Obesity and Its Association with Undiagnosed Diabetes Mellitus, High Blood Pressure and Hypercholesterolemia in the Malaysian Adult Population: A National Cross-Sectional Study Using NHMS Data
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Sampling
2.2. Ethical Consideration
2.3. Survey Materials and Data Collection
2.4. Study Variables
2.4.1. Independent Variables
2.4.2. Dependent Variables
2.4.3. Potential Confounders
2.5. Statistical Analyses
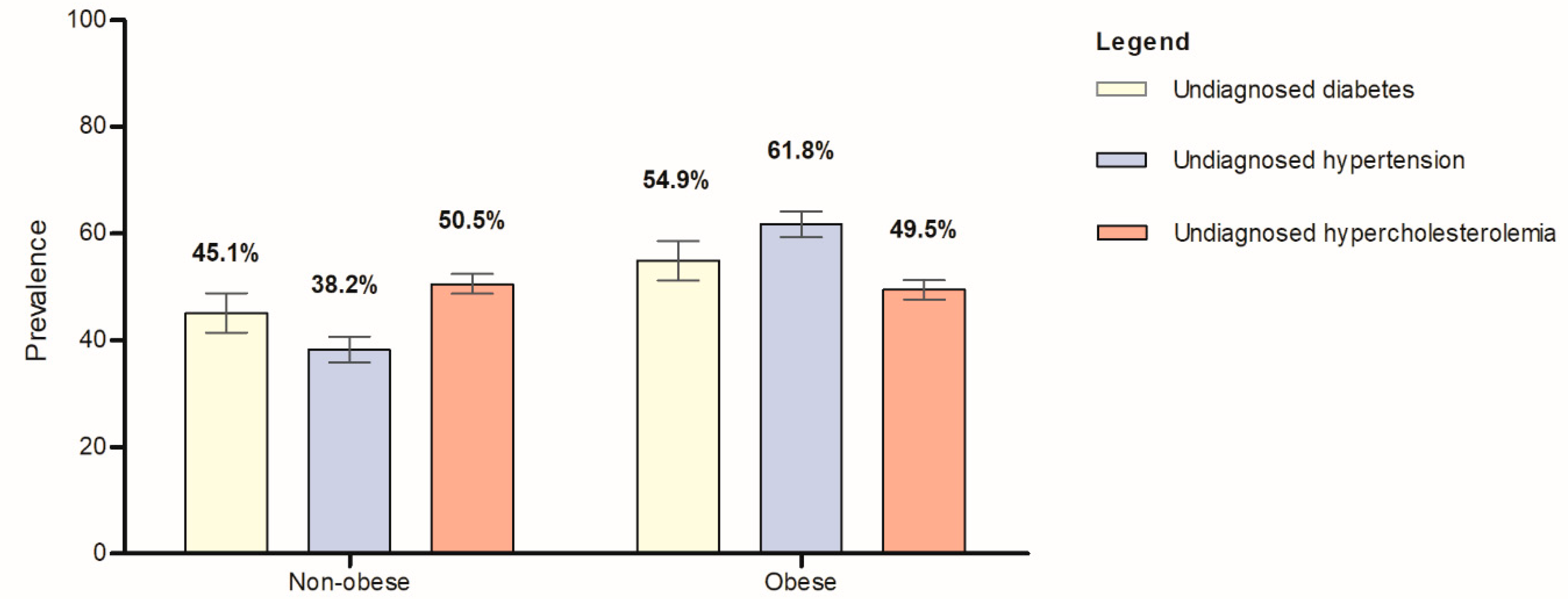
3. Results
4. Discussion
Strengths, Limitations, and Future Recommendations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hruby, A.; Hu, F.B. The Epidemiology of Obesity: A Big Picture. Pharmacoeconomics 2015, 33, 673–689. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, D.; Nóbrega, C.; Manco, L.; Padez, C. The contribution of genetics and environment to obesity. Br. Med. Bull. 2017, 123, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Beltrán-Carrillo, V.J.; Megías, Á.; González-Cutre, D.; Jiménez-Loaisa, A. Elements behind sedentary lifestyles and unhealthy eating habits in individuals with severe obesity. Int. J. Qual. Stud. Health Well-Being 2022, 17, 2056967. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Fact Sheet: Obesity and Overweight; WHO: Geneva, Switzerland, 2021; Available online: http://www.who.int/mediacentre/factsheets/fs311/en/ (accessed on 15 September 2022).
