Anterior Approach to Hip Arthroplasty with Early Mobilization Key for Reduced Hospital Length of Stay
Abstract
:1. Introduction
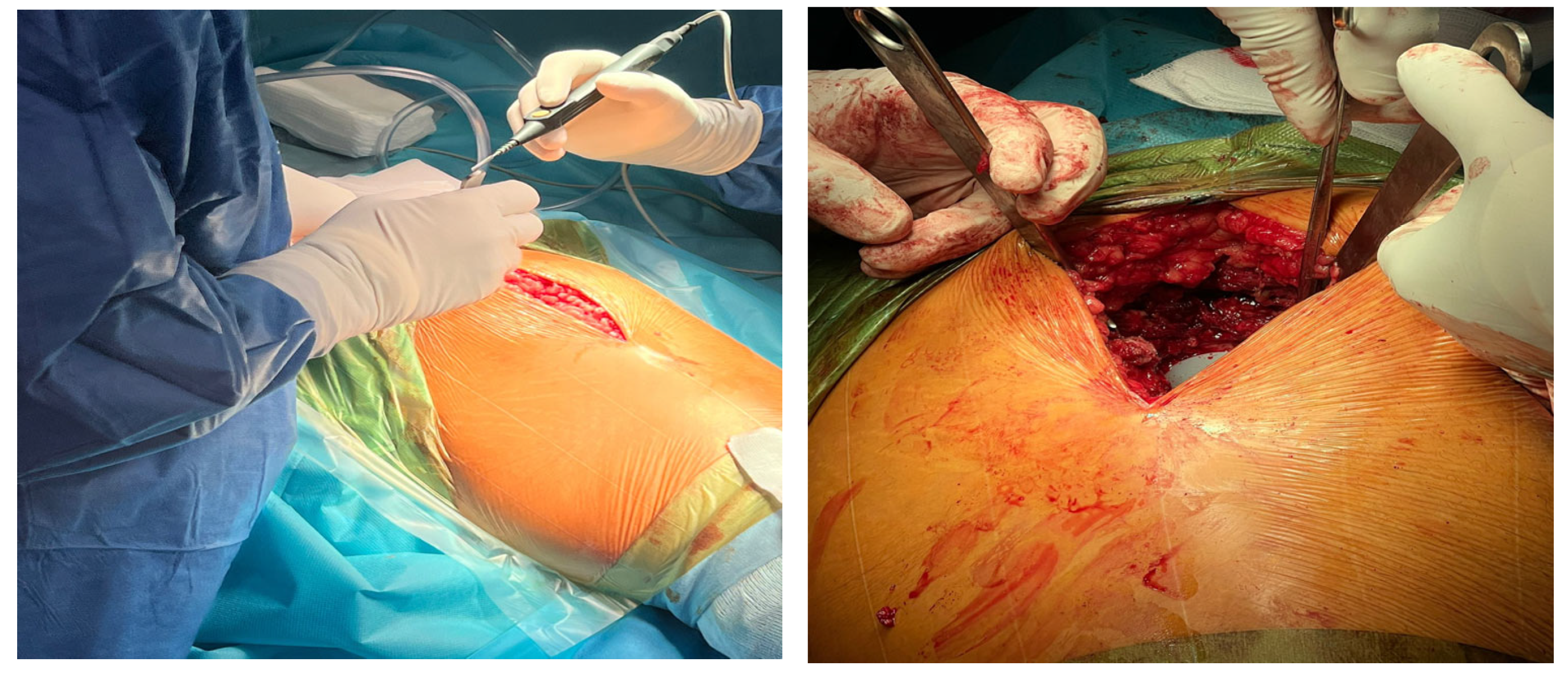
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
3.1. Baseline Demographic and Clinical Criteria for the Two Study Groups
3.2. Statistical Characteristics
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jamari, J.; Ammarullah, M.I.; Saad, A.P.M.; Syahrom, A.; Uddin, M.; Van der Heide, E.; Hasan, B. The Effect of Bottom Profile Dimples on the Femoral Head on Wear in Metal-on-Metal Total Hip Arthroplasty. J. Funct. Biomater. 2021, 12, 38. [Google Scholar] [CrossRef] [PubMed]
- Ammarullah, M.I.; Harton, R.; Supriyon, T.; Santoso, G.; Sugiharto, S.; Permana, M.S. Polycrystalline Diamond as a Potential Material for the Hard-on-Hard Bearing of Total Hip Prosthesis: Von Mises Stress Analysis. Biomedicines 2023, 11, 951. [Google Scholar] [CrossRef] [PubMed]
- Salaha, Z.F.M.; Ammarullah, M.I.; Abdullah, N.N.A.A.; Aziz, A.U.A.; Gan, H.S.; Abdul Abdullah, H.; Kadir, M.R.A.; Ramlee, M.H. Biomechanical Effects of the Porous Structure of Gyroid and Voronoi Hip Implants: A Finite Element Analysis Using an Experimentally Validated Model. Materials 2023, 16, 3298. [Google Scholar] [CrossRef] [PubMed]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Wibowo, D.B.; Kurdi, O.; Tauviqirrahman, M.; Jamari, J. Minimizing Risk of Failure from Ceramic-on-Ceramic Total Hip Prosthesis by Selecting Ceramic Materials Based on Tresca Stress. Sustainability 2022, 14, 13413. [Google Scholar] [CrossRef]
- Ammarullah, M.I.I.; Afif, Y.; Maula, M.I.; Winarni, T.I.; Tauviqirrahman, M.; Jamari, J. Tresca stress evaluation of Metal-on-UHMWPE total hip arthroplasty during peak loading from normal walking activity. Mater. Today 2022, 63, S143–S146. [Google Scholar] [CrossRef]
- Basri, H.; Syahrom, A.; Prakoso, A.T.; Wicaksono, D.; Amarullah, M.I.; Ramadhoni, T.S.; Nugraha, R.D. The Analysis of Dimple Geometry on Artificial Hip Joint to the Performance of Lubrication. J. Phys. Conf. Ser. 2019, 1198, 4. [Google Scholar] [CrossRef]
- Pogliacomi, F.; Paraskevopoulos, A.; Costantino, C.; Marenghi, P.; Ceccarelli, F. Influence of surgical experience in the learning curve of a new approach in hip replacement: Anterior mini-invasive vs. standard lateral. Hip Int. 2012, 22, 555–561. [Google Scholar] [CrossRef]
- Zawadsky, M.W.; Paulus, M.C.; Murray, P.J.; Johansen, M.A. Early outcome comparison between the direct anterior approach and the mini-incision posterior approach for primary total hip arthroplasty: 150 consecutive cases. J. Arthroplast. 2014, 29, 1256–1260. [Google Scholar] [CrossRef]
