Investigation of Factors Influencing the Effectiveness of Deformable Nanovesicles for Insulin Nebulization Inhalation
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Animals
2.3. Preparation of Deformable Nanovesicle Based on Insulin–Phospholipid Complexes (IPC-DNVs)
2.3.1. Preparation of IPC-DNVs with Different Particle Sizes
2.3.2. Preparation of IPC-DNVs with Different Deformability
2.3.3. Preparation of IPC-DNVs with Different Drug Load
2.4. Characterization
2.4.1. Determination of Size and Zeta Potential
2.4.2. Entrapment Efficiency (EE)
2.4.3. Deformability
2.5. Determination of Aerodynamic Characteristics
2.6. Uptake by RAW 264.7 Cells
2.6.1. Preparation of FITC-IPC-DNVs
2.6.2. Uptake Study
2.7. Hypoglycemic Effect In Vivo
2.7.1. Intratracheal Instillation Administration
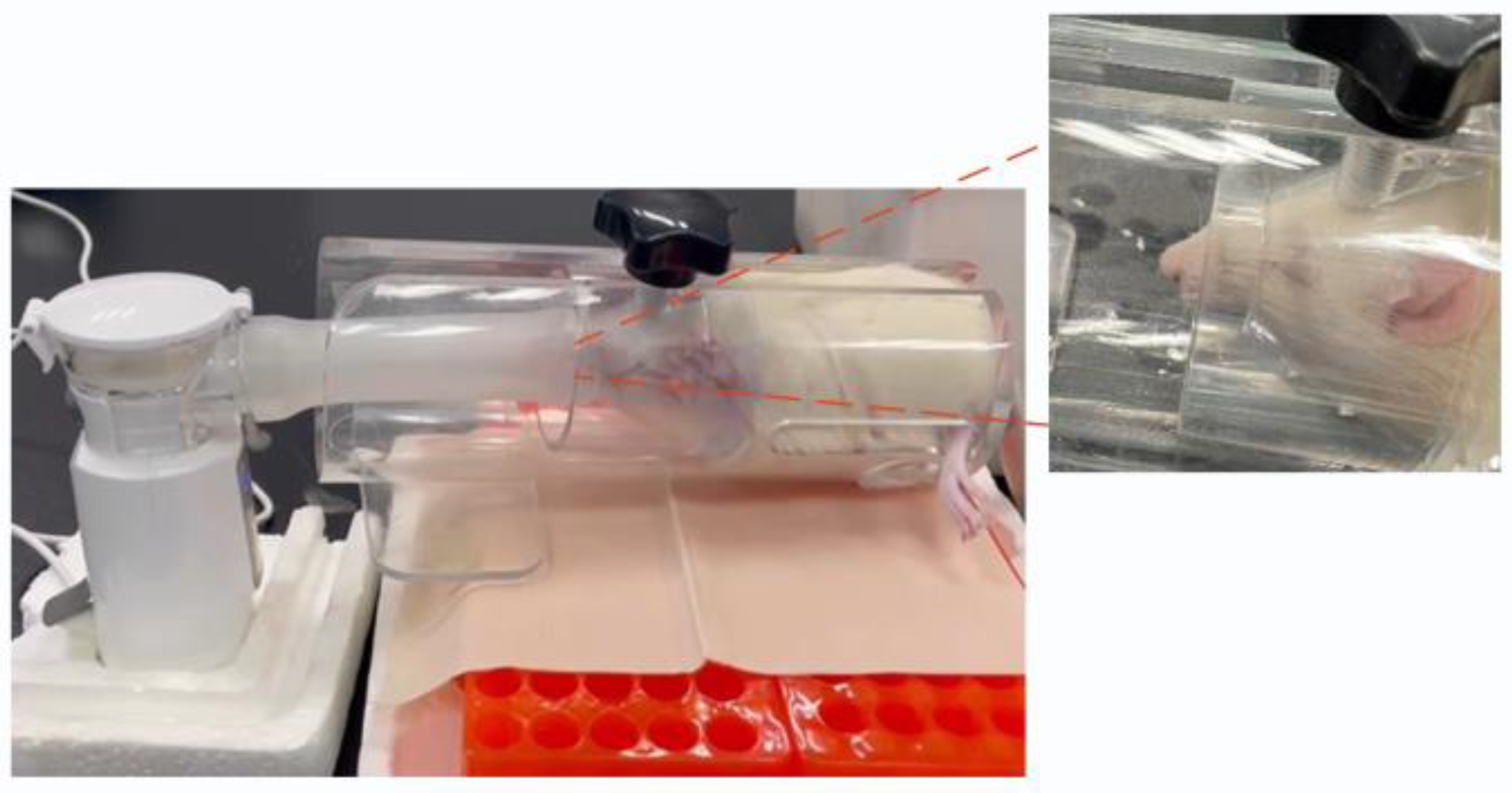
2.7.2. Nebulized Inhalation Administration
2.8. Statistical Analysis
3. Results
3.1. Preparation and Characterization of IPC-DNVs with Different Properties
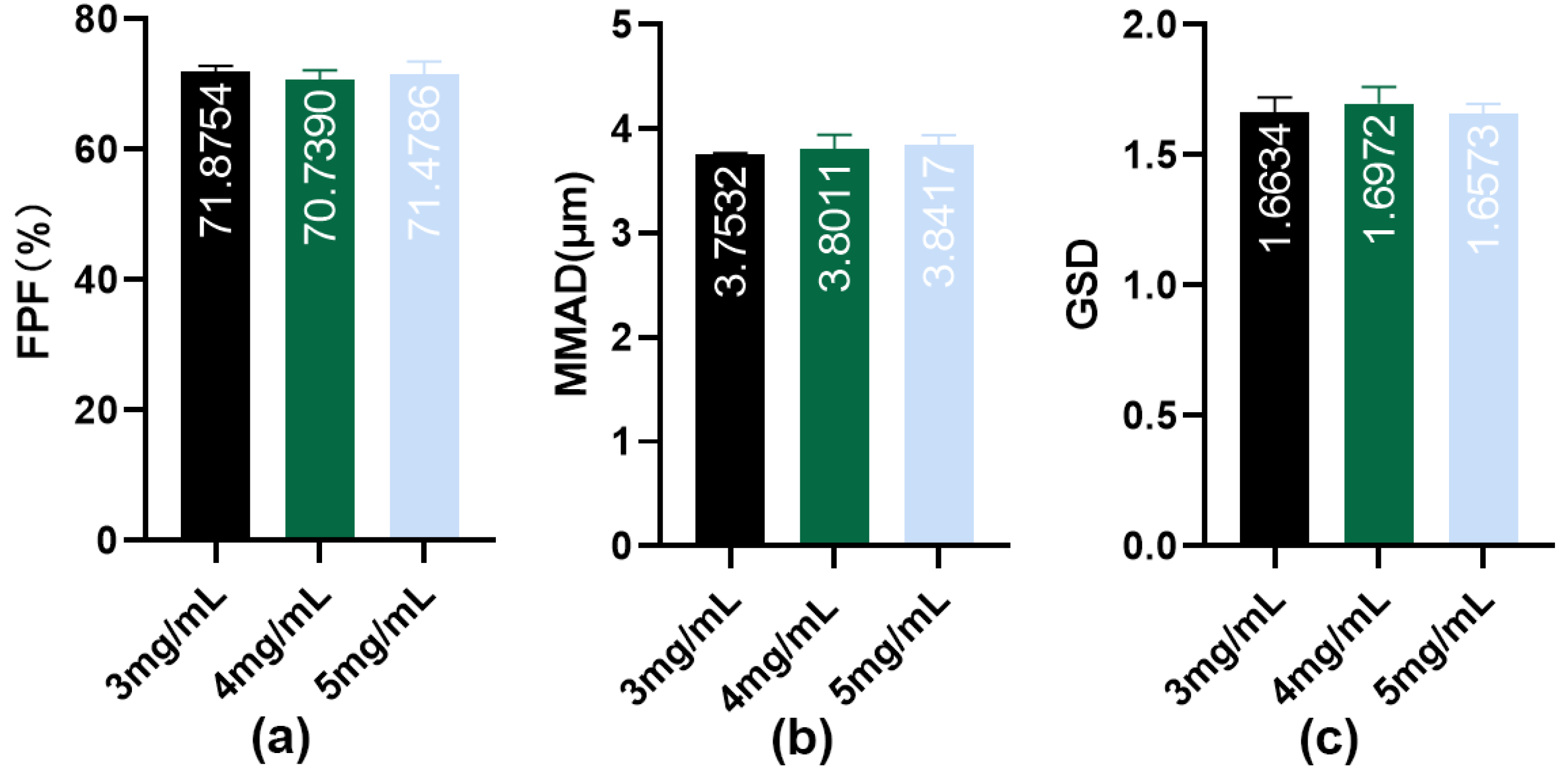
3.2. Impact of Different Properties on the Aerodynamic Characteristics of Aerosols Generated by Nebulization of IPC-DNVs
3.3. Impact of Different Properties on the Uptake of IPC-DNVs by RAW264.7 Cells
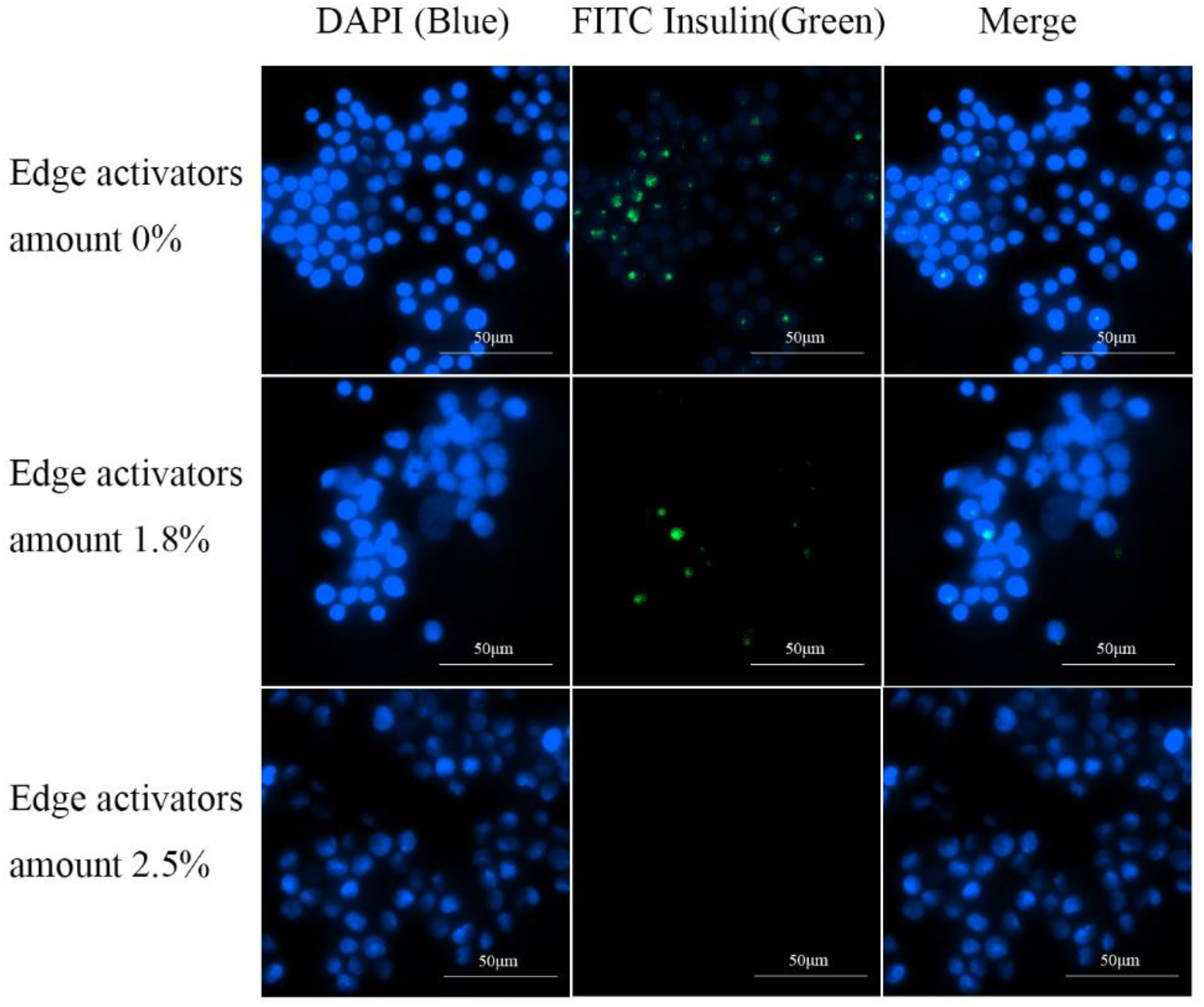
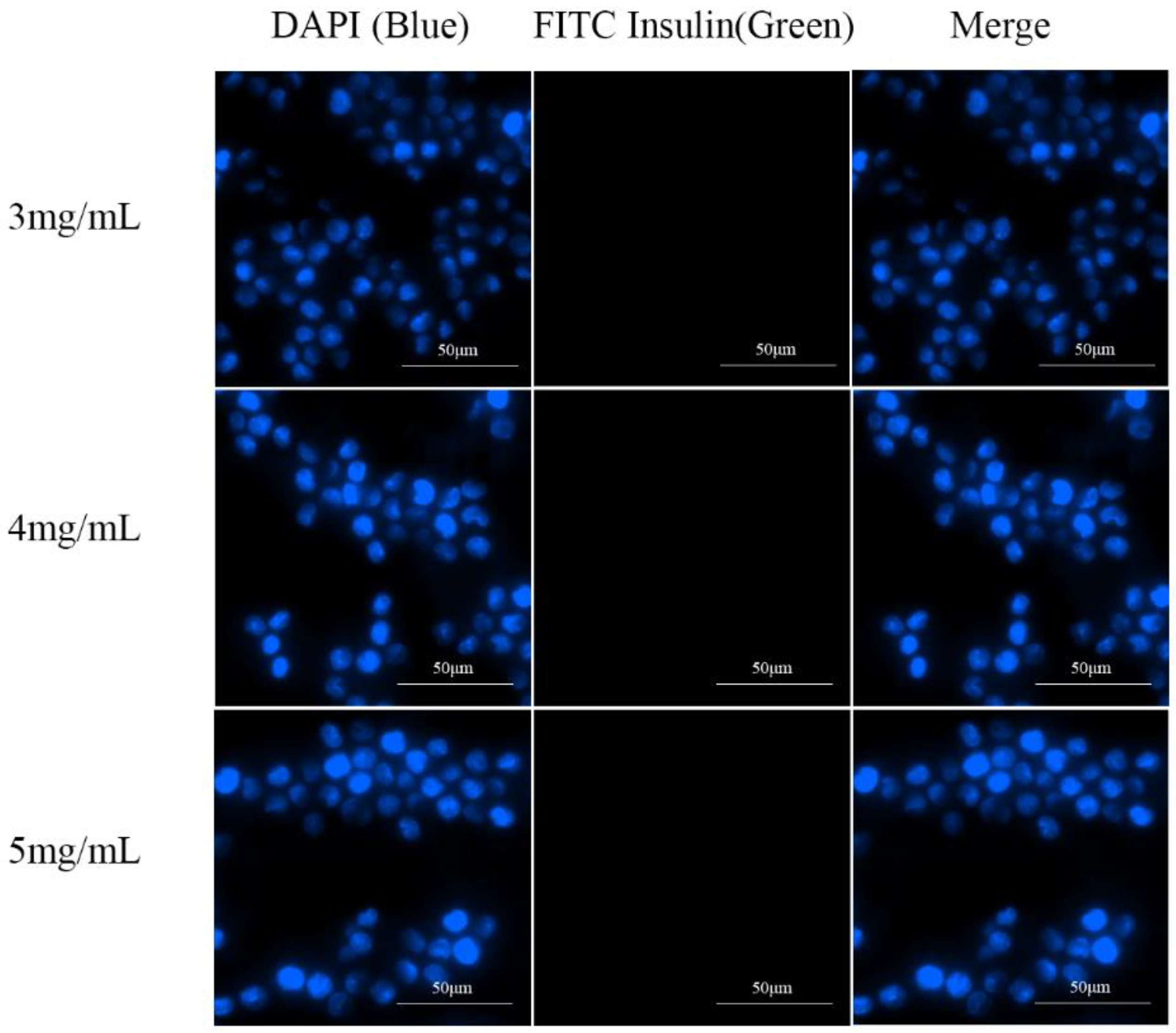
3.3.1. Qualitative Cellular Uptake Studies
3.3.2. Quantitative Cellular Uptake Studies
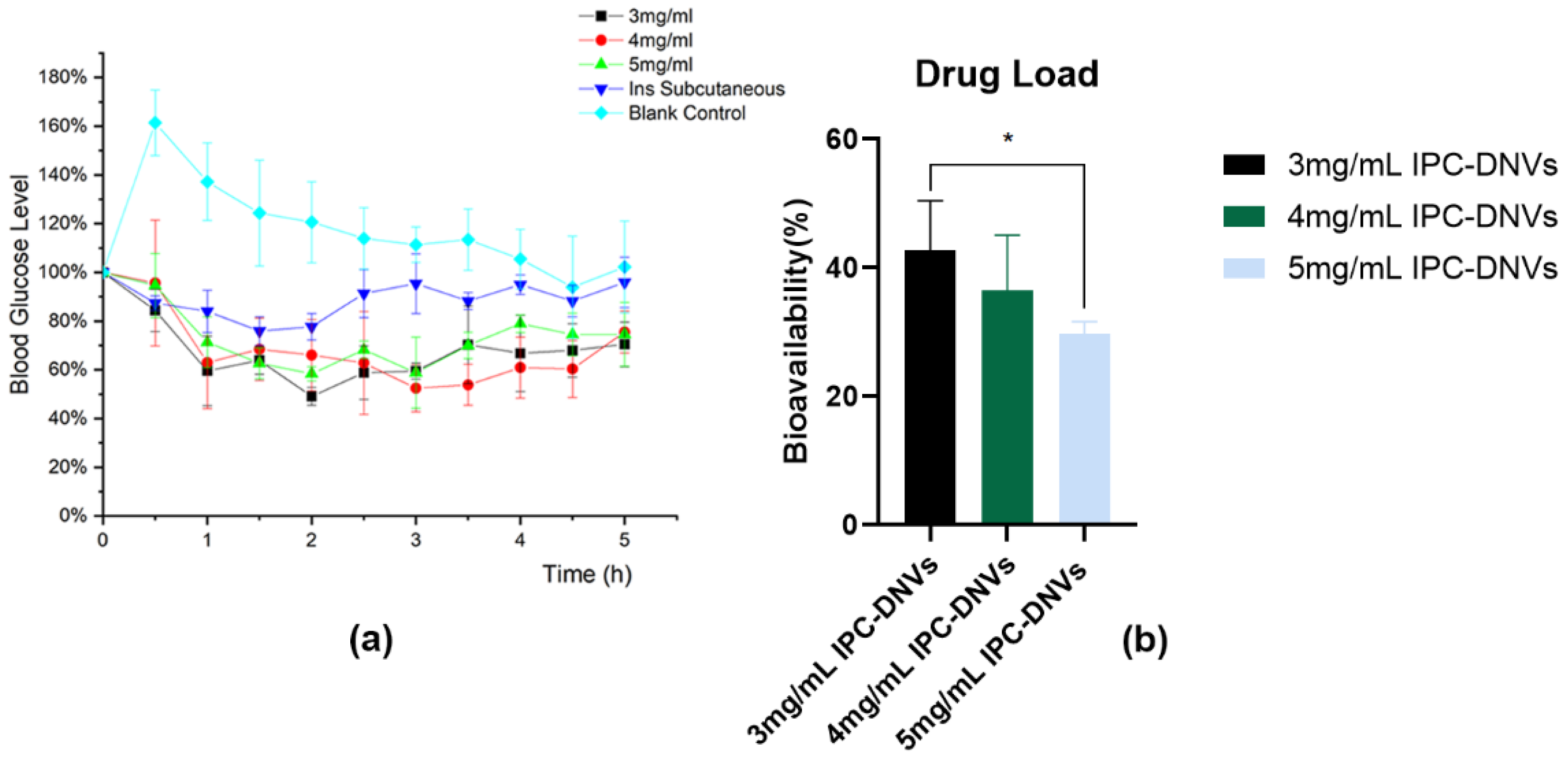
3.4. Hypoglycemic Effect of IPC-DNVs In Vivo
3.4.1. Impact of Different Properties on the Hypoglycemic Effect of IPC-DNVs In Vivo
3.4.2. Feasibility Verification of the Nebulized Inhalation of IPC-DNVs
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Peng, S.; Wang, W.; Zhang, R.; Wu, C.; Pan, X.; Huang, Z. Nano-Formulations for Pulmonary Delivery: Past, Present, and Future Perspectives. Pharmaceutics 2024, 16, 161. [Google Scholar] [CrossRef]