- Mohd-Sidik, S.; Lekhraj, R.; Foo, C. Prevalence, Associated Factors and Psychological Determinants of Obesity among Adults in Selangor, Malaysia. Int. J. Environ. Res. Public Health 2021, 18, 868. [Google Scholar] [CrossRef] [PubMed]
- Institute of Public Health (IPH). National Health and Morbidity Survey (NHMS); Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 1996. [Google Scholar]
- Institute of Public Health (IPH). National Health and Morbidity Survey (NHMS); Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 2019. [Google Scholar]
- Zatońska, K.; Psikus, P.; Basiak-Rasała, A.; Stępnicka, Z.; Gaweł-Dąbrowska, D.; Wołyniec, M.; Gibka, J.; Szuba, A.; Połtyn-Zaradna, K. Obesity and Chosen Non-Communicable Diseases in PURE Poland Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 2701. [Google Scholar] [CrossRef]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Institute of Public Health (IPH). National Health and Morbidity Survey (NHMS); Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 2015. [Google Scholar]
- Sommer, I.; Teufer, B.; Szelag, M.; Nussbaumer-Streit, B.; Titscher, V.; Klerings, I.; Gartlehner, G. The performance of anthropometric tools to determine obesity: A systematic review and meta-analyses. Sci. Rep. 2020, 10, 12699. [Google Scholar] [CrossRef]
- Bhattacharya, A.; Pal, B.; Mukherjee, S.; Roy, S.K. Assessment of nutritional status using anthropometric variables by multivariate analysis. BMC Public Health 2019, 19, 1045. [Google Scholar] [CrossRef]
- Krishnamoorthy, Y.; Rajaa, S.; Murali, S.; Sahoo, J.; Kar, S.S. Association Between Anthropometric Risk Factors and Metabolic Syndrome Among Adults in India: A Systematic Review and Meta-Analysis of Observational Studies. Prev. Chronic Dis. 2022, 19, E24. [Google Scholar] [CrossRef]
- Chen, S.; Chen, Y.; Liu, X.; Li, M.; Wu, B.; Li, Y.; Liang, Y.; Shao, X.; Holthofer, H.; Zou, H. Insulin resistance and metabolic syndrome in normal-weight individuals. Endocrine 2014, 46, 496–504. [Google Scholar] [CrossRef]
- Iacobini, C.; Pugliese, G.; Blasetti Fantauzzi, C.; Federici, M.; Menini, S. Metabolically healthy versus metabolically unhealthy obesity. Metabolism 2019, 92, 51–60. [Google Scholar] [CrossRef]
- Hopps, E.; Noto, D.; Caimi, G.; Averna, M.R. A novel component of the metabolic syndrome: The oxidative stress. Nutr. Metab. Cardiovasc. Dis. 2010, 20, 72–77. [Google Scholar] [CrossRef]
- Kalyan, M.; Dhore, P.; Purandare, V.; Deshpande, S.; Unnikrishnan, A.G. Obesity and its Link to Undiagnosed Diabetes mellitus Mellitus and High blood pressure in Rural Parts of Western India. Indian J. Endocrinol. Metab. 2020, 24, 155–159. [Google Scholar]
- O’Connor, E.A.; Evans, C.V.; Burda, B.U.; Walsh, E.S.; Eder, M.; Lozano, P. Screening for Obesity and Intervention for Weight Management in Children and Adolescents: Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA 2017, 317, 2427–2444. [Google Scholar] [CrossRef]
- Luna, F.; Luyckx, V.A. Why have Non-communicable Diseases been Left Behind? Asian Bioeth. Rev. 2020, 12, 5–25. [Google Scholar] [CrossRef]
- World Health Organization. The Asia-Pacific Perspective: Redefining Obesity and Its Treatment; World Health Organization: Geneva, Switzerland, 2000; Available online: https://apps.who.int/iris/bitstream/handle/10665/206936/0957708211_eng.pdf (accessed on 5 May 2022).
- Ministry of Health Malaysia. Clinical Practice Guidelines: Management of Dyslipidaemia, 5th ed.; Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 2017. Available online: https://www.moh.gov.my/moh/resources/Penerbitan/CPG/CARDIOVASCULAR/4.pdf (accessed on 25 April 2022).
