Influence of Pain, Risk Factors, and Functional Ability on Physical Activity Levels in Women with Anterior Knee Pain: A Cross-Sectional Study
Abstract
1. Introduction
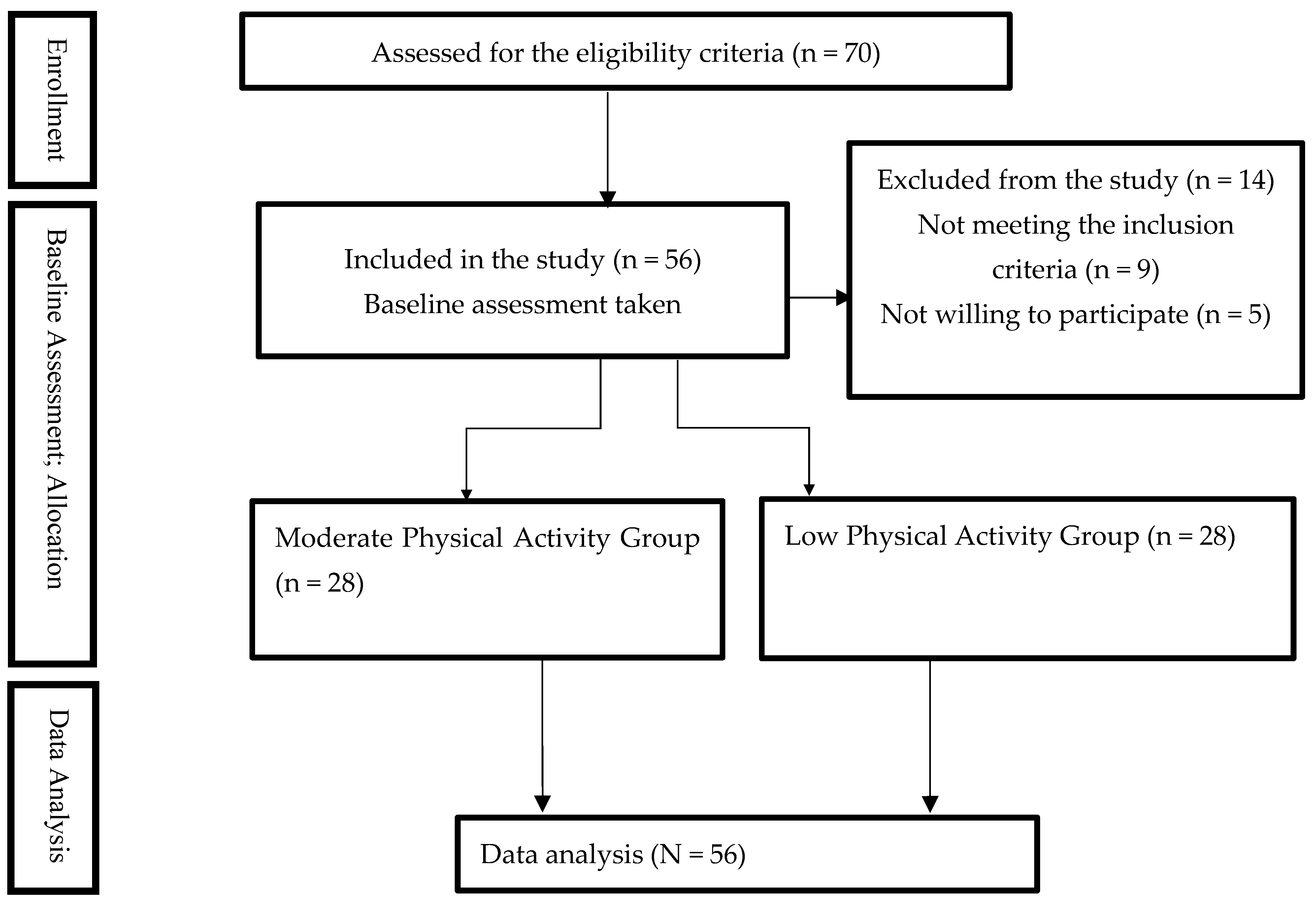
2. Methodology
Study Design
3. Instrumentation
4. Procedures
5. Physical Examination
5.1. Q-Angle
5.2. Patellar Glide Test
5.3. Standard Sit and Reach Test
5.4. Modified Thomas Test
5.5. Step Down
5.6. Double Squat
5.7. Statistical Analysis
6. Results
Between-Group Comparison (Moderate vs. Low Physical Activity)
7. Discussion
7.1. Physical Activity and Level of Pain
7.2. Physical Activity and Functional Abilities
7.3. Physical Activity and Anterior Knee Pain Risk Factors
8. Limitations of the Study
The Implementation of Treatment
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hasan, S.; Alonazi, A.; Anwer, S.; Jamal, A.; Parvez, S.; Alfaiz, F.A.S.; Li, H. Efficacy of patellar taping and electromyographic biofeedback training at various knee angles on quadriceps strength and functional performance in young adult male athletes with patellofemoral pain syndrome: A randomized controlled trial. Pain Res. Manag. 2022, 2022, 8717932. [Google Scholar] [CrossRef]
- Hasan, S. Quadriceps femoris strength training: Effect of neuromuscular electrical stimulation vs isometric exercise in osteoarthritis of knee. Indian J. Physiother. Occup. Ther. 2015, 9, 129. [Google Scholar] [CrossRef]
- Campolo, M.; Babu, J.; Dmochowska, K.; Scariah, S.; Varughese, J. A comparison of two taping techniques (kinesio and mcconnell) and their effect on anterior knee pain during functional activities. Int. J. Sports Phys. Ther. 2013, 8, 105–110. [Google Scholar]
- Borschneck, G.; St John, L.; Brundage, K.; Borschneck, D.P. Cross-Sectional Risk Factors of Anterior Knee Pain in Adolescents. Front. Pain Res. 2021, 2, 720236. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.E.; Selfe, J.; Thacker, D.; Hendrick, P.; Bateman, M.; Moffatt, F.; Rathleff, M.S.; Smith, T.O.; Logan, P. Incidence and prevalence of patellofemoral pain: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0190892. [Google Scholar] [CrossRef] [PubMed]
- Aldharman, S.S.; Almuhammadi, H.H.; Madkhali, A.Y.; Alnami, R.A.; Alkadi, M.A.; Albalawi, D.M.; Alhamaid, Y.A.; Khired, Z.A. Prevalence of Patellofemoral Pain and Knee Pain in the General Population of Saudi Arabia. Cureus 2022, 14, e30355. [Google Scholar] [CrossRef]
- Ramazzina, I.; Pogliacomi, F.; Bertuletti, S.; Costantino, C. Long term effect of selective muscle strengthening in athletes with patellofemoral pain syndrome. Acta Biomed. 2016, 87 (Suppl. S1), 60–68. [Google Scholar]
- Alonazi, A.; Hasan, S.; Anwer, S.; Jamal, A.; Parvez, S.; Alfaiz, F.A.S.; Li, H. Efficacy of electromyographic-biofeedback supplementation training with patellar taping on quadriceps strengthening in patellofemoral pain syndrome among young adult male athletes. Int. J. Environ. Res. Public Health 2021, 18, 4514. [Google Scholar] [CrossRef] [PubMed]
