Viral Infections Confined to Tattoos—A Narrative Review
Abstract
:1. Introduction
2. Brief History of Tattoos
3. Materials and Methods
4. Viral Infections Localized on Tattoos
4.1. Molluscum Contagiosum
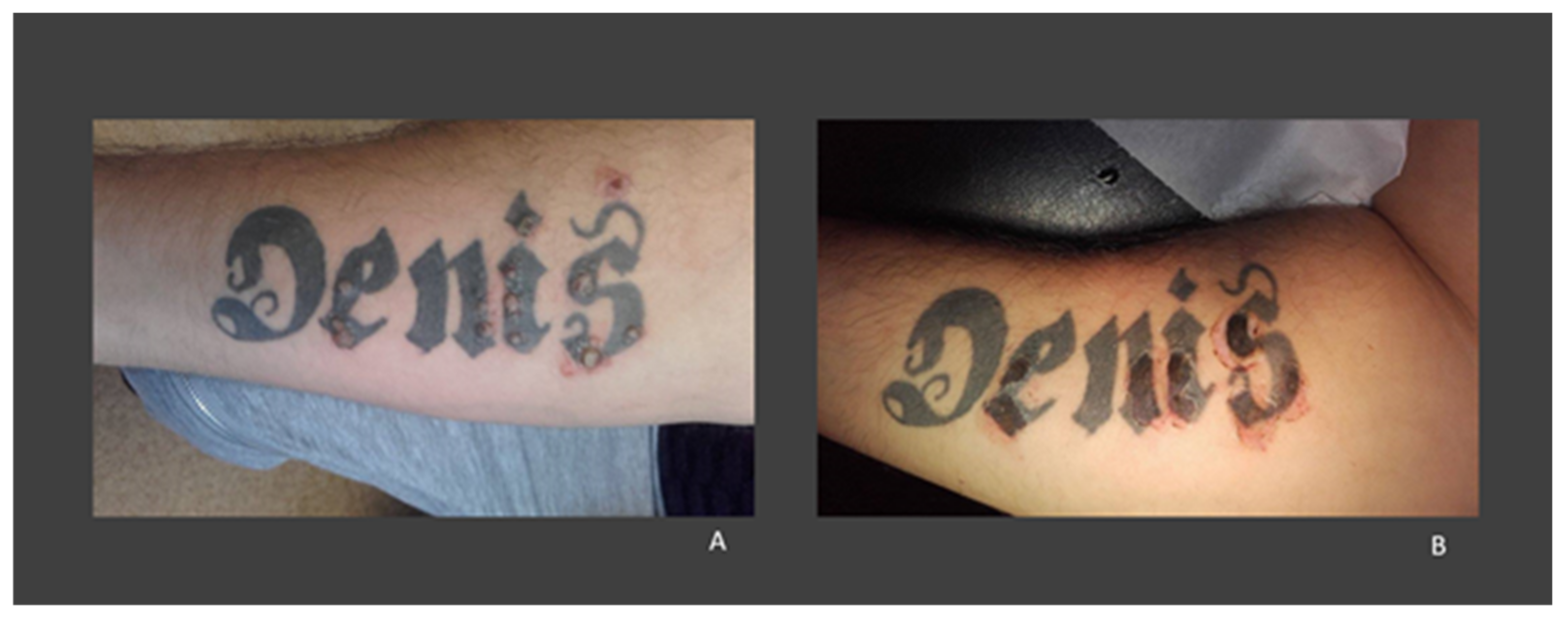
4.2. Warts
4.3. Herpes Simplex
5. Summary of the Characteristics of Viral Infections Confined to Tattoos
6. Potential Mechanisms Involved in the Occurrence of Viral Infections on Tattoos
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Islam, P.S.; Chang, C.; Selmi, C.; Generali, E.; Huntley, A.; Teuber, S.S.; Gershwin, M.E. Medical Complications of Tattoos: A Comprehensive Review. Clin. Rev. Allerg. Immunol. 2016, 50, 273–286. [Google Scholar] [CrossRef] [PubMed]
- Luebberding, S.; Alexiades-Armenakas, M. New Tattoo Approaches in Dermatology. Dermatol. Clin. 2014, 32, 91–96. [Google Scholar] [CrossRef]
- Gualdi, G.; Fabiano, A.; Moro, R.; Venturuzzo, A.; Monari, P.; Calzavara-Pinton, P.; Amerio, P. Tattoo: Ancient Art and Current Problems. J. Cosmet. Dermatol. 2021, 20, 602–604. [Google Scholar] [CrossRef] [PubMed]
- Laux, P.; Tralau, T.; Tentschert, J.; Blume, A.; Dahouk, S.A.; Bäumler, W.; Bernstein, E.; Bocca, B.; Alimonti, A. A Medical-Toxicological View of Tattooing. Lancet 2016, 387, 395–402. [Google Scholar] [CrossRef]
- Byard, R.W. Tattoos: Forensic Considerations. Forensic Sci. Med. Pathol. 2013, 9, 534–542. [Google Scholar] [CrossRef]
- Atkinson, M. Tattooed: The Sociogenesis of a Body Art; University of Toronto Press: Toronto, ON, Canada, 2003. [Google Scholar]
- Farley, C.L.; Van Hoover, C.; Rademeyer, C. Women and Tattoos: Fashion, Meaning, and Implications for Health. J. Midwifery Women’s Health 2019, 64, 154–169. [Google Scholar] [CrossRef]
- Lineberry, C. Tattoos: The Ancient and Mysterious History. 2007. Available online: https://www.smithsonianmag.com/history/tattoos-144038580/ (accessed on 9 May 2021).