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Himmelfarb, C.D.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. High Blood Press. 2018, 71, 1269–1324. [Google Scholar]
- Zhang, Y.L.; Guo, S.Q.; Ma, W.B.; Wang, J.; Bai, G.Q.; Yang, Q.; Ti, S.F.; Ma, R.; Wei, R.P.; Liu, W.X.; et al. Cut-off points of fasting fingertip capillary blood glucose for detecting both undiagnosed diabetes mellitus and pre-diabetes mellitus. Zhonghua Liu Xing Bing Xue Za Zhi 2010, 31, 1174–1178. [Google Scholar]
- National Coordinating Committee on Food and Nutrition. Malaysian Dietary Guidelines; Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 2020. Available online: https://nutrition.moh.gov.my/MDG2020/mobile/index.html#p=4 (accessed on 25 April 2022).
- International Physical Activity Questionnaire. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ). 2005. Available online: www.ipaq.ki.se (accessed on 25 April 2022).
- Venkatrao, M.; Nagarathna, R.; Majumdar, V.; Patil, S.S.; Rathi, S.; Nagendra, H. Prevalence of Obesity in India and Its Neurological Implications: A Multifactor Analysis of a Nationwide Cross-Sectional Study. Ann. Neurosci. 2020, 27, 153–161. [Google Scholar] [CrossRef]
- Haji Zainuddin, A.A. Prevalence and Socio-demographic Determinant of Overweight and Obesity among Malaysian Adult. Int. J. Public Health Res. 2016, 6, 661–669. [Google Scholar]
- Siddiqui, M.Z.; Donato, R. Overweight and obesity in India: Policy issues from an exploratory multi-level analysis. Health Policy Plan 2016, 31, 582–591. [Google Scholar] [CrossRef]
- Thapa, R.; Dahl, C.; Aung, W.P.; Bjertness, E. Urban-rural differences in overweight and obesity among 25–64 years old Myanmar residents: A cross-sectional, nationwide survey. BMJ Open 2021, 11, e042561. [Google Scholar] [CrossRef] [PubMed]
- Amanzadeh, B.; Sokal-Gutierrez, K.; Barker, J.C. An interpretive study of food, snack and beverage advertisements in rural and urban El Salvador. BMC Public Health 2015, 15, 521. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, T.-H.; Lee, J.J.; Yu, E.W.-R.; Hu, H.-Y.; Lin, S.-Y.; Ho, C.-Y. Association between obesity and education level among the elderly in Taipei, Taiwan between 2013 and 2015: A cross-sectional study. Sci. Rep. 2020, 10, 20285. [Google Scholar] [CrossRef] [PubMed]
- Bertoia, M.L.; Mukamal, K.J.; Cahill, L.; Hou, T.; Ludwig, D.; Mozaffarian, D.; Willett, W.C.; Hu, F.B.; Rimm, E.B. Changes in Intake of Fruits and Vegetables and Weight Change in United States Men and Women Followed for Up to 24 Years: Analysis from Three Prospective Cohort Studies. PLoS Med. 2015, 12, e1001878. [Google Scholar] [CrossRef]
- Hebden, L.; O’Leary, F.; Rangan, A.; Lie, E.S.; Hirani, V.; Allman-Farinelli, M. Fruit consumption and adiposity status in adults: A systematic review of current evidence. Crit. Rev. Food Sci. Nutr. 2017, 57, 2526–2540. [Google Scholar] [CrossRef]