- Briani, R.V.; Pazzinatto, M.F.; Silva, D.D.O.; Azevedo, F.M. Different pain responses to distinct levels of physical activity in women with patellofemoral pain. Braz. J. Phys. Ther. 2017, 21, 138–143. [Google Scholar] [CrossRef]
- Willy, R.W.; Hoglund, L.T.; Barton, C.J.; Bolgla, L.A.; Scalzitti, D.A.; Logerstedt, D.S.; Lynch, A.D.; Snyder-Mackler, L.; McDonough, C.M.; Altman, R.; et al. Patellofemoral pain: Clinical practice guidelines linked to the international classification of functioning, disability and health from the academy of orthopaedic physical therapy of the American physical therapy association. J. Orthop. Sports Phys. Ther. 2019, 49, CPG1–CPG95. [Google Scholar] [CrossRef]
- Glaviano, N.R.; Baellow, A.; Saliba, S. Physical activity levels in individuals with and without patellofemoral pain. Phys. Ther. Sport 2017, 27, 12–16. [Google Scholar] [CrossRef] [PubMed]
- Collins, N.J.; Barton, C.J.; van Middelkoop, M.; Callaghan, M.J.; Rathleff, M.S.; Vicenzino, B.T.; Davis, I.S.; Powers, C.M.; Macri, E.M.; Hart, H.F.; et al. 2018 Consensus statement on exercise therapy and physical interventions (orthoses, taping and manual therapy) to treat patellofemoral pain: Recommendations from the 5th International Patellofemoral Pain Research Retreat, Gold Coast, Australia, 2017. Br. J. Sports Med. 2018, 52, 1170–1178. [Google Scholar] [CrossRef] [PubMed]
- Powers, C.M.; Witvrouw, E.; Davis, I.S.; Crossley, K.M. Evidence-based framework for a pathomechanical model of patellofemoral pain: 2017 patellofemoral pain consensus statement from the 4th International Patellofemoral Pain Research Retreat, Manchester, UK: Part 3. Br. J. Sports Med. 2017, 51, 1713–1723. [Google Scholar] [CrossRef] [PubMed]
- Waryasz, G.R.; McDermott, A.Y. Patellofemoral pain syndrome (PFPS): A systematic review of anatomy and potential risk factors. Dyn. Med. 2008, 7, 1–14. [Google Scholar] [CrossRef]
- Kunene, S.H.; Ramklass, S.; Taukobong, N.P. Anterior knee pain and its extrinsic risk factors among runners in under-resourced communities in Ekurhuleni, Gauteng, South Africa. S. Afr. J. Sports Med. 2019, 31. [Google Scholar] [CrossRef]
- Ferreira, A.S.; Silva, D.d.O.; Del Priore, L.B.; Garcia, C.L.G.; Ducatti, M.H.M.; Botta, A.F.B.; Waiteman, M.C.; de Azevedo, F.M. Differences in pain and function between adolescent athletes and physically active non-athletes with patellofemoral pain. Phys. Ther. Sport 2018, 33, 70–75. [Google Scholar] [CrossRef]
- Gaitonde, D.Y.; Ericksen, A.; Robbins, R.C. Patellofemoral Pain Syndrome. Am. Fam. Physician 2019, 99, 88–94. [Google Scholar]