- Sanders, C.; Vail, D.A. Customizing the Body: The Art and Culture of Tattooing; Temple University Press: Philadelphia, PA, USA, 2009. [Google Scholar]
- Kosut, M. Tattoos and Body Modification. In Wright (Editor-in-Chief), International Encyclopedia of the Social & Behavioral Sciences, 2nd ed.; James, D., Ed.; Elsevier: Oxford, UK, 2015; Volume 24, pp. 34–35. [Google Scholar]
- Weiß, K.T.; Schreiver, I.; Siewert, K.; Luch, A.; Haslböck, B.; Berneburg, M.; Bäumler, W. Tattoos—More than Just Colored Skin? Searching for Tattoo Allergens. JDDG J. Dtsch. Dermatol. Ges. 2021, 19, 657–669. [Google Scholar] [CrossRef]
- Baranska, A.; Shawket, A.; Jouve, M.; Baratin, M.; Malosse, C.; Voluzan, O.; Vu Manh, T.-P.; Fiore, F.; Bajénoff, M.; Benaroch, P. Unveiling Skin Macrophage Dynamics Explains Both Tattoo Persistence and Strenuous Removal. J. Exp. Med. 2018, 215, 1115–1133. [Google Scholar] [CrossRef] [Green Version]
- Bäumler, W. Chemical Hazard of Tattoo Colorants. La Presse Médicale 2020, 49, 104046. [Google Scholar] [CrossRef]
- Patel, M.; Cobbs, C.G. Infections from Body Piercing and Tattoos. Infect. Leis. 2016, 307–323. [Google Scholar]
- Lane, E.W. An Account of the Manners and Customs of the Modern Egyptians; American University in Cairo Press: Cairo, Egypt, 2014. [Google Scholar]
- DeMello, M. Encyclopedia of Body Adornment; Greenwood Press: Westport, CT, USA, 2007. [Google Scholar]
- Deter-Wolf, A.; Robitaille, B.; Krutak, L.; Galliot, S. The World’s Oldest Tattoos. J. Archaeol. Sci. Rep. 2016, 5, 19–24. [Google Scholar] [CrossRef]
- Paszik, J. AE Ink: Investigating the Mechanics and Meanings of Ancient Egyptian Tattoos. Master’s Thesis, University College London, London, UK, 2017. [Google Scholar] [CrossRef]
- Gell, A. Wrapping in Images: Tattooing in Polynesia; Oxford University Press: New York, NY, USA, 1993. [Google Scholar]
- DeMello, M.; Rubin, G.S. Bodies of Inscription; Duke University Press: Durham, NC, USA, 2000. [Google Scholar]
- Lodder, M. Too Many Cooks. The origins of Western Tattooing: Exploding a Popular Myth. Total Tattoo Magazine, 23 September 2015; 70–71. [Google Scholar]
- Kosut, M. The Artification of Tattoo: Transformations within a Cultural Field. Cult. Sociol. 2013, 8, 2–8. [Google Scholar] [CrossRef]
- Unwin, P. ‘An Extremely Useful Invention’: Edison’s Electric Pen and the Unravelling of Old and New Media. Convergence 2019, 25, 607–626. [Google Scholar] [CrossRef]
- Barker, F. Notes of Cases on an Outbreak of Syphilis Following on Tattooing. Br. Med. J. 1889, 1, 985–989. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Steward, S.M. Bad Boys and Tough Tattoos: A Social History of the Tattoo with Gangs, Sailors, and Street-Corner Punks 1950–1965; Routledge: London, UK, 2013. [Google Scholar]
- Rubin, A. The Tattoo Renaissance; Museum of Cultural History; University of California: Los Angeles, CA, USA, 1988. [Google Scholar]
- Ralf, M. Manufacturing of Tattoo Ink Products Today and in Future: Europe. In Tattooed Skin and Health; Serup, J., Kluger, N., Bäumler, W., Eds.; Karger: Basel, Switzerland, 2015; Volume 48, pp. 197–199. [Google Scholar]
- Bonadonna, L. Survey of Studies on Microbial Contamination of Marketed Tattoo Inks. In Current Problems in Dermatology; Serup, J., Kluger, N., Baumler, W., Eds.; S. Karger AG: Basel, Switzerland, 2015; Volume 48, pp. 190–195. [Google Scholar] [CrossRef]
- Hodder, I. The Meanings of Things: Material Culture and Symbolic Expression; Routledge: London, UK, 2013. [Google Scholar]
