Trends and Impact Factors of Mental Health Service Utilization among Resettled Humanitarian Migrants in Australia: Findings from the BNLA Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Source
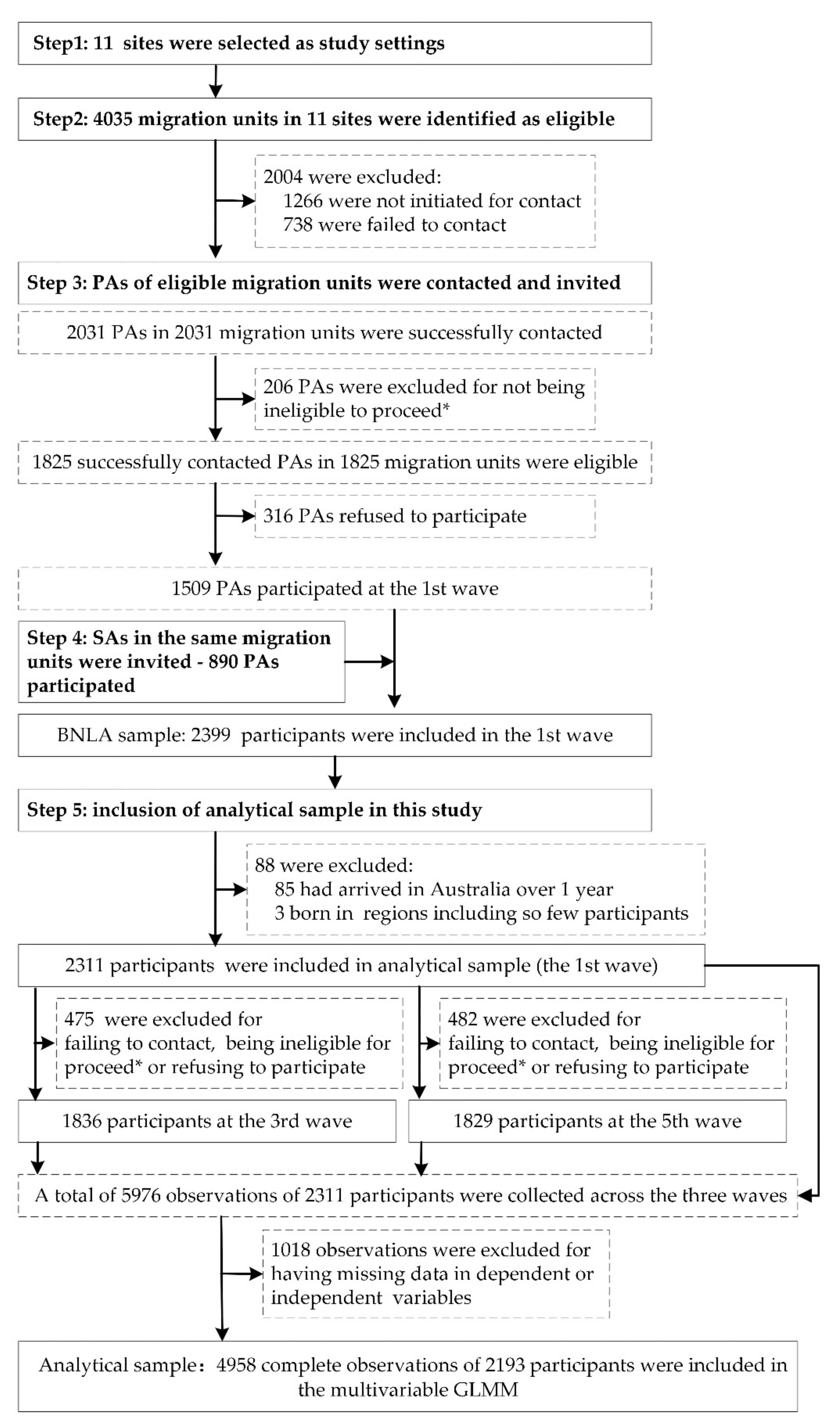
2.2. Participants and Sampling
2.3. Measurements
2.3.1. Outcome Variables: MHS Utilization
2.3.2. Explanatory Variables
2.4. Statistical Analysis
3. Results
3.1. Characteristics of Study Participants
3.2. Trends of the Prevalence of Common Mental Health Conditions among Resettled Humanitarian Migrants
3.3. Trends of the MHS Utilization among Resettled Humanitarian Migrants
3.4. Impact Factors of Having MHS Contacts among Humanitarian Migrants
3.5. Factors Associated with the Frequency of MHS Contacts among Humanitarian Migrants
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations High Commissioner for Refugees. Global Report 2020. Available online: https://www.unhcr.org/flagship-reports/globalreport/ (accessed on 20 August 2021).
