Cooling Efficiency of Sleeveless 3D-Printed Surgical Guides with Different Cylinder Designs
Abstract
:1. Introduction
2. Materials and Methods
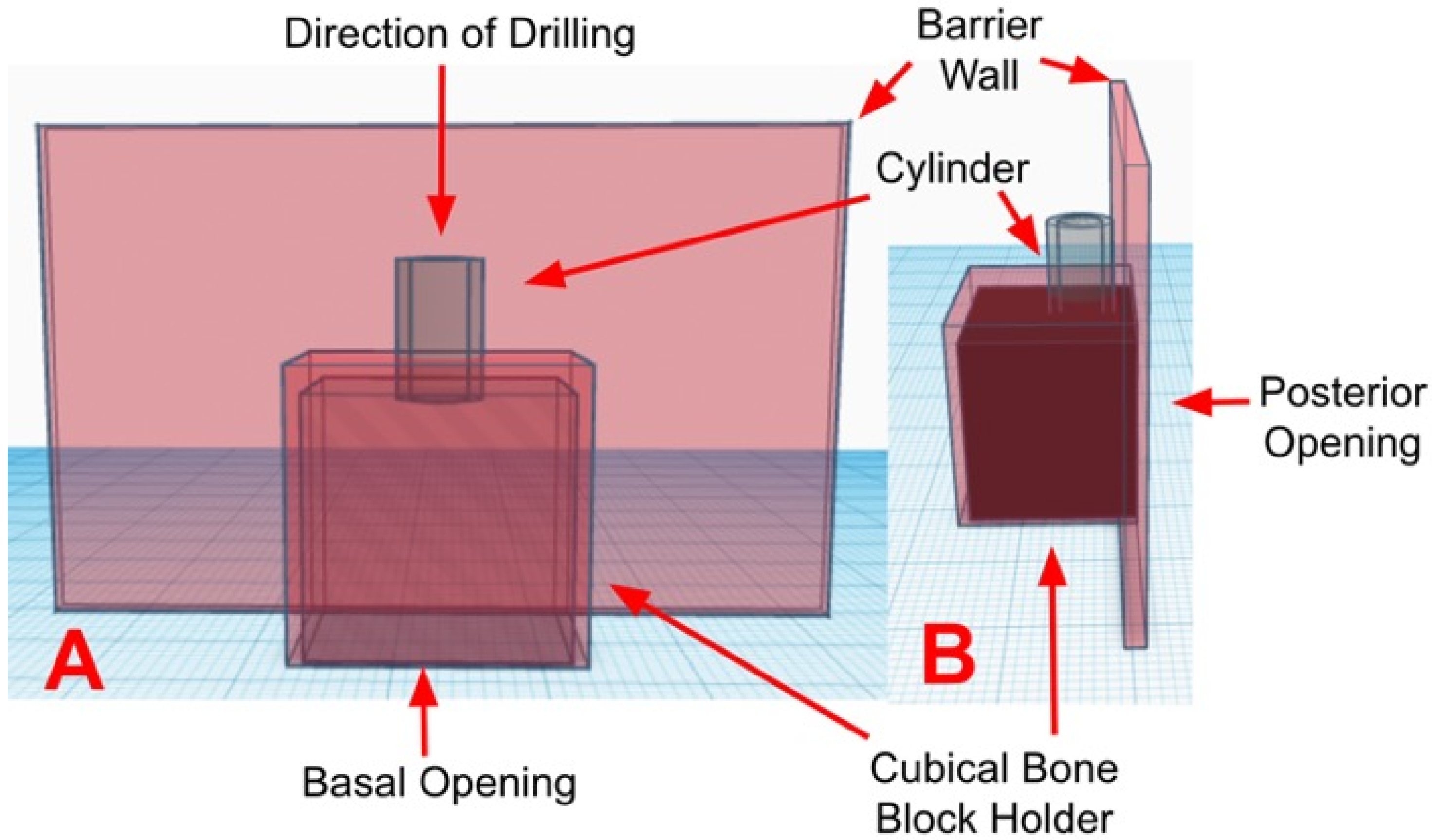
2.1. Design and Fabrication of the Surgical Guides
2.2. Fabrication of the Custom Polyurethane Blocks
2.3. Experiment Set-Up
2.4. Drilling and Temperature Live Recording
2.5. Statistical Analysis
3. Results
3.1. Temperature at the Coronal Region
3.2. Temperature in the Middle Region
3.3. Temperature in the Apical Region
4. Discussion
4.1. Limitations and Strengths of This Study
4.2. Clinical Significance
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Delgado-Ruiz, R.A.; Velasco Ortega, E.; Romanos, G.E.; Gerhke, S.; Newen, I.; Calvo-Guirado, J.L. Slow Drilling Speeds for Single-Drill Implant Bed Preparation. Experimental in Vitro Study. Clin. Oral Investig. 2018, 22, 349–359. [Google Scholar] [CrossRef]
- Heuzeroth, R.; Pippenger, B.E.; Sandgren, R.; Bellón, B.; Kühl, S. Thermal Exposure of Implant Osteotomies and Its Impact on Osseointegration-A Preclinical in Vivo Study. Clin. Oral Implants Res. 2021, 32, 672–683. [Google Scholar] [CrossRef]
- Eriksson, A.R.; Albrektsson, T. Temperature Threshold Levels for Heat-Induced Bone Tissue Injury: A Vital-Microscopic Study in the Rabbit. J. Prosthet. Dent. 1983, 50, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Marković, A.; Lazić, Z.; Mišić, T.; Šćepanović, M.; Todorović, A.; Thakare, K.; Janjić, B.; Vlahović, Z.; Glišić, M. Effect of Surgical Drill Guide and Irrigans Temperature on Thermal Bone Changes during Drilling Implant Sites-Thermographic Analysis on Bovine Ribs. Vojnosanit. Pregl. 2016, 73, 744–750. [Google Scholar] [CrossRef]
- Jung, O.; Lindner, C.; Pantermehl, S.; Barbeck, M. Heat Development During Medical Drilling: Influencing Factors and Examination Methods-Overview and First Results. In Vivo 2021, 35, 3011–3017. [Google Scholar] [CrossRef] [PubMed]
- Akhbar, M.F.A.; Sulong, A.W. Surgical Drill Bit Design and Thermomechanical Damage in Bone Drilling: A Review. Ann. Biomed. Eng. 2021, 49, 29–56. [Google Scholar] [CrossRef] [PubMed]
- Boa, K.; Barrak, I.; Varga, E.; Joob-Fancsaly, A.; Varga, E.; Piffko, J. Intraosseous Generation of Heat during Guided Surgical Drilling: An Ex Vivo Study of the Effect of the Temperature of the Irrigating Fluid. Br. J. Oral Maxillofac. Surg. 2016, 54, 904–908. [Google Scholar] [CrossRef]
- Sharawy, M.; Misch, C.E.; Weller, N.; Tehemar, S. Heat Generation during Implant Drilling: The Significance of Motor Speed. J. Oral Maxillofac. Surg. 2002, 60, 1160–1169. [Google Scholar] [CrossRef]
- Reingewirtz, Y.; Szmukler-Moncler, S.; Senger, B. Influence of Different Parameters on Bone Heating and Drilling Time in Implantology. Clin. Oral Implants Res. 1997, 8, 189–197. [Google Scholar] [CrossRef]
