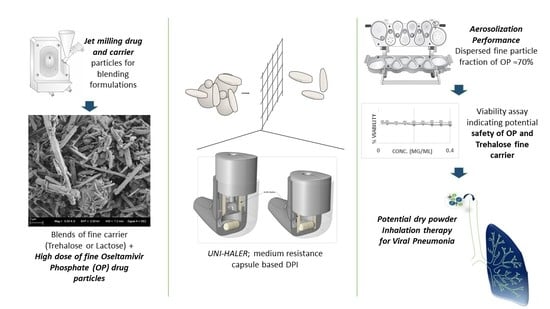
Development of High Dose Oseltamivir Phosphate Dry Powder for Inhalation Therapy in Viral Pneumonia
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Powder Preparation
2.2.1. Micronization
2.2.2. Milling
2.2.3. Particle-Size Distribution
2.2.4. Blending OP with Different Excipients
2.2.5. UV-Spectrophotometric Quantification
2.3. Trehalose Physicochemical Properties
2.3.1. X-ray Powder Diffraction
2.3.2. Specific Surface Area
2.3.3. Fluidization energy
2.3.4. Scanning Electron Microscope
2.4. Aerosolization Performance of OP/Diluent Blends
2.5. MTT Assay for Cytotoxicity Testing on Bronchial Adenocarcinoma Cells
3. Results and Discussion
3.1. Prepared Powder Particles
3.2. Effect of Micronization on Trehalose Physicochemical Characteristics
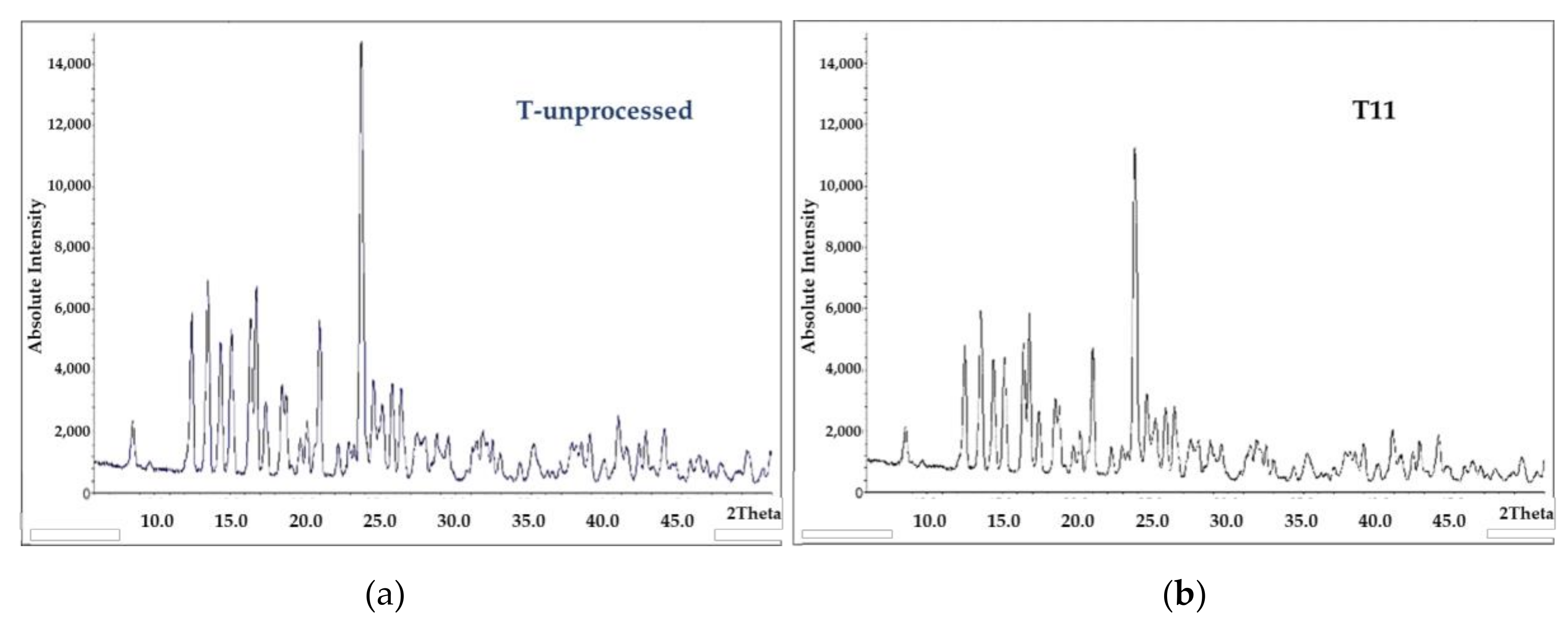
3.2.1. Micronized Trehalose Crystalline Structure
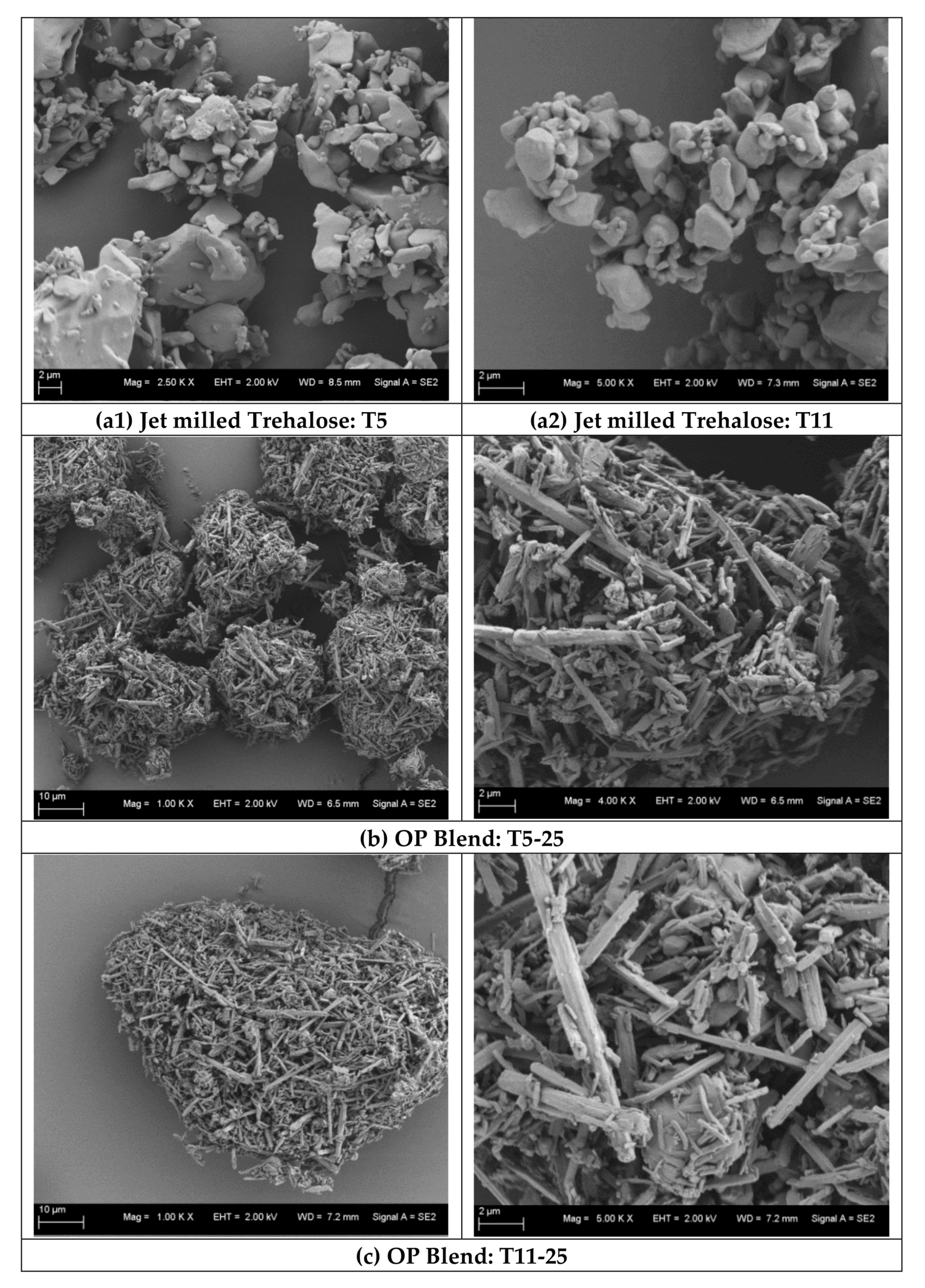
3.2.2. Micronized Trehalose Morphology and Orientation within Blends
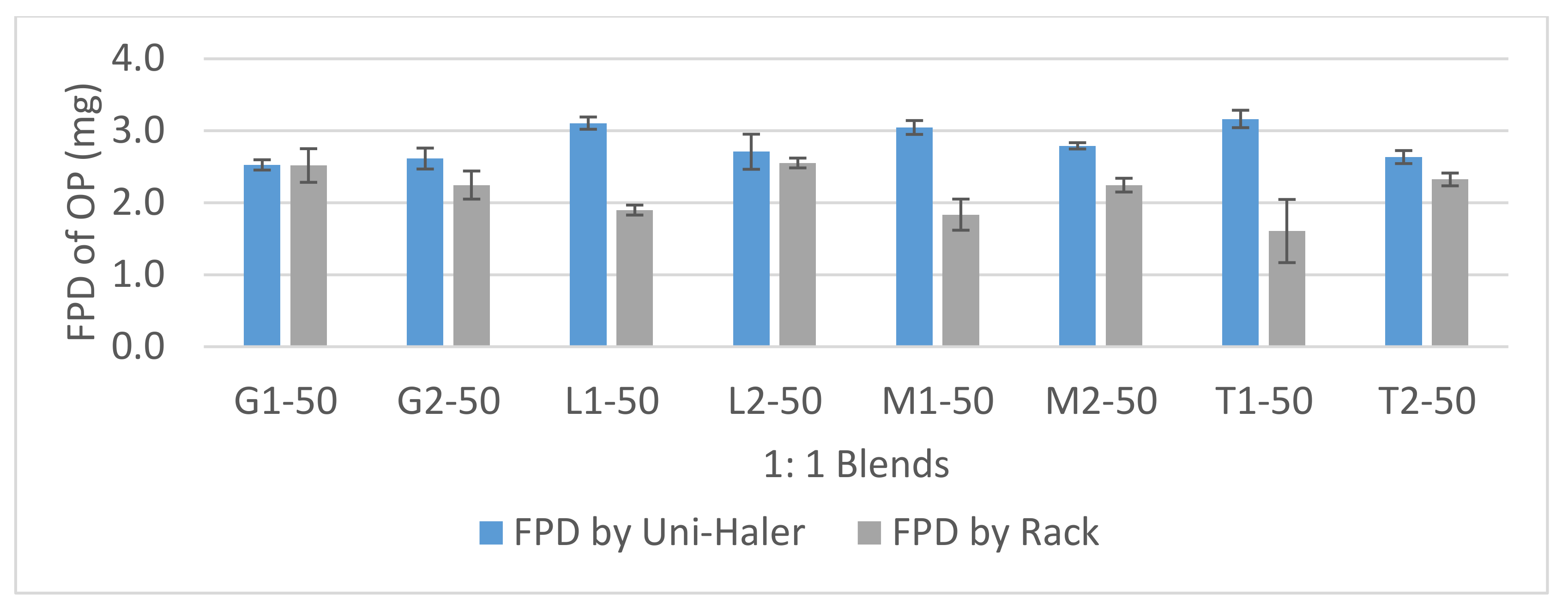
3.3. Aerosolization Performance of 1:1 Formulations
3.4. Aerosolization Performance of OP/Trehalose Formulations
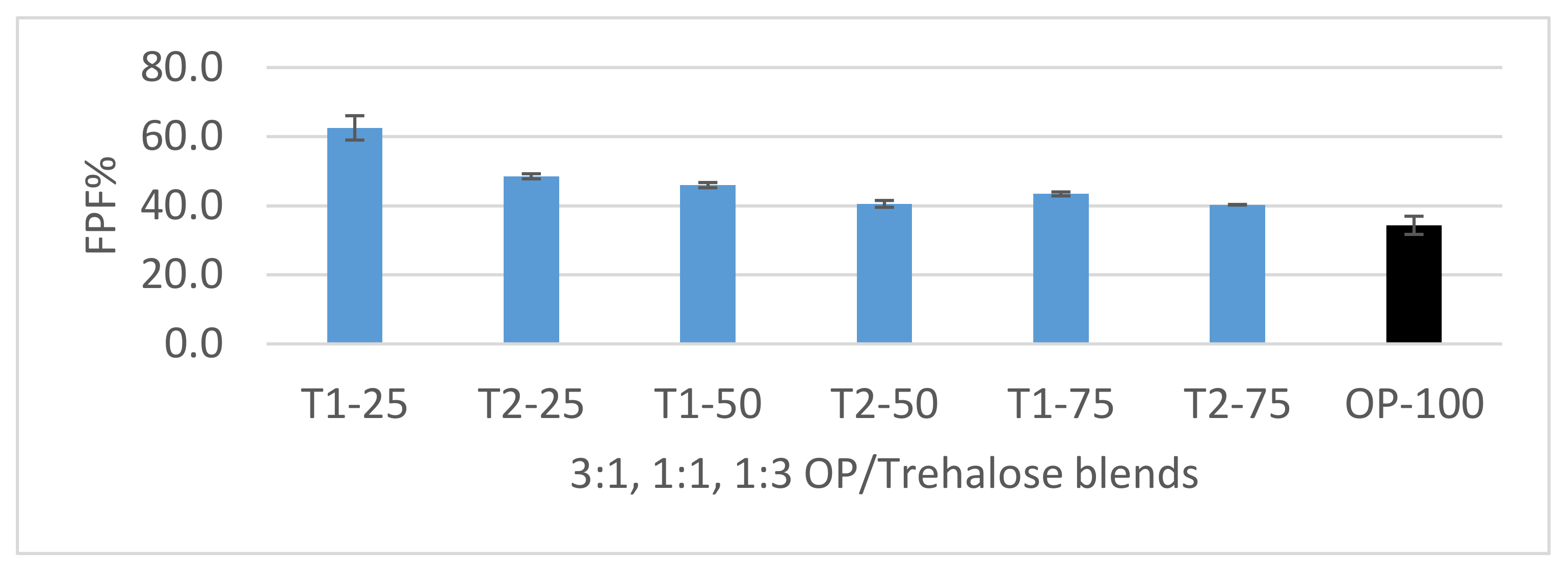
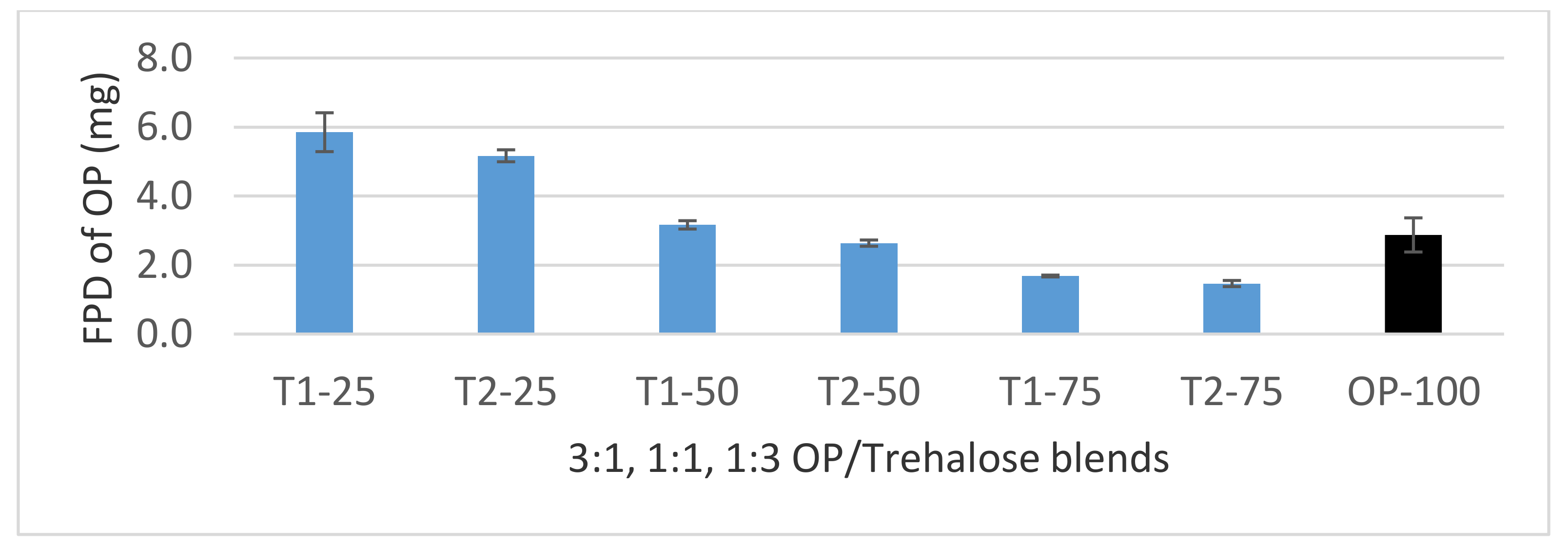
3.4.1. Dispersion of 3:1, 1:1, and 1:3 OP/Trehalose Formulations
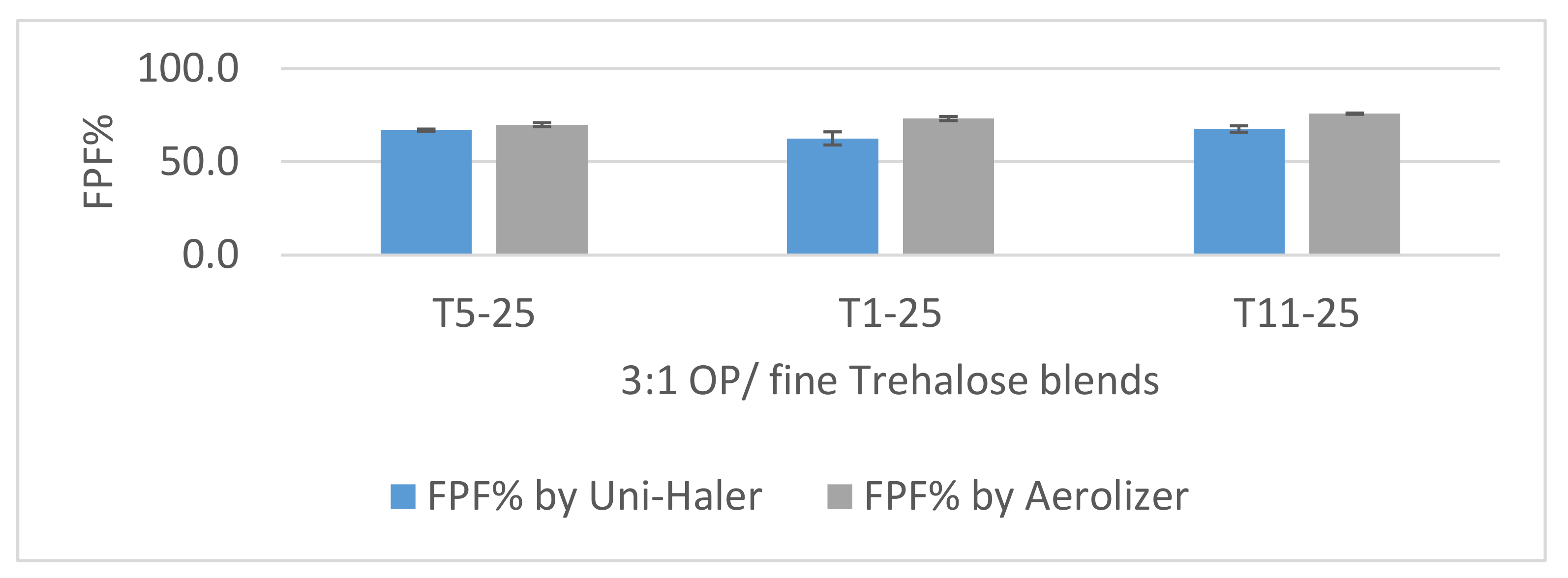
3.4.2. Dispersion of 3:1 OP/Fine Trehalose Formulations
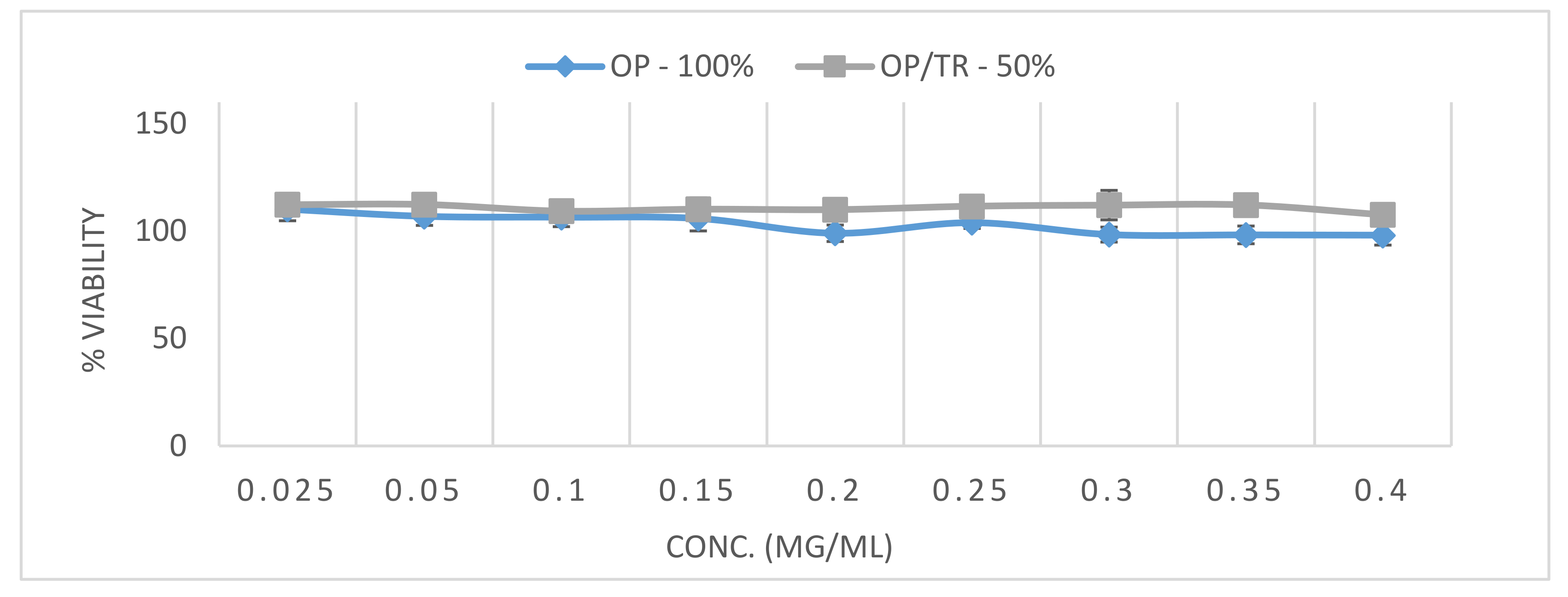
3.5. Cytotoxicity on Bronchial Adenocarcinoma Cells
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Brunaugh:, A.D.; Smyth, H.D.C. Formulation techniques for high dose dry powders. Int. J. Pharm. 2018, 547, 489–498. [Google Scholar] [CrossRef]
- Rubin, B.K.; Williams, R.W. Emerging aerosol drug delivery strategies: From bench to clinic. Adv. Drug Deliv. Rev. 2014, 75, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Rahimpour, Y.; Kouhsoltani, M.; Hamishehkar, H. Alternative carriers in dry powder inhaler formulations. Drug Discov. Today 2014, 19, 618–626. [Google Scholar] [CrossRef] [PubMed]
- Geller, D.E. Comparing clinical features of the nebulizer, metered-dose inhaler, and dry powder inhaler. Respir. Care 2005, 50, 1313. [Google Scholar] [PubMed]
- Telko, M.J.; Hickey, A.J. Dry powder inhaler formulation. Respir. Care 2005, 50, 1209–1227. [Google Scholar]