- United Nations High Commissioner for Refugees. Solutions. Available online: https://www.unhcr.org/solutions.html?query=repatriation,%20local%20integration%20and%20resettlement (accessed on 15 May 2022).
- Australia Government. Australia’s Offshore Humanitarian Program: 2018–19. Available online: https://www.rda.gov.au/news-and-media/australias-2018-19-humanitarian-program (accessed on 20 August 2021).
- United Nations High Commissioner for Refugees. UNHCR Projected Global Resettlement Needs 2021. Available online: https://reliefweb.int/report/world/unhcr-projected-global-resettlement-needs-2021 (accessed on 11 December 2021).
- Mazumdar, S.; Chong, S.; Eagar, S.; Fletcher-Lartey, S.; Jalaludin, B.; Smith, M. Exploring the Use of Hospital and Community Mental Health Services Among Newly Resettled Refugees. JAMA Netw. Open 2022, 5, e2212449. [Google Scholar] [CrossRef] [PubMed]
- Brijnath, B.; Antoniades, J.; Temple, J. Psychological distress among migrant groups in Australia: Results from the 2015 National Health Survey. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Fogden, G.; Berle, D.; Steel, Z. The Impact of Family Separation and Worry About Family on Psychological Adjustment in Refugees Resettled in Australia. J. Trauma. Stress 2020, 33, 894–907. [Google Scholar] [CrossRef] [PubMed]
- Byrow, Y.; Pajak, R.; Specker, P.; Nickerson, A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: A systematic review. Clin. Psychol. Rev. 2020, 75, 101812. [Google Scholar] [CrossRef]
- Nowak, A.C.; Namer, Y.; Hornberg, C. Health Care for Refugees in Europe: A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 1278. [Google Scholar] [CrossRef]
- Tonui, B.C. The cultural perceptions on mental health and post-resettlement challenges among Rwandan refugees in the U.S. Psychiatry Res. 2022, 313, 114642. [Google Scholar] [CrossRef]
- Kiselev, N.; Pfaltz, M.; Haas, F.; Schick, M.; Kappen, M.; Sijbrandij, M.; De Graaff, A.M.; Bird, M.; Hansen, P.; Ventevogel, P.; et al. Structural and socio-cultural barriers to accessing mental healthcare among Syrian refugees and asylum seekers in Switzerland. Eur. J. Psychotraumatology 2020, 11, 1717825. [Google Scholar] [CrossRef]
- De Montgomery, C.J.; Petersen, J.H.; Jervelund, S.S. Psychiatric healthcare utilisation among refugee adolescents and their peers in Denmark. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 1457–1468. [Google Scholar] [CrossRef]
- Noubani, A.; Diaconu, K.; Ghandour, L.; El Koussa, M.; Loffreda, G.; Saleh, S. A community-based system dynamics approach for understanding factors affecting mental Health and Health seeking behaviors in Beirut and Beqaa regions of Lebanon. Glob. Health 2020, 16, 28. [Google Scholar] [CrossRef]
- Hahn, K.; Steinhäuser, J.; Goetz, K. Equity in Health Care: A Qualitative Study with Refugees, Health Care Professionals, and Administrators in One Region in Germany. Biomed. Res. Int. 2020, 2020, 4647389. [Google Scholar] [CrossRef]
- Jarallah, Y.; Baxter, J. Gender disparities and psychological distress among humanitarian migrants in Australia: A moderating role of migration pathway? Confl. Health 2019, 13, 13. [Google Scholar] [CrossRef]
- Slewa-Younan, S.; Rioseco, P.; Guajardo, M.G.U.; Mond, J. Predictors of professional help-seeking for emotional problems in Afghan and Iraqi refugees in Australia: Findings from the Building a New Life in Australia Database. BMC Public Health 2019, 19, 1485. [Google Scholar] [CrossRef]
- Babatunde-Sowole, O.O.; DiGiacomo, M.; Power, T.; Davidson, P.M.; Jackson, D. Resilience of African migrant women: Implications for mental health practice. Int. J. Ment. Health Nurs. 2020, 29, 92–101. [Google Scholar] [CrossRef]
- Gubi, E.; Sjöqvist, H.; Viksten-Assel, K.; Bäärnhielm, S.; Dalman, C.; Hollander, A.C. Mental health service use among migrant and Swedish-born children and youth: A register-based cohort study of 472,129 individuals in Stockholm. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 161–171. [Google Scholar] [CrossRef]
