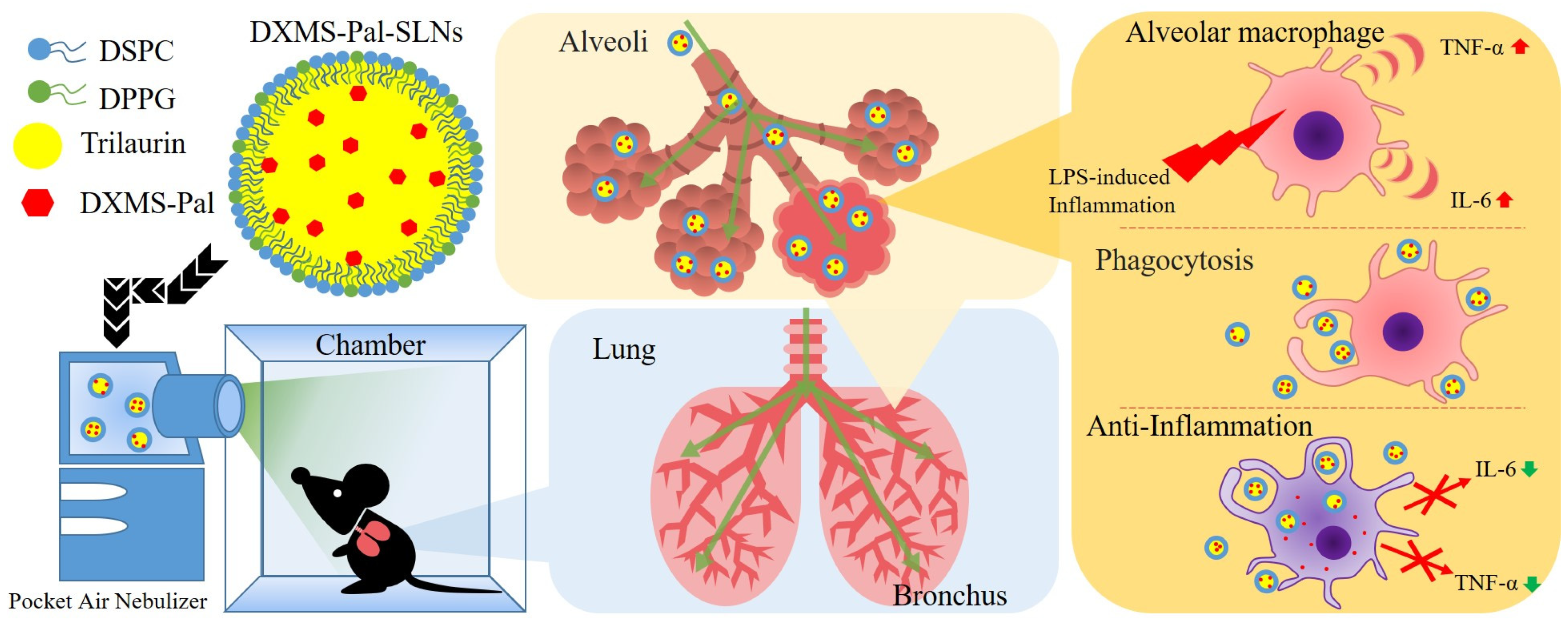
Solid Lipid Nanoparticles Loaded with Dexamethasone Palmitate for Pulmonary Inflammation Treatment by Nebulization Approach
Abstract
1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Preparation and Characterization of DXMS-Pal-SLNs
2.3. Drug Leakage Evaluation of SLNs
2.4. In Vitro Analysis
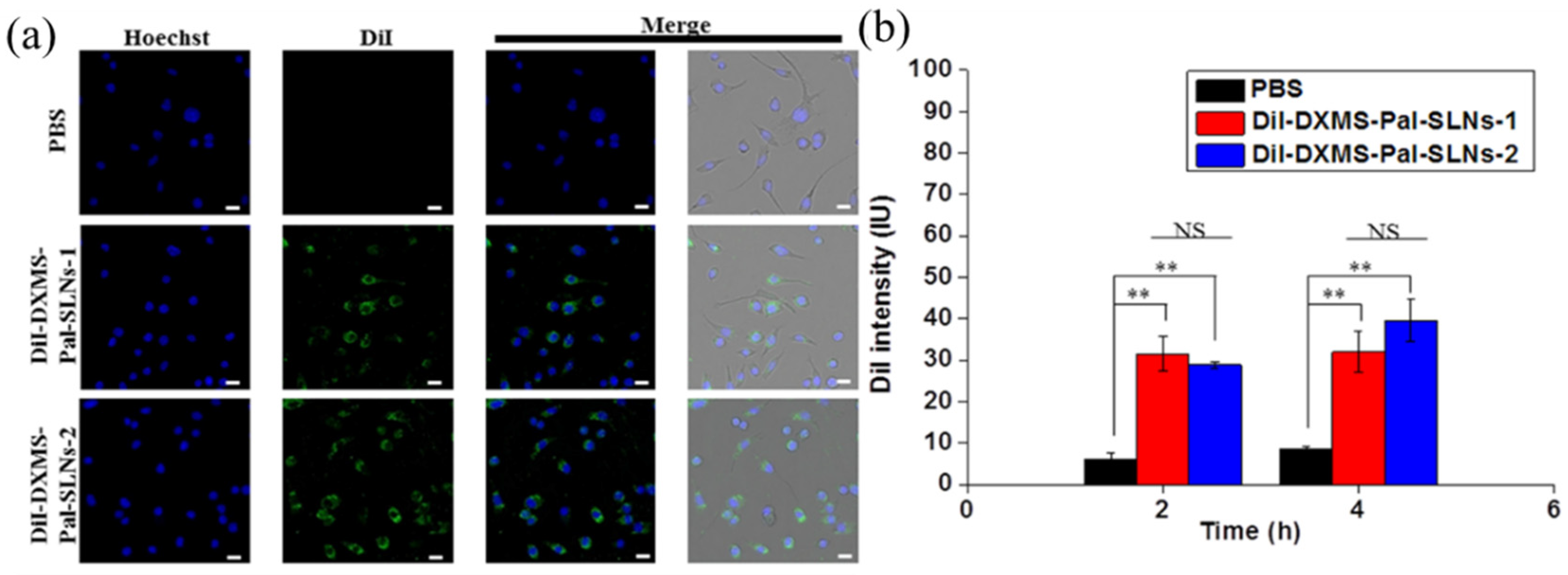
2.4.1. Uptake Study
2.4.2. Cytotoxicity
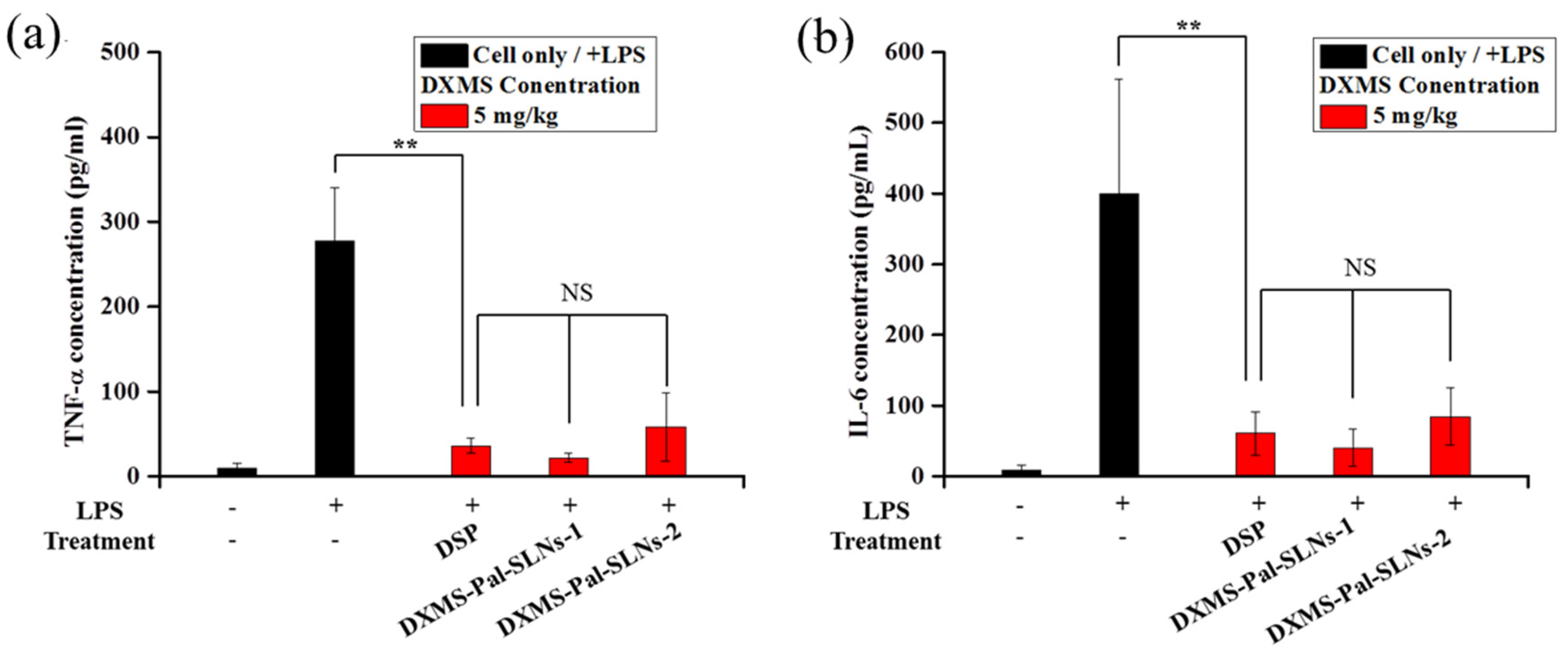
2.4.3. In Vitro Anti-Inflammatory Efficacy
2.5. In Vivo Study
2.5.1. Animal Model
2.5.2. Administration of DXMS-Pal-SLNs Via Intratracheal Injection
2.5.3. Administration of DXMS-Pal-SLNs Via Nebulization
2.5.4. H and E Staining
2.5.5. Hemolysis Test
2.6. Statistical Analysis
3. Results and Discussion
