Effects of Rhythm Step Training on Foot and Lower Limb Balance in Children and Adolescents with Flat Feet: A Radiographic Analysis
Abstract
1. Introduction
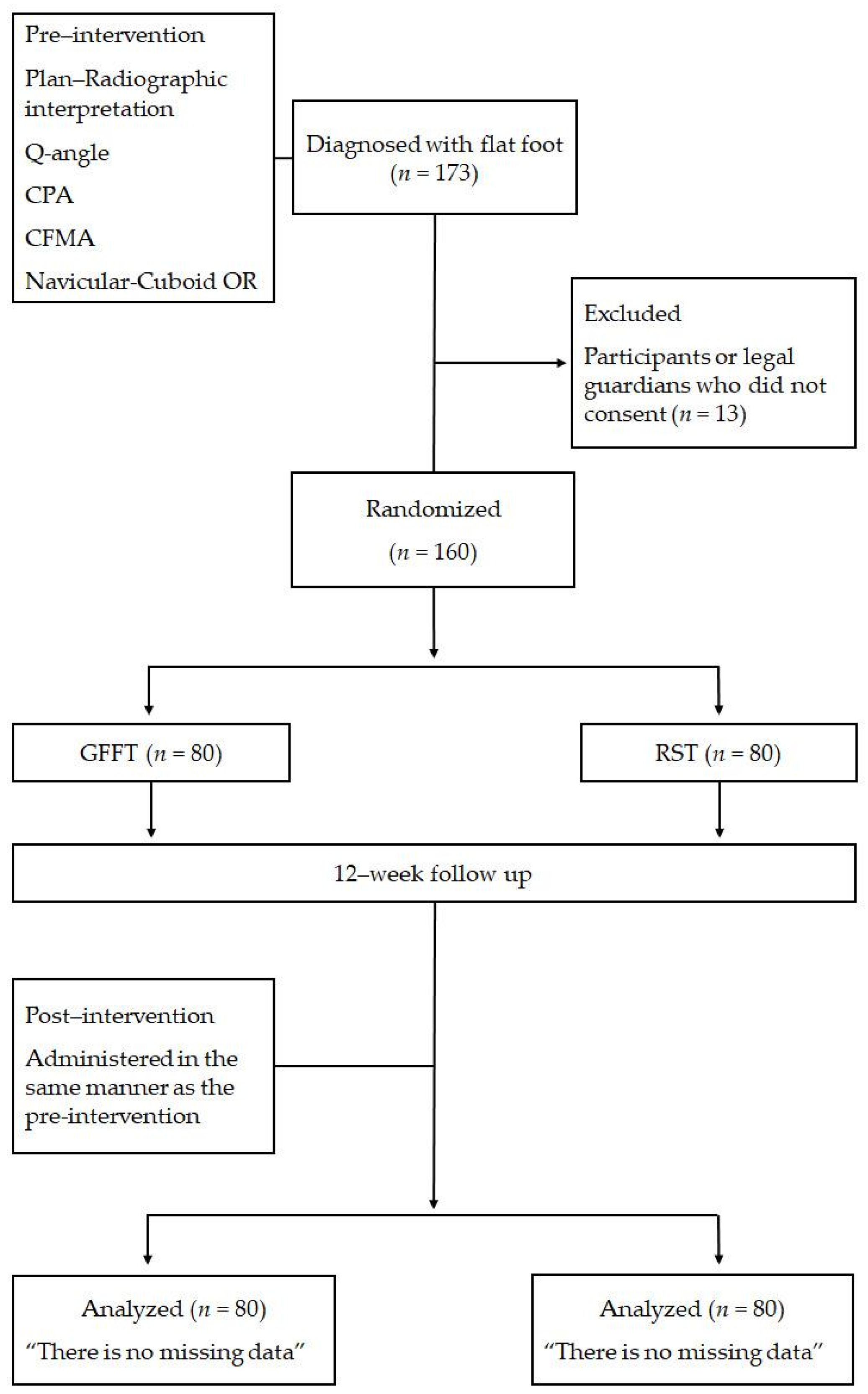
2. Materials and Methods
2.1. Participants
2.2. Procedures
2.3. Experimental Design and Measurements
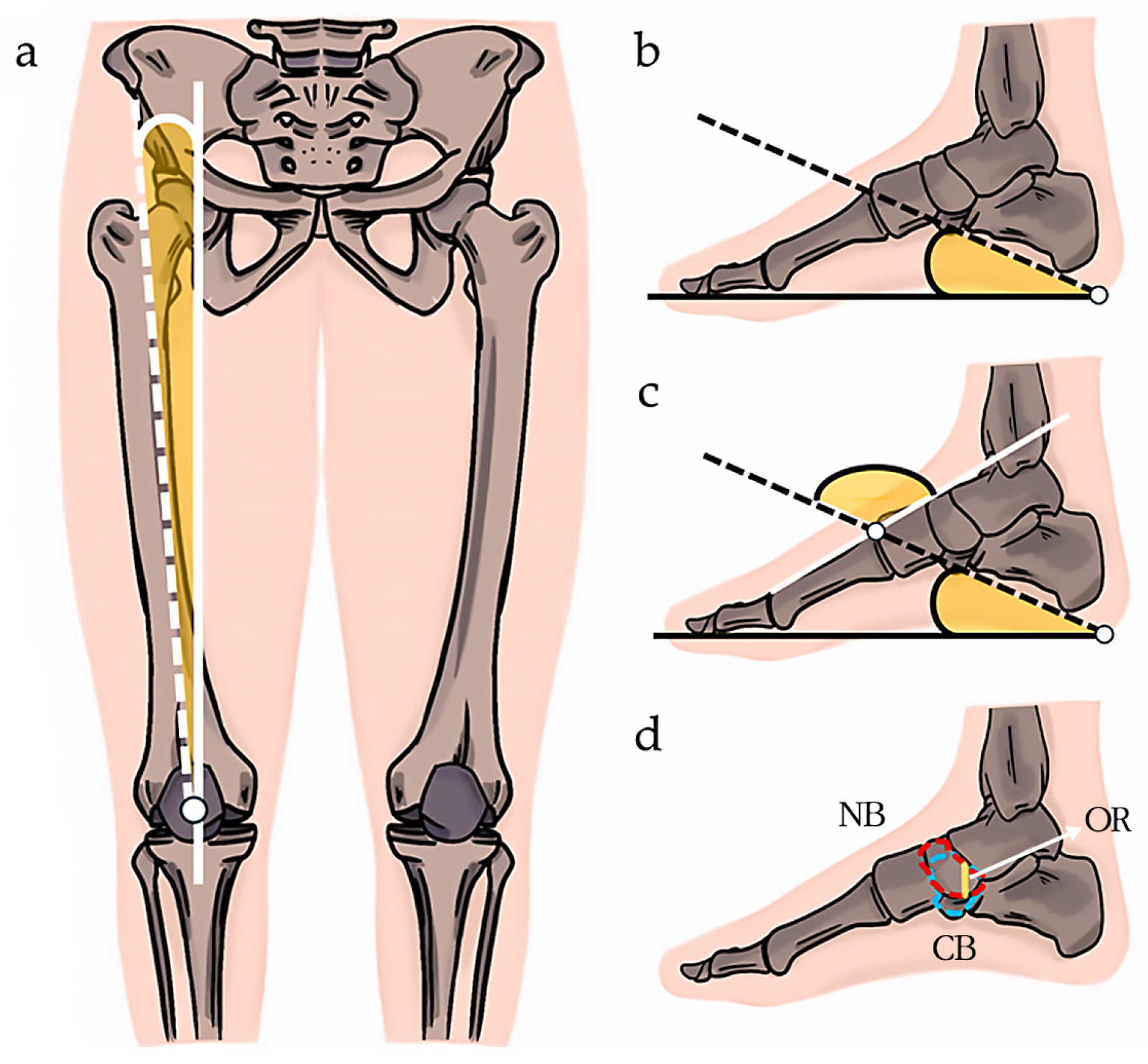
2.4. Q-Angle Measurement
2.5. CPA Measurement
2.6. CFMA Measurement
2.7. Navicular–Cuboid OR Measurement
2.8. GFFT and RST Exercise Programs
2.9. Statistical Analysis
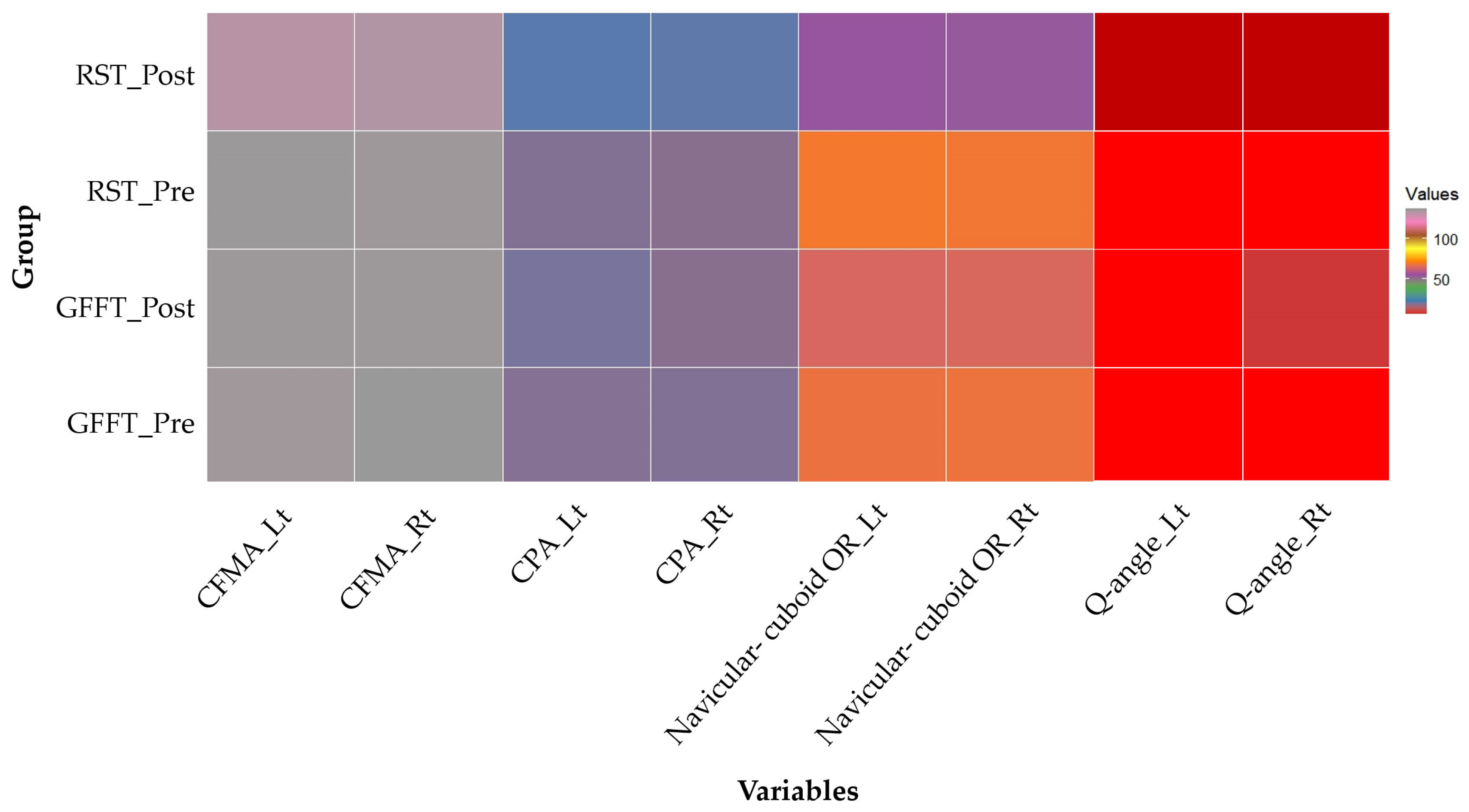
3. Results
3.1. Q-Angle Changes
3.2. CPA Changes
3.3. CFMA Changes
3.4. Navicular–Cuboid OR Changes
4. Discussion
4.1. Q-Angle Changes
4.2. CPA Changes
4.3. CFMA Changes
4.4. Navicular–Cuboid OR Changes
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saini, U.C.; Bali, K.; Sheth, B.; Gahlot, N.; Gahlot, A. Normal development of the knee angle in healthy Indian children: A clinical study of 215 children. J. Child. Orthop. 2010, 4, 579–586. [Google Scholar] [CrossRef]