- Andersen, R.M. National health surveys and the behavioral model of health services use. Med. Care 2008, 46, 647–653. [Google Scholar] [CrossRef]
- Chen, J.I.; Romero, G.D.; Karver, M.S. The relationship of perceived campus culture to mental health help-seeking intentions. J. Couns. Psychol. 2016, 63, 677–684. [Google Scholar] [CrossRef]
- Tanhan, A.; Francisco, V.T. Muslims and mental health concerns: A social ecological model perspective. J. Community Psychol. 2019, 47, 964–978. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Paget, S.; Ostojic, K.; Goldsmith, S.; Nassar, N.; McIntyre, S. Determinants of Hospital-Based Health Service Utilization in Cerebral Palsy: A Systematic Review. Arch. Phys. Med. Rehabil. 2022, 103, 1628–1637. [Google Scholar] [CrossRef]
- Chi, Z.; Han, H. Urban-Rural Differences: The Impact of Social Support on the Use of Multiple Healthcare Services for Older People. Front. Public Health 2022, 10, 851616. [Google Scholar] [CrossRef]
- Seidu, A.A. Using Anderson’s Model of Health Service Utilization to Assess the Use of HIV Testing Services by Sexually Active Men in Ghana. Front. Public Health 2020, 8, 512. [Google Scholar] [CrossRef]
- DeSa, S.; Gebremeskel, A.T.; Yaya, S. Barriers and facilitators to access mental health services among refugee women in high-income countries: Study protocol for a systematic review. Syst. Rev. 2020, 9, 186. [Google Scholar] [CrossRef]
- Deng, M.; Zhai, S.; Ouyang, X.; Liu, Z.; Ross, B. Factors influencing medication adherence among patients with severe mental disorders from the perspective of mental health professionals. BMC Psychiatry 2022, 22, 22. [Google Scholar] [CrossRef]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development. Available online: https://sdgs.un.org/2030agenda (accessed on 15 May 2022).
- Edwards, B.; Smart, D.; De Maio, J.; Silbert, M.; Jenkinson, R. Cohort Profile: Building a New Life in Australia (BNLA): The longitudinal study of humanitarian migrants. Int. J. Epidemiol. 2018, 47, 20–20h. [Google Scholar] [CrossRef]
- Chen, W.; Wu, S.; Ling, L.; Renzaho, A.M.N. Impacts of social integration and loneliness on mental health of humanitarian migrants in Australia: Evidence from a longitudinal study. Aust. N. Z. J. Public Health 2019, 43, 46–55. [Google Scholar] [CrossRef]
- Australian Institute of Family Stusdies. Building a New Life in Australia, BLNA Data User Guide; Release 2.0; Australian Institute of Family Stusdies: Melbourne, Australia, 2019. [Google Scholar]
- Mollica, R.F.; Caspi-Yavin, Y.; Bollini, P.; Truong, T.; Tor, S.; Lavelle, J. The Harvard Trauma Questionnaire. Validating a cross-cultural instrument for measuring torture, trauma, and posttraumatic stress disorder in Indochinese refugees. J. Nerv. Ment. Dis. 1992, 180, 111–116. [Google Scholar] [CrossRef]
- Andersen, T.E.; Hansen, M.; Ravn, S.L.; Seehuus, R.; Nielsen, M.; Vaegter, H.B. Validation of the PTSD-8 Scale in Chronic Pain Patients. Pain Med. 2018, 19, 1365–1372. [Google Scholar] [CrossRef]
- Chen, W.; Hall, B.J.; Ling, L.; Renzaho, A.M. Pre-migration and post-migration factors associated with mental health in humanitarian migrants in Australia and the moderation effect of post-migration stressors: Findings from the first wave data of the BNLA cohort study. Lancet Psychiatry 2017, 4, 218–229. [Google Scholar] [CrossRef]
- Kessler, R.C.; Andrews, G.; Colpe, L.J.; Hiripi, E.; Mroczek, D.K.; Normand, S.L.; Walters, E.E.; Zaslavsky, A.M. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 2002, 32, 959–976. [Google Scholar] [CrossRef]
- Boettcher, V.S.; Nowak, A.C.; Neuner, F. Mental health service utilization and perceived barriers to treatment among adult refugees in Germany. Eur. J. Psychotraumatology 2021, 12, 1910407. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. First Insights from the National Study of Mental Health and Wellbeing, 2020–2021. Available online: https://www.abs.gov.au/articles/first-insights-national-study-mental-health-and-wellbeing-2020-21 (accessed on 15 May 2022).