- Nour, M.; Lutze, S.A.; Grech, A.; Allman-Farinelli, M. The Relationship between Vegetable Intake and Weight Outcomes: A Systematic Review of Cohort Studies. Nutrients 2018, 10, 1626. [Google Scholar] [CrossRef]
- Tohill, B.C.; Seymour, J.; Serdula, M.; Kettel-Khan, L.; Rolls, B.J. What epidemiologic studies tell us about the relationship between fruit and vegetable consumption and body weight. Nutr Rev. 2004, 62, 365–374. [Google Scholar] [CrossRef]
- Shi, Z.; Yuan, B.; Hu, G.; Dai, Y.; Zuo, H.; Holmboe-Ottesen, G. Dietary pattern and weight change in a 5-year follow-up among Chinese adults: Results from the Jiangsu Nutrition Study. Br. J. Nutr. 2011, 105, 1047–1054. [Google Scholar] [CrossRef]
- Rautiainen, S.; Wang, L.; Lee, I.-M.; E Manson, J.; E Buring, J.; Sesso, H.D. Higher Intake of Fruit, but Not Vegetables or Fiber, at Baseline Is Associated with Lower Risk of Becoming Overweight or Obese in Middle-Aged and Older Women of Normal BMI at Baseline. J. Nutr. 2015, 145, 960–968. [Google Scholar] [CrossRef]
- Yu, Z.M.; DeClercq, V.; Cui, Y.; Forbes, C.; Grandy, S.; Keats, M.; Parker, L.; Sweeney, E.; Dummer, T.J.B. Fruit and vegetable intake and body adiposity among populations in Eastern Canada: The Atlantic Partnership for Tomorrow’s Health Study. BMJ Open 2018, 8, e018060. [Google Scholar] [CrossRef]
- Sarma, S.; Zaric, G.S.; Campbell, M.K.; Gilliland, J. The effect of physical activity on adult obesity: Evidence from the Canadian NPHS panel. Econ. Hum. Biol. 2014, 14, 1–21. [Google Scholar] [CrossRef]
- Cook, C.M.; Schoeller, D.A. Physical activity and weight control. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 419–424. [Google Scholar] [CrossRef]
- Fang, M.; Wang, D.; Coresh, J.; Selvin, E. Undiagnosed Diabetes mellitus in U.S. Adults: Prevalence and Trends. Diabetes Mellit. Care 2022, 45, 1994–2002. [Google Scholar] [CrossRef]
- Lim, O.W.; Yong, C.C. The Risk Factors for Undiagnosed and Known High blood pressure among Malaysians. Malays J. Med. Sci. 2019, 26, 98–112. [Google Scholar]
- Bushara, S.O.; Noor, S.K.; Elmadhoun, W.M.; Sulaiman, A.A.; Ahmed, M.H. Undiagnosed high blood pressure in a rural community in Sudan and association with some features of the metabolic syndrome: How serious is the situation? Ren Fail. 2015, 37, 1022–1026. [Google Scholar] [CrossRef]
- Al-Goblan, A.S.; A Al-Alfi, M.; Khan, M.Z. Mechanism linking diabetes mellitus and obesity. Diabetes Metab. Syndr. Obes. Targets Ther. 2014, 7, 587–591. [Google Scholar] [CrossRef]
- Li, X.; Xu, J.; Yao, H.; Guo, Y.; Chen, M.; Lu, W. Obesity and overweight prevalence and its association with undiagnosed high blood pressure in Shanghai population, China: A cross-sectional population-based survey. Front. Med. 2012, 6, 322–328. [Google Scholar] [CrossRef]