- Codorean, I.I.; Codorean, I.B. Condition Causing Anterior Knee Pain. In Clinical-MRI Correlations of Anterior Knee Pain: Common and Uncommon Causes; Springer: Berlin/Heidelberg, Germany, 2023; pp. 21–57. [Google Scholar]
- Moyano, F.R.; Valenza, M.C.; Martin, L.M.; Caballero, Y.C.; Gonzalez-Jimenez, E.; Demet, G.V. Effectiveness of different exercises and stretching physiotherapy on pain and movement in patellofemoral pain syndrome: A randomized controlled trial. Clin. Rehabil. 2013, 27, 409–417. [Google Scholar] [CrossRef]
- Rathleff, M.S.; Winiarski, L.; Krommes, K.; Graven-Nielsen, T.; Hölmich, P.; Olesen, J.L.; Holden, S.; Thorborg, K. Pain, sports participation, and physical function in adolescents with patellofemoral pain and Osgood-Schlatter disease: A matched cross-sectional study. J. Orthop. Sports Phys. Ther. 2020, 50, 149–157. [Google Scholar] [CrossRef]
- Thomee, R.; Augustsson, J.; Karlsson, J. Patel-lofemoral pain syndrome: A review of current issues. Sports Med. 1999, 28, 245–262. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: New York, NY, USA, 13 May 2013. [Google Scholar]
- Mulita, F.; Karpetas, G.; Liolis, E.; Vailas, M.; Tchabashvili, L.; Maroulis, I. Comparison of analgesic efficacy of acetaminophen monotherapy versus acetaminophen combinations with either pethidine or parecoxib in patients undergoing laparoscopic cholecystectomy: A randomized prospective study. Med. Glas 2021, 18, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Enciso, I.; Paz-Garcia, J.; Valtierra-Alvarez, J.; Preciado-Ramirez, J.; Almeida-Trinidad, R.; Guzman-Esquivel, J.; Mendoza-Hernandez, M.A.; Garcia-Vega, A.; Soriano-Hernandez, A.D.; Cortes-Bazan, J.L.; et al. A phase I–II controlled randomized trial using a promising novel cell-free formulation for articular cartilage regeneration as treatment of severe osteoarthritis of the knee. Eur. J. Med. Res. 2018, 23, 52. [Google Scholar] [CrossRef] [PubMed]
- Alghadir, A.H.; Anwer, S.; Iqbal, A.; Iqbal, Z.A. Test–retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J. Pain Res. 2018, 11, 851–856. [Google Scholar] [CrossRef]
- Alahmadi, M.A.; Almasoud, K.H.; Aljahani, A.H.; Alzaman, N.S.; Al Nozha, O.M.; Alahmadi, O.M.; Jalloun, R.A.; Alfadhli, E.M.; Alahmadi, J.M.; Zuair, A.A.; et al. Validity and reliability of the Arabic sedentary behavior questionnaire among university students aged between 18–30 years old. BMC Public Health 2023, 23, 128. [Google Scholar] [CrossRef]
- Helou, K.; El Helou, N.; Mahfouz, M.; Mahfouz, Y.; Salameh, P.; Harmouche-Karaki, M. Validity and reliability of an adapted arabic version of the long international physical activity questionnaire. BMC Public Health 2018, 18, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Piva, S.R.; Fitzgerald, G.K.; Irrgang, J.J.; Fritz, J.M.; Wisniewski, S.; McGinty, G.T.; Childs, J.D.; Domenech, M.A.; Jones, S.; Delitto, A. Associates of physical function and pain in patients with patellofemoral pain syndrome. Arch. Phys. Med. Rehabil. 2009, 90, 285–295. [Google Scholar] [CrossRef] [PubMed]