- Wang, P.S.; Aguilar-Gaxiola, S.; Alonso, J.; Angermeyer, M.C.; Borges, G.; Bromet, E.J.; Bruffaerts, R.; de Girolamo, G.; de Graaf, R.; Gureje, O.; et al. Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO world mental health surveys. Lancet 2007, 370, 841–850. [Google Scholar] [CrossRef]
- Yang, P.Q.; Hwang, S.H. Explaining Immigrant Health Service Utilization: A Theoretical Framework. Sage Open 2016, 6, 1–15. [Google Scholar] [CrossRef]
- Misra, T.; Connolly, A.M.; Klynman, N.; Majeed, A. Addressing mental health needs of asylum seekers and refugees in a London Borough: Developing a service model. Prim. Health Care Res. Dev. 2006, 7, 249–256. [Google Scholar]
- Messi, M.; Mueller, Y.; Haller, D.M.; Zeller, A.; Neuner-Jehle, S.; Streit, S.; Burnand, B.; Herzig, L. A cross-sectional study of Swiss ambulatory care services use by multimorbid patients in primary care in the light of the Andersen model. BMC Fam. Pract. 2020, 21, 150. [Google Scholar] [CrossRef]
- Li, L.; Yang, J.; Zhai, S.; Li, D. Determinants of Differences in Health Service Utilization between Older Rural-to-Urban Migrant Workers and Older Rural Residents: Evidence from a Decomposition Approach. Int. J. Environ. Res. Public Health 2022, 19, 6245. [Google Scholar] [CrossRef]
- Mårtensson, L.; Lytsy, P.; Westerling, R.; Wångdahl, J. Experiences and needs concerning health related information for newly arrived refugees in Sweden. BMC Public Health 2020, 20, 1044. [Google Scholar] [CrossRef]
- Wu, S.; Renzaho, A.M.N.; Brian, J.H.; Shi, L.; Ling, L.; Chen, W. Time-varying associations of pre-migration and post-migration stressors in refugees’ mental health during resettlement: A longitudinal study in Australia. Lancet Psychiatry 2020, 8, 36–47. [Google Scholar] [CrossRef]
- Govindasamy, D.; Ferrari, G.; Maruping, K.; Bodzo, P.; Mathews, C.; Seeley, J. A qualitative enquiry into the meaning and experiences of wellbeing among young people living with and without HIV in KwaZulu-Natal, South Africa. Soc. Sci. Med. 2020, 258, 113103. [Google Scholar] [CrossRef]
- Wali, N.; Georgeou, N.; Renzaho, A. Life Is Pulled Back by Such Things: Intersections between Language Acquisition, Qualifications, Employment and Access to Settlement Services Among Migrants in Western Sydney. J. Intercult. Stud. 2018, 39, 85–101. [Google Scholar] [CrossRef]
- Cheng, Z.M.; Wang, B.Z.; Taksa, L. Labor force participation and employment of humanitarian migrants: Evidence from the building a new life in australia longitudinal data. Macquarie Univ. Fac. Bus. Econ. Res. Pap. 2017, 168, 697–720. [Google Scholar]
- Salami, B.; Salma, J.; Hegadoren, K. Access and utilization of mental health services for immigrants and refugees: Perspectives of immigrant service providers. Int. J. Ment. Health Nurs. 2019, 28, 152–161. [Google Scholar] [CrossRef]