- Feng, X.; Shi, Y.; Zhang, Y.; Lei, F.; Ren, R.; Tang, X. Opportunities and Challenges for Inhalable Nanomedicine Formulations in Respiratory Diseases: A Review. Int. J. Nanomed. 2024, 19, 1509–1538. [Google Scholar] [CrossRef] [PubMed]
- Viegas, C.; Patrício, A.B.; Prata, J.M.; Nadhman, A.; Chintamaneni, P.K.; Fonte, P. Solid Lipid Nanoparticles vs. Nanostructured Lipid Carriers: A Comparative Review. Pharmaceutics 2023, 15, 1593. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Zhao, A.; Zhu, J.; Wang, C.; Shen, J.; Zheng, Z.; Pan, F.; Liu, Z.; Chen, Q.; Yang, Y. Inhaled Lipid Nanoparticles Alleviate Established Pulmonary Fibrosis. Small 2023, 19, e2300545. [Google Scholar] [CrossRef] [PubMed]
- Shirley, M. Amikacin Liposome Inhalation Suspension: A Review in Mycobacterium avium Complex Lung Disease. Drugs 2019, 79, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Hafez, S.M.; Hathout, R.M.; Sammour, O.A. Curcumin-loaded ultradeformable nanovesicles as a potential delivery system for breast cancer therapy. Colloids Surf. B Biointerfaces 2018, 167, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Yang, Y.; Xu, Y.; Meng, Y.; Ye, J.; Xia, X.; Liu, Y. Deformable Nanovesicle-Loaded Gel for Buccal Insulin Delivery. Pharmaceutics 2022, 14, 2262. [Google Scholar] [CrossRef] [PubMed]
- Aundhia, C.; Shah, N.; Talele, C.; Zanwar, A.; Kumari, M.; Patil, S. Enhancing Gene Therapy through Ultradeformable Vesicles for Efficient siRNA Delivery. Pharm. Nanotechnol. 2024, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.; Needham, R.; Yousaf, S.; Houacine, C.; Islam, Y.; Bnyan, R.; Sadozai, S.K.; Elrayess, M.A.; Elhissi, A. Impact of phospholipids, surfactants and cholesterol selection on the performance of transfersomes vesicles using medical nebulizers for pulmonary drug delivery. J. Drug Deliv. Sci. Technol. 2021, 66, 102822. [Google Scholar] [CrossRef]