- Petrochko, J.M.; Krakowski, A.C.; Donnelly, C.; Wilson, J.B.; Irick, J.B.; Stawicki, S.P. Tattoo-associated complications and related topics: A comprehensive review. Int. J. Acad. Med. 2019, 5, 19. [Google Scholar]
- Juhas, E.; English, J.C. Tattoo-Associated Complications. J. Pediatric Adolesc. Gynecol. 2013, 26, 125–129. [Google Scholar] [CrossRef]
- Serup, J.; Hutton Carlsen, K.; Sepehri, M. Tattoo Complaints and Complications: Diagnosis and Clinical Spectrum. In Current Problems in Dermatology; Serup, J., Kluger, N., Baumler, W., Eds.; S. Karger AG: Basel, Switzerland, 2015; Volume 48, pp. 48–60. [Google Scholar] [CrossRef]
- Kluger, N. An Update on Cutaneous Complications of Permanent Tattooing. Expert Rev. Clin. Immunol. 2019, 15, 1135–1143. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R. Tattoo-Associated Viral Infections: A Review. Clin. Cosmet. Investig. Dermatol. 2021, 14, 1529. [Google Scholar] [CrossRef]
- Meza-Romero, R.; Navarrete-Dechent, C.; Downey, C. Molluscum Contagiosum: An Update and Review of New Perspectives in Etiology, Diagnosis, and Treatment. CCID 2019, 12, 373–381. [Google Scholar] [CrossRef] [Green Version]
- Robinson, G.; Townsend, S.; Jahnke, M.N. Molluscum Contagiosum: Review and Update on Clinical Presentation, Diagnosis, Risk, Prevention, and Treatment. Curr. Dermatol. Rep. 2020, 9, 83–92. [Google Scholar] [CrossRef]
- Leung, A.K.C.; Barankin, B.; Hon, K.L.E. Molluscum Contagiosum: An Update. IAD 2017, 11, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Anstey, A.V.; Bugert, J.J. Molluscum Contagiosum Virus Infection. Lancet Infect. Dis. 2013, 13, 877–888. [Google Scholar] [CrossRef]
- Ruby, K.N.; Perry, A.E.; Linos, K. Expanding the Morphologic Heterogeneity of Stromal Changes in Molluscum Contagiosum Infection. Am. J. Dermatopathol. 2018, 40, 941–943. [Google Scholar] [CrossRef] [PubMed]
- Foulds, I.S. Molluscum Contagiosum: An Unusual Complication of Tattooing. BMJ 1982, 285, 607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salmaso, F.; Gnecchi, L.; Gianotti, R.; Veraldi, S. Molluscum Contagiosum on a Tattoo. Acta Derm.-Venereol. 2001, 81, 146–147. [Google Scholar] [PubMed] [Green Version]
- Perez Gala, S.; Alonso Perez, A.; Rios Buceta, L.; Aragues Montanes, M.; Garcia Diez, A. Molluscum Contagiosum on a Multicoloured Tattoo. J. Eur. Acad. Dermatol. Venerol. 2006, 20, 221–222. [Google Scholar] [CrossRef] [PubMed]
- Kluger, N.; Comte, C.; Guillot, B. Molluscum contagiosum sur tatouage. Ann. Dermatol. Vénéréol. 2007, 134, 506–507. [Google Scholar] [CrossRef]
- Panasiti, V.; Devirgiliis, V.; Roberti, V.; Curzio, M.; Calvieri, S. Molluscum Contagiosum on a Tattoo: Usefulness of Dermoscopy. Int. J. Dermatol. 2008, 47, 1318–1319. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Barrio, S.; González-Hermosa, M.R.; Ratón, J.A.; Díaz-Pérez, J.L. Molusco contagioso sobre tatuaje. Actas Dermo-Sifiliográficas 2009, 100, 152–154. [Google Scholar] [CrossRef]
- De Giorgi, V.; Grazzini, M.; Lotti, T. A Three-Dimensional Tattoo: Molluscum Contagiosum. Can. Med. Assoc. J. 2010, 182, E382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Molina, L.; Romiti, R. Molusco Contagioso Em Tatuagem. An. Bras. Dermatol. 2011, 86, 352–354. [Google Scholar] [CrossRef] [Green Version]
- Grillo, E.; Urech, M.; Vano-Galvan, S.; Pedro, J. Lesions on Tattooed Skin: A Case Study. Aust. Fam. Physician 2012, 41, 308–309. [Google Scholar] [PubMed]
- Tampa, M.; Sarbu, I.; Neamtu, V.; Anghel, A.; Mihele, D.; Benea, V.; Georgescu, S. O complicatie rara a tatuarii: Infectia cutanata cu virusul molluscum contagiosum. Rev. Med. Mod. 2012, 19, 129–132. [Google Scholar]