- Byrow, Y.; Pajak, R.; McMahon, T.; Rajouria, A.; Nickerson, A. Barriers to Mental Health Help-Seeking Amongst Refugee Men. Int. J. Environ. Res. Public Health 2019, 16, 2634. [Google Scholar] [CrossRef]


| Variables | Wave 1 (n = 2311) | Wave 3 (n = 1836) | Wave 5 (n = 1829) | p |
|---|---|---|---|---|
| Outcomes | ||||
| Having MHS contacts, No. (%) | 298 (13.0) | 556 (31.0) | 530 (29.4) | <0.001 |
| Frequency of MHS contacts, No. (%) | 0.360 1 | |||
| 1–2 times | NA | 160 (29.6) | 119 (23.8) | |
| 3–5 times | NA | 131 (24.2) | 157 (31.5) | |
| 6–9 times | NA | 97 (17.9) | 82 (16.4) | |
| ≥10 times | NA | 153 (28.3) | 141 (28.3) | |
| Predisposing characteristics | ||||
| Age, mean (SD), year | 35.5 (14.0) | 36.2 (14.3) | 36.1 (14.2) | NA |
| Gender (female), No. (%) | 1065 (46.1) | 869 (47.3) | 867 (47.4) | NA |
| Region of birth, No. (%) | ||||
| North Africa and the Middle East | 1286 (55.7) | 1036 (56.4) | 1079 (59.0) | NA |
| South-East Asia | 134 (5.8) | 104 (5.7) | 98 (5.4) | NA |
| South and Central Asia | 798 (34.5) | 641 (34.9) | 597 (32.6) | NA |
| Sub-Saharan Africa | 93 (4.0) | 55 (3.0) | 55 (3.0) | NA |
| Education level, No. (%) | ||||
| Never attend school | 376 (16.4) | 298 (16.4) | 287 (15.8) | NA |
| ≤6 years of schooling | 470 (20.5) | 398 (21.9) | 390 (21.5) | NA |
| ≥7 years of schooling | 1104 (48.2) | 869 (47.7) | 878 (48.4) | NA |
| Trade or technical qualification beyond school or university degree | 342 (14.9) | 256 (14.1) | 260 (14.3) | NA |
| Enabling resources | ||||
| Employment status (yes), No. (%) | 123 (5.4) | 357 (19.7) | 544 (29.9) | <0.001 |
| Financial hardships, No. (%) | ||||
| 0 | 1277 (58.2) | 984 (54.9) | 1189 (66.4) | <0.001 |
| 1–2 | 672 (30.6) | 527 (29.4) | 431 (24.1) | <0.001 |
| ≥3 | 245 (11.2) | 280 (15.6) | 171 (9.6) | 0.214 |
| Belongingness to the Australian community, No. (%) | ||||
| Hardly ever or never | 177 (8.0) | 66 (3.7) | 98 (5.4) | <0.001 |
| Some of the time | 436 (19.6) | 254 (14.1) | 278 (15.4) | <0.001 |
| Most of the time | 573 (25.7) | 425 (23.6) | 425 (23.5) | 0.088 |
| Always | 1040 (46.7) | 1058 (58.7) | 1008 (55.7) | <0.001 |
| Housing arrangement, No. (%) | ||||
| Temporary | 245 (10.8) | 142 (7.9) | 150 (8.3) | 0.003 |
| Short term lease | 833 (36.7) | 219 (12.2) | 173 (9.5) | <0.001 |
| Long term lease | 1150 (50.7) | 1321 (73.4) | 1224 (67.4) | <0.001 |
| Others | 39 (1.7) | 117 (6.5) | 269 (14.8) | <0.001 |
| Transport difficulty, No. (%) | ||||
| Always | 453 (20.1) | 174 (9.8) | 185 (10.3) | <0.001 |
| Most of the time | 415 (18.4) | 239 (13.5) | 169 (9.4) | <0.001 |
| Some of the time | 841 (37.3) | 701 (39.5) | 530 (29.4) | <0.001 |
| Never | 545 (24.2) | 663 (37.3) | 921 (51.0) | <0.001 |
| Perceived needs | ||||
| Degree of post-migration stress, mean (SD) | 2.6 (2.0) | 2.6 (2.0) | 2.1 (1.8) | <0.001 2 |