3.1. Characterization of DXMS-Pal-SLNs
3.2. Drug Leakage Behaviors of Drug-Loaded SLNs
3.3. In Vitro Cellular Uptake, Cytotoxicity and Anti-Inflammatory Efficacy
3.4. In Vivo Anti-Inflammatory Efficacy
3.5. Biosafety of DXMS-Pal-SLNs
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- American Thoracic Society. Urgent Progress Needed to End the Preventable Burden of Pneumonia and Deaths: The Forum of International Respiratory Societies. Available online: https://ginasthma.org/global-efforts-must-be-strengthened-to-end-the-preventable-burden-of-pneumonia-the-forum-of-international-respiratory-societies/ (accessed on 12 November 2021).
- Tanaka, S.; Inoue, M.; Yamaji, T.; Iwasaki, M.; Minami, T.; Tsugane, S.; Sawada, N.; The JPHC Study Group. Increased risk of death from pneumonia among cancer survivors: A propensity score-matched cohort analysis. Cancer Med. 2023, 12, 6689–6699. [Google Scholar] [CrossRef]
- Wang, H.; Chen, L.; Li, R.; Lv, C.; Xu, Y.; Xiong, Y. Polydopamine-coated mesoporous silica nanoparticles co-loaded with Ziyuglycoside I and Oseltamivir for synergistic treatment of viral pneumonia. Int. J. Pharm. 2023, 645, 123412–123431. [Google Scholar] [CrossRef]
- Yang, L.; Jin, J.; Luo, W.; Gan, Y.; Chen, B.; Li, W. Risk factors for predicting mortality of COVID-19 patients: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0243124. [Google Scholar] [CrossRef]
- WHO. Pneumonia in Children, Fact Sheets. 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/pneumonia (accessed on 16 June 2023).
