Abstract
Decentralization is considered an important component of participatory democracy. However, despite its widespread implementation in the healthcare sector, its impact on health systems’ performance remains unclear. Using a theoretical framework based on the World Health Organization’s five decentralization variables—geography and sociodemographics, organization of political processes, functions and economic weight, steering, and control—we conducted a scoping review to unveil causal mechanisms linking each feature to equity, efficiency, and effectiveness. Following the PRISMA protocol, 1627 articles were screened, and 63 were selected for data analysis, with a focus on middle- and high-income countries. The findings show that the most frequently discussed forms of decentralization are fiscal and administrative, with a primary focus on how governance mechanisms affect equity and efficiency. The effects of decentralized healthcare governance on equity, efficiency, and effectiveness are diverse and contingent on contextual factors and the implementation processes. The spatial context (geography) of decentralization negatively impacts equity, and steering strongly affects effectiveness. Functions and economic weight significantly influence efficiency, albeit with variability. Overall, decentralization falls short of delivering substantial healthcare system benefits, although this depends on contextual factors.
1. Introduction
Decentralization grants local governments decision-making autonomy in policy design and assigns a wide range of competencies that can significantly impact the performance of healthcare systems. The delegation of power and authority may manifest in various forms, leading to different types of decentralization, namely, political, administrative, or fiscal. However, there remains little consensus in the literature regarding their precise definitions [1,2].
Political decentralization involves the central administration conceding decision-making authority to local governments. Administrative decentralization pertains to the transfer of operational responsibilities, including the allocation of specific tasks and corresponding funding, without full delegation of decision-making power. Finally, fiscal decentralization entails the transfer of expenditure and revenue responsibilities from the central to local governments [3,4].
Within the healthcare sector, the evidence on the benefits of decentralization is far from conclusive. Three theories, which underpin the rationale for decentralization, help us grasp its impacts on healthcare systems [5,6]. Based on Tiebout’s [7] seminal work on local public goods, the “voting with your feet” theory elucidates how decentralization can either exacerbate or mitigate existing disparities in resource distribution, as people are able or not to choose their residency based on potential fiscal benefits or services. Drawing on Arrow’s [8] notion of information asymmetry in healthcare relations, the “close to ground” theory contends that governance closer to citizens enables the collection of local insights, leading decentralization to offer more tailored responses to community needs. Lastly, based on Hurwicz’s [9] work on governance, the “watching the watchers” theory highlights how decentralization fosters numerous interrelationships and mutual accountability among various stakeholders, so that the decentralization benefits depend on the accountability of local decision makers.
Applying these theories to the analysis of decentralization in healthcare offers a means to identify its advantages and disadvantages, despite the ongoing controversy in the literature [5,6]. Some scholars argue that decentralization contributes to enhanced equity in healthcare, improved service efficiency, effectiveness, and resource utilization [2,3]. Conversely, other studies point to negative consequences, including increased spending, complexity within sectors, augmented socio-territorial inequalities, and multi-level coordination and funding challenges [1,4,10].
In the realm of health policy decision making, considerations of equity, efficiency, and effectiveness typically play a central role [11]. On the one hand, this involves ensuring equal access to specific goods and services for individuals with equal needs (equity); on the other hand, it requires the optimization of existing resources (efficiency). Policymakers must also ensure that policies align with desired health objectives (effectiveness). An understanding of how policies within decentralized processes are designed to align with these objectives enables the identification of the impacts of health decentralization [5]. Moreover, knowledge of these impacts proves to be crucial for the sustainability of health systems, aiming to improve the population’s health and perform healthcare delivery functions that incorporate these principles [12]. This understanding serves as a foundation for informed decision making in the development and implementation of health policies.
More specifically, equity involves the fair distribution of existing resources with the goal of preventing citizens from facing differential treatment based on factors such as their place of residence, socioeconomic status, and gender, among others [13]. Equity, in this context, underscores a commitment to reducing and ultimately eliminating disparities in health and its determinants [14], focusing on the perspective of needs and the assurance of equal opportunities [2]. Efficiency, on the other hand, refers to the judicious use of resources, aiming to maximize health benefits for society while minimizing healthcare costs [15]. Efficiency can be divided into two categories: technical efficiency, which assesses the relationship between resources and results, shedding light on how resources are utilized, and allocative efficiency, which considers the effectiveness of resource allocation and distribution of results within the community. Effectiveness, in turn, entails the establishment of appropriate measures, interventions, or initiatives to achieve the intended results or objectives with the available resources. This reflects the degree to which actions or policies being implemented impact the health of individuals [16].