- Tahmasebi, S. The Effect of Surgical Guides on Heat Generation during Guided Implant Surgery: An In Vitro Study. Master’s Thesis, West Virginia University, Morgantown, WV, USA, 2013. [Google Scholar]
- Benington, I.C.; Biagioni, P.A.; Briggs, J.; Sheridan, S.; Lamey, P.-J. Thermal Changes Observed at Implant Sites during Internal and External Irrigation. Clin. Oral Implants Res. 2002, 13, 293–297. [Google Scholar] [CrossRef]
- Trisi, P.; Berardini, M.; Falco, A.; Podaliri Vulpiani, M.; Perfetti, G. Insufficient Irrigation Induces Peri-Implant Bone Resorption: An in Vivo Histologic Analysis in Sheep. Clin. Oral Implants Res. 2014, 25, 696–701. [Google Scholar] [CrossRef] [PubMed]
- Barrak, I.; Joób-Fancsaly, A.; Varga, E.; Boa, K.; Piffko, J. Effect of the Combination of Low-Speed Drilling and Cooled Irrigation Fluid on Intraosseous Heat Generation During Guided Surgical Implant Site Preparation: An In Vitro Study. Implant. Dent. 2017, 26, 541–546. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.-F.; Wu, J.-L.; Zhang, J.-X.; Peng, W.; Liao, W.-Q. Numerical and Experimental Analyses on the Temperature Distribution in the Dental Implant Preparation Area When Using a Surgical Guide. J. Prosthodont. 2018, 27, 42–51. [Google Scholar] [CrossRef]
- Misir, A.F.; Sumer, M.; Yenisey, M.; Ergioglu, E. Effect of Surgical Drill Guide on Heat Generated from Implant Drilling. J. Oral Maxillofac. Surg. 2009, 67, 2663–2668. [Google Scholar] [CrossRef] [PubMed]
- dos Santos, P.L.; Queiroz, T.P.; Margonar, R.; de Souza Carvalho, A.C.G.; Betoni, W.; Rezende, R.R.R.; dos Santos, P.H.; Garcia, I.R. Evaluation of Bone Heating, Drill Deformation, and Drill Roughness after Implant Osteotomy: Guided Surgery and Classic Drilling Procedure. Int. J. Oral Maxillofac. Implants 2014, 29, 51–58. [Google Scholar] [CrossRef]
- Adams, C.R.; Ammoun, R.; Deeb, G.R.; Bencharit, S. Influence of Metal Guide Sleeves on the Accuracy and Precision of Dental Implant Placement Using Guided Implant Surgery: An In Vitro Study. J. Prosthodont. 2023, 32, 62–70. [Google Scholar] [CrossRef]
- Tallarico, M.; Czajkowska, M.; Cicciù, M.; Giardina, F.; Minciarelli, A.; Zadrożny, Ł.; Park, C.-J.; Meloni, S.M. Accuracy of Surgical Templates with and without Metallic Sleeves in Case of Partial Arch Restorations: A Systematic Review. J. Dent. 2021, 115, 103852. [Google Scholar] [CrossRef]
- Oh, K.C.; Shim, J.-S.; Park, J.-M. In Vitro Comparison between Metal Sleeve-Free and Metal Sleeve-Incorporated 3D-Printed Computer-Assisted Implant Surgical Guides. Materials 2021, 14, 615. [Google Scholar] [CrossRef]
- Orgev, A.; Gonzaga, L.; Martin, W.; Morton, D.; Lin, W.-S. Addition of an Irrigation Channel to a Surgical Template to Facilitate Cooling during Implant Osteotomy. J. Prosthet. Dent. 2021, 126, 164–166. [Google Scholar] [CrossRef]
