External Apical Root Resorption in Orthodontic Patients Who Practice Combat Sports: A Case-Control Observational Pilot Study
Abstract
:1. Introduction
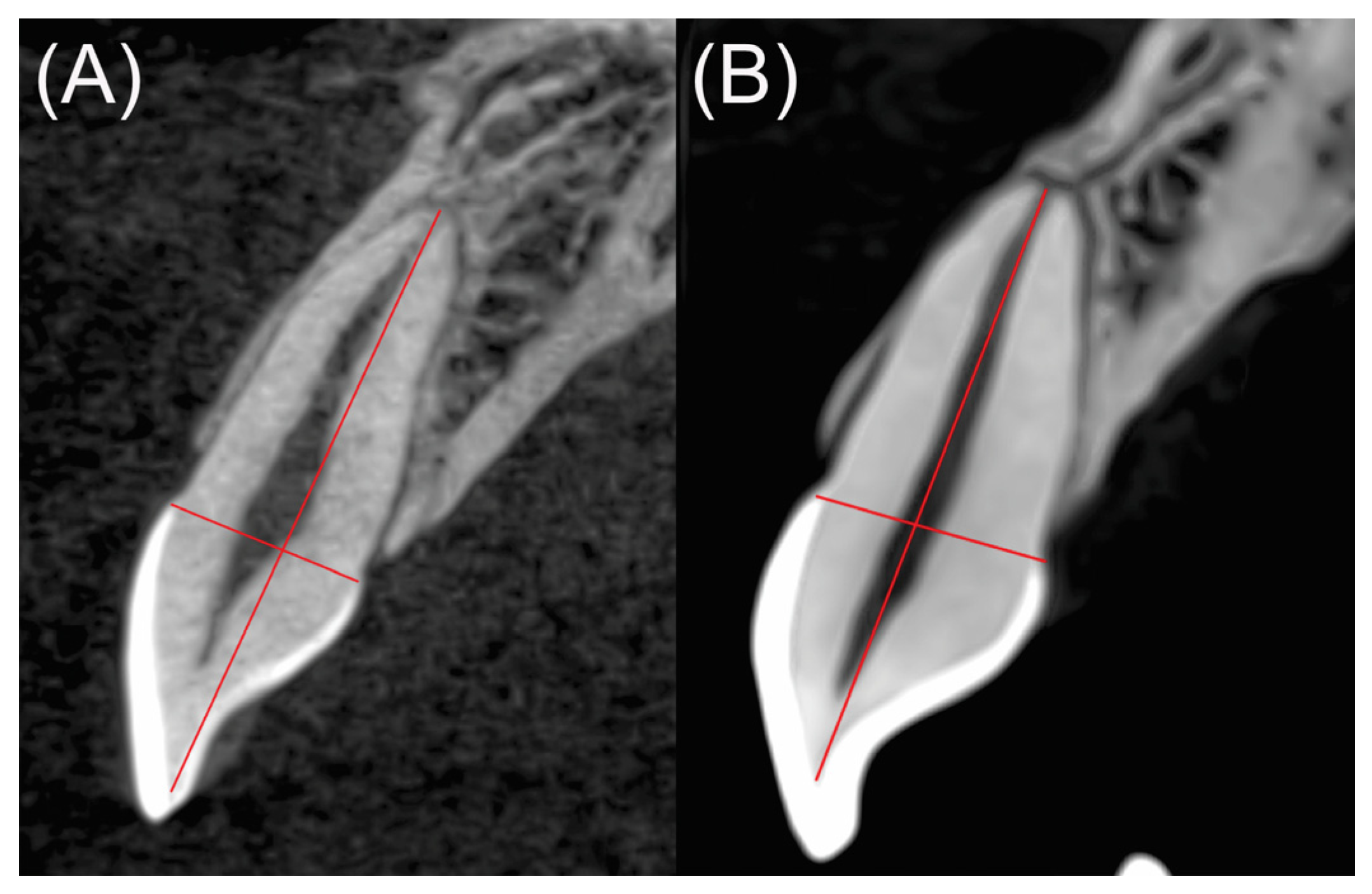
2. Materials and Methods
3. Results
Patients
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Westley, H. Risks and complications in orthodontic treatment. Dent. Nurs. 2010, 6, 318–321. [Google Scholar] [CrossRef]
- Linkous, E.R.; Trojan, T.M.; Harris, E.F. External apical root resorption and vectors of orthodontic tooth movement. Am. J. Orthod. Dentofac. Orthop. 2020, 158, 700–709. [Google Scholar] [CrossRef]
- Mirabella, A.D.; Årtun, J. Risk factors for apical root resorption of maxillary anterior teeth in adult orthodontic patients. Am. J. Orthod. Dentofac. Orthop. 1995, 108, 48–55. [Google Scholar] [CrossRef]
- Bayir, F.; Gumus, E.B. External apical root resorption after orthodontic treatment: Incidence, severity and risk factors. J. Dent. Res. Dent. Clin. Dent. Prospect. 2021, 15, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.Q.P.; Figueiredo, N.C.; Antonucci, C.C.M.; Lages, E.M.B.; Andrade, I., Jr.; Capelli, J., Jr. Predisposing factors for external apical root resorption associated with orthodontic treatment. Korean J. Orthod. 2019, 49, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, A.V.B.; De Molon, R.S.; Nokhbehsaim, M.; Deschner, J.; Cirelli, J.A. Contribution of biomechanical forces to inflammation-induced bone resorption. J. Clin. Periodontol. 2017, 44, 31–41. [Google Scholar] [CrossRef]
- Mota-Rodríguez, A.-N.; Olmedo-Hernández, O.; Argueta-Figueroa, L. A systematic analysis of evidence for surgically accelerated orthodontics. J. Clin. Exp. Dent. 2019, 11, e829–e838. [Google Scholar] [CrossRef] [PubMed]
- Asano, M.; Yamaguchi, M.; Nakajima, R.; Fujita, S.; Utsunomiya, T.; Yamamoto, H.; Kasai, K. IL-8 and MCP-1 induced by excessive orthodontic force mediates odontoclastogenesis in periodontal tissues. Oral Dis. 2010, 17, 489–498. [Google Scholar] [CrossRef]
- Feller, L.; Khammissa, R.A.G.; Thomadakis, G.; Fourie, J.; Lemmer, J. Apical External Root Resorption and Repair in Orthodontic Tooth Movement: Biological Events. BioMed Res. Int. 2016, 2016, 1–7. [Google Scholar] [CrossRef]
- Bender, I.B.; Byers, M.R.; Mori, K. Periapical replacement resorption of permanent, vital, endodontically treated incisors after orthodontic movement: Report of two cases. J. Endod. 1997, 23, 768–773. [Google Scholar] [CrossRef]