- Ruiz-Villaverde, R.; Sánchez-Cano, D. Pearled Papules over Tattoo: Molluscum Cotagiosum. Pan Afr. Med. J. 2013, 16. [Google Scholar] [CrossRef] [PubMed]
- Blasco-Morente, G.; Naranjo-Díaz, M.J.; Pérez-López, I.; Martínez-López, A.; Garrido-Colmenero, C. Molluscum Contagiosum Over Tattooed Skin. SQUMJ 2016, 16, e257–e258. [Google Scholar] [CrossRef] [PubMed]
- Cortés, V.O.; Alcudia, A.A.G.; Díaz, N.P. Molusco contagioso sobre tatuaje: Reporte de caso. Dermatol. CMQ 2018, 16, 28–31. [Google Scholar]
- Marcelino, F.F.N.; de Oliveira-Filho, J.; Junqueira, G.M.D.; Nogueira, M.F.; Michalany, A.O. Molusco Contagioso Como Complicação de Tatuagem: Um Relato de Caso e Revisão Da Literatura. Surg. Cosmet. Dermatol. 2021, 13, e20210008. [Google Scholar] [CrossRef]
- Bergh, R. Über Eigentümliche Geschwulstbildung in Einer Tätowierungsmarke. Mschr. Dermat. 1903, 37, 49–52. [Google Scholar]
- Tampa, M.; Mitran, C.I.; Mitran, M.I.; Nicolae, I.; Dumitru, A.; Matei, C.; Manolescu, L.; Popa, G.L.; Caruntu, C.; Georgescu, S.R. The Role of Beta HPV Types and HPV-Associated Inflammatory Processes in Cutaneous Squamous Cell Carcinoma. J. Immunol. Res. 2020, 2020, 5701639. [Google Scholar] [CrossRef]
- Egawa, N.; Doorbar, J. The Low-Risk Papillomaviruses. Virus Res. 2017, 231, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Okunade, K.S. Human Papillomavirus and Cervical Cancer. J. Obstet. Gynaecol. 2020, 40, 602–608. [Google Scholar] [CrossRef] [PubMed]
- Georgescu, S.R.; Mitran, C.I.; Mitran, M.I.; Caruntu, C.; Sarbu, M.I.; Matei, C.; Nicolae, I.; Tocut, S.M.; Popa, M.I.; Tampa, M. New Insights in the Pathogenesis of HPV Infection and the Associated Carcinogenic Processes: The Role of Chronic Inflammation and Oxidative Stress. J. Immunol. Res. 2018, 2018, 5315816. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lynch, M.D.; Cliffe, J.; Morris-Jones, R. Management of Cutaneous Viral Warts. BMJ 2014, 348, g3339. [Google Scholar] [CrossRef] [Green Version]
- McLaughlin, J.S.; Shafritz, A.B. Cutaneous Warts. J. Hand Surg. 2011, 36, 343–344. [Google Scholar] [CrossRef] [PubMed]
- Fox, T. Warts Occurring on Tattooed Lines. J. Cutan. Vener. Dis. 1884, 2, 216. [Google Scholar]
- Watkins, D.B. Viral Disease in Tattoos: Verruca Vulgaris. Arch. Dermatol. 1961, 84, 306–309. [Google Scholar] [CrossRef]
- Young, D.F.; Cole, G.W. The Verrucous Mermaid. Int. J. Dermatol. 1979, 18, 816–817. [Google Scholar] [CrossRef]
- Baxter, S.; Deck, D. Tattoo-Acquired Verruca Plana. Am. Fam. Physician 1993, 47, 732. [Google Scholar]
- Patrick Ragland, H.; Hubbell, C.; Stewart, K.R.; Nesbitt, L.T. Verruca vulgaris inoculated during tattoo placement. Int. J. Dermatol. 1994, 33, 796–797. [Google Scholar] [CrossRef]
- Miller, D.M.; Brodell, R.T. Verruca Restricted to the Areas of Black Dye within a Tattoo. Arch. Dermatol. 1994, 130, 1453–1454. [Google Scholar] [CrossRef]
- Trefzer, U.; Schmollack, K.-P.; Stockfleth, E.; Sterry, W.; Kolde, G. Verrucae in a Multicolored Decorative Tattoo. J. Am. Acad. Dermatol. 2004, 50, 478–479. [Google Scholar] [CrossRef]
- Brajac, I.; Loncarek, K.; Stojnic-Sosa, L.; Gruber, F. Delayed Onset of Warts over Tattoo Mark Provoked by Sunburn. J. Eur. Acad. Dermatol. Venerol. 2005, 19, 247–248. [Google Scholar] [CrossRef] [PubMed]