- Sattler, L.N.; Hing, W.A.; Vertullo, C.J. What is the Evidence to Support early Supervised Exercise Therapy after Primary Total Knee Replacement? A Systematic Review and Meta-Analysis. BMC Musculoskelet. Disord. 2019, 20, 42. [Google Scholar] [CrossRef] [Green Version]
- Ward, S.R.; Jones, R.E.; Long, W.T.; Thomas, D.J.; Dorr, L.D. Functional recovery of muscles after minimally invasive total hip arthroplasty. Instr. Course Lect.-Am. Acad. Orthop. Surg. 2008, 57, 252. [Google Scholar]
- Berend, K.R.; Lombardi, A.V., Jr.; Seng, B.E.; Adams, J.B. Enhanced early outcomes with the anterior supine intermuscular approach in primary total hip arthroplasty. J. Bone Jt. Surg. 2009, 91-A, 107–120. [Google Scholar] [CrossRef]
- Ilchmann, T.; Gersbach, S.; Zwicky, L.; Clauss, M. Standard transgluteal versus minimal invasive anterior approach in hip arthroplasty: A prospective, consecutive, cohort study. Orthop. Rev. 2013, 5, 31. [Google Scholar]
- Schweppe, M.L.; Seyler, T.M.; Plate, J.F.; Swenson, R.D.; Lang, J.E. Does surgical approach in total hip arthroplasty affect rehabilitation, discharge disposition and readmission rate? Surg. Technol. Int. 2013, 23, 219–227. [Google Scholar]
- Restrepo, C.; Parvizi, J.; Pour, A.E.; Hozack, W.J. Prospective randomized study of twosurgical approaches for total hip arthroplasty. J. Arthroplast. 2010, 25, 671–679. [Google Scholar] [CrossRef]
- Sebečić, B.; Starešinić, M.; Culjak, V.; Japjec, M. Minimally invasive hip arthroplasty: Advantages and disadvantages. Med. Glas. 2012, 9, 160–165. [Google Scholar]
- Olthof, M.; Stevens, M.; Bulstra, S.K.; van den Akker-Scheek, I. The association between comorbidity and length of hospital stay and costs in total hip arthroplasty patients: A systematic review. J. Arthroplast. 2014, 29, 1009–1014. [Google Scholar] [CrossRef]
- Abeles, A.; Kwasnicki, R.M.; Darzi, A. Enhanced recovery after surgery: Current research insights and future direction. World J. Gastrointest. Surg. 2017, 9, 37–45. [Google Scholar] [CrossRef] [Green Version]
- Stambough, J.B.; Nunley, R.M.; Curry, M.C.; Steger-May, K.; Clohisy, J.C. Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J. Arthroplast. 2015, 30, 521–526. [Google Scholar] [CrossRef] [Green Version]
- McMurry, J.; McNeil, H.; Lafortune, C.; Black, S.; Prorok, J.; Stolee, P. Measuring patients’ experience of rehabilitation services across the care continuum. Part II: Key dimensions. Arch. Phys. Med. Rehabil. 2016, 97, 121–230. [Google Scholar] [CrossRef]
- Tauviqirrahman, M.; Ammarullah, M.I.; Jamari, J.; Saputra, E.; Winarni, T.I.; Kurniawan, F.D.; Shiddiq, S.A.; Heide, E. Analysis of contact pressure in a 3D model of dual-mobility hip joint prosthesis under a gait cycle. Sci. Rep. 2023, 13, 3564. [Google Scholar] [CrossRef]