- Cheng, J.C.; Chan, P.S.; Chiang, S.C.; Hui, P.W. Angular and rotational profile of the lower limb in 2630 Chinese children. J. Pediatr. Orthop. 1991, 11, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Pantano, K.J.; White, S.C.; Gilchrist, L.A.; Leddy, J. Differences in peak knee valgus angles between individuals with high and low Q-angles during a single limb squat. Clin. Biomech. 2005, 20, 966–972. [Google Scholar] [CrossRef]
- Jafarnezhadgero, A.A.; Shad, M.M.; Majlesi, M.; Granacher, U. A comparison of running kinetics in children with and without genu varus: A cross sectional study. PLoS ONE 2017, 12, e0185057. [Google Scholar] [CrossRef]
- Mosca, V.S. Flexible flat foot in children and adolescents. J. Child. Orthop. 2010, 4, 107–121. [Google Scholar] [CrossRef] [PubMed]
- Carr, J.B.; Yang, S.; Lather, L.A. Pediatric pes planus: A state-of-the-art review. Pediatrics 2016, 137, e20151230. [Google Scholar] [CrossRef]
- Evans, A.M.; Rome, K. A Cochrane review of the evidence for non-surgical interventions for flexible pediatric flat feet. Eur. J. Phys. Rehabil. Med. 2011, 47, 69–89. [Google Scholar] [PubMed]