- Khasawneh, R.R.; Allouh, M.Z.; Abu-El-Rub, E. Measurement of the quadriceps (Q) angle with respect to various body parameters in young Arab population. PLoS ONE 2019, 14, e0218387. [Google Scholar] [CrossRef]
- Smith, T.O.; Hunt, N.J.; Donell, S.T. The reliability and validity of the Q-angle: A systematic review. Knee Surgery, Sports Traumatology. Arthroscopy 2008, 16, 1068–1079. [Google Scholar]
- Janssen, J.; Dey, P.; Celik, C.; Richards, J.; Selfe, J. How useful is a single measurement of patellar mobility in the assessment of patients with patellofemoral pain? Physiother. Pract. Res. 2019, 40, 29–35. [Google Scholar] [CrossRef]
- Halabchi, F.; Mazaheri, R.; Seif-Barghi, T. Patellofemoral pain syndrome and modifiable intrinsic risk factors; how to assess and address? Asian J. Sports Med. 2013, 4, 85–100. [Google Scholar] [CrossRef]
- Su, H.; Chang, N.J.; Wu, W.L.; Guo, L.Y.; Chu, I.H. Acute effects of foam rolling, static stretching, and dynamic stretching during warm-ups on muscular flexibility and strength in young adults. J. Sport Rehabilit. 2017, 26, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Wells, K.F.; Dillon, E.K. The sit and reach—A test of back and leg flexibility. Res. Q. Am. Assoc. Health Phys. Educ. Recreat. 1952, 23, 115–118. [Google Scholar]
- Liemohn, W.; Sharpe, G.L.; Wasserman, J.F. Criterion related validity of the sit-and-reach test. J. Strength Cond. Res. 1994, 8, 91–94. [Google Scholar]
- Harvey, D. Assessment of the flexibility of elite athletes using the modified Thomas test. . Br. J. Sports Med. 1998, 32, 68–70. [Google Scholar] [CrossRef]
- Clapis, P.A.; Davis, S.M.; Davis, R.O. Reliability of inclinometer and goniometric measurements of hip extension flexibility using the modified Thomas test. Physiother. Theory Pract. 2008, 24, 135–141. [Google Scholar] [CrossRef]
- Loudon, J.K.; Wiesner, D.; Goist-Foley, H.L.; Asjes, C.; Loudon, K.L. Intrarater Reliability of Functional Performance Tests for Subjects With Patellofemoral Pain Syndrome. J. Athl. Train. 2002, 37, 256–261. [Google Scholar] [PubMed] [PubMed Central]
- Thomeé, R.; Renstrom, P.; Karlsson, J.; Grimby, G. Patellofemoral pain syndrome in young women: I. A clinical analysis of alignment, common symptoms and functional activity level. Scand. J. Med. Sci. Sports 1995, 5, 237–244. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B.; Van Poortvliet, J.A.; Phillips, H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J. Bone Jt. Surg. Br. 1984, 66, 685–693. [Google Scholar] [CrossRef]
