Successful Implant Placement via Simultaneous Nasal Floor Augmentation in an Inferior Meatus Pneumatization Case
Abstract
:1. Introduction
2. Case Descriptions
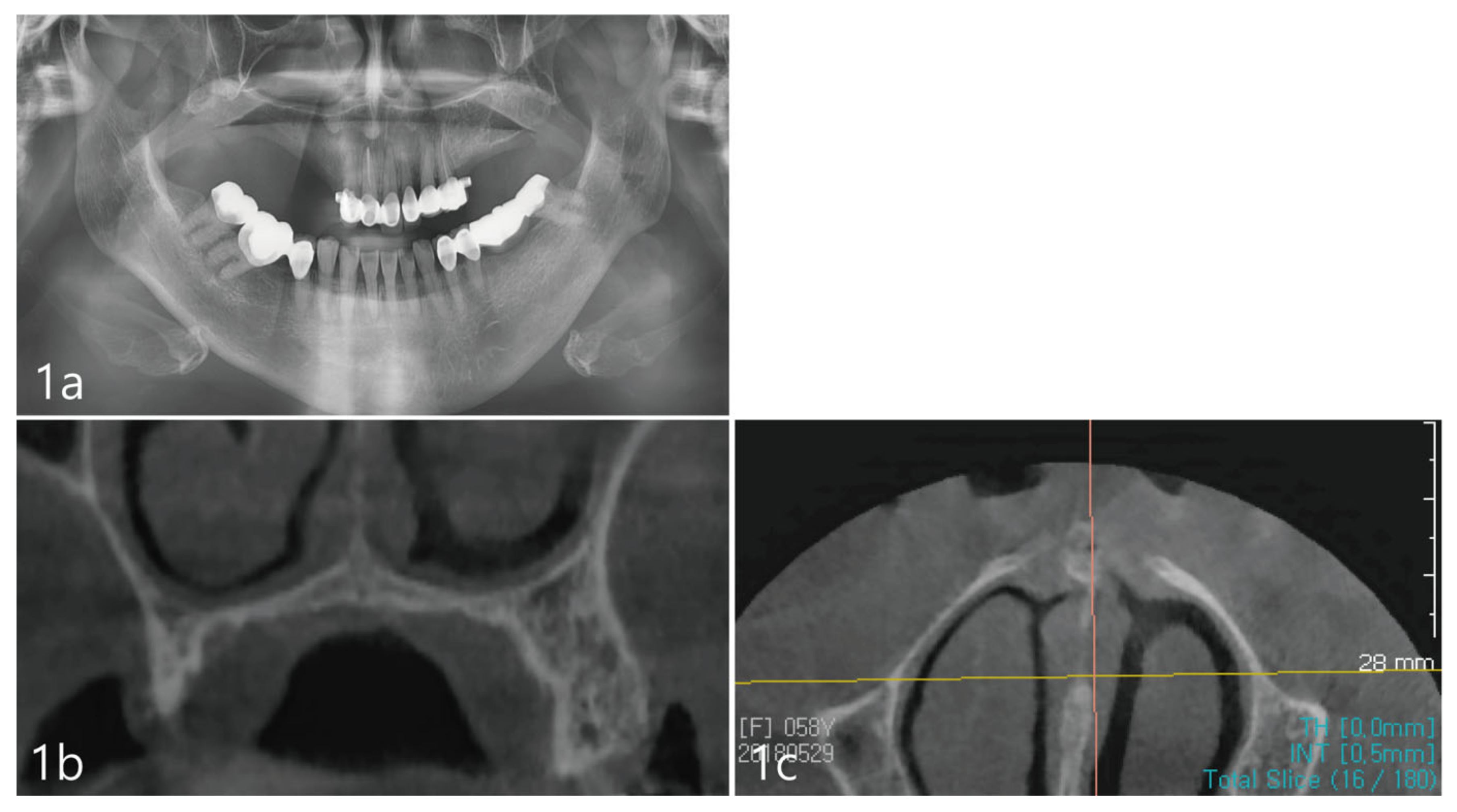
2.1. Patient Information
2.2. Procedure for Surgical Technique and Post-Operative Management
2.3. Radiographic Evaluation and Prosthetic Rehabilitation
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CBCT | Cone Beam Computed Tomography |
| H&E | Hematoxylin and Eosin |
References
- Greenstein, G.; Cavallaro, J.; Tarnow, D. Practical Application of Anatomy for the Dental Implant Surgeon. J. Periodontol. 2008, 79, 1833–1846. [Google Scholar] [CrossRef]
- Wallace, S.S.; Froum, S.J. Effect of Maxillary Sinus Augmentation on the Survival of Endosseous Dental Implants. A Systematic Review. Ann. Periodontol. 2003, 8, 328–343. [Google Scholar] [CrossRef]
- Scuderi, A.J.; Harnsberger, H.R.; Boyer, R.S. Pneumatization of the paranasal sinuses: Normal features of importance to the accurate interpretation of CT scans and MR images. Am. J. Roentgenol. 1993, 160, 1101–1104. [Google Scholar] [CrossRef]
- Park, W.; Kim, Y.; Kang, K.L.; Lim, H.; Han, J. Long-term outcomes of the implants accidentally protruding into nasal cavity extended to posterior maxilla due to inferior meatus pneumatization. Clin. Implant. Dent. Relat. Res. 2020, 22, 105–111. [Google Scholar] [CrossRef]
- Misch, C.E.; Resnik, R.; Misch-Dietsh, F. Maxillary sinus anatomy, pathology and graft surgery. Contemp. Implant. Dent. 2008, 3, 956. [Google Scholar]
- Brånemark, P.I.; Adell, R.; Albrektsson, T.; Lekholm, U.; Lindström, J.; Rockler, B. An experimental and clinical study of osseointegrated implants penetrating the nasal cavity and maxillary sinus. J. Oral Maxillofac. Surg. 1984, 42, 497–505. [Google Scholar] [CrossRef]
- Tatum, H. Maxillary and Sinus Implant Reconstructions. Dent. Clin. N. Am. 1986, 30, 207–229. [Google Scholar] [CrossRef]
- Summers, R.B. The osteotome technique: Part 3—Less invasive methods of elevating the sinus floor. Compendium 1994, 15, 698–700. [Google Scholar]
- Browaeys, H.; Bouvry, P.; De Bruyn, H. A Literature Review on Biomaterials in Sinus Augmentation Procedures. Clin. Implant. Dent. Relat. Res. 2007, 9, 166–177. [Google Scholar] [CrossRef]
- Shulman, L.B.; Jensen, O.T. Sinus Graft Consensus Conference. Introduction. Int. J. Oral Maxillofac. Implant. 1998, 13, 5–6. [Google Scholar]
- Mazor, Z.; Lorean, A.; Mijiritsky, E.; Levin, L. Nasal Floor Elevation Combined with Dental Implant Placement. Clin. Implant. Dent. Relat. Res. 2012, 14, 768–771. [Google Scholar] [CrossRef]
- El-Ghareeb, M.; Pi-Anfruns, J.; Khosousi, M.; Aghaloo, T.; Moy, P. Nasal Floor Augmentation for the Reconstruction of the Atrophic Maxilla: A Case Series. J. Oral Maxillofac. Surg. 2012, 70, e235–e241. [Google Scholar] [CrossRef]