- Qin, L.; Cui, Z.; Wu, Y.; Wang, H.; Zhang, X.; Guan, J.; Mao, S. Challenges and Strategies to Enhance the Systemic Absorption of Inhaled Peptides and Proteins. Pharm. Res. 2022, 40, 1037–1055. [Google Scholar] [CrossRef]
- Yong, J.; Shu, H.; Zhang, X.; Yang, K.; Luo, G.; Yu, L.; Li, J.; Huang, H. Natural Products-Based Inhaled Formulations for Treating Pulmonary Diseases. Int. J. Nanomed. 2024, 19, 1723–1748. [Google Scholar] [CrossRef] [PubMed]
- Mei, X.; Li, J.; Wang, Z.; Zhu, D.; Huang, K.; Hu, S.; Popowski, K.D.; Cheng, K. An inhaled bioadhesive hydrogel to shield non-human primates from SARS-CoV-2 infection. Nat. Mater. 2023, 22, 903–912. [Google Scholar] [CrossRef] [PubMed]
- Han, M.-M.; Tang, L.; Huang, B.; Li, X.-N.; Fang, Y.; Qi, L.; Duan, B.; Yao, Y.; He, Y.; Xing, L.; et al. Inhaled nanoparticles for treating idiopathic pulmonary fibrosis by inhibiting honeycomb cyst and alveoli interstitium remodeling. J. Control. Release 2024, 366, 732–745. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Chen, Y.; Ge, Y.; Hu, Y.; Li, M.; Jin, Y. Inhalation treatment of primary lung cancer using liposomal curcumin dry powder inhalers. Acta Pharm. Sin. B 2018, 8, 440–448. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Kankala, R.K.; Tang, N.; Xu, P.; Hao, L.; Yang, D.; Wang, S.; Zhang, Y.S.; Chen, A. Supercritical Fluid-Assisted Porous Microspheres for Efficient Delivery of Insulin and Inhalation Therapy of Diabetes. Adv. Heal. Mater. 2018, 8, e1800910. [Google Scholar] [CrossRef] [PubMed]
