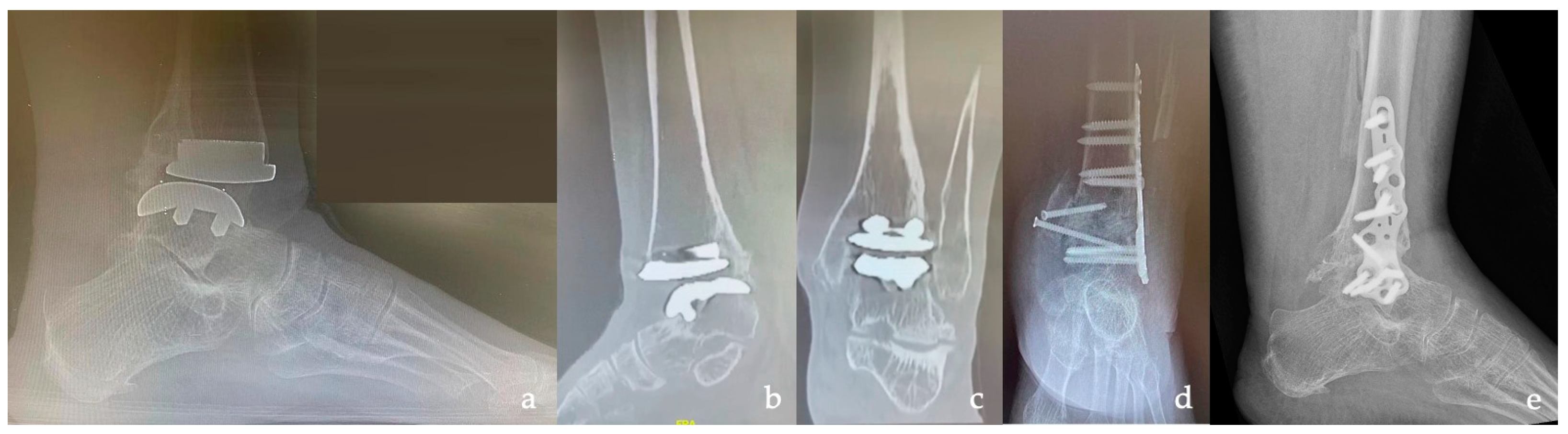
Tibiotalar and Tibiotalocalcaneal Arthrodesis with Paragon28 SilverbackTM Plating System in Patients with Severe Ankle and Hindfoot Deformity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Patients
2.2. Pre-Operative Management
- -
- Anterior distal tibial angle (ADTA), formed by the mechanical axis of the tibia and the TT joint orientation line in the sagittal plane (normal value: 80° ± 3°) [41];
- -
- Tibiotalar angle (TTA), defined by the tibial and talar articular surfaces in the TT joint (if it measures >10°, the joint is defined as incongruent) [41];
- -
- Coronal (or frontal) tibiotalar angle (CTTA), the superomedial angle between the longitudinal axis of the tibia, created by connecting two points in the middle of the proximal and the distal tibial shaft and the axis of the talus, defined by a line drawn through the talar shoulders in the anteroom-posterior view (normal value: 88.7° ± 5.1°) [42];
- -
- Hindfoot alignment angle (HAA), formed by the intersection of the longitudinal axis of the tibial shaft and the axis of the calcaneal tuberosity (normal value: 5.6° ± 5.4°) [43].