- Traini, D.; Young, P.M.; Jones, M.; Edge, S.; Price, R. Comparative study of erythritol and lactose monohydrate as carriers for inhalation: Atomic force microscopy and in vitro correlation. Eur. J. Pharm. Sci. 2006, 27, 243–251. [Google Scholar] [CrossRef]
- Andrade, F.; Rafael, D.; Videira, M.; Ferreira, D.; Sosnik, A.; Sarmento, B. Nanotechnology and pulmonary delivery to overcome resistance in infectious diseases. Adv. Drug Deliv. Rev. 2013, 65, 1816–1827. [Google Scholar] [CrossRef]
- Zhou, Q.T.; Armstrong, B.; Larson, I.; Stewart, P.J.; Morton, D.A. Understanding the influence of powder flowability, fluidization and de-agglomeration characteristics on the aerosolization of pharmaceutical model powders. Eur. J. Pharm. Sci. 2010, 40, 412–421. [Google Scholar] [CrossRef]
- Gradon, L.; Sosnowski, T.R. Formation of particles for dry powder inhalers. Adv. Powder Technol. 2014, 25, 43–55. [Google Scholar] [CrossRef]
- Pilcer, G.; Amighi, K. Formulation strategy and use of excipients in pulmonary drug delivery. Int. J. Pharm. 2010, 392, 1–19. [Google Scholar] [CrossRef]
- Florence, A.T.; Siepmann, J. Modern Pharmaceutics, 5th ed.; Informa Healthcare: New York, NY, USA; London, UK, 2009; ISBN 1420065645. [Google Scholar]
- Prime, D. Review of dry powder inhalers. Adv. Drug Deliv. Rev. 1997, 26, 51–58. [Google Scholar] [CrossRef]
- Tee, S.K.; Marriott, C.; Zeng, X.M.; Martin, G.P. The use of different sugars as fine and coarse carriers for aerosolised salbutamol sulphate. Int. J. Pharm. 2000, 208, 111–123. [Google Scholar] [CrossRef]
- Steckel, H.; Bolzen, N. Alternative sugars as potential carriers for dry powder inhalations. Int. J. Pharm. 2004, 270, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Sibum, I.; Hagedoorn, P.; de Boer, A.H.; Frijlink, H.W.; Grasmeijer, F. Challenges for pulmonary delivery of high powder doses. Int. J. Pharm. 2018, 548, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Leung, S.S.Y.; Tang, P.; Parumasivam, T.; Loh, Z.H.; Chan, H.K. Inhaled formulations and pulmonary drug delivery systems for respiratory infections. Adv. Drug Deliv. Rev. 2015, 85, 83–99. [Google Scholar] [CrossRef]
- Chvatal, A.; Farkas, Á.; Balásházy, I.; Szaborevesz, P.; Ambrus, R. Aerodynamic properties and in silico deposition of meloxicam potassium incorporated in a carrier-free DPI pulmonary system. Int. J. Pharm. 2017, 520, 70–78. [Google Scholar] [CrossRef]