- Fröhlich, E.; Salar-Behzadi, S. Oral inhalation for delivery of proteins and peptides to the lungs. Eur. J. Pharm. Biopharm. 2021, 163, 198–211. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.; Yuan, Z.; Zhang, P.; Liu, E.; McMullen, P.; Wu, K.; Hung, H.-C.; Jiang, S. Enhanced pulmonary systemic delivery of protein drugs via zwitterionic polymer conjugation. J. Control. Release 2020, 322, 170–176. [Google Scholar] [CrossRef]
- Ceschan, N.E.; Scioli-Montoto, S.; Sbaraglini, M.L.; Ruiz, M.E.; Smyth, H.D.; Bucalá, V.; Ramírez-Rigo, M.V. Nebulization of a polyelectrolyte-drug system for systemic hypertension treatment. Eur. J. Pharm. Sci. 2021, 170, 106108. [Google Scholar] [CrossRef]
- Ponkshe, P.; Wang, Y.; Tan, C. Systemic Protein Delivery via Inhalable Liposomes: Formulation and Pharmacokinetics. Pharmaceutics 2023, 15, 1951. [Google Scholar] [CrossRef]
- Adorni, G.; Seifert, G.; Buttini, F.; Colombo, G.; Stecanella, L.A.; Krämer, I.; Rossi, A. Aerosolization Performance of Jet Nebulizers and Biopharmaceutical Aspects. Pharmaceutics 2019, 11, 406. [Google Scholar] [CrossRef]
- Troy, M.; Van Vleet, J.; Tashkin, D.; Barjaktarevic, I. Recent advances predict a bright future for nebulizers. Curr. Opin. Pulm. Med. 2023, 29, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Pritchard, J.N.; Hatley, R.H.; Denyer, J.; von Hollen, D. Mesh nebulizers have become the first choice for new nebulized pharmaceutical drug developments. Ther. Deliv. 2018, 9, 121–136. [Google Scholar] [CrossRef] [PubMed]
- Falahati, M.; Hasan, A.; Zeinabad, H.A.; Serpooshan, V.; von der Thüsen, J.; Hagen, T.L.T. Engineering of pulmonary surfactant corona on inhaled nanoparticles to operate in the lung system. Nano Today 2023, 52. [Google Scholar] [CrossRef]