- Wojtys, E.M.; Beaman, D.N.; Glover, R.A.; Janda, D. Innervation of the human knee joint by substance-P fibers. Arthroscopy 1990, 6, 254–263. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Roselló-Sastre, E. Immunohistochemical analysis for neural markers of the lateral retinaculum in patients with isolated symptomatic patellofemoral malalignment. A neuroanatomic basis for anterior knee pain in the active young patient. Am. J. Sports Med. 2000, 28, 725–773. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V. Patellofemoral pain. Orthopade 2008, 37, 835–836, 838–840. [Google Scholar] [CrossRef] [PubMed]
- Draper, C.E.; Besier, T.F.; Santos, J.M.; Jennings, F.; Fredericson, M.; Gold, G.E.; Beaupre, G.S.; Delp, S.L. Using real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motion. J. Orthop. Res. 2009, 27, 571–577. [Google Scholar] [CrossRef]
- Keefe, F.J.; Rumble, M.E.; Scipio, C.D.; Giordano, L.A.; Perri, L.M. Psychological aspects of persistent pain: Current state of the science. J. Pain 2004, 5, 195–211. [Google Scholar] [CrossRef] [PubMed]
- King, C.D.; Sibille, K.T.; Goodin, B.R.; Cruz-Almeida, Y.; Glover, T.L.; Bartley, E.; Riley, J.L.; Herbert, M.S.; Sotolongo, A.; Schmidt, J.; et al. Experimental pain sensitivity differs as a function of clinical pain severity in symptomatic knee osteoarthritis. Osteoarthr. Cartil. 2013, 21, 1243–1252. [Google Scholar] [CrossRef]
- Farrokhi, S.; Keyak, J.; Powers, C. Individuals with patellofemoral pain exhibit greater patellofemoral joint stress: A finite element analysis study. Osteoarthr. Cartil. 2011, 19, 287–294. [Google Scholar] [CrossRef]
- Blønd, L.; Hansen, L. Patellofemoral pain syndrome in athletes: A 5.7-year retrospective follow-up study of 250 athletes. Acta Orthop. Belg. 1998, 64, 393–400. [Google Scholar] [PubMed]
- Duffey, M.J.; Martin, D.F.; Cannon, D.W.; Craven, T.; Messier, S.P. Etiologic factors associated with anterior knee pain in distance runners. Med. Sci. Sports Exerc. 2000, 32, 1825–1832. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Beser-Robles, M.; Navarro-Calvo, A.; López-Company, L.; Roselló-Añón, A.; Domenech-Fernández, J. Central sensitization negatively influences the level of disability in female patients with anterior knee pain. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2023, 31, 5381–5387. [Google Scholar] [CrossRef]
- Sigmund, K.J.; Bement, M.K.H.; Earl-Boehm, J.E. Exploring the Pain in Patellofemoral Pain: A Systematic Review and Meta-Analysis Examining Signs of Central Sensitization. J. Athl. Train. 2020, 56, 887–901. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Emami, M.-J.; Ghahramani, M.-H.; Abdinejad, F.; Namazi, H. Q-angle: An invaluable parameter for evaluation of anterior knee pain. Arch. Iran Med. 2007, 10, 24–26. [Google Scholar]
- Caylor, D.; Fites, R.; Worrell, T.W. The relationship between quadriceps angle and anterior knee pain syndrome. J. Orthop. Sports Phys. Ther. 1993, 17, 11–16. [Google Scholar] [CrossRef]