- Hoppentocht, M.; Hagedoorn, P.; Frijlink, H.; de Boer, A. Technological and practical challenges of dry powder inhalers and formulations. Adv. Drug Deliv. Rev. 2014, 75, 18–31. [Google Scholar] [CrossRef] [Green Version]
- Islam, N.; Cleary, M.J. Developing an efficient and reliable dry powder inhaler for pulmonary drug delivery—A review for multidisciplinary researchers. Med Eng. Phys. 2012, 34, 409–427. [Google Scholar] [CrossRef]
- Englund, J.A. Antiviral therapy of influenza. Semin. Pediatr. Infect. Dis. 2002, 13, 120–128. [Google Scholar] [CrossRef]
- Dreitlein, W.B.; Maratos, J.; Brocavich, J. Zanamivir and oseltamivir: Two new options for the treatment and prevention of influenza. Clin. Ther. 2001, 23, 327–355. [Google Scholar] [CrossRef]
- Oxford, J.S.; Lambkin, R.; Lambkin-Williams, R. Targeting influenza virus neuraminidase—A new strategy for antiviral therapy. Drug Discov. Today 1998, 3, 448–456. [Google Scholar] [CrossRef]
- Lindemann, L.; Jacobsen, H.; Schuhbauer, D.; Knoflach, F.; Gatti, S.; Wettstein, J.G.; Loetscher, H.; Chu, T.; Ebeling, M.; Paulson, J.C.; et al. In vitro pharmacological selectivity profile of oseltamivir prodrug (Tamiflu) and active metabolite. Eur. J. Pharmacol. 2009, 628, 6–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lotfi, M.; Hamblin, M.R.; Rezaei, N. COVID-19: Transmission, prevention, and potential therapeutic opportunities. Clin. Chim. Acta 2020, 508, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus&ndash Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061. [Google Scholar] [CrossRef]
- Hu, F.; Yin, G.; Chen, Y.; Song, J.; Ye, M.; Liu, J.; Chen, C.; Song, Y.; Tang, X.; Zhang, Y. Corticosteroid, oseltamivir and delayed admission are independent risk factors for prolonged viral shedding in patients with Coronavirus Disease 2019. Clin. Respir. J. 2020, 14, 1067–1075. [Google Scholar] [CrossRef]
- Tobaiqy, M.; Qashqary, M.; Al-Dahery, S.; Mujallad, A.; Hershan, A.; Kamal, M.; Helmi, N. Therapeutic management of patients with COVID-19: A systematic review. Infect. Prev. Pr. 2020, 2, 100061. [Google Scholar] [CrossRef]
- Beigel, J.H.; Bray, M. Current and future antiviral therapy of severe seasonal and avian influenza. Antivir. Res. 2008, 78, 91–102. [Google Scholar] [CrossRef]
