetic variants of STAT4 are associated with ankylosing spondylitis susceptibility and severity in a Chinese Han population. Int. J. Clin. Exp. Med. 2014, 7, 5877–5881. [Google Scholar] [PubMed]
- Ebrahimiyan, H.; Mostafaei, S.; Aslani, S.; Jamshidi, A.; Mahmoudi, M. Studying the Association between STAT4 Gene Polymorphism and Susceptibility to Rheumatoid Arthritis Disease: An Updated Meta-Analysis. Iran. J. Immunol. 2019, 16, 71–83. [Google Scholar] [PubMed]
- García-Ruiz, I.; de la Torre, P.; Díaz, T.; Esteban, E.; Fernández, I.; Muñoz-Yagüe, T.; Solís-Herruzo, J.A. Sp1 and Sp3 transcription factors mediate malondialdehyde-induced collagen alpha 1(I) gene expression in cultured hepatic stellate cells. J. Biol. Chem. 2002, 277, 30551–30558. [Google Scholar] [CrossRef] [PubMed]
- Gao, M.; Li, T.; Song, Z.; Wang, X.; Zhang, X.; Liu, W. Relationship Between IL1 Gene Polymorphism and Susceptibility to Ankylosing Spondylitis: An Updated and Supplemented Meta-Analysis. Biochem. Genet. 2022, 60, 1025–1038. [Google Scholar] [CrossRef]
- Biały, S.; Iwaszko, M.; Świerkot, J.; Bugaj, B.; Kolossa, K.; Jeka, S.; Bogunia-Kubik, K. Th2 Cytokines (Interleukin-5 and -9) Polymorphism Affects the Response to Anti-TNF Treatment in Polish Patients with Ankylosing Spondylitis. Int. J. Mol. Sci. 2022, 23, 13177. [Google Scholar] [CrossRef]
- Wielińska, J.; Świerkot, J.; Kolossa, K.; Bugaj, B.; Chaszczewska-Markowska, M.; Jeka, S.; Bogunia-Kubik, K. Polymorphisms within Genes Coding for IL-17A and F and Their Receptor as Clinical Hallmarks in Ankylosing Spondylitis. Mediat. Inflamm. 2021, 2021, 3125922. [Google Scholar] [CrossRef] [PubMed]
- Oliveira-Toré, C.F.; Moraes, A.G.; Martinez, G.F.; Neves, J.S.F.; Macedo, L.C.; Rocha-Loures, M.A.; Quirino, M.G.; Alves, H.V.; Sell, A.M.; Visentainer, J.E.L. Genetic Polymorphisms of Toll-like receptors 2 and 9 as Susceptibility Factors for the Development of Ankylosing Spondylitis and Psoriatic Arthritis. J. Immunol. Res. 2019, 2019, 1492092. [Google Scholar] [CrossRef]
- Wu, J.; Xiong, Z.; Sun, Y.; Song, J.; Niu, F.; Yan, M.; Jin, T. TIMP3 gene polymorphisms and relation to Ankylosing spondylitis susceptibility in Chinese Han population. Int. J. Immunogenet. 2019, 46, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Fu, L.; He, D.; Deng, J.; Zhu, J.; Xu, K.; Hu, D.; Li, J.; Wang, Y.; Hu, W.; et al. RUNX3 Polymorphisms Affect the Risk of Ankylosing Spondylitis. Med. Sci. Monit. 2020, 26, e919528. [Google Scholar] [CrossRef] [PubMed]
- Gao, S.; Liang, W.; Xu, T.; Xun, C.; Cao, R.; Deng, Q.; Zhang, J.; Sheng, W. Associations of Tumor Necrosis Factor Alpha Gene Polymorphisms and Ankylosing Spondylitis Susceptibility: A Meta-analysis Based on 35 Case-control Studies. Immunol. Investig. 2022, 51, 859–882. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Hu, X.; Wu, M.; Ma, Y.; Zhang, X.; Chen, M.; Yuan, Y.; Han, R.; Liu, R.; Guan, S.; et al. TNFAIP3 genetic polymorphisms reduce ankylosing spondylitis risk in Eastern Chinese Han population. Sci. Rep. 2019, 9, 10209. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Result in AS Patients | Reference |
|---|---|---|
| SOD | Increased | [76,78] |
| Decreased | [76,97] | |
| No significant change | [67] | |
| CAT | Increased | [76,78] |
| Decreased | [76,97] | |
| GPx | Increased | [76] |
| Decreased | [76,97] | |
| GST | Decreased | [76] |
| GR | Increased | [98] |
| Decreased | [76] | |
| TAS | Decreased | [45,76,79] |
| TOS | Increased | [45,98] |
| MDA | Increased | [34,67,97,98] |