| Overall health, mean (SD) | 3.1 (1.3) | 3.1 (1.4) | 3.1 (1.4) | 0.340 2 |
| PTSD (yes), No. (%) | 735 (33.3) | 581 (32.8) | 513 (28.6) | 0.002 |
| HR-SMI (yes), No. (%) | 378 (16.9) | 346 (19.2) | 306 (17.0) | 0.815 |
| Variables | OR (95% CI) | p1 | aOR (95% CI) | p2 |
|---|---|---|---|---|
| Resettlement time | 1.36 (1.30, 1.42) | <0.001 | 1.43 (1.35, 1.52) | <0.001 |
| Predisposing characteristics | ||||
| Age (year) | 1.58 (1.45, 1.73) | <0.001 | 1.16 (1.04, 1.28) | 0.006 |
| Gender (female) | 1.43 (1.20, 1.71) | <0.001 | 0.99 (0.82, 1.19) | 0.903 |
| Region of birth | ||||
| North Africa and the Middle East (ref) | 1.00 | NA | 1.00 | NA |
| South-East Asia | 0.33 (0.21, 0.52) | <0.001 | 0.72 (0.44, 1.17) | 0.185 |
| South and Central Asia | 0.82 (0.68, 1.00) | 0.047 | 1.15 (0.91, 1,45) | 0.243 |
| Sub-Saharan Africa | 1.01 (0.63, 1.63) | 0.959 | 1.57 (0.93, 2.64) | 0.090 |
| Education level | ||||
| Never attended school (ref) | 1.00 | NA | 1.00 | NA |
| ≤6 years of schooling | 0.83 (0.62, 1.10) | 0.193 | 1.09 (0.81, 1.48) | 0.559 |
| ≥7 years of schooling | 0.65 (0.50, 0.83) | 0.001 | 0.96 (0.71, 1.28) | 0.765 |
| Trade or technical qualification beyond school or university degree | 0.65 (0.47, 0.89) | 0.008 | 0.81 (0.57, 1.17) | 0.267 |
| Enabling resources | ||||
| Employment status (yes) | 0.39 (0.31, 0.49) | <0.001 | 0.71 (0.55, 0.92) | 0.010 |
| Financial hardships | ||||
| 0 (ref) | 1.00 | NA | 1.00 | NA |
| 1–2 | 1.47 (1.23, 1.76) | <0.001 | 1.04 (0.85, 1.26) | 0.731 |
| ≥3 | 3.05 (2.42, 3.85) | <0.001 | 1.69 (1.31, 2.18) | <0.001 |
| Belongingness to the Australian community | ||||
| Hardly ever or never (ref) | 1.00 | NA | 1.00 | NA |
| Some of the time | 0.86 (0.60, 1.24) | 0.425 | 1.19 (0.79, 1.78) | 0.407 |
| Most of the time | 0.69 (0.49, 0.99) | 0.044 | 1.14 (0.77, 1.70) | 0.512 |
| Always | 0.75 (0.54, 1.06) | 0.102 | 1.51 (1.03, 2.21) | 0.034 |
| Housing arrangement | ||||
| Temporary (ref) | 1.00 | NA | 1.00 | NA |
| Short term lease | 0.89 (0.65, 1.22) | 0.467 | 0.88 (0.62, 1.25) | 0.468 |
| Long term lease | 0.91 (0.70, 1.20) | 0.510 | 0.92 (0.67, 1.25) | 0.579 |
| Others | 0.75 (0.51, 1.09) | 0.134 | 0.86 (0.57, 1.32) | 0.493 |
| Transport difficulty | ||||
| Always (ref) | 1.00 | NA | 1.00 | NA |
| Most of the time | 0.89 (0.68, 1.17) | 0.412 | 1.10 (0.81, 1.49) | 0.556 |
| Some of the time | 0.56 (0.44, 0.70) | <0.001 | 1.01 (0.78, 1.32) | 0.931 |
| Never | 0.35 (0.28, 0.45) | <0.001 | 0.81 (0.61,1.08) | 0.149 |
| Perceived needs | ||||
| Degree of post-migration stress | 1.22 (1.17, 1.27) | <0.001 | 1.06 (1.01, 1.11) | 0.017 |
| Overall health | 1.75 (1.65, 1.86) | <0.001 | 1.41 (1.31, 1.52) | <0.001 |
| PTSD (yes) | 3.64 (3.09, 4.28) | <0.001 | 2.08 (1.72, 2.52) | <0.001 |