- Saez, M.; Rodriguez-Martin, M.; Sidro-Sarto, M.; Cabrera de Paz, R.; Rodriguez-Garcia, F.; Fagundo-Gonzalez, E.; Carnerero, A.; Guimera, F.; Garcia-Bustinduy, M.; Sanchez, R.; et al. Multiple Verrucae Vulgaris in a Young Woman’s Tattoo. J. Eur. Acad. Dermatol. Venerol. 2006, 20, 356–357. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.Y.; Shin, H.S.; Won, C.H.; Cho, S. Facial Verruca Plana That Developed after Semipermanent Tattooing. Ann. Dermatol. 2009, 21, 92. [Google Scholar] [CrossRef] [Green Version]
- Wanat, K.A.; Tyring, S.; Rady, P.; Kovarik, C.L. Human Papillomavirus Type 27 Associated with Multiple Verruca within a Tattoo: Report of a Case and Review of the Literature: HPV27 Associated with Multiple Verruca in a Tattoo. Int. J. Dermatol. 2014, 53, 882–884. [Google Scholar] [CrossRef]
- Navarro-Vidal, B.; González-Olivares, M.; Aguado-Lobo, M.; Borbujo Martinez, J.M. Vulgaris Verruca on a Tattoo. Med. Clín. Engl. Ed. 2015, 145, e35. [Google Scholar] [CrossRef]
- Fania, L.; Sordi, D.; Pagnanelli, G.; CavanI, A.; Mazzanti, C. Tattoo and Warts: Efficacy of Topical Immunotherapy. Eur. J. Dermatol. 2017, 27, 322–323. [Google Scholar] [CrossRef]
- Krecké, N.; Smola, S.; Vogt, T.; Müller, C.S.L. HPV-47-Induced and Tattoo-Associated Verrucae Planae: Report of a Case and Review of the Literature. Dermatol. Ther. 2017, 7, 549–554. [Google Scholar] [CrossRef] [Green Version]
- Nemer, K.M.; Hurst, E.A. Confluent Verruca Vulgaris Arising within Bilateral Eyebrow Tattoos: Successful Treatment with Ablative Laser and Topical 5% Imiquimod Cream. Dermatol. Surg. 2019, 45, 473–475. [Google Scholar] [CrossRef]
- Georgescu, S.R.; Musa, E.; Limbau, A.; Benea, V.; Tampa, M. A rare complication of tattooing: Verruca restricted to the black pigment in a tattoo. In Proceedings of the 14th EADV Spring Symposium, Brussels, Belgium, 25–28 May 2017. [Google Scholar]
- Kirchhof, M.G.; Wong, S.M. Tattoos and Human Papilloma Virus: A Case Report of Tattoo-Associated Flat Warts (Verrucae Planae). SAGE Open Med. Case Rep. 2019, 7, 2050313X1985741. [Google Scholar] [CrossRef]
- Yuan, T. Multiple Verrucae Vulgaris in a Young Man’s Tattoo: A Case Report. Int. J. Dermatol. Venereol. 2019, 2, 120–121. [Google Scholar] [CrossRef]
- Chen, Y.J.; Nabi, O.; Diao, P.; Wan, R.Y.; Li, L. Verruca Plana on a Tattoo: A Case Report. Medicine 2020, 99, e19744. [Google Scholar] [CrossRef] [PubMed]
- Veasey, J.V.; Erthal, A.L.N.; Lellis, R.F. In Vivo and Ex Vivo Dermoscopy of Lesions from Implantation of Human Papillomavirus in Tattoos: Report of Two Cases. An. Bras. Dermatol. 2020, 95, 78–81. [Google Scholar] [CrossRef] [PubMed]
- Cohen, P.R. Verruca Vulgaris Occurring on a Tattoo: Case Report and Review of Tattoo-Associated Human Papillomavirus Infections. Cureus 2021, 13, e17575. [Google Scholar] [CrossRef] [PubMed]
- Kluger, N. Viral Warts and Seborrhoeic Keratoses on Tattoos: A Review of Nine Cases. J. Eur. Acad. Dermatol. Venereol. 2017, 31, e340–e342. [Google Scholar] [CrossRef]
- Ramey, K.; Ibrahim, J.; Brodell, R.T. Verruca Localization Predominately in Black Tattoo Ink: A Retrospective Case Series. J. Eur. Acad. Dermatol. Venereol. 2016, 30, e34–e36. [Google Scholar] [CrossRef]
- Widener, R.W.; Whitley, R.J. Herpes Simplex Virus. In Handbook of Clinical Neurology; Elsevier: Amsterdam, The Netherlands, 2014; Volume 123, pp. 251–263. [Google Scholar] [CrossRef]
- Whitley, R.; Baines, J. Clinical Management of Herpes Simplex Virus Infections: Past, Present, and Future. F1000Research 2018, 7, 1726. [Google Scholar] [CrossRef] [Green Version]
- Singh, N.; Tscharke, D.C. Herpes Simplex Virus Latency Is Noisier the Closer We Look. J. Virol. 2020, 94, e01701-19. [Google Scholar] [CrossRef] [Green Version]