- Boling, M.C.; Padua, D.A.; Marshall, S.W.; Guskiewicz, K.; Pyne, S.; Beutler, A. A prospective investigation of biomechanical risk factors for patellofemoral pain syndrome: The Joint Undertaking to Monitor and Prevent ACL Injury (JUMP-ACL) cohort. Am. J. Sports Med. 2009, 37, 2108–2116. [Google Scholar] [CrossRef] [PubMed]
- Witvrouw, E.; Lysens, R.; Bellemans, J.; Cambier, D.; Vanderstraeten, G. Intrinsic risk factors for the development of anterior knee pain in an athletic population. A two-year prospective study. Am. J. Sports Med. 2000, 28, 480–488. [Google Scholar] [CrossRef] [PubMed]
- Conlan, T.; Garth, W.P., Jr.; Lemons, J.E. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J. Bone Joint Surg. Am. 1993, 75, 682–693. [Google Scholar] [CrossRef] [PubMed]
- Hirokawa, S. Effects of variation on extensor elements and operative procedures in patellofemoral disorders. J. Biomech. 1992, 25, 1393–1401. [Google Scholar] [CrossRef] [PubMed]
- Post, W.R. Patellofemoral pain: Results of nonoperative treatment. Clin. Orthop. Relat. Res. 2005, 436, 55–59. [Google Scholar] [CrossRef]
- Smith, A.D.; Stroud, L.; McQueen, C. Flexibility and anterior knee pain in adolescent elite figure skaters. J. Pediatr. Orthop. 1991, 11, 77–82. [Google Scholar] [CrossRef]
- Kibler, W.B. Strength and flexibility findings in anterior knee pain syndrome in athletes. Am. J. Sports Med. 1987, 15, 20. [Google Scholar]
- Piva, S.R.; Goodnite, E.A.; Childs, J.D. Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. J. Orthop. Sports Phys. Ther. 2005, 35, 793–801. [Google Scholar] [CrossRef]
- Boling, M.; Padua, D.; Marshall, S.; Guskiewicz, K.; Pyne, S.; Beutler, A. Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scand. J. Med. Sci. Sports 2010, 20, 725–730. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Characteristics | Moderate (n = 28) | Low (n = 28) | p-Value (Independent Sample t-Test) | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Age (years) | 31.75 | 6.53 | 30.29 | 5.02 | 0.351 |
| Height (cm) | 158.71 | 6.31 | 158.18 | 4.91 | 0.724 |
| Weight (kg) | 65.54 | 8.80 | 61.75 | 9.88 | 0.136 |
| BMI (kg/m2) | 25.11 | 3.20 | 24.21 | 3.82 | 0.348 |
| Duration of symptoms (week) | 31.75 | 6.53 | 30.29 | 5.02 | 0.033 * |
| Physical activity level(MET∙min∙wk−1) | 685.96 | 51.75 | 505.57 | 43.64 | <0.001 * |
| Previous injury | Number (%) | 0.284 (Chi-square test) | |||
| Yes | 13 (46.4%) | 17 (60.7%) | |||
| No | 15 (53.6%) | 11 (39.3%) | |||
| Location of symptoms | Number (%) | 0.155(Chi-square test) | |||
| Prepatellar | 6 (21.4%) | 9 (32.1%) | |||
| Retro-patellar | 8 (28.6%) | 12 (42.9%) | |||
| Around knee | 14 (50%) | 7 (25.0%) | |||