- Ho, D.-K.; Nichols, B.L.; Edgar, K.J.; Murgia, X.; Loretz, B.; Lehr, C.-M. Challenges and strategies in drug delivery systems for treatment of pulmonary infections. Eur. J. Pharm. Biopharm. 2019, 144, 110–124. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.T.; Lee, H.; Kim, J.; Jung, Y.; Choi, E.; Jeong, J.H.; Jeong, J.-H.; Lee, J.H.; Youn, Y.S. Alveolar macrophage phagocytosis-evading inhaled microgels incorporating nintedanib-PLGA nanoparticles and pirfenidone-liposomes for improved treatment of pulmonary fibrosis. Bioact. Mater. 2024, 33, 262–278. [Google Scholar] [CrossRef]
- Subramanian, S.; Khan, I.; Korale, O.; Alhnan, M.A.; Ahmed, W.; Najlah, M.; Taylor, K.M.; Elhissi, A. A simple approach to predict the stability of phospholipid vesicles to nebulization without performing aerosolization studies. Int. J. Pharm. 2016, 502, 18–27. [Google Scholar] [CrossRef]
- Khan, I.; Apostolou, M.; Bnyan, R.; Houacine, C.; Elhissi, A.; Yousaf, S.S. Paclitaxel-loaded micro or nano transfersome formulation into novel tablets for pulmonary drug delivery via nebulization. Int. J. Pharm. 2020, 575, 118919. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, X.; Xue, J.; Chai, J.; Qin, L.; Guan, J.; Zhang, X.; Mao, S. Exploring the intrinsic micro-/nanoparticle size on their in vivo fate after lung delivery. J. Control. Release 2022, 347, 435–448. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Qin, L.; Song, R.; Su, J.; Yuan, Y.; Zhang, X.; Mao, S. Elucidating inhaled liposome surface charge on its interaction with biological barriers in the lung. Eur. J. Pharm. Biopharm. 2022, 172, 101–111. [Google Scholar] [CrossRef]
- Zhao, J.; Su, J.; Qin, L.; Zhang, X.; Mao, S. Exploring the influence of inhaled liposome membrane fluidity on its interaction with pulmonary physiological barriers. Biomater. Sci. 2020, 8, 6786–6797. [Google Scholar] [CrossRef]