- Ashry, A.; Elattar, M.S.; Elsamni, O.A.; Soliman, I.S. Effect of Guiding Sleeve Design on Intraosseous Heat Generation During Implant Site Preparation (In Vitro Study). J. Prosthodont. 2022, 31, 147–154. [Google Scholar] [CrossRef]
- Teich, S.; Bocklet, M.; Evans, Z.; Gutmacher, Z.; Renne, W. 3D Printed Implant Surgical Guides with Internally Routed Irrigation for Temperature Reduction during Osteotomy Preparation: A Pilot Study. J. Esthet. Restor. Dent. 2022, 34, 796–803. [Google Scholar] [CrossRef]
- Choi, Y.-S.; Oh, J.-W.; Lee, Y.; Lee, D.-W. Thermal Changes during Implant Site Preparation with a Digital Surgical Guide and Slot Design Drill: An Ex Vivo Study Using a Bovine Rib Model. J. Periodontal Implant. Sci. 2022, 52, 411–421. [Google Scholar] [CrossRef]
- Galli, M.; Mendonça, G.; Meneghetti, P.; Bekkali, M.; Travan, S.; Wang, H.-L.; Li, J. Sleeveless Guided Implant Placement Compared to Conventional Approaches: An in Vitro Study at Healed Sites and Fresh Extraction Sockets. Int. J. Oral Implantol. 2023, 16, 117–132. [Google Scholar]
- Raabe, C.; Schuetz, T.S.; Chappuis, V.; Yilmaz, B.; Abou-Ayash, S.; Couso-Queiruga, E. Accuracy of Keyless vs. Drill-Key Implant Systems for Static Computer-Assisted Implant Surgery Using Two Guide-Hole Designs Compared to Freehand Implant Placement: An in Vitro Study. Int. J. Implant. Dent. 2023, 9, 4. [Google Scholar] [CrossRef] [PubMed]
- Tallarico, M.; Lumbau, A.I.; Park, C.-J.; Puddu, A.; Sanseverino, F.; Amarena, R.; Meloni, S.M. In Vitro Evaluation of Bioburden, Three-Dimensional Stability, and Accuracy of Surgical Templates without Metallic Sleeves after Routinely Infection Control Activities. Clin. Implant. Dent. Relat. Res. 2021, 23, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Ozan, O.; Şeker, E.; Çakmak, G.; Guo, X.; Yilmaz, B. Effect of Guide Sleeve Material, Region, Diameter, and Number of Times Drills Were Used on the Material Loss from Sleeves and Drills Used for Surgical Guides: An In Vitro Study. J. Prosthet. Dent. 2022, 128, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Tuce, R.A.; Neagu, M.; Pupazan, V.; Neagu, A.; Arjoca, S. The 3D Printing and Evaluation of Surgical Guides with an Incorporated Irrigation Channel for Dental Implant Placement. Bioengineering 2023, 10, 1168. [Google Scholar] [CrossRef] [PubMed]
- Parvizi, S.; Cameron, A.; Tadakamadla, S.; Figueredo, C.M.S.; Reher, P. A Novel Irrigation System to Reduce Heat Generation during Guided Implantology: An In Vitro Study. J. Clin. Med. 2023, 12, 3944. [Google Scholar] [CrossRef]






| Cylinder Type and Region of Evaluation | n | Mean ± StDev | 95% CI |
|---|---|---|---|