- Claus, S.; Weiler, C.; Schiewe, J.; Friess, W. How can we bring high drug doses to the lung? Eur. J. Pharm. Biopharm. 2014, 86, 1–6. [Google Scholar] [CrossRef]
- Hosokawa, M. Structure and Catalytic Properties of Carboxylesterase Isozymes Involved in Metabolic Activation of Prodrugs. Molecules 2008, 13, 412–431. [Google Scholar] [CrossRef] [Green Version]
- Tang, Y.; Zhang, H.; Lu, X.; Jiang, L.; Xi, X.; Liu, J.; Zhu, J. Development and evaluation of a dry powder formulation of liposome-encapsulated oseltamivir phosphate for inhalation. Drug Deliv. 2015, 22, 608–618. [Google Scholar] [CrossRef]
- Sahastrabudhe, H.; Kenjale, P.; Pokharkar, V. Development of sustained release Oseltamivir phosphate dry powder inhaler: In-vitro and in-vivo Toxicological Studies. Curr. Drug Deliv. 2020, 17, 1–11. [Google Scholar] [CrossRef] [PubMed]
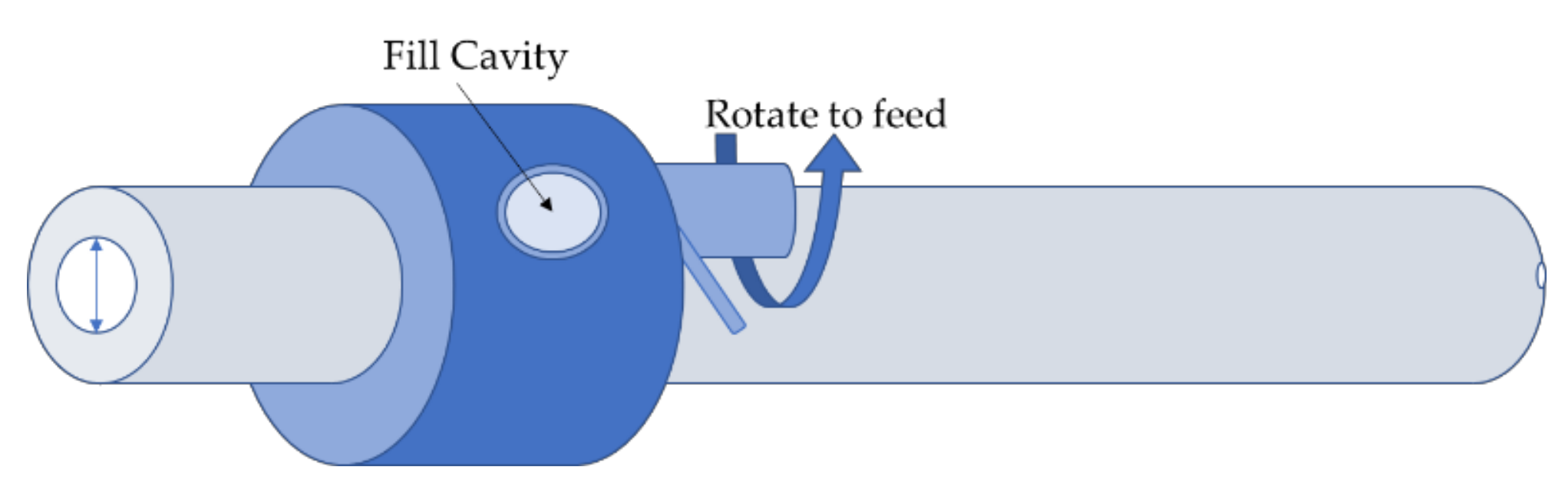
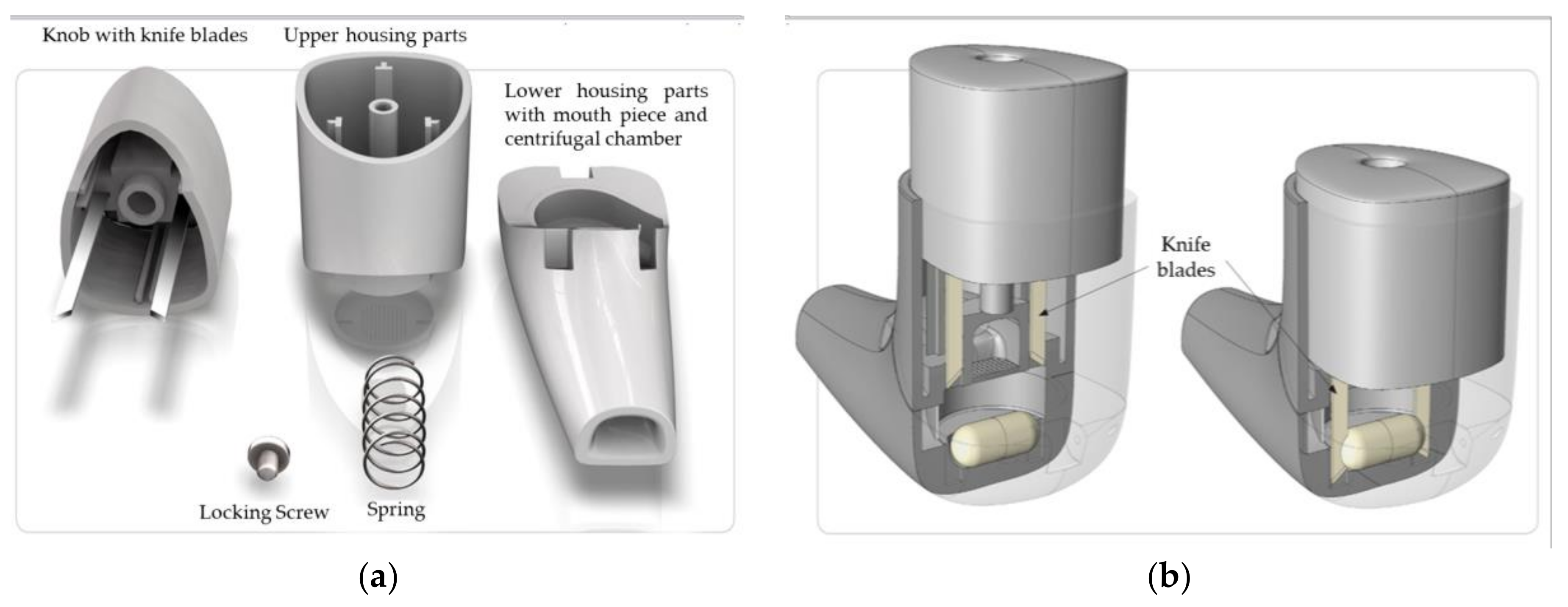
- Friebel, C.; Steckel, H.; Müller, B.W. Rational design of a dry powder inhaler: Device design and optimisation. J. Pharm. Pharmacol. 2012, 64, 1303–1315. [Google Scholar] [CrossRef] [PubMed]
- De Boer, A.; Gjaltema, D.; Hagedoorn, P.; Schaller, M.; Witt, W.; Frijlink, H.W. Design and application of a new modular adapter for laser diffraction characterization of inhalation aerosols. Int. J. Pharm. 2002, 249, 233–245. [Google Scholar] [CrossRef]
- Cordts, E.; Steckel, H. Capabilities and limitations of using powder rheology and permeability to predict dry powder inhaler performance. Eur. J. Pharm. Biopharm. 2012, 82, 417–423. [Google Scholar] [CrossRef]
- United States Pharmacopeial Convention. The United States Pharmacopeia: The National Formulary; USP 37-NF 24; United States Pharmacopeial Convention: Rockville, MD, USA, 2014; ISBN 978-1-936424-22-1. [Google Scholar]
- Scherließ, R. The MTT assay as tool to evaluate and compare excipient toxicity in vitro on respiratory epithelial cells. Int. J. Pharm. 2011, 411, 98–105. [Google Scholar] [CrossRef]
- Mansour, H.M.; Xu, Z.; Hickey, A.J. Dry Powder Aerosols Generated by Standardized Entrainment Tubes from Alternative Sugar Blends: 3. Trehalose Dihydrate and d-Mannitol Carriers. J. Pharm. Sci. 2010, 99, 3430–3441. [Google Scholar] [CrossRef]