2.3. Surgical Technique
2.4. Post-Operative Management
2.5. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barg, A.; Pagenstert, G.I.; Hügle, T.; Gloyer, M.; Wiewiorski, M.; Henninger, H.B.; Valderrabano, V. Ankle osteoarthritis: Etiology, diagnostics, and classification. Foot Ankle Clin. 2013, 18, 411–426. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, C.L.; Zimmerman, M.B.; O’Rourke, M.; Brown, T.D.; Buckwalter, J.A.; Johnston, R. Impact of comorbidities on the measurement of health in patients with ankle osteoarthritis. J. Bone Jt. Surg. Am. 2006, 88, 2366–2372. [Google Scholar] [CrossRef] [PubMed]
- Albert, E. Einige Falle kunstlicher Ankylosen: Bildung an paralytischen Gliedmassen. Wien. Med. Presse 1882, 23, 726–728. [Google Scholar]
- Zhang, C.; Shi, Z.; Mei, G. Locking plate versus retrograde intramedullary nail fixation for tibiotalocalcaneal arthrodesis A retrospective analysis. Indian J. Orthop. 2015, 49, 227–232. [Google Scholar] [CrossRef]
- Heck, B.A.; Schenk, U.; Benali, Y.; Stahl, J.P. Early Results of a Posterolateral Polyaxial Angle-Stable Plate for Tibiotalocalcaneal Arthrodesis. J. Foot Ankle Surg. 2015, 54, 428–432. [Google Scholar] [CrossRef]
- DeHeer, P.A.; Catoire, S.M.; Taulman, J.; Borer, B. Ankle Arthrodesis. A Literature Review. Clin. Podiatr. Med. Surg. 2012, 29, 509–527. [Google Scholar] [CrossRef]
- Cianni, L.; Bocchi, M.B.; Vitiello, R.; Greco, T.; De Marco, D.; Masci, G.; Maccauro, G.; Pitocco, D.; Perisano, C. Arthrodesis in the charcot foot: A systematic review. Orthop. Rev. 2020, 12, 64–68. [Google Scholar] [CrossRef]
- Lachman, J.R.; Adams, S.B. Tibiotalocalcaneal Arthrodesis for Severe Talar Avascular Necrosis. Foot Ankle Clin. 2019, 24, 143–161. [Google Scholar] [CrossRef]
- Greco, T.; Polichetti, C.; Cannella, A.; La Vergata, V.; Maccauro, G.; Perisano, C. Ankle hemophilic arthropathy: Literature review. Am. J. Blood Res. 2021, 11, 206–216. [Google Scholar] [PubMed]
- Greco, T.; Fulchignoni, C.; Cianni, L.; Maccauro, G.; Perisano, C. Surgical management of tibial metastases: A systematic review. Acta Biomed. 2022, 92, e2021552. [Google Scholar] [CrossRef] [PubMed]
- Kusnezov, N.; Dunn, J.C.; Koehler, L.R.; Orr, J.D. Anatomically Contoured Anterior Plating for Isolated Tibiotalar Arthrodesis: A Systematic Review. Foot Ankle Spec. 2017, 10, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Caravelli, S.; Ambrosino, G.; Vocale, E.; Di Ponte, M.; Puccetti, G.; Perisano, C.; Greco, T.; Rinaldi, V.G.; Marcheggiani Muccioli, G.M.; Zaffagnini, S.; et al. Custom-Made Implants in Ankle Bone Loss: A Retrospective Assessment of Reconstruction/Arthrodesis in Sequelae of Septic Non-Union of the Tibial Pilon. Medicina 2022, 58, 1641. [Google Scholar] [CrossRef] [PubMed]
- Guo, C.; Yan, Z.; Barfield, W.R.; Hartsock, L.A. Ankle arthrodesis using anatomically contoured anterior plate. Foot Ankle Int. 2010, 31, 492–498. [Google Scholar] [CrossRef]
- Asomugha, E.U.; Den Hartog, B.D.; Junko, J.T.; Alexander, I.J. Tibiotalocalcaneal Fusion for Severe Deformity and Bone Loss. J. Am. Acad. Orthop. Surg. 2016, 24, 125–134. [Google Scholar] [CrossRef]
- Park, J.J.; Son, W.S.; Woo, I.H.; Park, C.H. Combined transfibular and anterior approaches increase union rate and decrease non-weight-bearing periods in ankle arthrodesis: Combined approaches in ankle arthrodesis. J. Clin. Med. 2021, 10, 5915. [Google Scholar] [CrossRef]
- Kim, J.-G.; Ha, D.-J.; Gwak, H.-C.; Kim, C.-W.; Kim, J.-H.; Lee, S.-J.; Kim, Y.-J.; Lee, C.-R.; Park, J.-H. Ankle Arthrodesis: A Comparison of Anterior Approach and Transfibular Approach. Clin. Orthop. Surg. 2018, 10, 368–373. [Google Scholar] [CrossRef]