- Angin, S.; Demirbuken. Comparative Kinesiology of the Human Body, 1st ed.; Elsevier: Amsterdam, The Netherlands, 2020; pp. 411–439. [Google Scholar]
- Mckeon, P.O.; Hertel, J.; Bramble, D.; Davis, I. The foot core system: A new paradigm for understanding intrinsic foot muscle function. Br. J. Sports Med. 2015, 49, 290. [Google Scholar] [CrossRef]
- Golchini, A.; Rahnama, N. The effect of systematic corrective exercises on the ankle proprioception in people with functional pronation distortion syndrome: A randomized controlled clinical trial study. J. Res. Rehabil. Sci. 2019, 14, 366–374. [Google Scholar]
- Najafi, M.; Shojaedin, S.; Hadadnezhad, M.; Barati, A.H. Effect of eight-week corrective exercises on the activity of involved muscles in ankle balance strategies in girls with lower limb pronation syndrome. Sci. J. Rehabil. Med. 2018, 7, 77–87. [Google Scholar]
- Sahrmann, S.; Azevedo, D.C.; Dillen, V.L. Diagnosis and treatment of movement system impairment syndromes. Braz. J. Phys. Ther. 2017, 21, 391–399. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.M.; Lee, T.K.; Lee, S.H. Prevalence of flatfoot among young korean males and the correlation among flatfoot angles measured in weight-bearing lateral radiographs. Medicine 2022, 101, e29720. [Google Scholar] [CrossRef] [PubMed]
- Toullec, E. Adult flatfoot. Orthop. Traumatol. Surg. Res. 2015, 101, S11–S17. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.; Burke, E.R. Scientific, medical, and practical aspects of stretching. Clin. Sports Med. 1991, 10, 63–86. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.S.; Kim, J.J.; Kim, H.W.; Lewis, M.P.; Wall, I. Impact of mechanical stretch on the cell behaviors of bone and surrounding tissues. J. Tissue Eng. 2016, 13, 2041731415618342. [Google Scholar] [CrossRef]
- Health Insurance Review & Assessment Service. HIRA Bigdata Open Portal. The Number of Patients Who Visited the Hospital for Flat Feet. Available online: https://opendata.hira.or.kr/op/opc/olap3thDsInfoTab3.do (accessed on 16 January 2024).