| Cor-NI | 10 | 39.69 ± 8.82 | (36.83, 42.55) |
| Mid-NI | 25.989 ± 0.551 | (25.324, 26.654) | |
| Api-NI | 25.591 ± 0.494 | (24.852, 26.330) | |
| Cor-Sol | 10 | 25.005 ± 0.586 | (22.142, 27.868) |
| Mid-Sol | 24.443 ± 0.768 | (23.778, 25.108) | |
| Api-Sol | 24.221 ± 0.964 | (23.482, 24.960) | |
| Cor-Win | 10 | 21.451 ± 0.703 | (18.588, 24.314) |
| Mid-Win | 21.139 ± 0.533 | (20.474, 21.804) | |
| Api-Win | 21.133 ± 0.565 | (20.394, 21.872) | |
| Cor-Por | 10 | 25.630 ± 1.004 | (22.767, 28.493) |
| Mid-Por | 24.909 ± 1.766 | (24.244, 25.574) | |
| Api-Por | 24.691 ± 1.952 | (23.952, 25.430) |
| Comparisons | Difference of Means | SE of Difference | 95% CI | T-Value | p-Value |
|---|---|---|---|---|---|
| Cor-Win vs. Cor-Sol | −3.554 | 0.289 | (−4.375, −2.733) | −12.28 | p < 0.001 |
| Cor-Por vs. Cor-Sol | 0.625 | 0.368 | (−0.438, 1.688) | 1.70 | 0.359 |
| Cor-NI vs. Cor-Sol | 14.68 | 2.80 | (5.96, 23.41) | 5.25 | 0.002 |
| Cor-Por vs. Cor-Win | 4.179 | 0.388 | (3.072, 5.286) | 10.78 | p < 0.001 |
| Cor-NI vs. Cor-Win | 18.24 | 2.80 | (9.53, 26.95) | 6.51 | p < 0.001 |
| Cor-NI vs. Cor-Por | 14.06 | 2.81 | (5.34, 22.78) | 5.01 | 0.003 |
| Mid-Win vs. Mid-Sol | −3.304 | 0.296 | (−4.148, −2.460) | −11.18 | p < 0.001 |
| Mid-Por vs. Mid-Sol | 0.466 | 0.609 | (−1.334, 2.266) | 0.77 | 0.868 |
| Mid-NI vs. Mid-Sol | 1.546 | 0.299 | (0.692, 2.400) | 5.17 | p < 0.001 |
| Mid-Por vs. Mid-Win | 3.770 | 0.583 | (2.005, 5.535) | 6.46 | p < 0.001 |
| Mid-NI vs. Mid-Win | 4.850 | 0.243 | (4.164, 5.536) | 20.00 | p < 0.001 |
| Mid-NI vs. Mid-Por | 1.080 | 0.585 | (−0.686, 2.846) | 1.85 | 0.305 |
| Api-Win vs. Api-Sol | −3.088 | 0.353 | (−4.110, −2.066) | -8.74 | p < 0.001 |
| Api-Por vs. Api-Sol | 0.470 | 0.689 | (−1.546, 2.486) | 0.68 | 0.902 |
| Api-NI vs. Api-Sol | 1.370 | 0.343 | (0.369, 2.371) | 4.00 | 0.007 |
| Api-Por vs. Api-Win | 3.558 | 0.643 | (1.608, 5.508) | 5.54 | p < 0.001 |
| Api-NI vs. Api-Win | 4.458 | 0.237 | (3.787, 5.129) | 18.79 | p < 0.001 |
| Api-NI vs. Api-Por | 0.900 | 0.637 | (−1.046, 2.846) | 1.41 | 0.519 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, A.; Brintouch, I.; Romanos, G.; Delgado-Ruiz, R. Cooling Efficiency of Sleeveless 3D-Printed Surgical Guides with Different Cylinder Designs. Medicina 2024, 60, 239. https://doi.org/10.3390/medicina60020239
Ali A, Brintouch I, Romanos G, Delgado-Ruiz R. Cooling Efficiency of Sleeveless 3D-Printed Surgical Guides with Different Cylinder Designs. Medicina. 2024; 60(2):239. https://doi.org/10.3390/medicina60020239
Chicago/Turabian StyleAli, Aisha, Ido Brintouch, Georgios Romanos, and Rafael Delgado-Ruiz. 2024. "Cooling Efficiency of Sleeveless 3D-Printed Surgical Guides with Different Cylinder Designs" Medicina 60, no. 2: 239. https://doi.org/10.3390/medicina60020239