The implementation of decentralization in healthcare, however, varies across different countries, resulting in diverse outcomes and impacts. For instance, the process of implementing decentralization in Italy covered the entire health sector. Reforms aimed at strengthening the regions were adopted with a dual focus: bolstering the reimbursement system on the one hand and fortifying the political system on the other. Although a carefully thought-out process, varying interpretations between regions compromised the achievement of equity. In turn, the decentralization process to the regions in Norway was radical and occurred swiftly. Administrative and management components were decentralized to the regional level, but the funding model remained centralized. In comparison to the Italian case, the extent of decentralization in Norway was more limited, encompassing only hospital healthcare [1].
Furthermore, there is a significant gap in our understanding of how decentralization affects the equity, efficiency, and effectiveness of health systems in a wide-ranging manner. The aim of this study is to provide a comprehensive overview of the evidence that informs healthcare decentralization practices and its impacts, supported by a conceptual model.
To achieve this objective, we designed a scoping review to identify available evidence, clarify key concepts, and examine research methodologies in this field [17]. For this review, hypotheses were developed based on the World Health Organization’s [1] five decentralization variables—geography and sociodemographics, organization of political processes, functions and economic weight, steering, and control—to uncover the causal mechanisms of each variable on equity, efficiency, and effectiveness.
Each decentralization variable is defined in terms of its potential impact when decentralization is implemented. “Geography and sociodemographics” indicates that the impacts of decentralization vary according to the size and socio-economic composition of the decentralized entities. “Organization of political processes” refers to the formal decision-making structures, the potential for citizen participation, and the proximity between governance and individuals. “Functions and economic weight” involve the transfer of power over fiscal decisions to local governments. “Steering” corresponds to the presence or absence of central coordination in defining objectives and guidelines for local governments. Finally, “control” corresponds to the presence or absence of monitoring and evaluation instruments by the central administration to gather information on how decisions are implemented at decentralized levels [1].
To address the specific objective of this scoping review, we formulated the hypotheses presented in Table 1.

Table 1.
Hypotheses formulated.
The remainder of this paper is structured as follows. The next section presents the methods employed in this scoping review, including the protocol and the research process. Subsequently, we present the results according to different analytical criteria. Finally, we provide a comprehensive discussion of the findings, along with key conclusions, a discussion of the inherent research limitations, and suggestions for future research avenues.
2. Materials and Methods
2.1. Method
This scoping review used the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) protocol, a model originally developed in the context of health sciences to enhance the reliability and replicability of literature reviews and meta-analyses [18].
2.2. Search Strategy
The identification of publications resulted from research conducted in January 2023 using two multidisciplinary databases: Scopus and Web of Science. We employed the following keywords: (decentrali*) AND (regional* OR “regional power” OR “regional government*” OR municipal* OR “local power” OR “local government*”) AND (health OR healthcare OR “health service*” OR “health center*” OR “health care”).
The search was constrained by language (English and Portuguese), document type, and time frame: (i) for Scopus, we selected “article” + “book chapter” + “conference article”, and (ii) for Web of Science, we chose “article” + “book chapter” + “procedural article”, with a time horizon of 2001–2022.
2.3. Inclusion and Exclusion Criteria
We included all publications that addressed relationships involving quantitative and qualitative empirical results regarding decentralization and its impact on equity, efficiency, and effectiveness in the context of healthcare. Furthermore, publications were only included if they evaluated this process concerning the entire healthcare system, while those focusing solely on a particular service or specific population group were excluded. Only studies in English from middle- and high-income countries that assessed any of the three types of decentralization between 2001 and 2022 were incorporated. Opinion articles, theses, or other non-scientific journal publications were not considered.
Regarding exclusion criteria, articles not published in English, lacking an abstract, or not providing access to the full text were excluded. Additionally, systematic literature reviews, theoretical studies without empirical evidence, and those referring to low- and/or low-middle-income countries were excluded, as well as articles that did not address the concepts under analysis or were not relevant to the objective of this scoping review.
2.4. Study Selection and Data Extraction
The selection of publications was conducted in three stages: (i) initially, duplicate publications and those lacking abstracts were eliminated; (ii) subsequently, publications’ titles and abstracts were assessed based on the inclusion and exclusion criteria to exclude irrelevant publications; (iii) finally, the full texts of the eligible publications were retrieved and reviewed for inclusion. All these stages were executed using the Rayyan software.