- Brodin, P. SARS-CoV-2 infections in children: Understanding diverse outcomes. Immunity 2022, 55, 201–209. [Google Scholar] [CrossRef]
- Costabile, G.; Mitidieri, E.; Visaggio, D.; Provenzano, R.; Miro, A.; Quaglia, F.; Angelo, I.; Frangipani, E.; Sorrentino, R.; Visca, P.; et al. Boosting lung accumulation of gallium with inhalable nano-embedded microparticles for the treatment of bacterial pneumonia. Int. J. Pharm. 2020, 629, 122400–122415. [Google Scholar] [CrossRef]
- Losier, A.; Gupta, G.; Caldararo, M.; Cruz, C.S.D. The impact of coronavirus disease 2019 on viral, bacterial, and fungal respiratory infections. Clin. Chest Med. 2022, 44, 87–94. [Google Scholar] [CrossRef]
- Das, U.N. Bioactive lipids in COVID-19-further evidence. Arch. Med. Res. 2021, 52, 107–120. [Google Scholar] [CrossRef]
- Nazerian, Y.; Ghasemi, M.; Yassaghi, Y.; Nazerian, A.; Hashemi, S.M. Role of SARS-CoV-2-induced cytokine storm in multi-organ failure: Molecular pathways and potential therapeutic options. Int. Immunopharmacol. 2022, 113, 109428–109445. [Google Scholar] [CrossRef]
- Chu, M.; Wang, H.; Bian, L.; Huang, J.; Wu, D.; Zhang, R.; Fei, F.; Chen, Y.; Xia, J. Nebulization therapy with umbilical cord mesenchymal stem cell-derived exosomes for COVID-19 pneumonia. Stem. Cell Rev. Rep. 2022, 18, 2152–2163. [Google Scholar] [CrossRef]
- Darmawan, E.; Kusumawati, L. The combination of salbutamol nebulizer and oral procaterol to the indonesian children with pneumonia. Iran. J. Pharm. Sci. 2020, 16, 59–72. [Google Scholar] [CrossRef]
- Zhang, H.; Liu, Y.; Yuan, B.; Wang, W.; Jin, Y.; Wei, X. Alkaline tea tree oil nanoemulsion nebulizers for the treatment of pneumonia induced by drug-resistant Acinetobacter baumannii. J. Drug Deliv. Sci. Technol. 2023, 79, 104047. [Google Scholar] [CrossRef]
- Klein, D.M.; Poortinga, A.; Verhoeven, F.M.; Bonn, D.; Bonnet, S.; Rijn, C.J.M.v. Degradation of lipid based drug delivery formulations during nebulization. Chem. Phys. 2021, 547, 111192–111196. [Google Scholar] [CrossRef]
- Chandel, A.; Goyal, A.K.; Ghosh, G.; Rath, G. Recent advances in aerosolised drug delivery. Biomed. Pharmacother 2019, 112, 108601–108612. [Google Scholar] [CrossRef]
- Leong, E.W.X.; Ruowen, G. Lipid nanoparticles as delivery vehicles for inhaled therapeutics. Biomedicines 2022, 10, 2179. [Google Scholar] [CrossRef]
- Chen, H.H.; Huang, W.C.; Chiang, W.H.; Liu, T.I.; Shen, M.Y.; Hsu, Y.H.; Lin, S.C.; Chiu, H.C. pH-Responsive therapeutic solid lipid nanoparticles for reducing P-glycoprotein-mediated drug efflux of multidrug resistant cancer cells. Int. J. Nanomed. 2015, 10, 5035–5048. [Google Scholar] [CrossRef]
- Lin, C.-H.; Chen, C.-H.; Lin, Z.-C.; Fang, J.-Y. Recent advances in oral delivery of drugs and bioactive natural products using solid lipid nanoparticles as the carriers. J. Food Drug Anal. 2017, 25, 219–234. [Google Scholar] [CrossRef]
- Carvalho, F.O.; Silva, É.R.; Nunes, P.S.; Felipe, F.A.; Ramos, K.P.P.; Ferreira, L.A.S.; Lima, V.N.B.; Shanmugam, S.; Oliveira, A.S.; Guterres, S.S.; et al. Effects of the solid lipid nanoparticle of carvacrol on rodents with lung injury from smoke inhalation. Naunyn Schmiedebergs Arch. Pharmacol. 2020, 393, 445–455. [Google Scholar] [CrossRef]