- Jung, Y.-H.; Cho, B.-H. External root resorption after orthodontic treatment: A study of contributing factors. Imaging Sci. Dent. 2011, 41, 17–21. [Google Scholar] [CrossRef] [PubMed]
- Kindelan, S.A.; Day, P.F.; Kindelan, J.D.; Spencer, J.R.; Duggal, M.S. Dental trauma: An overview of its influence on the management of orthodontic treatment. Part 1. J. Orthod. 2008, 35, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Preoteasa, C.T.; Ionescu, E.; Preoteasa, E.; Comes, C.A.; Buzea, M.C.; Grămescu, A. Orthodontically induced root resorption correlated with morphological characteristics. Romanian J. Morphol. Embryol. 2009, 50, 257–262. [Google Scholar]
- van Gastel, J.; Quirynen, M.; Teughels, W.; Carels, C. The relationships between malocclusion, fixed orthodontic appliances and periodontal disease. A review of the literature. Aust. Orthod. J. 2007, 23, 121–129. [Google Scholar] [PubMed]
- Mohlin, B.; Axelsson, S.; Paulin, G.; Pietilä, T.; Bondemark, L.; Brattström, V.; Hansen, K.; Holm, A.-K. TMD in Relation to Malocclusion and Orthodontic Treatment: A Systematic Review. Angle Orthod. 2007, 77, 542–548. [Google Scholar] [CrossRef]
- d’Apuzzo, F.; Nucci, L.; Delfino, I.; Portaccio, M.; Minervini, G.; Isola, G.; Serino, I.; Camerlingo, C.; Lepore, M. Application of Vibrational Spectroscopies in the Qualitative Analysis of Gingival Crevicular Fluid and Periodontal Ligament during Orthodontic Tooth Movement. J. Clin. Med. 2021, 10, 1405. [Google Scholar] [CrossRef]
- Cardaropoli, D.; Gaveglio, L. The Influence of Orthodontic Movement on Periodontal Tissues Level. Semin. Orthod. 2007, 13, 234–245. [Google Scholar] [CrossRef]
- Elkordy, S.A.; Palomo, L.; Palomo, J.M.; Mostafa, Y.A. Do fixed orthodontic appliances adversely affect the periodontium? A systematic review of systematic reviews. Semin. Orthod. 2019, 25, 130–157. [Google Scholar] [CrossRef]
- Alzamora, T.S. Factores de riesgo que predisponen a la reabsorción radicular durante el tratamiento ortodóncico. Rev. Esp. Ortod. 2000, 30, 351–363. [Google Scholar]
- Castro-Gutiérrez, M.E.M.; Argueta-Figueroa, L.; Fuentes-Mascorro, G.; Moreno-Rodríguez, A.; Torres-Rosas, R. Novel Approaches for the Treatment of Necrotic Immature Teeth Using Regenerative Endodontic Procedures: A Systematic Review and Meta-Analysis. Appl. Sci. 2021, 11, 5199. [Google Scholar] [CrossRef]
- Ávila-Curiel, B.X.; Gómez-Aguirre, J.N.; Gijón-Soriano, A.L.; Acevedo-Mascarúa, A.E.; Argueta-Figueroa, L.; Torres-Rosas, R. Intervenciones complementarias para el tratamiento de dolor en pacientes con alteraciones temporomandibulares: Una revisión sistemática. Rev. Int. Acupunt. 2020, 14, 151–159. [Google Scholar] [CrossRef]