- Nath, P.; Kabir, M.A.; Doust, S.K.; Ray, A. Diagnosis of Herpes Simplex Virus: Laboratory and Point-of-Care Techniques. Infect. Dis. Rep. 2021, 13, 518–539. [Google Scholar] [CrossRef]
- Marshall, C.S.; Murphy, F.; McCarthy, S.E.; Cheng, A.C. Herpes Compunctorum: Cutaneous Herpes Simplex Virus Infection Complicating Tattooing. Med. J. Aust. 2007, 187, 598. [Google Scholar] [CrossRef]
- Kluger, N.; Armingaud, P. Herpes Simplex Infection on a Recent Tattoo. A New Case of “Herpes Compuctorum”. Int. J. Dermatol. 2017, 56, e9–e10. [Google Scholar] [CrossRef] [PubMed]
- AlQuorain, N.A.; Yousef, H.A.; AlJabre, S.H.; AlAkloby, O.M.; Al-Natour, S.H. Cosmetic Lip Tattoo Sequelae: A Case Report and Review of Literature. J. Dermatol. Dermatol. Surg. 2017, 21, 87–90. [Google Scholar] [CrossRef]
- Begolli Gerqari, A.; Ferizi, M.; Kotori, M.; Halimi, S.; Daka, A.; Hapciu, S.; Begolli, I.; Begolli, M.; Gerqari, I. Activation of Herpes Simplex Infection after Tattoo. Acta Dermatovenerol. Croat. 2018, 26, 75. [Google Scholar] [PubMed]
- De Cuyper, C.; Maria Luisa Pérez-Cotapos, S. Dermatologic Complications with Body Art; Springer: Berlin/Heidelberg, Germany, 2010. [Google Scholar]
- Gülseren, D.; Tan, Ç.; Yaz, İ.; Özbek, B.; Çağdaş, D.; Tezcan, İ. Expression of HLA Class I and Class II Genes in Patients with Multiple Skin Warts. Exp. Dermatol. 2021, 30, 1642–1649. [Google Scholar] [CrossRef]
- Ruocco, V.; Brunetti, G.; Puca, R.; Ruocco, E. The Immunocompromised District: A Unifying Concept for Lymphoedematous, Herpes-Infected and Otherwise Damaged Sites. J. Eur. Acad. Dermatol. Venereol. 2009, 23, 1364–1373. [Google Scholar] [CrossRef] [PubMed]
- Karakass, M.; Durdu, M.; Özbilen, A. Molluscum Contagiosum on Region of Burned Skin: Wolf” s Isotopic Response. J. Eur. Acad. Dermatol. Venereol. 2006, 20, 1014–1016. [Google Scholar] [CrossRef] [PubMed]
- Hasson, A.; Requena, L.; Arias, D.; Martin, L.; De Castro, A. Linear Pemphigus Vulgaris along a Surgical Scar. Dermatology 1991, 182, 191–192. [Google Scholar] [CrossRef]
- Hendricks, W.M. Basal Cell Carcinoma Arising in a Chickenpox Scar. Arch. Dermatol. 1980, 116, 1304–1305. [Google Scholar] [CrossRef]
- Mizukawa, Y.; Shiohara, T. Trauma-Localized Fixed Drug Eruption: Involvement of Burn Scars, Insect Bites and Venipuncture Sites. Dermatology 2002, 205, 159–161. [Google Scholar] [CrossRef]
- Huynh, T.N.; Jackson, J.D.; Brodell, R.T. Tattoo and Vaccination Sites: Possible Nest for Opportunistic Infections, Tumors, and Dysimmune Reactions. Clin. Dermatol. 2014, 32, 678–684. [Google Scholar] [CrossRef]
- Lehner, K.; Santarelli, F.; Vasold, R.; König, B.; Landthaler, M.; Bäumler, W. Black Tattoo Inks Are a Source of Problematic Substances Such as Dibutyl Phthalate. Contact Dermat. 2011, 65, 231–238. [Google Scholar] [CrossRef] [PubMed]
- Lehner, K.; Santarelli, F.; Vasold, R.; Penning, R.; Sidoroff, A.; König, B.; Landthaler, M.; Bäumler, W. Black tattoos entail substantial uptake of genotoxicpolycyclic aromatic hydrocarbons (PAH) in human skin and regional lymph nodes. PLoS ONE 2014, 9, e92787. [Google Scholar] [CrossRef] [PubMed]
- Georgescu, S.R.; Ene, C.D.; Tampa, M.; Matei, C.; Benea, V.; Nicolae, I. Oxidative Stress-Related Markers and Alopecia Areata through Latex Turbidimetric Immunoassay Method. Mater. Plast. 2016, 53, 522–526. [Google Scholar]
- Jacobsen, N.R.; Clausen, P.A. Carbon Black Nanoparticles and Other Problematic Constituents of Black Ink and Their Potential to Harm Tattooed Humans. Curr. Probl. Dermatol. 2015, 48, 170–175. [Google Scholar] [PubMed]