- Paranjpe, M.; Müller-Goymann, C.C. Nanoparticle-mediated pulmonary drug delivery: A review. Int. J. Mol. Sci. 2014, 15, 5852–5873. [Google Scholar] [CrossRef]
- Nassimi, M.; Schleh, C.; Lauenstein, H.D.; Hussein, R.; Hoymann, H.G.; Koch, W.; Pohlmann, G.; Krug, N.; Sewald, K.; Rittinghause, S.; et al. A toxicological evaluation of inhaled solid lipid nanoparticles used as a potential drug delivery system for the lung. Eur. J. Pharm. Biopharm. 2010, 75, 107–116. [Google Scholar] [CrossRef]
- Corzo, C.; Meindl, C.; Lochmann, D.; Reyer, S.; Salar-Behzadi, S. Novel approach for overcoming the stability challenges of lipid-based excipients. Part 3: Application of polyglycerol esters of fatty acids for the next generation of solid lipid nanoparticles. Eur. J. Pharm. Biopharm. 2020, 152, 44–55. [Google Scholar] [CrossRef]
- Dionne, R.A.; Gordon, S.M.; Rowan, J.; Kent, A.; Brahim, J.S. Dexamethasone suppresses peripheral prostanoid levels without analgesia in a clinical model of acute inflammation. J. Oral Maxillofac. Surg. 2003, 61, 997–1003. [Google Scholar] [CrossRef]
- Klemm, P.; Harris, H.J.; Perretti, M. Effect of rolipram in a murine model of acute inflammation: Comparison with the corticoid dexamethasone. Eur. J. Pharmacol. 1995, 281, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Stern, A.; Skalsky, K.; Avni, T.; Carrara, E.; Leibovici, L.; Paul, M. Corticosteroids for pneumonia. Cochrane Database Syst. Rev. 2017, 12, CD007720. [Google Scholar] [CrossRef] [PubMed]
- Tramer, M.R.; von Elm, E.; Loubeyre, P.; Hauser, C. Pharmacological prevention of serious anaphylactic reactions due to iodinated contrast media: Systematic review. Br. Med. J. 2006, 333, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Horby, P.; Lim, W.S.; Emberson, J.R.; Mafham, M.; Bell, J.L.; Linsell, L.; Staplin, N.; Brightling, C.; Ustianowski, A.; Elmahi, E.; et al. Dexamethasone in hospitalized patients with COVID-19. N. Engl. J. Med. 2021, 384, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Johns, M.; George, S.; Taburyanskaya, M.; Poon, Y.K. A review of the evidence for corticosteroids in COVID-19. J. Pharm. Pract. 2022, 35, 626–637. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.-T.; Hong, M.-Y.; Chen, C.-L.; Hwang, C.-Y.; Tsai, C.-C.; Chuang, C.-C. Mutant glucocorticoid receptor binding elements on the interleukin-6 promoter regulate dexamethasone effects. BMC Immunol. 2021, 22, 24. [Google Scholar] [CrossRef] [PubMed]
- Hochhaus, G.; Barth, J.; Al-Fayoumi, S.; Suarez, S.; Derendorf, H.; Hochhaus, R.; Mollmann, H. Pharmacokinetics and pharmacodynamics of dexamethasone sodium-m-sulfobenzoate (DS) after intravenous and intramuscular administration: A comparison with dexamethasone phosphate (DP). J. Clin. Pharmacol. 2001, 41, 425–434. [Google Scholar] [CrossRef] [PubMed]
- McClintock, D.; Austel, M.; Jr, R.M.G.; Banovic, F. Oral dexamethasone sodium phosphate solution significantly reduces pruritus and clinical lesions in feline hypersensitivity dermatitis: An open-label study. Vet. Dermatol. 2021, 32, 497-e137. [Google Scholar] [CrossRef] [PubMed]