- Villaman-Santacruz, H.; Torres-Rosas, R.; Acevedo-Mascarua, A.; Argueta-Figueroa, L. Root resorption factors associated with orthodontic treatment with fixed appliances: A systematic review and meta-analysis. Dent. Med. Probl. 2022, in press. [Google Scholar]
- Ioannidou-Marathiotou, I.; Zafeiriadis, A.; Papadopoulos, M.A. Root resorption of endodontically treated teeth following orthodontic treatment: A meta-analysis. Clin. Oral Investig. 2012, 17, 1733–1744. [Google Scholar] [CrossRef] [PubMed]
- Yi, J.; Li, M.; Li, Y.; Li, X.; Zhao, Z. Root resorption during orthodontic treatment with self-ligating or conventional brackets: A systematic review and meta-analysis. BMC Oral Health 2016, 16, 1–8. [Google Scholar] [CrossRef]
- Petti, S.; Glendor, U.; Andersson, L. World traumatic dental injury prevalence and incidence, a meta-analysis-One billion living people have had traumatic dental injuries. Dent. Traumatol. 2018, 34, 71–86. [Google Scholar] [CrossRef]
- Zaleckiene, V.; Peciuliene, V.; Brukiene, V.; Drukteinis, S. Traumatic dental injuries: Etiology, prevalence and possible outcomes. Stomatologija 2014, 16, 7–14. [Google Scholar]
- Soares, A.J.; Souza, G.A.; Pereira, A.C.; Vargas-Neto, J.; Zaia, A.A.; Silva, E.J.N.L. Frequency of root resorption following trauma to permanent teeth. J. Oral Sci. 2015, 57, 73–78. [Google Scholar] [CrossRef]
- Lam, R. Epidemiology and outcomes of traumatic dental injuries: A review of the literature. Aust. Dent. J. 2016, 61, 4–20. [Google Scholar] [CrossRef]
- Polmann, H.; Melo, G.; Réus, J.C.; Domingos, F.L.; de Souza, B.D.M.; Padilha, A.C.; Duque, T.M.; Porporatti, A.L.; Flores-Mir, C.; Canto, G.D.L. Prevalence of dentofacial injuries among combat sports practitioners: A systematic review and meta-analysis. Dent. Traumatol. 2020, 36, 124–140. [Google Scholar] [CrossRef]
- Uzel, I.; Aykut-Yetkiner, A.; Ersin, N.; Ertuğrul, F.; Oncag, O.; Attin, R. Dental Trauma and Mouthguard Usage among Soccer Players in Izmir, Turkey. Dent. J. 2014, 2, 78–84. [Google Scholar] [CrossRef]
- Schoenfeld, D.A. Statistical Considerations for a Parallel Trial where the Outcome is a Measurement MGH Biostatistics Center: Massachusetts General Hospital Mallinckrodt General Clinical Research Center. Available online: http://hedwig.mgh.harvard.edu/sample_size/js/js_parallel_quant.html (accessed on 31 January 2019).