- Van Den Bergh, J.P.A.; Ten Bruggenkate, C.M.; Disch, F.J.M.; Tuinzing, D.B. Anatomical aspects of sinus floor elevations. Clin. Oral Implant. Res. 2000, 11, 256–265. [Google Scholar] [CrossRef]
- Cho, Y.-D.; Namgung, D.-J.; Kim, K.-H.; Kim, S.; Seol, Y.-J.; Lee, Y.-M.; Ku, Y. Long-Term Human Histologic Evaluation of Sinus Bone Augmentation and Simultaneous Implant Placement. Int. J. Periodontics Restor. Dent. 2022, 42, 93–100. [Google Scholar] [CrossRef]
- Lee, J.-S.; Cha, J.-K.; Thoma, D.S.; Jung, U.-W. Report of a human autopsy case in maxillary sinuses augmented using a synthetic bone substitute: Micro-computed tomographic and histologic observations. Clin. Oral Implant. Res. 2018, 29, 339–345. [Google Scholar] [CrossRef]
- Wertz, R.A. Changes in nasal airflow incident to rapid maxillary expansion. Angle Orthod. 1968, 38, 1–11. [Google Scholar] [CrossRef]
- Hartgerink, D.V.; Vig, P.S.; Orth, D.; Abbott, D.W. The effect of rapid maxillary expansion on nasal airway resistance. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 381–389. [Google Scholar] [CrossRef]
- Cordaro, L.; Bosshardt, D.D.; Palattella, P.; Rao, W.; Serino, G.; Chiapasco, M. Maxillary sinus grafting with Bio-Oss or Straumann Bone Ceramic: Histomorphometric results from a randomized controlled multicenter clinical trial. Clin. Oral Implant. Res. 2008, 19, 796–803. [Google Scholar] [CrossRef]
- Tosta, M.; Cortes, A.R.G.; Corrêa, L.; Pinto, D.D.S., Jr.; Tumenas, I.; Katchburian, E. Histologic and histomorphometric evaluation of a synthetic bone substitute for maxillary sinus grafting in humans. Clin. Oral Implant. Res. 2013, 24, 866–870. [Google Scholar] [CrossRef]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, W.-B.; Crasto, G.J.; Park, W.; Han, J.-Y.; Kang, P. Successful Implant Placement via Simultaneous Nasal Floor Augmentation in an Inferior Meatus Pneumatization Case. Medicina 2023, 59, 357. https://doi.org/10.3390/medicina59020357
Park W-B, Crasto GJ, Park W, Han J-Y, Kang P. Successful Implant Placement via Simultaneous Nasal Floor Augmentation in an Inferior Meatus Pneumatization Case. Medicina. 2023; 59(2):357. https://doi.org/10.3390/medicina59020357
Chicago/Turabian StylePark, Won-Bae, Gazelle Jean Crasto, Wonhee Park, Ji-Young Han, and Philip Kang. 2023. "Successful Implant Placement via Simultaneous Nasal Floor Augmentation in an Inferior Meatus Pneumatization Case" Medicina 59, no. 2: 357. https://doi.org/10.3390/medicina59020357
APA StylePark, W.-B., Crasto, G. J., Park, W., Han, J.-Y., & Kang, P. (2023). Successful Implant Placement via Simultaneous Nasal Floor Augmentation in an Inferior Meatus Pneumatization Case. Medicina, 59(2), 357. https://doi.org/10.3390/medicina59020357