Following this, a thorough analysis of the selected publications’ full texts was carried out. Data from each included publication were extracted using a data extraction tool that encompassed the following elements: (i) publication authors, title, and year of publication; (ii) countries under study; (iii) objective of the study; (iv) type of decentralization; (v) outcomes analyzed (equity, efficiency, and effectiveness); (vi) decentralization variables; (vii) data collection methods; (viii) results; and (ix) conclusions.
Throughout each stage of the selection and analysis process, all publications were reviewed by a minimum of two authors following the four-eyes principle [19], and any disagreements were resolved through consensus.
3. Results
3.1. Study Selection
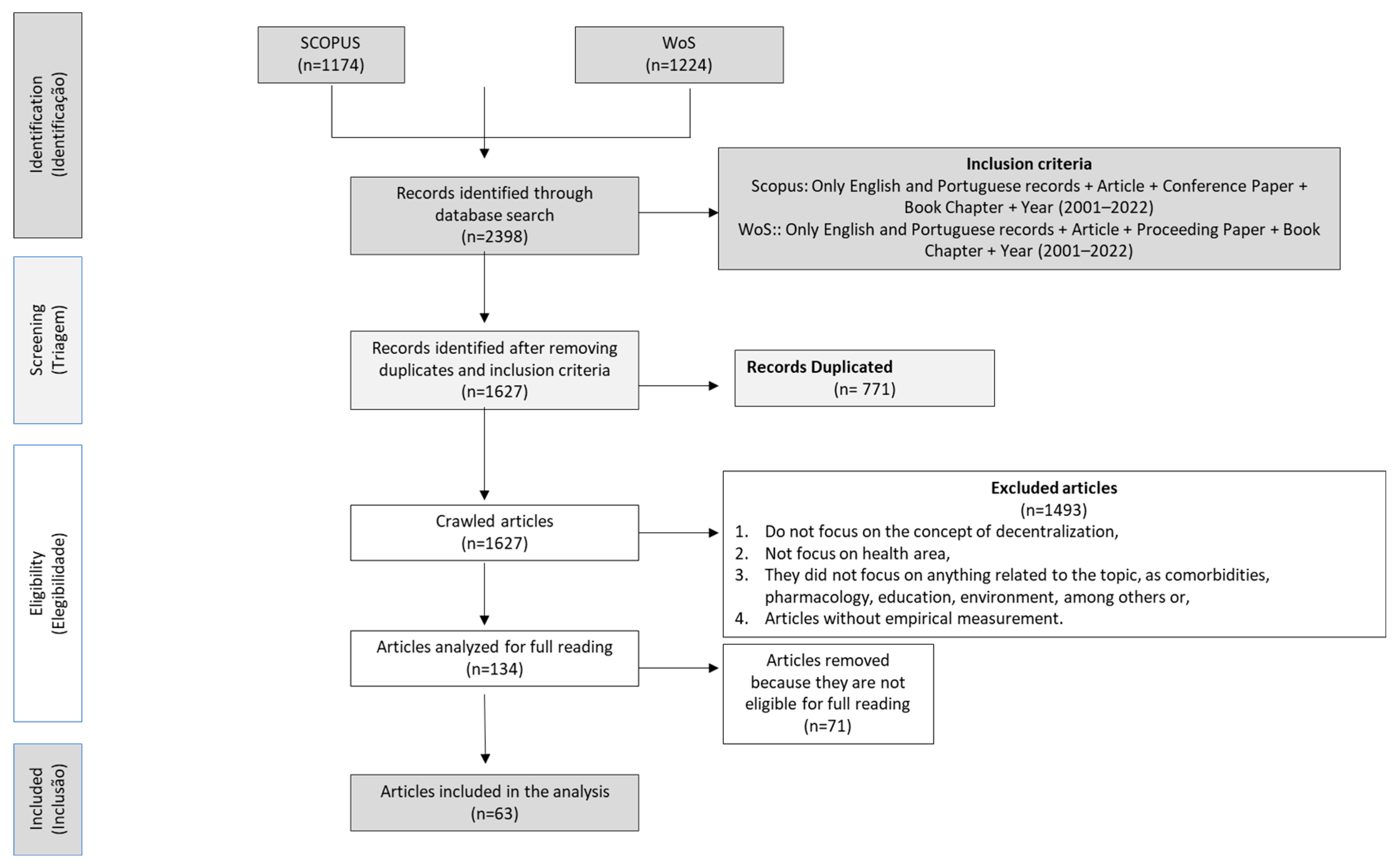
The initial search across databases yielded a total of 2398 publications, with 1174 found in the SCOPUS database and 1224 in the Web of Science.