- Mohandesan, H.; Ravanmehr, H.; Valaei, N. A radiographic analysis of external apical root resorption of maxillary incisors during active orthodontic treatment. Eur. J. Orthod. 2007, 29, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, A.L.; Julious, S.A.; Cooper, C.L.; Campbell, M.J. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat. Methods Med Res. 2016, 25, 1057–1073. [Google Scholar] [CrossRef] [PubMed]
- Yuen, K.K. The Two-Sample Trimmed t for Unequal Population Variances. Biometrika 1974, 61, 165–170. [Google Scholar] [CrossRef]
- Nanekrungsan, K.; Patanaporn, V.; Janhom, A.; Korwanich, N. External apical root resorption in maxillary incisors in orthodontic patients: Associated factors and radiographic evaluation. Imaging Sci. Dent. 2012, 42, 147–154. [Google Scholar] [CrossRef] [Green Version]
- Brin, I.; Ben-Bassat, Y.; Heling, I.; Engelberg, A. The influence of orthodontic treatment on previously traumatized permanent incisors. Eur. J. Orthod. 1991, 13, 372–377. [Google Scholar] [CrossRef]
- Andreasen, J.O.; Andreasen, F.M. Root resorption following traumatic dental injuries. Proc. Finn. Dent. Soc. 1992, 88, 95–114. [Google Scholar] [PubMed]
- Huang, H.-M.; Han, C.-S.; Cui, S.-J.; Zhou, Y.-K.; Xin, T.-Y.; Zhang, T.; Zhu, S.-B.; Zhou, Y.-H.; Yang, R.-L. Mechanical force-promoted osteoclastic differentiation via periodontal ligament stem cell exosomal protein ANXA3. Stem Cell Rep. 2022, 17, 1842–1858. [Google Scholar] [CrossRef]
- Paddenberg, E.; Krenmayr, B.; Jantsch, J.; Kirschneck, C.; Proff, P.; Schröder, A. Dietary salt and myeloid NFAT5 (nuclear factor of activated T cells 5) impact on the number of bone-remodelling cells and frequency of root resorption during orthodontic tooth movement. Ann. Anat. Anat. Anz. 2022, 244, 151979. [Google Scholar] [CrossRef]
- Hecova, H.; Tzigkounakis, V.; Merglova, V.; Netolicky, J. A retrospective study of 889 injured permanent teeth. Dent. Traumatol. 2010, 26, 466–475. [Google Scholar] [CrossRef]
- Petti, S.; Andreasen, J.O.; Glendor, U.; Andersson, L. NA0D—The new Traumatic Dental Injury classification of the World Health Organization. Dent. Traumatol. 2022, 38, 170–174. [Google Scholar] [CrossRef]
- Aras, I.; Unal, I.; Huniler, G.; Aras, A. Root resorption due to orthodontic treatment using self-ligating and conventional brackets. J. Orofac. Orthop. 2018, 79, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Haq, A.A.A.; Zhou, Y. Root resorption of self-ligating and conventional preadjusted brackets in severe anterior crowding Class I patients: A longitudinal retrospective study. BMC Oral Health 2015, 15, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Spurrier, S.W.; Hall, S.H.; Joondeph, D.R.; Shapiro, P.A.; Riedel, R.A. A comparison of apical root resorption during orthodontic treatment in endodontically treated and vital teeth. Am. J. Orthod. Dentofac. Orthop. 1990, 97, 130–134. [Google Scholar] [CrossRef]
- Castro, I.; Valladares-Neto, J.; Estrela, C. Contribution of cone beam computed tomography to the detection of apical root resorption after orthodontic treatment in root-filled and vital teeth. Angle Orthod. 2014, 85, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.; Kim, M.J.; Jeong, H.S.; Lee, I.; Lee, S.Y. Mechanisms of Sports Concussion in Taekwondo: A Systematic Video Analysis of Seven Cases. Int. J. Environ. Res. Public Health 2022, 19, 10312. [Google Scholar] [CrossRef]
- Shirani, G.; Motamedi, M.H.K.; Ashuri, A.; Eshkevari, P.S. Prevalence and patterns of combat sport related maxillofacial injuries. J. Emergencies Trauma Shock 2010, 3, 314–317. [Google Scholar]
- Manzo-Toledo, A.; Torres-Rosas, R.; Mendieta-Zerón, H.; Arriaga-Pizano, L.; Argueta-Figueroa, L. Hydroxychloroquine in the treatment of COVID-19 disease: A systematic review and meta-analysis. Med J. Indones. 2021, 30, 20–32. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G.; Cochrane Statistical Methods Group. Analysing data and undertaking meta-analyses. In Cochrane Handbook for Systematic Reviews of Interventions; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2019; pp. 241–284. [Google Scholar]
- Gobernación, S.D. NORMA Oficial Mexicana NOM-012-SSA3–2012, Que Establece los Criterios Para la Ejecución de Proyectos de Investigación Para la Salud en seres Humanos: Diario Oficial De La Federación 2012. Available online: https://dof.gob.mx/nota_detalle.php?codigo=5284148&fecha=04/01/2013#gsc.tab=0 (accessed on 15 December 2019).