- Ógáin, O.N.; Li, J.; Tajber, L.; Corrigan, O.I.; Healy, A.M. Particle engineering of materials for oral inhalation by dry powder inhalers. I—Particles of sugar excipients (trehalose and raffinose) for protein delivery. Int. J. Pharm. 2011, 405, 23–35. [Google Scholar] [CrossRef]
- Jones, M.; Hooton, J.C.; Dawson, M.L.; Ferrie, A.R.; Price, R. An Investigation into the Dispersion Mechanisms of Ternary Dry Powder Inhaler Formulations by the Quantification of Interparticulate Forces. Pharm. Res. 2007, 25, 337–348. [Google Scholar] [CrossRef] [Green Version]
- Pitchayajittipong, C.; Price, R.; Shur, J.; Kaerger, J.S.; Edge, S. Characterisation and functionality of inhalation anhydrous lactose. Int. J. Pharm. 2010, 390, 134–141. [Google Scholar] [CrossRef]
- Nykamp, G.; Carstensen, U.; Müller, B. Jet milling—A new technique for microparticle preparation. Int. J. Pharm. 2002, 242, 79–86. [Google Scholar] [CrossRef]
- Vatsaraj, N.B.; Gao, D.; Kowalski, D.L. Optimization of the operating conditions of a lab scale Aljet mill using lactose and sucrose: A technical note. AAPS PharmSciTech 2003, 4, 141–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malcolmson, R.J.; Embleton, J.K. Dry powder formulations for pulmonary delivery. Pharm. Sci. Technol. Today 1998, 1, 394–398. [Google Scholar] [CrossRef]
- Kawashima, Y.; Serigano, T.; Hino, T.; Yamamoto, H.; Takeuchi, H. Effect of surface morphology of carrier lactose on dry powder inhalation property of pranlukast hydrate. Int. J. Pharm. 1998, 172, 179–188. [Google Scholar] [CrossRef]
- Renner, N.; Steckel, H.; Urbanetz, N.; Scherließ, R. Nano- and Microstructured model carrier surfaces to alter dry powder inhaler performance. Int. J. Pharm. 2017, 518, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Young, P.M.; Thompson, J.; Woodcock, D.; Aydin, M.; Price, R. The Development of a Novel High-Dose Pressurized Aerosol Dry-Powder Device (PADD) for the Delivery of Pumactant for Inhalation Therapy. J. Aerosol. Med. 2004, 17, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Farkas, D.R.; Hindle, M.; Longest, P.W. Characterization of a New High-Dose Dry Powder Inhaler (DPI) Based on a Fluidized Bed Design. Ann. Biomed. Eng. 2015, 43, 2804–2815. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Clercq, E. Antiviral agents active against influenza A viruses. Nat. Rev. Drug Discov. 2006, 5, 1015–1025. [Google Scholar] [CrossRef]