- Markowicz, M.; Skrobot, W.; Łabuć, A.; Poszytek, P.; Orlikowska, A.; Perzanowska, E.; Krasowska, K.; Drewek, K.; Kaczor, J.J. The rehabilitation program improves balance control in children with excessive body weight and flat feet by activating the intrinsic muscles of the foot: A preliminary study. J. Clin. Med. 2023, 12, 3364. [Google Scholar] [CrossRef]
- Lipnowski, S.; Leblanc, C.M. Healthy active living: Physical activity guidelines for children and adolescents. Paediatr. Child Health 2012, 17, 209–212. [Google Scholar] [CrossRef]
- Almeida-Neto, P.F.; Oliveira, V.M.M.; Matos, D.G.; Santos, I.K.D.; Baxter-Jones, A.; Pinto, V.C.M.; Cesário, T.M.; Aidar, F.J.; Dantas, P.M.S.; Cabral, B.G.A.T. Factors related to lower limb performance in children and adolescents aged 7 to 17 years: A systematic review with meta-analysis. PLoS ONE 2021, 16, e0258144. [Google Scholar] [CrossRef]
- Arima, S.; Maeda, N.; Tsutsumi, S.; Ishihara, H.; Ikuta, Y.; Ushio, K.; Fujishita, H.; Kobayashi, T.; Komiya, M.; Morikawa, M.; et al. Association of the intrinsic foot muscles and plantar fascia with repetitive rebound jumping and jump landing in adolescent athletes: An ultrasound-based study. Gait Posture 2023, 99, 146–151. [Google Scholar] [CrossRef]
- Park, K.S.; Williams, D.M.; Etnier, J.L. Exploring the use of music to promote physical activity: From the viewpoint of psychological hedonims. Front. Psychol. 2023, 14, 1021825. [Google Scholar] [CrossRef]
- Tabei, K.I.; Satoh, M.; Ogawa, J.I.; Tokita, T.; Nakaguchi, N.; Nakao, K.; Kida, H.; Tomimoto, H. Physical exercise with music reduces gray and white matter loss in the frontal cortex of elderly people: The mihama-kiho scan project. Front. Aging Neurosci. 2017, 9, 174. [Google Scholar] [CrossRef]
- Park, S.K.; Jee, Y.S. Effects of Rhythm step training on physical and cognitive functions in adolescents: A prospective randomized controlled trial. Healthcare 2022, 10, 712. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.S.; Koh, K.; Yang, J.S.; Shim, J.K. Efficacy of rhythmic exercise and walking exercise in older adults’ exercise participation rates and physical function outcomes. Geriatr. Gerontol. Int. 2017, 17, 2311–2318. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.C.; Yeow, K.M.; Yeow, Y.J. Imaging approaches for accurate determination of the quadriceps angle. Orthop. Surg. 2020, 12, 1270–1276. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.M.; Chung, C.Y.; Park, M.S.; Lee, S.H.; Cho, J.H.; Choi, I.H. Reliability and validity of radiographic measurements in hind foot varus and valgus. J. Bone Jt. Surg. Am. 2010, 92, 2319–2327. [Google Scholar] [CrossRef] [PubMed]
- Abd-Elmonem, A.M.; El-Negamy, E.H.; Mahran, M.A.; Ramadan, A.T. Clinical and radiological outcomes of corrective exercises and neuromuscular electrical stimulation in children with flexible flat feet: A randomized controlled trial. Gait Posture 2021, 88, 297–303. [Google Scholar] [CrossRef]
- Koo, S.B.; Chun, S.H.; Lee, K.M.; Cho, B.C.; Koo, Y.J.; Kang, D.W.; Park, M.S. Sex differences in pedobarographic findings and relationship between radiographic and pedobarographic measurements in young healthy adults. Clin. Orthop. Surg. 2018, 10, 216–224. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.; Nieman, D.C.; Swain, D. American college of sports medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Sivachandiran, S.; Kumar, G.V. Effect of corrective exercises programme among athletes with flat feet on foot alignment factors. Int. J. Sports Health Phys. Educ. 2016, 3, 193–196. [Google Scholar]