- van den Heuvel, S.B.M.; Doorgakant, A.; Birnie, M.F.N.; Blundell, C.M.; Schepers, T. Open Ankle Arthrodesis: A Systematic Review of Approaches and Fixation Methods. Foot Ankle Surg. 2021, 27, 339–347. [Google Scholar] [CrossRef]
- Yasui, Y.; Hannon, C.P.; Seow, D.; Kennedy, J.G. Ankle arthrodesis: A systematic approach and review of the literature. World J. Orthop. 2016, 7, 700–708. [Google Scholar] [CrossRef]
- Vilày Rico, J.; Rodriguez-Martin, J.; Parra-Sanchez, G.; Marti Lopez-Amor, C. Arthroscopic tibiotalocalcaneal arthrodesis with locked retrograde compression nail. J. Foot Ankle Surg. 2013, 52, 523–528. [Google Scholar] [CrossRef]
- Ogilvie-Harris, D.J.; Fitsialos, D.; Hedman, T.P. Arthrodesis of the ankle. A comparison of two versus three screw fixation in a crossed configuration. Clin. Orthop. Relat. Res. 1994, 304, 195–199. [Google Scholar] [CrossRef]
- Prissel, M.A.; Simpson, G.A.; Sutphen, S.A.; Hyer, C.F.; Berlet, G.C. Ankle Arthrodesis: A Retrospective Analysis Comparing Single Column, Locked Anterior Plating to Crossed Lag Screw Technique. J. Foot Ankle Surg. 2017, 56, 453–456. [Google Scholar] [CrossRef]
- Im, J.; Jung, H.-G.; Lim, J.-W.; Song, W.T. Ankle-Hindfoot Reconstruction by Tibiotalocalcaneal (TTC) Arthrodesis Using Multiple Cannulated Screws: 32 Cases. Foot Ankle Orthop. 2022, 7, 2473011421S0025. [Google Scholar] [CrossRef]
- Tarkin, I.S.; Mormino, M.A.; Clare, M.P.; Haider, H.; Walling, A.K.; Sanders, R.W. Anterior plate supplementation increases ankle arthrodesis construct rigidity. Foot Ankle Int. 2007, 28, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.M.; Douleh, D.G.; Thomson, A.B. Comparison of Ankle Fusion Rates with and without Anterior Plate Augmentation. Foot Ankle Int. 2017, 38, 419–423. [Google Scholar] [CrossRef]
- Woods, J.B.; Lowery, N.J.; Burns, P.R. Permanent antibiotic impregnated intramedullary nail in diabetic limb salvage: A case report and literature review. Diabet. Foot Ankle 2012, 3, 11908. [Google Scholar] [CrossRef] [PubMed]
- Moeckel, B.H.; Patterson, B.M.; Inglis, A.E.; Sculco, T.P. Ankle arthrodesis. A comparison of internal and external fixation. Clin. Orthop. Relat. Res. 1991, 268, 78–83. [Google Scholar]
- Thordarson, D.B.; Markolf, K.L.; Cracchiolo, A. 3rd External fixation in arthrodesis of the ankle. A biomechanical study comparing a unilateral frame with a modified transfixion frame. J. Bone Joint Surg. Am. 1994, 76, 1541–1544. [Google Scholar] [CrossRef]
- Chou, L.B.; Mann, R.A.; Yaszay, B.; Graves, S.C.; McPeake, W.T.; Dreeben, S.M.; Horton, G.A.; Katcherian, D.A.; Clanton, T.O.; Miller, R.A.; et al. Tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2000, 21, 804–808. [Google Scholar] [CrossRef]
- Ahmad, J.; Pour, A.E.; Raikin, S.M. The modified use of a proximal humeral locking plate for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 2007, 28, 977–983. [Google Scholar] [CrossRef] [PubMed]
- Urquhart, M.W.; Mont, M.A.; Michelson, J.D.; Krackow, K.A.; Hungerford, D.S. Osteonecrosis of the talus: Treatment by hindfoot fusion. Foot Ankle Int. 1996, 17, 275–282. [Google Scholar] [CrossRef]
- Haddad, S.L.; Coetzee, J.C.; Estok, R.; Fahrbach, K.; Banel, D.; Nalysnyk, L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J. Bone Jt. Surg. Am. 2007, 89, 1899–1905. [Google Scholar] [CrossRef]
- Horwitz, T. The use of transfibular approach in arthrodesis of the ankle joint. Am. J. Surg. 1942, 60, 550–552. [Google Scholar] [CrossRef]
- Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth. 2019, 13, S31–S34. [Google Scholar] [CrossRef]
- Silverback™ TT/TTC Plating System. Available online: https://paragon28.com/products/silverback-ankle-fusion-plating-system/ (accessed on 1 January 2020).