| Level of Activity | Low | Moderate | T-Value | p-Value (Independent Sample t-Test) |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| VAS | 5.20 ± 1.81 | 6.00 ± 1.19 | 1.97 | 0.040 * |
| Double squat | 12.04 ± 3.9 | 11.75 ± 3.83 | 0.27 | 0.783 |
| Step down | 11.54 ± 3.33 | 10.00 ± 5.16 | 1.32 | 0.191 |
| Q-angle | 12.57 ± 3.73 | 13.54 ± 3.23 | 1.1 | 0.305 |
| Modified Thomas test | 64.79 ± 6.71 | 60.75 ± 9.9 | 1.7 | 0.081 |
| Sit and reach test | 23.73 ± 5.26 | 25.07 ± 7.58 | 0.76 | 0.446 |
| Glide test | 1.45 ± 0.34 | 1.45 ± 0.44 | 0.03 | 0.973 |
| Variables | Correlation with Pain and Functional Ability | |||||
|---|---|---|---|---|---|---|
| Pain | Double Squat | Step Down | ||||
| r-Coefficient | p-Value | r-Coefficient | p-Value | r-Coefficient | p-Value | |
| Q-angle | 0.253 | 0.60 | −0.113 | 0.409 | 0.039 | 0.775 |
| Modified Thomas Test | −0.172 | 0.206 | −0.100 | 0.464 | −0.167 | 0.219 |
| Sit and Reach Test | −0.026 | 0.850 | 0.362 | 0.006 * | 0.179 | 0.186 |
| Glide Test | 0.052 | 0.706 | 0.232 | 0.085 | 0.005 | 0.973 |
| Pain | 1 | - | −0.045 | 0.741 | −0.347 | 0.009 * |
| Correlation | PA-Mod-1 | PA-Mod-2 | PA-Mod-3 | PA-Low-1 | PA-Low-2 | PA-Low-3 |
|---|---|---|---|---|---|---|
| BMI vs. PA level | −0.912 | −0.003 | 0.136 | −0.215 | −0.145 | −0.095 |
| BMI vs. VAS | 0.291 | 0.311 | 0.156 | 0.650 | −0.198 | −0.392 |
| BMI vs. Q-angle | −0.879 | −0.600 | 0.421 | −0.642 | −0.252 | −0.321 |
| PA Level vs. VAS | −0.379 | −0.106 | 0.496 | −0.428 | 0.262 | −0.026 |
| PA Level vs. Q-angle | 0.688 | −0.248 | 0.181 | 0.178 | 0.166 | 0.049 |
| VAS vs. Q-angle | −0.088 | 0.336 | 0.080 | −0.369 | 0.458 | 0.616 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alharbi, A.H.; Seyam, M.K.; Alanazi, A.; Almansour, A.; Hasan, S. Influence of Pain, Risk Factors, and Functional Ability on Physical Activity Levels in Women with Anterior Knee Pain: A Cross-Sectional Study. Medicina 2024, 60, 1467. https://doi.org/10.3390/medicina60091467
Alharbi AH, Seyam MK, Alanazi A, Almansour A, Hasan S. Influence of Pain, Risk Factors, and Functional Ability on Physical Activity Levels in Women with Anterior Knee Pain: A Cross-Sectional Study. Medicina. 2024; 60(9):1467. https://doi.org/10.3390/medicina60091467
Chicago/Turabian StyleAlharbi, Amjad Hajaj, Mohamed K. Seyam, Ahmad Alanazi, Ahmed Almansour, and Shahnaz Hasan. 2024. "Influence of Pain, Risk Factors, and Functional Ability on Physical Activity Levels in Women with Anterior Knee Pain: A Cross-Sectional Study" Medicina 60, no. 9: 1467. https://doi.org/10.3390/medicina60091467
APA StyleAlharbi, A. H., Seyam, M. K., Alanazi, A., Almansour, A., & Hasan, S. (2024). Influence of Pain, Risk Factors, and Functional Ability on Physical Activity Levels in Women with Anterior Knee Pain: A Cross-Sectional Study. Medicina, 60(9), 1467. https://doi.org/10.3390/medicina60091467