- Sharma, R.; Vaibhav, V.; Meshram, R.; Singh, B.; Khorwal, G. A Systematic review on quadriceps angle in relation to knee abnormalities. Cureus 2023, 15, e34355. [Google Scholar] [CrossRef]
- Çankaya, T.; Dursun, Ö.; Davazlı, B.; Toprak, H.; Çankaya, H.; Alkan, B. Assessment of quadriceps angle in children aged between 2 and 8 years. Turk. Arch. Pediatr. 2020, 55, 124–130. [Google Scholar]
- Khasawneh, R.R.; Allouh, M.Z.; Abu-El-Rub, E. Measurement of the quadriceps (Q) angle with respect to various body parameters in young Arab population. PLoS ONE 2019, 14, e0218387. [Google Scholar] [CrossRef]
- Bhalara, A.; Talsaniya, D.; Nikita, G.N. Q Angle in children population aged between 7 to 12 years. Int. J. Health Sci. Res. 2013, 3, 57–64. [Google Scholar]
- Rajeev, C.; Mudasir, M.; Ammar, A.; Deepak, K.; Sangita, C. Effect of various parameters on quadriceps angle in adult Indian population. J. Clin. Orthop. Trauma 2019, 10, 149–154. [Google Scholar]
- Wilkosz, P.; Kabacinski, J.; Mackala, K.; Murawa, M.; Ostarello, J.; Rzepnicka, A.; Szczesny, L.; Fryzowicz, A.; Maczynski, J.; Dworak, L.B. Isokinetic and Isometric Assessment of the knee joint extensors and flexors of professional volleyball players. Int. J. Environ. Res. Public Health 2021, 18, 6780. [Google Scholar] [CrossRef]
- Zhang, Y.; Su, Q.; Zhang, Y.; Ge, H.; Wei, W.; Cheng, B. Multivariate analysis of the relationship between gluteal muscle contracture and coxa valga. BMC Musculoskelet. Disord. 2021, 22, 561. [Google Scholar] [CrossRef] [PubMed]
- Nienke, E.L.; Sita, M.A.B.; Marienke, M. Factors associated with patellofemoral pain syndrome: A systematic review. Br. J. Sports Med. 2013, 47, 193–206. [Google Scholar]
- Ramírez-delaCruz, M.; Bravo-Sánchez, A.; Esteban-García, P.; Jiménez, F.; Abián-Vicén, J. Effects of plyometric training on lower body muscle architecture, tendon structure, stiffness and physical performance: A systematic review and meta–analysis. Sports Med. Open 2022, 8, 40. [Google Scholar] [CrossRef]
- Lamm, B.M.; Stasko, P.A.; Gesheff, M.G.; Bhave, A. Normal foot and ankle radiographic angles, measurements, and reference points. J. Foot Ankle Surg. 2016, 55, 991–998. [Google Scholar] [CrossRef]
- Bok, S.K.; Lee, H.K.; Kim, B.O.; Ahn, S.Y.; Song, Y.S.; Park, I. The effect of different foot orthosis inverted angles on plantar pressure in children with flexible flat feet. PLoS ONE 2016, 11, e0159831. [Google Scholar] [CrossRef]
- Youn, K.-J.; Ahn, S.-Y.; Kim, B.-O.; Park, I.-S.; Bok, S.-K. Long-term effect of rigid foot orthosis in children older than six years with flexible flat foot. Ann. Rehabil. Med. 2019, 43, 224–229. [Google Scholar] [CrossRef] [PubMed]
- Pauk, J.; Ihnatouski, M.; Najafi, B. Assessing plantar pressure distribution in children with flat foot arch: Application of the Clarke angle. J. Am. Podiatr. Med. Assoc. 2014, 104, 622–632. [Google Scholar] [CrossRef]
- Tourillon, R.; Gojanovic, B.; Fourchet, F. How to evaluate and improve foot strength in athletes: An update. Front. Sports Act. Living 2019, 11, 46. [Google Scholar] [CrossRef] [PubMed]
- Kamalakannan, M.; Priya, S.S.; Swetha, V. Efficacy of Jumping rope for young age students in relation with bilateral flat foot. Biomedicine 2020, 40, 236–240. [Google Scholar]
- Buddecke, D.E.; Polk, M.A.; Barp, E.A. Metatarsal fractures. Clin. Podiatr. Med. Surg. 2010, 27, 601–624. [Google Scholar] [CrossRef] [PubMed]