- Jones, M.; Santo, J.G.; Yakub, B.; Dennison, M.; Master, H.; Buckton, G. The relationship between drug concentration, mixing time, blending order and ternary dry powder inhalation performance. Int. J. Pharm. 2010, 391, 137–147. [Google Scholar] [CrossRef]
- Jones, M.D.; Hooton, J.C.; Dawson, M.L.; Ferrie, A.R.; Price, R. Dehydration of trehalose dihydrate at low relative humidity and ambient temperature. Int. J. Pharm. 2006, 313, 87–98. [Google Scholar] [CrossRef]
- Sussich, F.; Urbani, R.; Princivalle, F.; Cesàro, A. Polymorphic Amorphous and Crystalline Forms of Trehalose. J. Am. Chem. Soc. 1998, 120, 7893–7899. [Google Scholar] [CrossRef]
- Pilcer, G.; Wauthoz, N.; Amighi, K. Lactose characteristics and the generation of the aerosol. Adv. Drug Deliv. Rev. 2012, 64, 233–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Boer, A.H.; Chan, H.; Price, R. A critical view on lactose-based drug formulation and device studies for dry powder inhalation: Which are relevant and what interactions to expect? Adv. Drug Deliv. Rev. 2012, 64, 257–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nalluri, V.R.; Kuentz, M. Flowability characterisation of drug-excipient blends using a novel powder avalanching method. Eur. J. Pharm. Biopharm. 2010, 74, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Tiddens, H.A.W.M.; Geller, D.; Challoner, P.; Speirs, R.; Kesser, K.; Overbeek, S.; Humble, D.; Shrewsbury, S.; Standaert, T. Effect of Dry Powder Inhaler Resistance on the Inspiratory Flow Rates and Volumes of Cystic Fibrosis Patients of Six Years and Older. J. Aerosol. Med. 2006, 19, 456–465. [Google Scholar] [CrossRef]
- Srichana, T.; Martin, G.P.; Marriott, C. Dry powder inhalers: The influence of device resistance and powder formulation on drug and lactose deposition in vitro. Eur. J. Pharm. Sci. 1998, 7, 73–80. [Google Scholar] [CrossRef]
- Young, P.M.; Edge, S.; Traini, D.; Jones, M.; Price, R.; El-Sabawi, D.; Urry, C.M.; Smith, C. The influence of dose on the performance of dry powder inhalation systems. Int. J. Pharm. 2005, 296, 26–33. [Google Scholar] [CrossRef]
- Steckel, H.; Markefka, P.; Tewierik, H.; Kammelar, R. Functionality testing of inhalation grade lactose. Eur. J. Pharm. Biopharm. 2004, 57, 495–505. [Google Scholar] [CrossRef]