- El-Beltagi, H.S.; Mohamed, H.I. Reactive Oxygen Species, Lipid Peroxidation and Antioxidative Defense Mechanism. Not. Bot. Horti Agrobot. Cluj-Napoca 2013, 41, 44–57. [Google Scholar] [CrossRef] [Green Version]
- Mitran, C.I.; Nicolae, I.; Tampa, M.; Mitran, M.I.; Caruntu, C.; Sarbu, M.I.; Ene, C.D.; Matei, C.; Ionescu, A.C.; Georgescu, S.R.; et al. The Relationship between the Soluble Receptor for Advanced Glycation End Products and Oxidative Stress in Patients with Palmoplantar Warts. Medicina 2019, 55, 706. [Google Scholar] [CrossRef] [Green Version]
- Stone, V.; Johnston, H.; Clift, M.J. Air Pollution, Ultrafine and Nanoparticle Toxicology: Cellular and Molecular Interactions. IEEE Trans. Nanobiosci. 2007, 6, 331–340. [Google Scholar] [CrossRef]
- Regensburger, J.; Lehner, K.; Maisch, T.; Vasold, R.; Santarelli, F.; Engel, E.; Gollmer, A.; König, B.; Landthaler, M.; Bäumler, W. Tattoo Inks Contain Polycyclic Aromatic Hydrocarbons That Additionally Generate Deleterious Singlet Oxygen: PAHs in Tattoo Inks. Exp. Dermatol. 2009, 19, e275–e281. [Google Scholar] [CrossRef]
- Christensen, L.; Suggs, A.; Baron, E. Ultraviolet Photobiology in Dermatology. Adv. Exp. Med. Biol. 2017, 996, 89–104. [Google Scholar] [CrossRef]
- Nicolae, I.; Ene, C.D.; Georgescu, S.R.; Tampa, M.; Matei, C.; Ceausu, E. Effects of UV Radiation and Oxidative DNA Adduct 8-Hydroxy-2′-deoxiguanosine on the Skin Diseases. Rev. Chim. 2014, 65, 1036–1041. [Google Scholar]
- Akgul, B.; Lemme, W.; Garcia-Escudero, R.; Storey, A.; Pfister, H.J. UV-B Irradiation Stimulates the Promoter Activity of the High-Risk, Cutaneous Human Papillomavirus 5 and 8 in Primary Keratinocytes. Arch. Virol. 2005, 150, 145–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rho, N. Activation of Flat Warts (Verrucae Planae) on the Q-Switched Laser-Assisted Tattoo Removal Site. Med. Lasers 2014, 3, 84–86. [Google Scholar] [CrossRef] [Green Version]
- Amella, C.A.; Lofgren, L.A.; Ronn, A.M.; Nouri, M.; Shikowitz, M.J.; Steinberg, B.M. Latent Infection Induced with Cottontail Rabbit Papillomavirus. A Model for Human Papillomavirus Latency. Am. J. Pathol. 1994, 144, 1167–1171. [Google Scholar] [PubMed]

| Sex | Age (Years) | Tattoo Localisation | Ink Colour | Latency Period | Reference |
|---|---|---|---|---|---|
| male | 20 | left arm | polychrome- carbon pigment * | 3 months | Foulds (1982) [40] |
| female | 20 | left forearm | black | 3 weeks | Salmaso et al. (2001) [41] |
| male | 20 | left calf | polychrome-brownish-grey ink * | 5 months | Perez Gala et al. (2006) [42] |
| male | 59 | chest | monochromatic | 3 months | Kluger et al. (2007) [43] |
| male | 24 | right lumbar region | black | 2 weeks | Panasiti et al. (2008) [44] |
| male | 36 | right arm | black | 3 weeks | Perez-Barrio et al. (2009) [45] |
| male | 30 | arm | black | 20 days | De Giorgi et al. (2010) [46] |
| male | 22 | back | black | 4 weeks | Molina et al. (2011) [47] |
| male | 33 | right upper arm | polychrome | 5 months | Grillo et al. (2012) [48] |
| male | 32 | left abdominal flank | black | 3 weeks | Tampa et al. (2012) [49] |
| male | 23 | right abdominal flank | black | N/A | Ruiz-Villaverde et al. (2013) [50] |
| male | 33 | right arm | black | 3 months | Blasco Morente et al. (2016) [51] |
| female | 16 | posterior thorax | blue | N/A | Cortes et al. (2017) [52] |
| female | 64 | right eyebrow | dark | 1 month | Marcelino et al. (2021) [53] |
| Sex | Age (Years) | Tattoo Localisation | Ink Colour | Latency Period | Reference |