- Herman, W.H.; Ye, W.; Griffin, S.J.; Simmons, R.K.; Davies, M.J.; Khunti, K.; Rutten, G.E.; Sandbaek, A.; Lauritzen, T.; Borch-Johnsen, K.; et al. Early Detection and Treatment of Type 2 Diabetes mellitus Reduce Cardiovascular Morbidity and Mortality: A Simulation of the Results of the Anglo-Danish-Dutch Study of Intensive Treatment in People with Screen-Detected Diabetes mellitus in Primary Care (ADDITION-Europe). Diabetes Mellit. Care 2015, 38, 1449–1454. [Google Scholar]


| Characteristic | Estimated Population | Count (n) | (%) | 95% CI |
|---|---|---|---|---|
| Sociodemographic | ||||
| Sex | ||||
| Male | 7,349,538 | 6802 | 51.4 | 50.3–52.4 |
| Female | 6,961,477 | 7223 | 48.6 | 47.6–49.7 |
| Age group (years old) | ||||
| 18–29 | 5,618,744 | 4336 | 39.3 | 37.9–40.6 |
| 30–39 | 3,506,540 | 3214 | 24.5 | 23.3–25.8 |
| 40–49 | 2,376,196 | 2567 | 16.6 | 15.7–17.6 |
| 50–59 | 1,614,064 | 2098 | 11.3 | 10.6–12.0 |
| ≥60 | 1,195,471 | 1810 | 8.4 | 7.8–9.0 |
| Ethnicity | ||||
| Malay | 7,820,984 | 9256 | 54.7 | 51.7–57.6 |
| Chinese | 3,644,065 | 2318 | 25.5 | 22.8–28.3 |
| Indian | 968,769 | 972 | 6.8 | 5.8–7.9 |
| Other Bumiputera | 1,665,962 | 1280 | 11.6 | 10.1–13.4 |
| Others | 211,236 | 199 | 1.5 | 1.0–2.1 |
| Residential area | ||||
| Urban | 10,920,733 | 8041 | 76.3 | 75.1–77.5 |
| Rural | 3,390,282 | 5984 | 23.7 | 22.5–24.9 |
| Marital status | ||||
| Single | 4,902,331 | 3703 | 34.3 | 32.9–35.7 |
| Married | 8,646,849 | 9265 | 60.4 | 59.0–61.8 |
| Widow/widower/divorcee | 761,834 | 1057 | 5.3 | 4.9–5.8 |
| Education level | ||||
| No formal education | 514,075 | 675 | 3.6 | 3.2–4.1 |
| Primary | 2,108,803 | 2637 | 14.9 | 14.0–15.8 |
| Secondary | 7,295,664 | 7054 | 51.5 | 50.2–52.9 |
| Tertiary | 4,238,517 | 3543 | 29.9 | 28.4–31.5 |
| Monthly household income | ||||
| B40 | 9,637,764 | 10,051 | 67.3 | 65.3–69.3 |
| M40 | 3,641,622 | 3222 | 25.4 | 23.9–27.1 |
| T20 | 1,031,629 | 752 | 7.2 | 6.0–8.6 |
| Occupation | ||||
| Government | 1,477,554 | 1698 | 12.3 | 11.2–13.5 |
| Private | 5,702,054 | 4518 | 47.5 | 45.9–49.1 |
| Self-employed | 2,625,292 | 2946 | 21.9 | 20.6–23.1 |
| Unpaid/homemaker | 1,902,359 | 2158 | 15.8 | 15.0–16.7 |
| Retiree | 295,486 | 381 | 2.5 | 2.1–2.8 |
| Lifestyle factors | ||||
| General Obesity | ||||
| Underweight | 1,085,293 | 945 | 8.2 | 7.5–8.9 |
| Normal | 4,097,610 | 3722 | 30.9 | 29.8–32.0 |
| Overweight/Obese | 8,075,208 | 8357 | 60.9 | 59.7–62.1 |
| Central adiposity | ||||
| Normal | 7,660,972 | 7056 | 58.1 | 56.7–59.4 |
| Obese | 5,534,879 | 5922 | 41.9 | 40.6–43.3 |
| Alcohol intake | ||||
| Never | 12,205,147 | 12,602 | 85.4 | 83.8–86.9 |
| Ever | 2,084,719 | 1406 | 14.6 | 13.1–16.2 |
| Smoking | ||||
| Never | 10,880,437 | 10,773 | 76.1 | 74.9–77.2 |
| Current | 3,217,163 | 3041 | 22.5 | 21.4–23.6 |
| Former | 206,763 | 205 | 1.4 | 1.2–1.7 |
| Physical activity | ||||
| Inactive | 4,561,762 | 4257 | 32.3 | 31.1–33.5 |
| Active | 9,559,315 | 9582 | 67.7 | 66.5–68.9 |
| Daily fruit and vegetable | ||||
| Inadequate | 13,825,446 | 13,531 | 97.2 | 96.8–97.6 |
| Adequate | 391,066 | 407 | 2.8 | 2.4–3.2 |
| Health status | ||||
| Undiagnosed diabetes mellitus | 1,370,631 | 1567 | 9.6 | 8.8–10.4 |