- Neville, C.; Flemister, A.S.; Houck, J.R. Deep posterior compartment strength and foot kinematics in subjects with stage II posterior tibial tendon dysfunction. Foot Ankle Int. 2010, 31, 302–328. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Ishikawa, H.; Shibuya, T.; Takai, C.; Nomura, Y.; Kobayashi, D.; Abe, A. Changes in radiographic findings and plantar pressure distribution following forefoot reconstructive surgery for patients with rheumatoid arthritis. Mod. Rheumatol. 2020, 30, 967–974. [Google Scholar] [CrossRef]
- Okamura, K.; Fukuda, K.; Oki, S.; Ono, T.; Tanaka, S.; Kanai, S. Effects of plantar intrinsic foot muscle strengthening exercise on static and dynamic foot kinematics: A pilot randomized controlled single-blind trial in individuals with pes planus. Gait Posture 2020, 75, 40–45. [Google Scholar] [CrossRef]
- Morikawa, M.; Maeda, N.; Komiya, M.; Hirota, A.; Mizuta, R.; Kobayashi, T.; Kaneda, K.; Nishikawa, Y.; Urabe, Y. Contribution of plantar fascia and intrinsic foot muscles in a single-leg drop landing and repetitive rebound jumps: An ultrasound-based study. Int. J. Environ. Res. Public Health 2021, 18, 4511. [Google Scholar] [CrossRef]
- Squibb, M.; Sheerin, K.; Francis, P. Measurement of the developing foot in shod and barefoot paediatric populations: A narrative review. Children 2022, 9, 750. [Google Scholar] [CrossRef]
- Riddick, R.; Farris, D.J.; Kelly, L.A. The foot is more than a spring: Human foot muscles perform work to adapt to the energetic requirements of locomotion. J. R. Soc. Interface 2019, 16, 20180680. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.W.; Park, K.B.; Kwak, Y.H.; Jin, S.; Park, H. Radiographic assessment of foot alignment in juvenile hallux valgus and its relationship to flatfoot. Foot. Ankle. Int. 2019, 40, 1079–1086. [Google Scholar] [CrossRef]
- Inarejos Clemente, E.J.; Gómez, M.P.A.; March, J.C.; Restrepo, R. Ankle and foot deformities in children. Semin. Musculoskelet. Radiol. 2023, 27, 367–377. [Google Scholar] [CrossRef]
- Cowley, E.; Marsden, J. The effects of prolonged running on foot posture: A repeated measures study of half marathon runners using the foot posture index and navicular height. J. Foot Ankle Res. 2013, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Jonely, H.; Brismée, J.M.; Sizer, P.S., Jr.; James, C.R. Relationships between clinical measures of static foot posture and plantar pressure during static standing and walking. Clin. Biomech. 2011, 26, 873–879. [Google Scholar] [CrossRef] [PubMed]
- Banu, U.; Emin, U.E.; Eda, A. Effects of short foot exercises on foot posture, pain, disability and plantar pressure in pes planus. J. Sport Rehabil. 2020, 29, 436–440. [Google Scholar]
- Haun, C.; Brown, C.N.; Hannigan, K.; Johnson, S.T. The effects of the short foot exercise on navicular drop: A critically appraised topic. J. Sport Rehabil. 2020, 30, 152–157. [Google Scholar] [CrossRef]
| Sex | GFFT (n = 80) | RST (n = 80) | |||
|---|---|---|---|---|---|
| M | F | M | F | ||
| Variables | 40 | 40 | 37 | 43 | |
| Age (year) | 8.40 ± 1.84 | 7.88 ± 1.54 | 8.14 ± 1.95 | 8.60 ± 2.18 | |
| Height (cm) | 125.93 ± 10.22 | 122.18 ± 9.95 | 126.54 ± 12.90 | 127.44 ± 14.32 | |
| Weight (kg) | 30.30 ± 9.87 | 25.10 ± 6.08 | 28.86 ± 8.52 | 28.00 ± 7.00 | |
| BMI (kg/m2) | 15.43 ± 2.51 | 16.38 ± 2.52 | 17.84 ± 3.57 | 17.03 ± 2.67 | |
| Intensity | RPE | Exercise | ||
|---|---|---|---|---|
| GFFT | RST | |||
| Warm-up | 1–12 weeks 30 reps × 3 sets | 6–9 | Foam rolling exercise | |
| Main Exercise | 1–2 weeks (5 s × 10 reps) × 3 sets | 10–12 | Toe exercise Calf raise Hip cell Hip bridge | Toe exercise Full squat Calf raise Cat and dog core Jump |