- Liu, Q.; Xue, J.; Zhang, X.; Chai, J.; Qin, L.; Guan, J.; Zhang, X.; Mao, S. The influence of a biomimetic pulmonary surfactant modification on the in vivo fate of nanoparticles in the lung. Acta Biomater. 2022, 147, 391–402. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, X.; Zhang, Y.; Ye, J.; Wang, H.-L.; Xia, X.; Liu, Y. Mechanisms of deformable nanovesicles based on insulin-phospholipid complex for enhancing buccal delivery of insulin. Int. J. Nanomed. 2018, 13, 7319–7331. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Guo, Y.; Xu, Y.; Meng, Y.; Zhang, X.; Xia, X.; Liu, Y. Factors affecting the buccal delivery of deformable nanovesicles based on insulin–phospholipid complex: An in vivo investigation. Drug Deliv. 2020, 27, 900–908. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Gong, T.; Fu, H.; Wang, C.; Wang, X.; Chen, Q.; Zhang, Q.; He, Q.; Zhang, Z. Solid lipid nanoparticles for pulmonary delivery of insulin. Int. J. Pharm. 2008, 356, 333–344. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Zhang, R.; Beng, H.; Deng, L.; Ke, Q.; Tan, W. Effects of flow pattern, device and formulation on particle size distribution of nebulized aerosol. Int. J. Pharm. 2019, 560, 35–46. [Google Scholar] [CrossRef]
- Lombry, C.; Edwards, D.A.; Préat, V.; Vanbever, R. Alveolar macrophages are a primary barrier to pulmonary absorption of macromolecules. Am. J. Physiol. Cell. Mol. Physiol. 2004, 286, L1002–L1008. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Wang, C.; Ren, S.; Pan, J.; Wang, Y.; Shen, Y.; Zeng, Z.; Cui, H.; Zhao, X. Versatile Oral Insulin Delivery Nanosystems: From Materials to Nanostructures. Int. J. Mol. Sci. 2022, 23, 3362. [Google Scholar] [CrossRef] [PubMed]
- Dailey, G.; Ahmad, A.; Polsky, S.; Shah, V. A novel option for prandial insulin therapy: Inhaled insulin. Postgrad. Med. 2016, 128, 839–847. [Google Scholar] [CrossRef] [PubMed]