| Undiagnosed high blood pressure | 2,780,088 | 3276 | 19.4 | 18.5–20.4 |
| Undiagnosed hypercholesterolemia | 6,102,589 | 6554 | 42.6 | 41.3–44.0 |
| Characteristic | Estimated Population | Count (n) | Underweight (n = 945) | Normal (n = 3722) | Overweight/Obese (n = 8357) | p-Value * | |||
|---|---|---|---|---|---|---|---|---|---|
| Prevalence (%) | 95% CI | Prevalence (%) | 95% CI | Prevalence (%) | 95% CI | ||||
| Sociodemographic | |||||||||
| Sex | 0.09 | ||||||||
| Male | 6,913,170 | 6406 | 7.6 | 6.7–8.6 | 30.5 | 28.9–32.1 | 61.9 | 60.2–63.6 | |
| Female | 6,344,941 | 6618 | 8.8 | 7.8–10.0 | 31.4 | 29.8–33.0 | 59.8 | 58.1–61.5 | |
| Age groups (years) | <0.0001 | ||||||||
| 18–29 | 5,191,917 | 3983 | 13.4 | 12.0–14.9 | 37.7 | 35.7–39.6 | 49.0 | 46.9–51.0 | |
| 30–39 | 3,196,043 | 2933 | 5.0 | 4.0–6.1 | 26.9 | 24.8–29.2 | 68.1 | 65.8–70.3 | |
| 40–49 | 2,275,513 | 2465 | 4.4 | 3.3–5.7 | 23.6 | 21.4–25.9 | 72.1 | 69.4–74.6 | |
| 50–59 | 1,513,664 | 1993 | 2.7 | 1.9–3.9 | 26.7 | 24.1–29.4 | 70.6 | 67.8–73.3 | |
| ≥60 | 1,080,974 | 1650 | 8.5 | 6.7–10.7 | 31.6 | 28.8–34.6 | 59.9 | 56.6–63.1 | |
| Ethnicity | <0.0001 | ||||||||
| Malay | 7,235,399 | 8591 | 7.9 | 7.1–8.8 | 29.1 | 27.9–30.3 | 63.0 | 61.6–64.3 | |
| Chinese | 3,311,338 | 2110 | 10.1 | 8.3–12.1 | 37.8 | 35.2–40.6 | 52.1 | 49.1–55.1 | |
| Indian | 903,031 | 906 | 6.2 | 4.1–9.1 | 21.7 | 18.2–25.7 | 72.1 | 67.7–76.2 | |
| Other Bumiputera | 1,603,952 | 1224 | 7.1 | 5.4–9.1 | 29.5 | 26.1–33.0 | 63.5 | 59.6–67.2 | |
| Others | 204,391 | 193 | 4.7 | 2.2–9.8 | 34.8 | 27.0–43.6 | 60.4 | 51.6–68.6 | |
| Residential area | 0.22 | ||||||||
| Urban | 10,068,977 | 7439 | 8.1 | 7.2–9.0 | 30.5 | 29.2–31.8 | 61.4 | 59.9–62.9 | |
| Rural | 3,189,134 | 5585 | 8.5 | 7.5–9.6 | 32.3 | 30.3–34.3 | 59.2 | 57.1–61.3 | |
| Marital status | <0.0001 | ||||||||
| Single | 4,623,681 | 3492 | 14.2 | 12.6–15.9 | 37.9 | 35.8–40.0 | 47.9 | 45.7–50.2 | |
| Married | 7,942,613 | 8565 | 4.9 | 4.3–5.5 | 26.6 | 25.4–27.9 | 68.5 | 67.1–69.8 | |
| Widow/widower/divorcee | 691,817 | 967 | 6.4 | 4.6–8.8 | 33.2 | 29.3–37.3 | 60.4 | 56.3–64.4 | |
| Education level | <0.01 | ||||||||
| No formal education | 448,826 | 598 | 10.8 | 7.9–14.6 | 33.2 | 28.4–38.5 | 56.0 | 50.6–61.3 | |
| Primary | 1,972,388 | 2488 | 5.8 | 4.6–7.2 | 31.4 | 28.8–34.1 | 62.8 | 60.0–65.6 | |
| Secondary | 6,813,524 | 6582 | 9.2 | 8.2–10.4 | 30.2 | 28.7–31.7 | 60.6 | 58.9–62.3 | |
| Tertiary | 3,890,678 | 3258 | 7.3 | 6.2–8.6 | 31.6 | 29.5–33.8 | 61.1 | 58.7–63.4 | |
| Monthly household income | 0.07 | ||||||||
| B40 | 8,938,318 | 9333 | 8.6 | 7.8–9.5 | 31.0 | 29.7–32.3 | 60.5 | 59.0–61.9 | |
| M40 | 3,366,294 | 2990 | 8.1 | 6.8–9.6 | 30.4 | 28.0–32.8 | 61.5 | 58.7–64.3 | |
| T20 | 953,499 | 701 | 4.7 | 3.2–6.8 | 32.3 | 28.2–36.8 | 63.0 | 58.5–67.3 | |
| Occupation | <0.0001 | ||||||||
| Government | 1,379,375 | 1581 | 4.7 | 3.5–6.4 | 23.1 | 20.3–26.3 | 72.1 | 68.8–75.2 | |