| Maxillary teeth | Mandibular teeth | |||
|---|---|---|---|---|
| Control | Exposed | Control | Exposed | |
| Mean | 1.251 | 2.171 | 1.939 | 2.258 |
| SD | 1.100 | 1.827 | 1.653 | 3.120 |
| Minimum | 0.000 | 0.100 | 0.020 | 0.010 |
| Maximum | 4.950 | 8.100 | 7.400 | 17.240 |
| W | p | |||
| Maxillary teeth | 589.000 | 0.004 * | ||
| Mandibular teeth | 938.500 | 0.695 | ||
| Teeth | 11 | 12 | 13 |
| Control (mean ± SD) | 0.84 ± 0.74 | 0.54 ± 0.35 | 2.20 ± 1.47 |
| Exposed (mean ± SD) | 2.10 ± 0.63 | 1.61 ± 1.21 | 2.92 ± 3.22 |
| p-value | 0.004 * | 0.026 * | 0.797 |
| Teeth | 21 | 22 | 23 |
| Control (mean ± SD) | 1.09 ± 0.98 | 1.45 ± 1.28 | 1.36 ± 0.92 |
| Exposed (mean ± SD) | 2.03 ± 1.40 | 2.11 ± 2.25 | 2.23 ± 1.55 |
| p-value | 0.259 | 0.701 | 0.259 |
| Teeth | 31 | 32 | 33 |
| Control (mean ± SD) | 1.18 ± 1.60 | 1.88 ± 1.19 | 3.21 ± 2.85 |
| Exposed (mean ± SD) | 4.36 ± 6.09 | 2.54 ± 3.75 | 1.33 ± 1.59 |
| p-value | 0.097 | 0.383 | 0.128 |
| Teeth | 41 | 42 | 43 |
| Control (mean ± SD) | 1.76 ± 1.13 | 1.83 ± 0.69 | 1.75 ± 1.45 |
| Exposed (mean ± SD) | 1.64 ± 1.22 | 1.98 ± 1.42 | 1.66 ± 1.40 |
| p-value | 0.902 | 0.949 | 0.902 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Acevedo-Mascarúa, A.E.; Torres-Rosas, R.; Pérez-Cervera, Y.; Pérez-Cruz, D.; Ku-Valenzuela, L.Z.; Gijón-Soriano, A.L.; Argueta-Figueroa, L. External Apical Root Resorption in Orthodontic Patients Who Practice Combat Sports: A Case-Control Observational Pilot Study. Medicina 2022, 58, 1342. https://doi.org/10.3390/medicina58101342
Acevedo-Mascarúa AE, Torres-Rosas R, Pérez-Cervera Y, Pérez-Cruz D, Ku-Valenzuela LZ, Gijón-Soriano AL, Argueta-Figueroa L. External Apical Root Resorption in Orthodontic Patients Who Practice Combat Sports: A Case-Control Observational Pilot Study. Medicina. 2022; 58(10):1342. https://doi.org/10.3390/medicina58101342
Chicago/Turabian StyleAcevedo-Mascarúa, Alfonso Enrique, Rafael Torres-Rosas, Yobana Pérez-Cervera, Daniel Pérez-Cruz, Lizbeth Zulema Ku-Valenzuela, Ana Lilia Gijón-Soriano, and Liliana Argueta-Figueroa. 2022. "External Apical Root Resorption in Orthodontic Patients Who Practice Combat Sports: A Case-Control Observational Pilot Study" Medicina 58, no. 10: 1342. https://doi.org/10.3390/medicina58101342