- Hamishehkar, H.; Emami, J.; Najafabadi, A.R.; Gilani, K.; Minaiyan, M.; Mahdavi, H.; Nokhodchi, A. Influence of carrier particle size, carrier ratio and addition of fine ternary particles on the dry powder inhalation performance of insulin-loaded PLGA microcapsules. Powder Technol. 2010, 201, 289–295. [Google Scholar] [CrossRef]
- Kinnunen, H.; Hebbink, G.; Peters, H.; Shur, J.; Price, R. An Investigation into the Effect of Fine Lactose Particles on the Fluidization Behaviour and Aerosolization Performance of Carrier-Based Dry Powder Inhaler Formulations. AAPS PharmSciTech 2014, 15, 898–909. [Google Scholar] [CrossRef] [Green Version]
- Shur, J.; Harris, H.; Jones, M.D.; Kaerger, J.S.; Price, R. The Role of Fines in the Modification of the Fluidization and Dispersion Mechanism Within Dry Powder Inhaler Formulations. Pharm. Res. 2008, 25, 1631–1640. [Google Scholar] [CrossRef]
- Shalash, A.O.; Molokhia, A.M.; Elsayed, M.M.A. Insights into the roles of carrier microstructure in adhesive/carrier-based dry powder inhalation mixtures: Carrier porosity and fine particle content. Eur. J. Pharm. Biopharm. 2015, 96, 291–303. [Google Scholar] [CrossRef] [PubMed]
- Scherließ, R.; Etschmann, C. DPI formulations for high dose applications—Challenges and opportunities. Int. J. Pharm. 2018, 548, 49–53. [Google Scholar] [CrossRef] [PubMed]
- De Boer, A.H.; Hagedoorn, P.; Hoppentocht, M.; Buttini, F.; Grasmeijer, F.; Frijlink, H.W. Dry powder inhalation: Past, present and future. Expert Opin. Drug Deliv. 2017, 14, 499–512. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Excipient/Diluent | Diluent Grade | Fine Diluent’s Particle Size Distribution | Blend Ratio OP/Diluent | Micronized OP Formulations with Diluent | ||
|---|---|---|---|---|---|---|
| X10 | X50 | X90 | ||||
| Glucose | Micronized | 1.19 ± 0.02 | 5.46 ± 0.21 | 21.32 ± 0.67 | 1:1 | G1-50 |
| Milled | 3.79 ± 0.21 | 20.23 ± 0.72 | 39.2 ± 0.93 | G2-50 | ||
| Lactose | Micronized (LH300) | 0.84 ± 0.01 | 4.43 ± 0.03 | 7.71 ± 0.31 | L1-50 | |
| Milled (ML006) | 1.71 ± 0.02 | 18.1 ± 0.37 | 46.14 ± 1.1 | L2-50 | ||
| Mannitol | Micronized | 0.77 ± 0.02 | 2.26 ± 0.03 | 6.42 ± 0.23 | M1-50 | |
| Milled | 1.7 ± 0.04 | 16.7 ± 0.49 | 46.35 ± 1.21 | M2-50 | ||