| Private | 5,275,335 | 4199 | 7.9 | 6.9–9.1 | 32.6 | 30.6–34.6 | 59.5 | 57.5–61.5 | |
| Self-employed | 2,517,246 | 2827 | 6.2 | 5.1–7.6 | 30.6 | 28.2–33.1 | 63.1 | 60.6–65.6 | |
| Unpaid/homemaker | 1,747,038 | 1979 | 6.1 | 4.6–8.1 | 27.1 | 24.6–29.7 | 66.8 | 63.9–69.6 | |
| Retiree | 277,297 | 360 | 6.5 | 3.8–10.9 | 28.1 | 22.6–34.2 | 65.5 | 59.1–71.3 | |
| Lifestyle factors | |||||||||
| Daily fruit and vegetable intake | 0.04 | ||||||||
| Adequate | 360,253 | 374 | 5.6 | 3.2–9.6 | 25.4 | 20.3–31.3 | 69.0 | 62.8–74.7 | |
| Inadequate | 12,826,531 | 12,584 | 8.2 | 7.5–9.0 | 31.0 | 29.9–32.2 | 60.8 | 59.5–62.1 | |
| Alcohol intake | |||||||||
| Never | 11,295,888 | 11,697 | 8.1 | 7.4–8.9 | 30.5 | 29.4–31.7 | 61.3 | 60.0–62.6 | 0.36 |
| Ever | 1,953,619 | 1316 | 8.5 | 6.5–11.2 | 33.0 | 29.7–36.6 | 58.4 | 54.5–62.2 | |
| Smoking | <0.01 | ||||||||
| Never | 9,988,546 | 9916 | 8.0 | 7.2–8.9 | 30.0 | 28.8–31.3 | 61.9 | 60.6–63.3 | |
| Current | 3,070,519 | 2910 | 8.9 | 7.6–10.4 | 34.2 | 31.8–36.7 | 56.9 | 54.3–59.5 | |
| Former | 197,418 | 195 | 5.0 | 1.7–14.1 | 24.4 | 17.7–32.6 | 70.6 | 61.6–78.3 | |
| Physical activity | <0.0001 | ||||||||
| Inactive | 4,069,283 | 3775 | 10.3 | 9.0–11.8 | 33.1 | 31.1–35.1 | 56.6 | 54.5–58.7 | |
| Active | 9,037,925 | 9096 | 7.2 | 6.4–8.0 | 29.8 | 28.5–31.1 | 63.0 | 61.6–64.5 | |
| Characteristic | Estimated Population | Count (n) | Normal (n = 7056) | Obese (n = 5922) | p-Value * | ||
|---|---|---|---|---|---|---|---|
| Prevalence (%) | 95 % CI | Prevalence (%) | 95 % CI | ||||
| Sociodemographic | |||||||
| Sex | <0.0001 | ||||||
| Male | 6,885,792 | 6389 | 67.5 | 65.8–69.1 | 32.5 | 30.9–34.2 | |
| Female | 6,310,059 | 6589 | 47.8 | 45.9–49.6 | 52.2 | 50.4–54.1 | |
| Age groups (years) | <0.0001 | ||||||
| 18–29 | 5,156,836 | 3953 | 69.5 | 67.5–71.5 | 30.5 | 28.5–32.5 | |
| 30–39 | 3,177,090 | 2923 | 53.3 | 50.8–55.7 | 46.7 | 44.3–49.2 | |
| 40–49 | 2,268,503 | 2460 | 49.9 | 47.1–52.7 | 50.1 | 47.3–52.9 | |
| 50–59 | 1,513,532 | 1993 | 46.5 | 43.4–49.7 | 53.5 | 50.3- 56.6 | |
| ≥60 | 1,079,889 | 1649 | 50.7 | 47.3–54.1 | 49.3 | 45.9–52.7 | |
| Ethnicity | <0.0001 | ||||||
| Malay | 7,205,534 | 8562 | 57.8 | 56.3–59.4 | 42.2 | 40.6–43.7 | |
| Chinese | 3,276,382 | 2094 | 63.5 | 60.5–66.5 | 36.5 | 33.5–39.5 | |
| Indian | 904,374 | 907 | 40.3 | 35.6–45.2 | 59.7 | 54.8–64.4 | |
| Other Bumiputera | 1,603,998 | 1223 | 56.9 | 53.2–60.6 | 43.1 | 39.4–46.8 | |
| Others | 205,563 | 192 | 66.1 | 54.0–76.4 | 33.9 | 23.6–46.0 | |
| Residential area | 0.20 | ||||||
| Urban | 10,014,803 | 7408 | 57.6 | 56.0–59.3 | 42.4 | 40.7–44.0 | |
| Rural | 3,181,048 | 5570 | 59.4 | 57.2–61.5 | 40.6 | 38.5–42.8 | |
| Marital status | <0.0001 | ||||||
| Single | 4,588,325 | 3464 | 70.6 | 68.6–72.6 | 29.4 | 27.4–31.4 | |
| Married | 7,915,725 | 8547 | 51.8 | 50.2–53.4 | 48.2 | 46.6–49.8 | |
| Widow/widower/divorcee | 691,800 | 967 | 46.6 | 42.5–50.8 | 53.4 | 49.2–57.5 | |
| Education level | <0.01 | ||||||