- Ammarullah, M.I.; Afif, I.Y.; Maula, M.I.; Winarni, T.I.; Tauviqirrahman, M.; Akbar, I.; Basri, H.; Heide, E.; Jamari, J. Tresca Stress Simulation of Metal-on-Metal Total Hip Arthroplasty during Normal Walking Activity. Materials 2021, 14, 7554. [Google Scholar] [CrossRef] [PubMed]
- Putra, R.U.; Basri, H.; Prakoso, T.A.; Chandra, H.; Ammarullah, M.I.; Akbar, I.; Syahrom, A.; Kamarul, T. Level of Activity Changes Increases the Fatigue Life of the Porous Magnesium Scaffold, as Observed in Dynamic Immersion Tests, over Time. Sustainability 2023, 15, 823. [Google Scholar] [CrossRef]
- Hansen, T.B. Fast track in hip arthroplasty. EFORT Open Rev. 2017, 2, 179–188. [Google Scholar] [CrossRef] [PubMed]
- Vendittoli, P.A.; Pellei, K.; Desmeules, F.; Massé, V.; Loubert, C.; Lavigne, M.; Fafard, J.; Fortier, L.P. Enhanced Recovery Short-Stay Hip and Knee Joint Replacement Program Improves Patients Outcomes while Reducing Hospital Costs. Orthop. Traumatol. Surg. Res. 2019, 105, 1237–1243. [Google Scholar] [CrossRef]
- Chua, M.J.; Hart, A.J.; Mittal, R.; Harris, I.A.; Xuan, W.; Naylor, J.M. Early mobilisation after total hip or knee arthroplasty: A multicentre prospective observational study. PLoS ONE 2017, 12, e0179820. [Google Scholar] [CrossRef] [Green Version]
- Ripollés-Melchor, J.; Aldecoa, C.; Fernández-García, R.; Varela-Durán, M.; Aracil-Escoda, N.; García-Rodríguez, D.; Cabezudo-de-la-Muela, L.; Hormaechea-Bolado, L.; Nacarino-Alcorta, B.; Hoffmann, R.; et al. Early Mobilization after total Hip or Knee Arthroplasty: A Substudy of the POWER.2 Study. Braz. J. Anesthesiol. 2021, in press. [Google Scholar]
- Den Hertog, A.; Gliesche, K.; Timm, J.; Mühlbauer, B.; Zebrowski, S. Pathway-Controlled Fast-Track Rehabilitation after Total Knee Arthroplasty: A Randomized Prospective Clinical Study Evaluating the Recovery Pattern, Drug Consumption, and Length of Stay. Arch. Orthop. Trauma Surg. 2012, 132, 1153–1163. [Google Scholar] [CrossRef] [Green Version]
- Bodrogi, A.; Dervin, G.F.; Beaule, P.E. Management of patients undergoing same-day discharge primary total hip and knee arthroplasty. CMAJ 2020, 192, E34–E39. [Google Scholar] [CrossRef] [Green Version]
- Pivec, R.; Issa, K.; Naziri, Q.; Kapadia, B.H.; Bonutti, P.M.; Mont, M.A. Opioid use prior to total hip arthroplasty leads to worse clinical outcomes. Int. Orthop. 2014, 38, 1159–1165. [Google Scholar] [CrossRef] [Green Version]
- Hebl, J.R.; Dilger, J.A.; Byer, D.E.; Kopp, S.L.; Stevens, S.R.; Pagnano, M.W.; Hanssen, A.D.; Horlocker, T.T. A pre-emptive multimodal pathway featuring peripheral nerve block improves perioperative outcomes after major orthopedic surgery. Reg. Anesth. Pain. Med. 2008, 33, 510–517. [Google Scholar] [CrossRef]