| Trehalose | Micronized 1 | 0.67 ± 0.01 | 2.23 ± 0.07 | 6.5 ± 0.27 | T1-50 | |
| 1:3 | T1-75 | |||||
| 3:1 | T1-25 | |||||
| Micronized 2 | 0.57 ± 0.01 | 1.68 ± 0.02 | 3.96 ± 0.11 | T11-25 | ||
| Micronized 3 | 0.99 ± 0.02 | 5.26 ± 0.12 | 20.3 ± 0.97 | T5-25 | ||
| Milled | 1.51 ± 0.07 | 14.97 ± 0.73 | 40.15 ± 5.09 | 1:1 | T2-50 | |
| 1:3 | T2-75 | |||||
| 3:1 | T2-25 | |||||
| Trehalose Micronized Grades | Fluidization Energy (mJ) | Specific Surface Area (m2/g) |
|---|---|---|
| T5 | 51.1 ± 2.4 | 1.25 ± 0.04 |
| T1 | 93.9 ± 2.0 | 2.36 ± 0.01 |
| T11 (finest) | 136.2 ± 2.6 | 2.73 ± 0.01 |
| Source of Variation | Sum of Squares (SS) | Degrees of Freedom (DF) | Mean Square (MS) | p-Value * | Significant? (Yes/No) | |
|---|---|---|---|---|---|---|
| Carrier type | Lactose, Mannitol, Trehalose, Glucose | 25.21 | 3 | 8.402 | =0.0458 | Yes |
| Carrier size | Micronized, Milled | 35.88 | 1 | 35.88 | =0.0012 | Yes |
| Inhaler device | Uni-haler, Rack | 1734 | 1 | 1734 | <0.0001 | Yes |
| Carrier type × Carrier size | 16.37 | 3 | 5.456 | =0.1435 | No | |
| Carrier type × Inhaler device | 196.4 | 3 | 65.47 | <0.0001 | Yes | |
| Carrier size × Inhaler device | 145.3 | 2 | 145.3 | <0.0001 | Yes | |
| Carrier type × Carrier size × Inhaler device | 197.5 | 3 | 65.85 | <0.0001 | Yes | |
| Residual | 90.15 | 32 | 2.817 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aziz, S.; Scherlieβ, R.; Steckel, H. Development of High Dose Oseltamivir Phosphate Dry Powder for Inhalation Therapy in Viral Pneumonia. Pharmaceutics 2020, 12, 1154. https://doi.org/10.3390/pharmaceutics12121154
Aziz S, Scherlieβ R, Steckel H. Development of High Dose Oseltamivir Phosphate Dry Powder for Inhalation Therapy in Viral Pneumonia. Pharmaceutics. 2020; 12(12):1154. https://doi.org/10.3390/pharmaceutics12121154
Chicago/Turabian StyleAziz, Shahir, Regina Scherlieβ, and Hartwig Steckel. 2020. "Development of High Dose Oseltamivir Phosphate Dry Powder for Inhalation Therapy in Viral Pneumonia" Pharmaceutics 12, no. 12: 1154. https://doi.org/10.3390/pharmaceutics12121154
APA StyleAziz, S., Scherlieβ, R., & Steckel, H. (2020). Development of High Dose Oseltamivir Phosphate Dry Powder for Inhalation Therapy in Viral Pneumonia. Pharmaceutics, 12(12), 1154. https://doi.org/10.3390/pharmaceutics12121154