- Lorscheider, M.; Tsapis, N.; Simón-Vázquez, R.; Guiblin, N.; Ghermani, N.; Reynaud, F.; Canioni, R.; Abreu, S.; Chaminade, P.; Fattal, E. Nanoscale lipophilic prodrugs of dexamethasone with enhanced pharmacokinetics. Mol. Pharm. 2019, 16, 2999–3010. [Google Scholar] [CrossRef]
- Kim, J.-K.; Yuan, H.; Nie, J.; Yang, Y.-T.; Leggas, M.; Potter, P.M.; Rinehart, J.; Jay, M.; Lu, X. High payload dual therapeutic-imaging nanocarriers for triggered tumor delivery. Small 2012, 8, 2895–2903. [Google Scholar] [CrossRef]
- Simon-Vazquez, R.; Tsapis, N.; Lorscheider, M.; Rodriguez, A.; Calleja, P.; Mousnier, L.; de Miguel Villegas, E.; Gonzalez-Fernandez, A.; Fattal, E. Improving dexamethasone drug loading and efficacy in treating arthritis through a lipophilic prodrug entrapped into PLGA-PEG nanoparticles. Drug Deliv. Transl. Res. 2022, 12, 1270–1284. [Google Scholar] [CrossRef] [PubMed]
- Yeo, J.; Lee, Y.M.; Lee, J.; Park, D.; Kim, K.; Kim, J.; Park, J.; Kim, W.J. Nitric oxide-scavenging nanogel for treating rheumatoid arthritis. Nano Lett. 2019, 19, 6716–6724. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Saeed, A.F.U.H.; Liu, Q.; Jiang, Q.; Xu, H.; Xiao, G.G.; Rao, L.; Duo, Y. Macrophages in immunoregulation and therapeutics. Signal Transduct. Target. Ther. 2023, 8, 207. [Google Scholar] [CrossRef] [PubMed]
- Duque, G.A.; Descoteaux, A. Macrophage cytokines: Involvement in immunity and infectious diseases. Mol. Innate Immun. 2014, 5, 491–503. [Google Scholar] [CrossRef]
- Lorscheider, M.; Tsapis, N.; Ur-Rehman, M.; Gaudin, F.; Stolfa, I.; Abreu, S.; Mura, S.; Chaminade, P.; Espeli, M.; Fattal, E. Dexamethasone palmitate nanoparticles: An efficient treatment for rheumatoid arthritis. J. Control. Release 2019, 296, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Stanzel, F. Bronchoalveolar lavage. J. Bronchol. Interv. Pulmonol. 2012, chapter 16 165–176. Available online: https://link.springer.com/chapter/10.1007/978-1-4614-4292-9_16 (accessed on 1 January 2012).
- Dubina, M.V.; Gomonova, V.V.; Taraskina, A.E.; Vasilyeva, N.V.; Sayganov, S.A. Pathogenesis-based preexposure prophylaxis associated with a low risk of SARS-CoV-2 infection in healthcare workers at a designated COVID-19 hospital: A pilot study. BMC Infect. Dis. 2021, 21, 536. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Chen, D.; Li, L.; Zou, Y.X.; Shang, Y.; Zhang, C.; Zhang, L.; Pan, J.; Chen, Q.; Ai, T.; et al. CARE: An observational study of adherence to home nebulizer therapy among children with asthma. Ther. Adv. Respir. Dis. 2021, 15, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ruan, J.L.; Tulloch, N.L.; Muskheli, V.; Genova, E.E.; Mariner, P.D.; Anseth, K.S.; Murry, C.E. An improved cryosection method for polyethylene glycol hydrogels used in tissue engineering. Tissue Eng. Part C Methods 2013, 19, 794–801. [Google Scholar] [CrossRef]
- Khullar, P.; Singh, V.; Mahal, A.; Dave, P.N.; Thakur, S.; Kaur, G.; Singh, J.; Kamboj, S.S.; Bakshi, M.S. Bovine serum albumin bioconjugated gold nanoparticles: Synthesis, hemolysis, and cytotoxicity toward cancer cell lines. J. Phys. Chem. C 2012, 116, 8834–8843. [Google Scholar] [CrossRef]
- Németh, Z.; Csóka, I.; Jazani, R.S.; Sipos, B.; Haspel, H.; Kozma, G.; Kónya, Z.D.D.G. Quality by design-driven zeta potential optimisation study of liposomes with charge imparting membrane additives. Pharmaceutics 2022, 14, 1798. [Google Scholar] [CrossRef]