- Yoon, R.S.; Nellans, K.W.; Geller, J.A.; Kim, A.D.; Jacobs, M.R.; Macaulay, W. Patient education before hip or knee arthroplasty lowers length of stay. J. Arthroplast. 2010, 25, 547–551. [Google Scholar] [CrossRef]
- Wakabayashi, H.; Hasegawa, M.; Naito, Y.; Tone, S.; Sudo, A. Minimum 10-Year Results of Modular Metal-On-Metal Total Hip Arthroplast. J. Clin. Med. 2022, 11, 6505. [Google Scholar] [CrossRef]
- Abrishami, A.; Chan, J.; Chung, F.; Wong, J. Preoperative pain sensitivity and its correlation with postoperative pain and analgesic consumption: A qualitative systematic review. Anesthesiology 2011, 114, 445–457. [Google Scholar] [CrossRef] [Green Version]
- Jin, Z.; Gan, T.J.; Bergese, S.D. Prevention and Treatment of Postoperative Nausea and Vomiting (PONV): A Review of Current Recommendations and Emerging Therapies. Ther. Clin. Risk Manag. 2020, 16, 1305–1317. [Google Scholar] [CrossRef]
- Hersnaes, P.N.; Gromov, K.; Otte, K.S.; Gebuhr, P.H.; Troelsen, A. Harris Hip Score and SF-36 Following Metal-on-Metal Total Hip Arthroplasty and Hip Resurfacing—A Randomized Controlled Trial with 5-Years Follow up Including 75 Patients. BMC Musculoskelet. Disord. 2021, 22, 781. [Google Scholar] [CrossRef]
- Russo, M.W.; Macdonell, J.R.; Paulus, M.C.; Keller, J.M.; Zawadsky, M.W. Increased complications in obese patients undergoing direct anterior total hip arthroplasty. J. Arthroplast. 2015, 30, 1384–1387. [Google Scholar] [CrossRef]
- Huschak, G.; Thilo, B.; Udo, X.K. Obesity in anesthesia and intensive care. Best Pract. Res. Clin. Endocrinol. Metab. 2013, 27, 247–260. [Google Scholar] [CrossRef]
- Ortiz-Declet, V.R.; Iacobelli, D.A.; Yuen, L.C.; Perets, I.; Chen, A.W.; Domb, B.G. Birmingham Hip Resurfacing vs. Total Hip Arthroplasty: A Matched-Pair Comparison of Clinical Outcomes. J. Arthroplast. 2017, 32, 3647–3651. [Google Scholar] [CrossRef]
- Lübbeke, A.; Stern, R.; Garavaglia, G.; Zurcher, L.; Hoffmeyer, P. Differences in outcomes of obese women and men undergoing primary total hip arthroplasty. Arthritis Rheum. 2007, 57, 327–334. [Google Scholar] [CrossRef] [Green Version]
- Costa, M.L.; Achten, J.; Parsons, N.R.; Edlin, R.P.; Foguet, P.; Prakash, U.; Griffin, D.R. Total Hip Arthroplasty versus Resurfacing Arthroplasty in the Treatment of Patients with Arthritis of the Hip Joint: Single Centre, Parallel Group, Assessor Blinded, Randomised Controlled Trial. BMJ 2012, 344, e2147. [Google Scholar] [CrossRef] [Green Version]
- Learmonth, I.D.; Young, C.; Rorabeck, C. The Operation of the Century: Total Hip Replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef] [PubMed]