- Castro, M.D. Ankle biomechanics. Foot Ankle Clin. 2002, 7, 679–693. [Google Scholar] [CrossRef] [PubMed]
- Paul-Dauphin, A.; Guillemin, F.; Virion, J.-M.; Briançon, S. Bias and Precision in Visual Analogue Scales: A Randomized Controlled Trial. Am. J. Epidemiol. 1999, 150, 1117–1127. [Google Scholar] [CrossRef] [PubMed]
- Kitaoka, H.B.; Alexander, I.J.; Adelaar, R.S.; Nunley, J.A.; Myerson, M.S.; Sanders, M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994, 15, 349–353. [Google Scholar] [CrossRef]
- Budiman-Mak, E.; Conrad, K.J.; Roach, K.E. The Foot Function Index: A measure of foot pain and disability. J. Clin. Epidemiol. 1991, 44, 561–570. [Google Scholar] [CrossRef]
- Ware, J.E.J.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Takakura, Y.; Tanaka, Y.; Kumai, T.; Tamai, S. Low tibial osteotomy for osteoarthritis of the ankle. Results of a new operation in 18 patients. J. Bone Jt. Surg. Br. 1995, 77, 50–54. [Google Scholar] [CrossRef]
- Bonasia, D.E.; Dettoni, F.; Femino, J.E.; Phisitkul, P.; Germano, M.; Amendola, A. Total ankle replacement: Why, when and how? Iowa Orthop. J. 2010, 30, 119–130. [Google Scholar] [PubMed]
- Willegger, M.; Holinka, J.; Nemecek, E.; Bock, P.; Wanivenhaus, A.H.; Windhager, R.; Schuh, R. Reliability of the radiographic sagittal and frontal tibiotalar alignment after ankle arthrodesis. PLoS ONE 2016, 11, e0154224. [Google Scholar] [CrossRef] [PubMed]
- Polichetti, C.; Borruto, M.I.; Lauriero, F.; Caravelli, S.; Mosca, M.; Maccauro, G.; Greco, T.; Perisano, C. Adult Acquired Flatfoot Deformity: A Narrative Review about Imaging Findings. Diagnostics 2023, 13, 225. [Google Scholar] [CrossRef] [PubMed]
- Cody, E.A.; Williamson, E.R.; Burket, J.C.; Deland, J.T.; Ellis, S.J. Correlation of Talar Anatomy and Subtalar Joint Alignment on Weightbearing Computed Tomography with Radiographic Flatfoot Parameters. Foot Ankle Int. 2016, 37, 874–881. [Google Scholar] [CrossRef] [PubMed]
- Akra, G.A.; Middleton, A.; Adedapo, A.O.; Port, A.; Finn, P. Outcome of ankle arthrodesis using a transfibular approach. J. Foot Ankle Surg. 2010, 49, 508–512. [Google Scholar] [CrossRef]
- Steginsky, B.D.; Suhling, M.L.; Vora, A.M. Ankle Arthrodesis with Anterior Plate Fixation in Patients at High Risk for Nonunion. Foot Ankle Spec. 2020, 13, 211–218. [Google Scholar] [CrossRef]
- Gharehdaghi, M.; Rahimi, H.; Mousavian, A. Anterior ankle arthrodesis with molded plate: Technique and outcomes. Arch. Bone Jt. Surg. 2014, 2, 203–209. [Google Scholar]
- Slater, G.L.; Sayres, S.C.; O’Malley, M.J. Anterior ankle arthrodesis. World J. Orthop. 2014, 5, 1–5. [Google Scholar] [CrossRef]
- Colman, A.B.; Pomeroy, G.C. Transfibular ankle arthrodesis with rigid internal fixation: An assessment of outcome. Foot Ankle Int. 2007, 28, 303–307. [Google Scholar] [CrossRef]
- Mohamedean, A.; Said, H.G.; El-Sharkawi, M.; El-Adly, W.; Said, G.Z. Technique and short-term results of ankle arthrodesis using anterior plating. Int. Orthop. 2010, 34, 833–837. [Google Scholar] [CrossRef]
- Townshend, D.; Di Silvestro, M.; Krause, F.; Penner, M.; Younger, A.; Glazebrook, M.; Wing, K. Arthroscopic versus open ankle arthrodesis: A multicenter comparative case series. J. Bone Jt. Surg. Am. 2013, 95, 98–102. [Google Scholar] [CrossRef]