|---|---|---|---|---|---|
| male | 21 | left arm | black | soon after tattooing | Watkins (1961) [62] |
| male | 24 | left scapula | black | 2 years | Young et al. (1979) [63] |
| male | 21 | N/A | black | 6 months | Baxter et al. (1993) [64] |
| male | 27 | right scapular area | dark blue | 8 years | Ragland et al. (1994) [65] |
| male | 33 | right upper arm | black | 8 years | Miller et al. (1994) [66] |
| male | 29 | left arm | polychrome-dark blue * | 8 years | Trefzer et al. (2004) [67] |
| male | 32 | back (left scapular area) after sunburn | dark blue | 2.5 years | Brajac et al. (2005) [68] |
| female | 17 | left leg | dark blue and red-dark blue * | 3 months | Saez et al. (2006) [69] |
| female | 39 | face | dark | 1 year | Jung et al. (2009) [70] |
| female | 31 | right ankle | polychrome | 2 years | Wanat et al. (2014) [71] |
| male | 25 | the back of the left hand | polychrome | N/A | Navarro-Vidal et al. (2015) [72] |
| male | 24 | right arm | polychrome-dark, red * | 4.5 years | Fania et al. (2017) [73] |
| male | 35 | left arm | polychrome-dark * | 3.6 years | Fania et al. (2017) [73] |
| male | 47 | forearm | black | 12 years | Krecke et al. (2017) [74] |
| female | 66 | both eyebrows | dark grey/black | 8 years | Nemer et al. (2018) [75] |
| male | 30 | left forearm | black | 3 months | Georgescu et al. (2017) [76] |
| male | 36 | right forearm | black | more than 20 years | Kirchhof et al. (2019) [77] |
| male | 25 | right upper arm | dark blue | 3 months | Yuan (2019) [78] |
| female | 27 | left leg | black | 2 years | Chen et al. (2020) [79] |
| male | 39 | left calf | polychrome | 1 year | Veasey et al. (2020) [80] |
| male | 33 | left upper limb | polychrome | 6 years | Veasey et al. (2020) [80] |
| female | 44 | left lower leg | polychrome-black *, red | 26 years | Cohen(2021) [81] |
| Sex | Age (Years) | Tattoo Localisation | Ink Colour | Latency Period | Reference |
|---|---|---|---|---|---|
| male | 30 | left arm | black | 3 days | Marshall et al. (2007) [88] |
| female | 31 | right flank | black | 3 days | Kluger et al. (2017) [89] |
| female | 48 | lips | red | 2 days | AlQuorain et al. (2017) [90] |
| female | 46 | lips | red | 2 days | Begolli Gerqari et al. (2018) [91] |
| Parameter | Molluscum Contagiosum | Warts | Herpes Simplex |
|---|---|---|---|
| Age (mean ± SD) | 30.85 ± 14.38 years | 32.04 ± 10.7 years | 38.75 ± 9.56 years |
| Male:Female ratio | 3.6:1 | 2.6:1 | 0.3:1 |
| Latency period (mean ± SD) | 2.04 ± 1.69 months | 5.93 ± 6.77 years | 2.5 ± 0.56 days |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tampa, M.; Mitran, M.I.; Mitran, C.I.; Matei, C.; Amuzescu, A.; Buzatu, A.A.; Georgescu, S.R. Viral Infections Confined to Tattoos—A Narrative Review. Medicina 2022, 58, 342. https://doi.org/10.3390/medicina58030342
Tampa M, Mitran MI, Mitran CI, Matei C, Amuzescu A, Buzatu AA, Georgescu SR. Viral Infections Confined to Tattoos—A Narrative Review. Medicina. 2022; 58(3):342. https://doi.org/10.3390/medicina58030342
Chicago/Turabian StyleTampa, Mircea, Madalina Irina Mitran, Cristina Iulia Mitran, Clara Matei, Andreea Amuzescu, Alina Andreea Buzatu, and Simona Roxana Georgescu. 2022. "Viral Infections Confined to Tattoos—A Narrative Review" Medicina 58, no. 3: 342. https://doi.org/10.3390/medicina58030342
APA StyleTampa, M., Mitran, M. I., Mitran, C. I., Matei, C., Amuzescu, A., Buzatu, A. A., & Georgescu, S. R. (2022). Viral Infections Confined to Tattoos—A Narrative Review. Medicina, 58(3), 342. https://doi.org/10.3390/medicina58030342