- Patel, B.; Gupta, N.; Ahsan, F. Particle engineering to enhance or lessen particle uptake by alveolar macrophages and to in-fluence the therapeutic outcome. Eur. J. Pharm. Biopharm. 2015, 89, 163–174. [Google Scholar] [CrossRef]
- Soni, S.S.; Kim, K.M.; Sarkar, B.; Rodell, C.B. Uptake of Cyclodextrin Nanoparticles by Macrophages is Dependent on Particle Size and Receptor-Mediated Interactions. ACS Appl. Bio Mater. 2024; ahead of print. [Google Scholar] [CrossRef]
- Flament, M.; Leterme, P.; Burnouf, T.; Gayot, A. Jet nebulisation: Influence of dynamic conditions and nebuliser on nebulisation quality. Application to the α 1 protease inhibitor. Int. J. Pharm. 1997, 148, 93–101. [Google Scholar] [CrossRef]
- Ngan, C.L.; Asmawi, A.A. Lipid-based pulmonary delivery system: A review and future considerations of formulation strategies and limitations. Drug Deliv. Transl. Res. 2018, 8, 1527–1544. [Google Scholar] [CrossRef] [PubMed]
- Sun, D.; Zhang, G.; Xie, M.; Wang, Y.; Liang, X.; Tu, M.; Su, Z.; Zeng, R. Softness enhanced macrophage-mediated therapy of inhaled apoptotic-cell-inspired nanosystems for acute lung injury. J. Nanobiotechnol. 2023, 21, 172. [Google Scholar] [CrossRef]
- Wang, W.; Yang, B.; Huang, Z.; Huang, Y.; Hu, P.; Pan, X.; Wu, C. Investigating the Effect of Particle Size on Cellular Uptake by Aggregation-Caused Quenching Probe–Encapsulating Solid Lipid Nanoparticles, Inhaled. J. Pharm. Innov. 2021, 17, 1109–1115. [Google Scholar] [CrossRef]







| Amount of Edge Activators | Size (nm) | Zeta Potential (mv) | EE (%) | DI (μg/cm2/s) |
|---|---|---|---|---|
| 0% | 102.57 ± 0.21 | −45.68 ± 0.41 | 64.04 ± 0.22 | 6.56 ± 0.66 |
| 1.8% | 101.57 ± 0.31 | −40.18 ± 0.08 | 79.17 ± 1.71 | 29.75 ± 0.28 |