- Loewy, E.M.; Goodson, K.M.; Huang, K.; Perkins, A.; Walling, A.K. 2021 Roger A. Mann Award Winner: Long-Term Revision Rates and Functional Outcomes of Total Ankle Arthroplasty and Ankle Arthrodesis. Foot Ankle Orthop. 2022, 7, 2473011421S00044. [Google Scholar] [CrossRef]
- Usuelli, F.G.; Maccario, C.; Granata, F.; Indino, C.; Vakhshori, V.; Tan, E.W. Clinical and Radiological Outcomes of Transfibular Total Ankle Arthroplasty. Foot Ankle Int. 2019, 40, 24–33. [Google Scholar] [CrossRef] [PubMed]


| Patients | 20 | |
| Sex (M-F) | 13-7 | |
| Age (Mean, Range) | 60.0 (40–74) years old | |
| Causes of OA/Deformities | Post-traumatic | 11 (55%) |
| Primary | 4 (20%) | |
| CNO | 2 (10%) | |
| Talus AVN | 2 (10%) | |
| TAR aseptic loosening | 1 (5%) | |
| Side (Left-Right) | 9–11 | |
| Takakura Classification * | Grade 1 | 0 (0%) |
| Grade 2 | 2 (10%) | |
| Grade 3a | 4 (21%) | |
| Grade 3b | 4 (21%) | |
| Grade 4 | 9 (48%) | |
| TT pre-op ROM (Mean, Range) | 43° (27–65) | |
| Type of Plate | Anterior TT | 10 (50%) |
| Anterior TTC | 6 (30%) | |
| Lateral TT | 3 (15%) | |
| Lateral TTC | 1 (5%) | |
| Surgical Time (Mean, Range) | 101.8 (78–121) min | |
| Follow-Up (Mean, Range) | 21 (18–29) months | |
| Bone Union | (20/20) 100% | ||
| Time of union (mean, range) | 14 (12—48) weeks | ||
| Complications | One delayed consolidationOne wound dehiscence | ||
| Pre-op | Post-op * | p-value | |
| VAS | 7.9 ± 1.4 (5–10) | 2.2 ± 1.1 (1–4) | 0.002 § |
| AOFAS | 23.2 ± 11.9 (7–44) | 68.6 ± 8.9 (50–78) | 0.002 § |
| FFI | 70 ± 13 (54–88) | 29 ± 14 (15–50) | 0.002 § |
| SF-36 | 29.2 ± 3 (23–33) | 51.9 ± 6.2 (42–60) | 0.002 § |
| ADTA | 83.0° ± 12.0° (71–102) † | 77.8° ± 4.8° (65–82) ‡ | - |
| TTA | 23° ± 9.0° (17–38) † | 8 ± 2 (5–12) ‡ | - |
| CTTA | 97.5° ± 7° (90–108) † | 89.3° ± 2° (87–92) ‡ | - |
| HAA | 20° ± 5° (14–29) † | 9° ± 5° (5–13) ‡ | - |
| VAS Post-Op | AOFAS Post-Op | FFI Post-Op | SF-36 Post-Op | |
|---|---|---|---|---|
| VAS post-op | 1 | |||
| AOFAS post-op | −0.47 * | 1 | ||
| FFI post-op | 0.31 | −0.80 * | 1 | |
| SF-36 post-op | −0.49 * | 0.25 | 0.13 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Perisano, C.; Cannella, A.; Polichetti, C.; Mascio, A.; Comisi, C.; De Santis, V.; Caravelli, S.; Mosca, M.; Spedicato, G.A.; Maccauro, G.; et al. Tibiotalar and Tibiotalocalcaneal Arthrodesis with Paragon28 SilverbackTM Plating System in Patients with Severe Ankle and Hindfoot Deformity. Medicina 2023, 59, 344. https://doi.org/10.3390/medicina59020344
Perisano C, Cannella A, Polichetti C, Mascio A, Comisi C, De Santis V, Caravelli S, Mosca M, Spedicato GA, Maccauro G, et al. Tibiotalar and Tibiotalocalcaneal Arthrodesis with Paragon28 SilverbackTM Plating System in Patients with Severe Ankle and Hindfoot Deformity. Medicina. 2023; 59(2):344. https://doi.org/10.3390/medicina59020344
Chicago/Turabian StylePerisano, Carlo, Adriano Cannella, Chiara Polichetti, Antonio Mascio, Chiara Comisi, Vincenzo De Santis, Silvio Caravelli, Massimiliano Mosca, Giorgio Alfredo Spedicato, Giulio Maccauro, and et al. 2023. "Tibiotalar and Tibiotalocalcaneal Arthrodesis with Paragon28 SilverbackTM Plating System in Patients with Severe Ankle and Hindfoot Deformity" Medicina 59, no. 2: 344. https://doi.org/10.3390/medicina59020344