- Jadhav, D.; Vavia, P. Dexamethasone sodium phosphate loaded modified cyclodextrin based nanoparticles: An efficient treatment for rheumatoid arthritis. J. Pharm. Sci. 2021, 110, 1206–1218. [Google Scholar] [CrossRef] [PubMed]
- Zhou, X.; Zezi, M.Y.A.; Li, D.; Wang, J. Telmisartan ameliorates LPS-induced pneumonia in rats through regulation of the PPARγ/NF-κB pathway. Microbiol. Immunol. 2022, 66, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Bian, X.-X.; Zhao, X.; Ma, C.-H.; Shen, C.-P. Arbutin alleviates LPS induced sepsis pneumonia in mice. Evid. Based Complement. Alternat. Med 2022, 2022, 1–8. [Google Scholar] [CrossRef]
- Tian, J.; Wang, X.-L.; Wang, L.-C.; Chen, F.; Tian, Y.; Ma, L.; Pan, C.-Y.; Wang, Y.-P. Qiangli Wuhu mixture alleviates LPS-induced pneumonia by inhibiting theTLR4/NF-jB/NLRP3 pathway: A study based on network pharmacology. Pharm. Boil. 2022, 60, 1331–1340. [Google Scholar] [CrossRef]
- Seeley, J.J.; Ghosh, S. Molecular mechanisms of innate memory and tolerance to LPS. J. Leukoc. Biol. 2017, 101, 107–119. [Google Scholar] [CrossRef] [PubMed]






| Sample | DXMS-Pal | Size | PDI | ZP | LE/LC (DXMS-Pal) | LC (DXMS) |
|---|---|---|---|---|---|---|
| (mg) | (Dh nm) | (mV) | (%) | (%) | ||
| DXMS-Pal-SLNs-1 | 4 | 183.4 ± 2.3 | 0.2 ± 0.03 | −45.7 | 94.0 ± 1.1/15.8 ± 1.2 | 9.8 ± 0.7 |
| DXMS-Pal-SLNs-2 | 6 | 195.4 ± 3.3 | 0.2 ± 0.02 | −47.9 | 93.9 ± 3.2/23.3 ± 1.4 | 14.5 ± 0.9 |
| DXMS-Pal-SLNs-3 | 8 | 196.1 ± 5.1 (precipitate over 7 days at 4 °C) | 0.2 ± 0.02 | −23.2 | 97.4 ± 2.6/26.3 ± 2.2 | 16.4 ± 1.3 |
| Sample | Before Nebulization | After Nebulization | |||
|---|---|---|---|---|---|
| Volume (mL) | Volume (mL) | Recovery (%) | Size (Dh nm) | PDI | |
| DXMS-Pal-SLNs-1 | 2.0 | 1.8 ± 0.05 | 90.2 ± 2.3 | 171.5 ± 1.9 | 0.2 ± 0.02 |
| DXMS-Pal-SLNs-2 | 2.0 | 1.9 ± 0.07 | 86.2 ± 1.4 | 180.6 ± 1.7 | 0.2 ± 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, H.-H.; Sang, C.-H.; Chou, C.-W.; Lin, Y.-T.; Chang, Y.-S.; Chiu, H.-C. Solid Lipid Nanoparticles Loaded with Dexamethasone Palmitate for Pulmonary Inflammation Treatment by Nebulization Approach. Pharmaceutics 2024, 16, 878. https://doi.org/10.3390/pharmaceutics16070878
Chen H-H, Sang C-H, Chou C-W, Lin Y-T, Chang Y-S, Chiu H-C. Solid Lipid Nanoparticles Loaded with Dexamethasone Palmitate for Pulmonary Inflammation Treatment by Nebulization Approach. Pharmaceutics. 2024; 16(7):878. https://doi.org/10.3390/pharmaceutics16070878
Chicago/Turabian StyleChen, Hsin-Hung, Chen-Hsiang Sang, Chang-Wei Chou, Yi-Ting Lin, Yi-Shou Chang, and Hsin-Cheng Chiu. 2024. "Solid Lipid Nanoparticles Loaded with Dexamethasone Palmitate for Pulmonary Inflammation Treatment by Nebulization Approach" Pharmaceutics 16, no. 7: 878. https://doi.org/10.3390/pharmaceutics16070878
APA StyleChen, H.-H., Sang, C.-H., Chou, C.-W., Lin, Y.-T., Chang, Y.-S., & Chiu, H.-C. (2024). Solid Lipid Nanoparticles Loaded with Dexamethasone Palmitate for Pulmonary Inflammation Treatment by Nebulization Approach. Pharmaceutics, 16(7), 878. https://doi.org/10.3390/pharmaceutics16070878