| 2.5% | 83.87 ± 0.71 | −35.85 ± 0.56 | 83.97 ± 0.54 | 39.30 ± 0.99 |
| Target Size | Size (nm) | Zeta Potential (mv) | EE (%) |
|---|---|---|---|
| 80 nm | 83.87 ± 0.71 | −35.85 ± 0.56 | 83.97 ± 0.54 |
| 150 nm | 150.60 ± 1.55 | −47.33 ± 0.32 | 86.926 ± 0.18 |
| 230 nm | 238.70 ± 1.80 | −46.13 ± 0.08 | 88.06 ± 2.64 |
| 500 nm | 477.83 ± 11.21 | −49.09 ± 0.31 | 88.31 ± 4.54 |
| Drug Load | Size (nm) | Zeta Potential (mv) | EE (%) |
|---|---|---|---|
| 3 mg/mL | 83.87 ± 0.71 | −35.85 ± 0.56 | 83.97 ± 0.54 |
| 4 mg/mL | 89.13 ± 0.15 | −36.04 ± 0.43 | 84.47 ± 0.43 |
| 5 mg/mL | 85.00 ± 0.40 | −35.00 ± 0.38 | 82.85 ± 5.59 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yu, J.; Meng, Y.; Wen, Z.; Jiang, Y.; Guo, Y.; Du, S.; Liu, Y.; Xia, X. Investigation of Factors Influencing the Effectiveness of Deformable Nanovesicles for Insulin Nebulization Inhalation. Pharmaceutics 2024, 16, 879. https://doi.org/10.3390/pharmaceutics16070879
Yu J, Meng Y, Wen Z, Jiang Y, Guo Y, Du S, Liu Y, Xia X. Investigation of Factors Influencing the Effectiveness of Deformable Nanovesicles for Insulin Nebulization Inhalation. Pharmaceutics. 2024; 16(7):879. https://doi.org/10.3390/pharmaceutics16070879
Chicago/Turabian StyleYu, Jinghan, Yingying Meng, Zhiyang Wen, Yu Jiang, Yiyue Guo, Simeng Du, Yuling Liu, and Xuejun Xia. 2024. "Investigation of Factors Influencing the Effectiveness of Deformable Nanovesicles for Insulin Nebulization Inhalation" Pharmaceutics 16, no. 7: 879. https://doi.org/10.3390/pharmaceutics16070879
APA StyleYu, J., Meng, Y., Wen, Z., Jiang, Y., Guo, Y., Du, S., Liu, Y., & Xia, X. (2024). Investigation of Factors Influencing the Effectiveness of Deformable Nanovesicles for Insulin Nebulization Inhalation. Pharmaceutics, 16(7), 879. https://doi.org/10.3390/pharmaceutics16070879