After removing duplicate publications (n = 771 publications), 1627 publications underwent analyses of the title, keywords, and abstract. Following these criteria, 1493 publications were excluded as they did not meet the inclusion and exclusion criteria, i.e., they were not published in English, were literature reviews, or were unrelated to health decentralization.
Subsequently, the full texts of the remaining 134 publications were examined, and 71 publications were excluded either due to not meeting the inclusion criteria or being inaccessible. In these instances, attempts were made to contact the authors for full access to the publications, without response. Consequently, 63 articles were deemed eligible for this systematic review, as illustrated in the PRISMA diagram below (Figure 1).
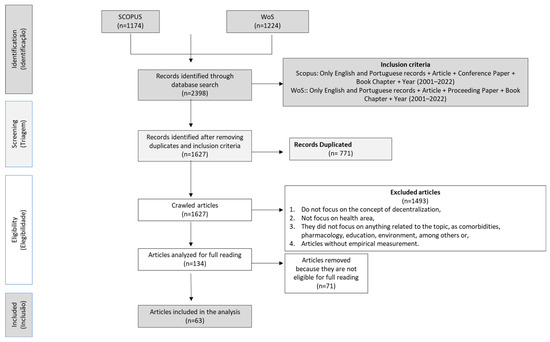
Figure 1.
PRISMA flowchart.
3.2. Characterization of the Studies
3.2.1. Evolution of Publications by Year
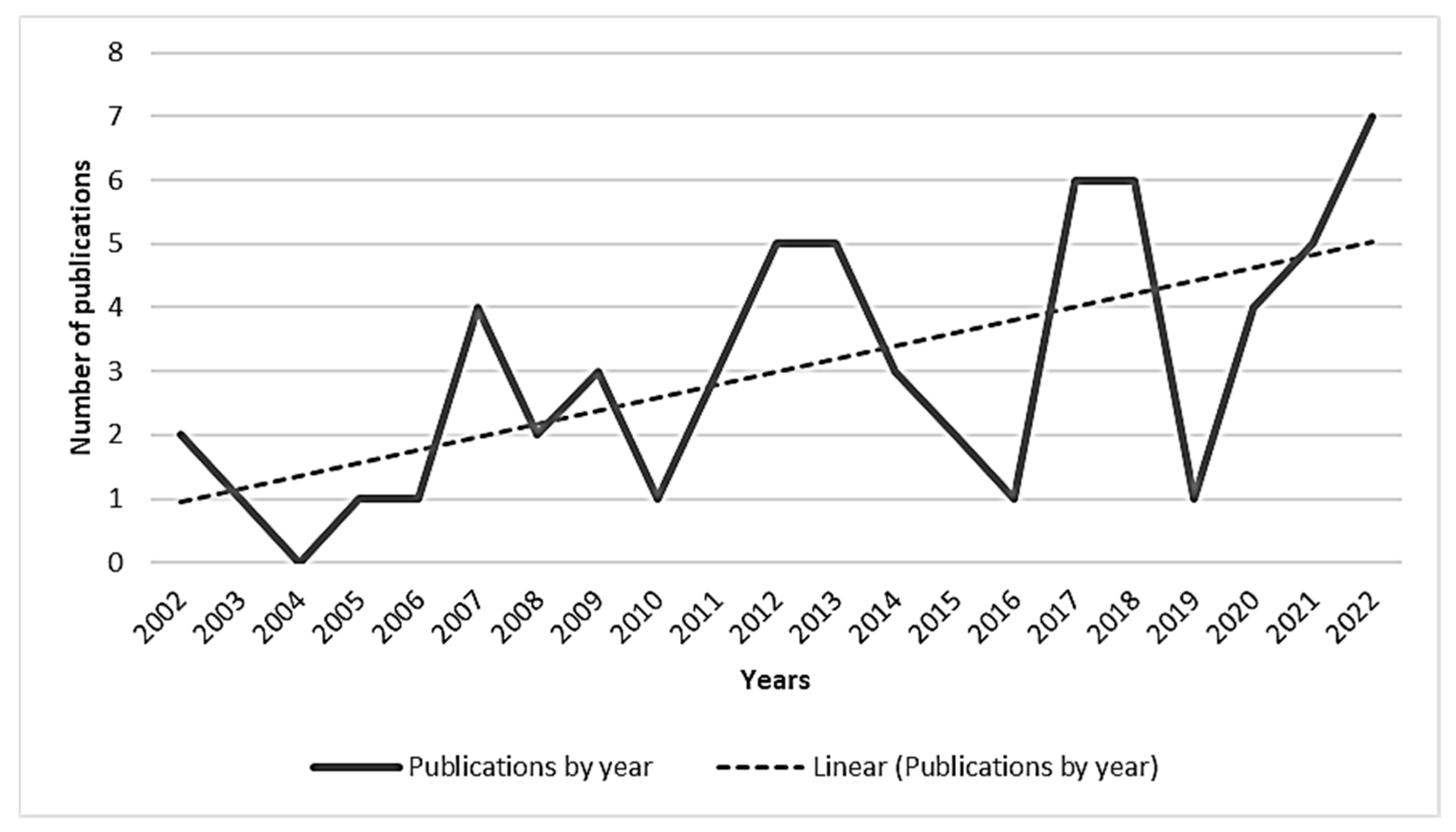
The articles included in the literature review spanned from 2002 (two articles) to 2022 (seven articles). Figure 2 illustrates an increasing trend in publications, notably surging after 2017. Despite a decline in 2019, 46% of publications emerged after that date.