- Ma, H.H.; Chou, T.A.; Tsai, S.W.; Chen, C.F.; Wu, P.K.; Chen, W.M. The Efficacy of Intraoperative Periarticular Injection in Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. BMC Musculoskelet. Disord. 2019, 20, 269. [Google Scholar] [CrossRef] [PubMed]



| Anterior Approach (n = 66) | Lateral Approach (n = 49) | Statistical Significance (p) | |
|---|---|---|---|
| Gender (M/F) | 32/34 | 19/30 | 0.3972 |
| Age—media (SD) | 62.9 (12.5) | 65.3 (10.7) | 0.3080 |
| Environment of origin (U/R) | 49/17 | 32/17 | 0.4055 |
| BMI (kg/m2)—media (SD) | 28.5 (3.9) | 29.9 (5.7) | 0.1333 |
| Comorbidities (percentage—%): | 0.4513 | ||
| 43 (65.2) | 30 (61.2) | |
| 1 (1.5) | 2 (4.1) | |
| 0 (0) | 1 (2.0) | |
| 0 (0) | 2 (4.1) | |
| 13 (19.7) | 10 (20.4) | |
| 1 (1.5) | 1 (2.0) |
| Anterior Approach (n = 66) | Lateral Approach (n = 49) | Statistical Significance (p) | |
|---|---|---|---|
| Postoperative mobilization score 12 h—median (IQR) | 0 (0–2) | 1 (0–2) | 0.4286 |
| Postoperative mobilization score 24 h—median (IQR) | 2 (2–3) | 2 (1–3) | 0.3406 |
| Postoperative mobilization score 48 h—median (IQR) | 3 (3–4) | 3 (2–4) | 0.2196 |
| Postoperative mobilization score 96 h—median (IQR) | 4 (3.75–5) | 4 (3–4) | 0.0237 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bontea, M.; Bimbo-Szuhai, E.; Macovei, I.C.; Maghiar, P.B.; Sandor, M.; Botea, M.; Romanescu, D.; Beiusanu, C.; Cacuci, A.; Sachelarie, L.; et al. Anterior Approach to Hip Arthroplasty with Early Mobilization Key for Reduced Hospital Length of Stay. Medicina 2023, 59, 1216. https://doi.org/10.3390/medicina59071216
Bontea M, Bimbo-Szuhai E, Macovei IC, Maghiar PB, Sandor M, Botea M, Romanescu D, Beiusanu C, Cacuci A, Sachelarie L, et al. Anterior Approach to Hip Arthroplasty with Early Mobilization Key for Reduced Hospital Length of Stay. Medicina. 2023; 59(7):1216. https://doi.org/10.3390/medicina59071216
Chicago/Turabian StyleBontea, Mihaela, Erika Bimbo-Szuhai, Iulia Codruta Macovei, Paula Bianca Maghiar, Mircea Sandor, Mihai Botea, Dana Romanescu, Corina Beiusanu, Adriana Cacuci, Liliana Sachelarie, and et al. 2023. "Anterior Approach to Hip Arthroplasty with Early Mobilization Key for Reduced Hospital Length of Stay" Medicina 59, no. 7: 1216. https://doi.org/10.3390/medicina59071216
APA StyleBontea, M., Bimbo-Szuhai, E., Macovei, I. C., Maghiar, P. B., Sandor, M., Botea, M., Romanescu, D., Beiusanu, C., Cacuci, A., Sachelarie, L., & Huniadi, A. (2023). Anterior Approach to Hip Arthroplasty with Early Mobilization Key for Reduced Hospital Length of Stay. Medicina, 59(7), 1216. https://doi.org/10.3390/medicina59071216