| No formal education | 449,409 | 598 | 53.7 | 48.5–58.9 | 46.3 | 41.1–51.5 | |
| Primary | 1,966,809 | 2482 | 53.2 | 50.4–55.9 | 46.8 | 44.1–49.6 | |
| Secondary | 6,785,169 | 6560 | 58.9 | 57.2–60.6 | 41.1 | 39.4–42.8 | |
| Tertiary | 3,865,710 | 3243 | 59.2 | 56.9–61.5 | 40.8 | 38.5–43.1 | |
| Monthly household income | 0.72 | ||||||
| B40 | 8,911,796 | 9312 | 57.9 | 56.4–59.5 | 42.1 | 40.5–43.6 | |
| M40 | 3,352,715 | 2976 | 58.8 | 56.1–61.5 | 41.2 | 38.5–43.9 | |
| T20 | 931,340 | 690 | 56.6 | 51.5–61.6 | 43.4 | 38.4–48.5 | |
| Occupation | <0.0001 | ||||||
| Government | 1,376,088 | 1578 | 51.4 | 48.0–54.7 | 48.6 | 45.3–52.0 | |
| Private | 5,237,209 | 4174 | 62.3 | 60.3–64.2 | 37.7 | 35.8–39.7 | |
| Self-employed | 2,509,444 | 2819 | 60.0 | 57.4–62.5 | 40.0 | 37.5–42.6 | |
| Unpaid/homemaker | 1,746,749 | 1978 | 41.0 | 38.0–44.0 | 59.0 | 56.0–62.0 | |
| Retiree | 280,248 | 362 | 52.3 | 45.5–59.1 | 47.7 | 40.9–54.5 | |
| Lifestyle factors | |||||||
| Daily fruit and vegetable intake | <0.01 | ||||||
| Adequate | 355,074 | 368 | 48.7 | 42.6–54.9 | 51.3 | 45.1–57.4 | |
| Inadequate | 12,771,069 | 12,545 | 58.3 | 56.9–59.6 | 41.7 | 40.4–43.1 | |
| Alcohol intake | <0.01 | ||||||
| Never | 11,241,642 | 11,656 | 57.3 | 55.9–58.7 | 42.7 | 41.3–44.1 | |
| Ever | 1,945,606 | 1311 | 62.5 | 59.0–65.8 | 37.5 | 34.2–41.0 | |
| Smoking | <0.0001 | ||||||
| Never | 9,933,316 | 9880 | 54.2 | 52.6–55.8 | 45.8 | 44.2–47.4 | |
| Current | 3,063,489 | 2900 | 70.3 | 68.0–72.6 | 29.7 | 27.4–32.0 | |
| Former | 197,418 | 195 | 61.8 | 53.2–69.8 | 38.2 | 30.2–46.8 | |
| Physical activity | 0.53 | ||||||
| Inactive | 4,060,179 | 3766 | 58.5 | 56.3–60.7 | 41.5 | 39.3–43.7 | |
| Active | 8,989,194 | 9063 | 57.7 | 56.2–59.3 | 42.3 | 40.7–43.8 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koo, H.C.; Tan, L.K.; Lim, G.P.; Kee, C.C.; Omar, M.A. Obesity and Its Association with Undiagnosed Diabetes Mellitus, High Blood Pressure and Hypercholesterolemia in the Malaysian Adult Population: A National Cross-Sectional Study Using NHMS Data. Int. J. Environ. Res. Public Health 2023, 20, 3058. https://doi.org/10.3390/ijerph20043058
Koo HC, Tan LK, Lim GP, Kee CC, Omar MA. Obesity and Its Association with Undiagnosed Diabetes Mellitus, High Blood Pressure and Hypercholesterolemia in the Malaysian Adult Population: A National Cross-Sectional Study Using NHMS Data. International Journal of Environmental Research and Public Health. 2023; 20(4):3058. https://doi.org/10.3390/ijerph20043058
Chicago/Turabian StyleKoo, Hui Chin, Lay Kim Tan, Geok Pei Lim, Chee Cheong Kee, and Mohd Azahadi Omar. 2023. "Obesity and Its Association with Undiagnosed Diabetes Mellitus, High Blood Pressure and Hypercholesterolemia in the Malaysian Adult Population: A National Cross-Sectional Study Using NHMS Data" International Journal of Environmental Research and Public Health 20, no. 4: 3058. https://doi.org/10.3390/ijerph20043058