| AOPP | Increased | [97] |
| CP | Increased | [80,81,82] |
| Factor | Participation in AS | Population | References |
|---|---|---|---|
| Smoking | Decreased physical mobility parameters including modified Schober’s index, cervical rotation, later lumbar flexion, chest expansion, and occiput-to-wall distances. Increased systemic inflammation parameters | Chinese | [157] |
| Exposure of no more than ten pack-years may contribute to a higher prevalence of hip involvement in AS | Chinese | [160] | |
| Increased risk of psoriasis, decreased risk of acute anterior uveitis | United Kingdom | [159] | |
| Smoking is associated with spinal radiographic progression in patients in first 10 years of the disease | German | [7] |
| Polymorphism | Genotype | Influence on AS | Population | References |
|---|---|---|---|---|
| IL-1A-889 (rs1800587) | various | increases the risk of AS in studied populations | English and Tunisian | [251] |
| IL1F7 exon 2 (rs3811047) | G allele | is negatively correlated with susceptibility to AS | Canadian and Chinese | [251] |
| IL5 (rs2069812) | A allele | associated with lower CRP and VAS values | Polish | [252] |
| IL9 (rs2069885) | A allele | associated with lower CRP and VAS values | Polish | [252] |
| IL17F (rs763780) | G allele | should be considered as a promising biomarker of disease activity and anti-TNF treatment outcome | Polish | [253] |
| IL17RA (rs48419554) | G allele | may serve as a potential marker of disease severity in Polish AS patients | Polish | [253] |
| TLR2 (rs5743708) | A allele | haplotypes appear to be involved in the development of clinical forms of SpA and can be a possible therapeutic target for the spondyloarthritis. | Brasil | [254] |
| TLR9 (rs187084_rs5743836) | T/C allele | haplotypes appear to be involved in the development of clinical forms of SpA and can be a possible therapeutic target for the spondyloarthritis. | Brasil | [254] |
| TIMP3 (rs11547635) | may be associated with susceptibility to AS | Chinese | [255] | |
| RUNX3 (rs760805) | T allele | can contribute to AS incidence | Chinese | [256] |
| TNFα (rs1799724) | C vs T allele | reduced risk of AS | Asians | [257] |
| TNFα (rs1800629) | G vs A allele | significantly increased the risk of AS in Caucasians and decreased the risk of AS in mixed populations. | Asians, Caucasian | [257] |
| TNFα (rs361525) | G vs A allele, GG vs GA genotype | linked to an elevated AS susceptibility | Asians | [257] |
| TNFα (rs1800630) | C allele | linked to an elevated AS susceptibility | Asians | [257] |
| TNFAIP3 (rs10499194) | T allele, CT genotype | may be associated with a reduced risk of AS. | Chinese Han | [258] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bilski, R.; Kamiński, P.; Kupczyk, D.; Jeka, S.; Baszyński, J.; Tkaczenko, H.; Kurhaluk, N. Environmental and Genetic Determinants of Ankylosing Spondylitis. Int. J. Mol. Sci. 2024, 25, 7814. https://doi.org/10.3390/ijms25147814
Bilski R, Kamiński P, Kupczyk D, Jeka S, Baszyński J, Tkaczenko H, Kurhaluk N. Environmental and Genetic Determinants of Ankylosing Spondylitis. International Journal of Molecular Sciences. 2024; 25(14):7814. https://doi.org/10.3390/ijms25147814
Chicago/Turabian StyleBilski, Rafał, Piotr Kamiński, Daria Kupczyk, Sławomir Jeka, Jędrzej Baszyński, Halina Tkaczenko, and Natalia Kurhaluk. 2024. "Environmental and Genetic Determinants of Ankylosing Spondylitis" International Journal of Molecular Sciences 25, no. 14: 7814. https://doi.org/10.3390/ijms25147814