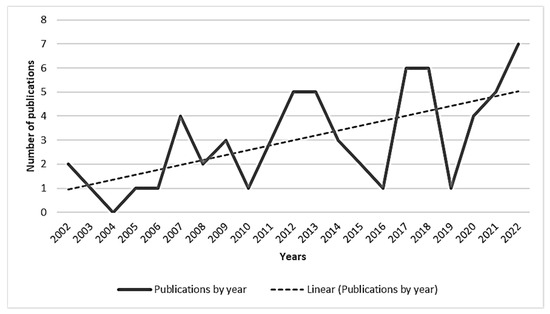
Figure 2.
Number of publications per year.
3.2.2. Scientific Journal Ranking
The analyzed sample comprises 63 publications from scientific journals. Notably, eight journals published two or more articles: Health Policy, Social Science and Medicine, Ciência e Saúde Coletiva, Cadernos de Saúde Publica, Saúde e Sociedade, International Journal of Health Planning and Management, European Journal of Health Economics, and Health Services Management Research (Table 2).

Table 2.
Journals with two or more articles published.
3.2.3. Geographical Distribution
Table 3 portrays the distribution of included studies by continents. Europe and America contributed significantly with 35 and 24 studies, respectively (66.7% and 42.9%). In contrast, Asia had a marginal contribution with five studies.

Table 3.
Geographical distribution per continent.
Further geographical analysis reveals a concentration of studies in European countries, particularly Italy (25.4%, n = 14) and Spain (15.9%, n = 10), historically characterized by high levels of decentralization in the health sector. In America, Brazil stands out with 28.6% of the articles (n = 17) (Table 4).

Table 4.
Geographical distribution per country.
3.2.4. Institutions of Authors, Degree of Internationalization, and Interdisciplinarity
Table 5 and Table 6 show that only 13 articles involved multinational teams, while most articles focused on studies conducted within a single country and authored by individuals from a single institution. The primary affiliation of authors was with universities, and collaboration was predominant, with one exception where the authors were affiliated with the World Bank and UNICEF. Interdisciplinarity was notably prevalent, particularly among authors from Italy and the United Kingdom.

Table 5.
Research degree of internationalization and interdisciplinarity.

Table 6.
Examples of articles illustrating the internationalization and interdisciplinarity in research. Research degree of internationalization and interdisciplinarity.