| HR-SMI (yes) | 4.71 (3.92, 5.67) | <0.001 | 1.99 (1.59, 2.49) | <0.001 |
| Variables | OR (95% CI) | p1 | aOR (95% CI) | p2 |
|---|---|---|---|---|
| Predisposing characteristics | ||||
| Age (year) | 1.02 (1.01, 1.04) | <0.001 | 1.00 (0.99, 1.02) | 0.625 |
| Gender (female) | 1.57 (1.14, 2.15) | 0.005 | 1.50 (1.04, 2.16) | 0.032 |
| Education level | ||||
| Never attended school (ref) | 1.00 | NA | 1.00 | NA |
| ≤6 years of schooling | 0.76 (0.52, 1.11) | 0.151 | 0.90 (0.59, 1.40) | 0.651 |
| ≥7 years of schooling | 1.67 (1.18, 2.35) | 0.003 | 1.54 (1.05, 2.26) | 0.029 |
| Trade or technical qualification beyond school or university degree | 1.04 (0.77, 1.40) | 0.790 | 1.07 (0.77, 1.48) | 0.689 |
| Enabling resources | ||||
| Employment status (yes) | 0.40 (0.26, 0.61) | <0.001 | 0.71 (0.43, 1.18) | 0.191 |
| Financial hardships | ||||
| 0 (ref) | 1.00 | NA | 1.00 | NA |
| 1–2 | 1.70 (1.18, 2.46) | 0.005 | 1.28 (0.84, 1.96) | 0.257 |
| ≥3 | 1.49 (0.90, 2.45) | 0.119 | 1.24 (0.70, 2.20) | 0.457 |
| Belongingness to the Australian community | ||||
| Hardly ever or never (ref) | 1.00 | NA | 1.00 | NA |
| Some of the time | 1.16 (0.55, 2.41) | 0.700 | 1.22 (0.53, 2.80) | 0.637 |
| Most of the time | 1.56 (0.76, 3.18) | 0.225 | 1.63 (0.72, 3.70) | 0.240 |
| Always | 1.00 (0.52, 1.94) | 0.994 | 1.30 (0.60, 2.80) | 0.508 |
| Perceived needs | ||||
| Degree of post-migration stress | 1.12 (1.02, 1.22) | 0.014 | 1.03 (0.93, 1.15) | 0.578 |
| Overall health | 1.62 (1.43, 1.84) | <0.001 | 1.45 (1.22, 1.71) | <0.001 |
| PTSD (yes) | 2.66 (1.92, 3.69) | <0.001 | 1.93 (1.33, 2.82) | <0.001 |
| HR-SMI (yes) | 2.54 (1.79, 3.59) | <0.001 | 1.44 (0.94, 2.19) | 0.094 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zheng, M.; Chen, F.; Pan, Y.; Kong, D.; Renzaho, A.M.N.; Sahle, B.W.; Mahumud, R.A.; Ling, L.; Chen, W. Trends and Impact Factors of Mental Health Service Utilization among Resettled Humanitarian Migrants in Australia: Findings from the BNLA Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 10119. https://doi.org/10.3390/ijerph191610119
Zheng M, Chen F, Pan Y, Kong D, Renzaho AMN, Sahle BW, Mahumud RA, Ling L, Chen W. Trends and Impact Factors of Mental Health Service Utilization among Resettled Humanitarian Migrants in Australia: Findings from the BNLA Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(16):10119. https://doi.org/10.3390/ijerph191610119
Chicago/Turabian StyleZheng, Meng, Feng Chen, Yan Pan, Di Kong, Andre M. N. Renzaho, Berhe W. Sahle, Rashidul Alam Mahumud, Li Ling, and Wen Chen. 2022. "Trends and Impact Factors of Mental Health Service Utilization among Resettled Humanitarian Migrants in Australia: Findings from the BNLA Cohort Study" International Journal of Environmental Research and Public Health 19, no. 16: 10119. https://doi.org/10.3390/ijerph191610119