| 3–7 weeks 30 reps × 3 sets | Squat Lunge Balance | Forward and backward Jump step (mat and trek) Side jump step (mat and trek) Cross step (mat and trek) Total jump step (mat and trek) | ||
| 8–12 weeks 30 reps × 3 sets | Step box up and down Step box side up and down Step box jumping | One leg forward step Back jump step Turn 180 jump step | ||
| Cool-down | 1–12 weeks 30 reps × 3 sets | 6–9 | Achilles tendon stretching and foam rolling exercise | |
| Variables | Group | Pre Intervention | Post Intervention | F | p | |||
|---|---|---|---|---|---|---|---|---|
| Lower limbs | Q-angle | Lt | GFFT | 6.60 ± 1.53 | 6.53 ± 1.17 | G | 31.876 | 0.000 *** |
| T | 20.973 | 0.000 *** | ||||||
| RST | 6.97 ± 1.52 | 8.22 ± 1.39 ###††† | ||||||
| G × T | 26.538 | 0.000 *** | ||||||
| Rt | GFFT | 6.94 ± 1.45 | 6.48 ± 1.45 † | G | 17.731 | 0.000 *** | ||
| T | 11.534 | 0.000 *** | ||||||
| RST | 6.81 ± 1.37 | 8.12 ± 1.26 ###††† | ||||||
| G × T | 49.582 | 0.000 *** | ||||||
| Arch | CPA | Lt | GFFT | 18.93 ± 1.53 | 19.85 ± 3.31 †† | G | 4.844 | 0.029 * |
| T | 50.327 | 0.000 *** | ||||||
| RST | 19.03 ± 3.48 | 21.62 ± 2.59 ###††† | ||||||
| G × T | 11.394 | 0.001 ** | ||||||
| Rt | GFFT | 19.15 ± 3.45 | 18.54 ± 3.01 † | G | 5.642 | 0.019 * | ||
| T | 17.617 | 0.000 *** | ||||||
| RST | 18.55 ± 3.16 | 21.30 ± 3.56 ###††† | ||||||
| G × T | 43.623 | 0.000 *** | ||||||
| CFMA | Lt | GFFT | 135.56 ± 12.20 | 136.18 ± 5.42 | G | 3.061 | 0.082 | |
| T | 6.203 | 0.014 * | ||||||
| RST | 136.51 ± 6.24 | 131.86 ± 5.90 ###††† | ||||||
| G × T | 10.646 | 0.001 ** | ||||||
| Rt | GFFT | 136.80 ± 6.05 | 136.19 ± 5.53 | G | 8.733 | 0.004 ** | ||
| T | 15.062 | 0.000 *** | ||||||
| RST | 135.77 ± 5.81 | 132.78 ± 4.88 ###††† | ||||||
| G × T | 6.602 | 0.011 * | ||||||
| Navicular–cuboid OR | Lt | GFFT | 67.81 ± 11.70 | 64.17 ± 11.66 † | G | 5.569 | 0.020 * | |
| T | 67.296 | 0.000 *** | ||||||
| RST | 69.48 ± 13.61 | 54.61 ± 13.88 ###††† | ||||||
| G × T | 24.765 | 0.000 *** | ||||||
| Rt | GFFT | 68.00 ± 12.89 | 64.59 ± 10.53 † | G | 8.717 | 0.004 ** | ||
| T | 84.457 | 0.000 *** | ||||||
| RST | 69.02 ± 5.81 | 53.84 ± 12.57 ###††† | ||||||
| G × T | 33.917 | 0.000 *** | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-M.; Min, B.-C.; Cho, B.-C.; Hwang, K.-R.; Kim, M.-K.; Lee, J.-H.; Choi, M.-J.; Kim, H.-H.; Kang, M.-S.; Min, K.-B. Effects of Rhythm Step Training on Foot and Lower Limb Balance in Children and Adolescents with Flat Feet: A Radiographic Analysis. Medicina 2024, 60, 1420. https://doi.org/10.3390/medicina60091420
Park J-M, Min B-C, Cho B-C, Hwang K-R, Kim M-K, Lee J-H, Choi M-J, Kim H-H, Kang M-S, Min K-B. Effects of Rhythm Step Training on Foot and Lower Limb Balance in Children and Adolescents with Flat Feet: A Radiographic Analysis. Medicina. 2024; 60(9):1420. https://doi.org/10.3390/medicina60091420
Chicago/Turabian StylePark, Ji-Myeong, Byung-Cho Min, Byeong-Chae Cho, Kyu-Ri Hwang, Myung-Ki Kim, Jeong-Ha Lee, Min-Jun Choi, Hyeon-Hee Kim, Myung-Sung Kang, and Kyoung-Bin Min. 2024. "Effects of Rhythm Step Training on Foot and Lower Limb Balance in Children and Adolescents with Flat Feet: A Radiographic Analysis" Medicina 60, no. 9: 1420. https://doi.org/10.3390/medicina60091420
APA StylePark, J.-M., Min, B.-C., Cho, B.-C., Hwang, K.-R., Kim, M.-K., Lee, J.-H., Choi, M.-J., Kim, H.-H., Kang, M.-S., & Min, K.-B. (2024). Effects of Rhythm Step Training on Foot and Lower Limb Balance in Children and Adolescents with Flat Feet: A Radiographic Analysis. Medicina, 60(9), 1420. https://doi.org/10.3390/medicina60091420