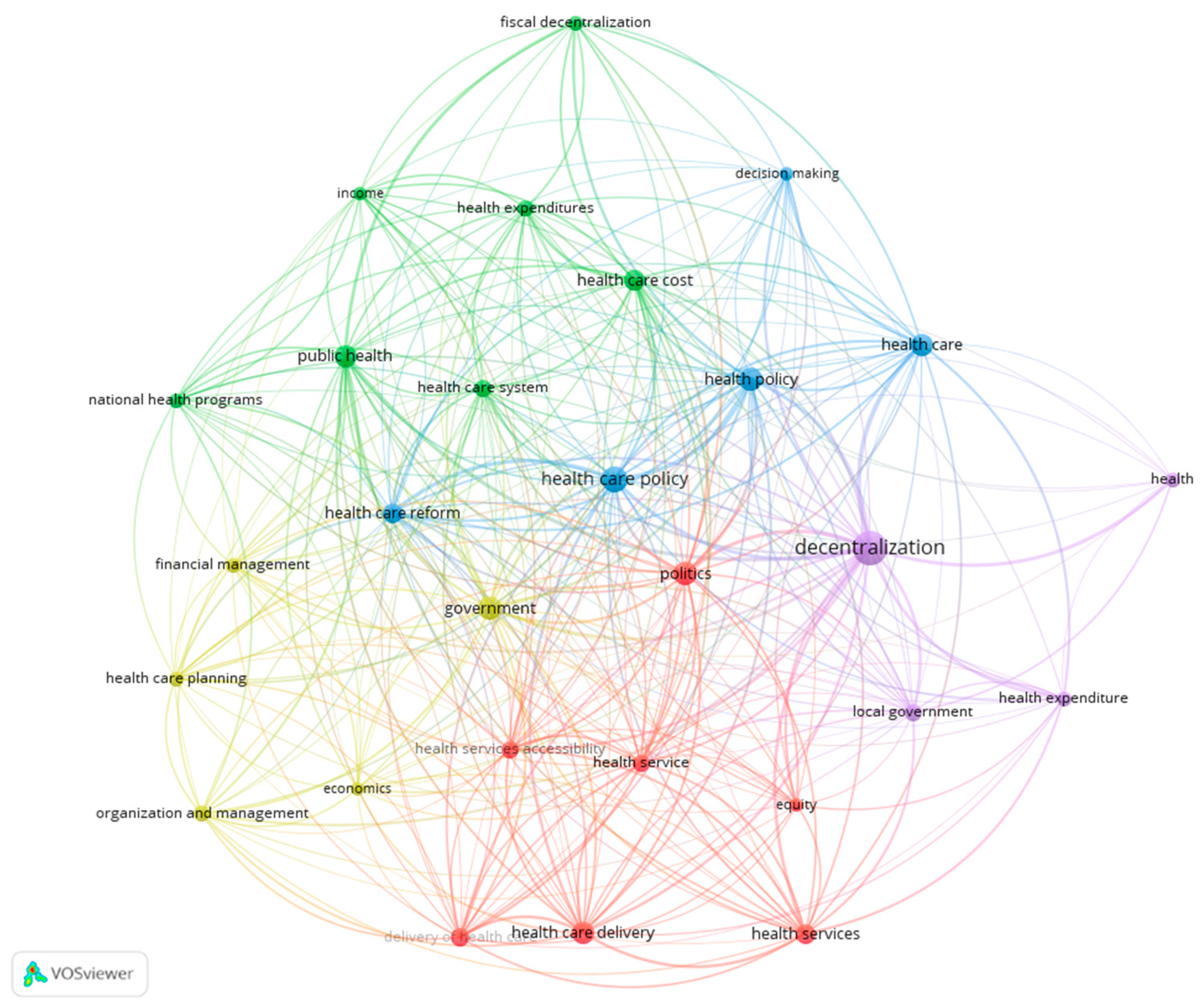
3.2.5. Keyword Analysis with Co-Occurrence
Keyword co-occurrence reflects the research hotspots in the analyzed publications, providing support for data analysis. In this context, the content was examined by analyzing the distribution of keywords. The keyword co-occurrence threshold was set at five, and 28 items were visualized using the VOSviewer software (version 1.6.20) (Figure 3). The size of the nodes and words represents the weights of the nodes. The larger the node and word, the greater the weight. Additionally, the distance between two nodes reflects the strength of the relation between them.
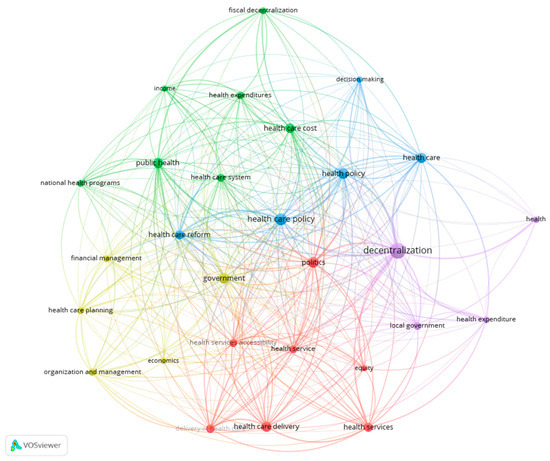
Figure 3.
Keyword co-occurrence network.
VOSviewer categorized the keywords into five distinct colored clusters. The keyword “decentralization” holds the highest frequency (32), followed by “healthcare policy” (18), “politics” (15), “health policy” (15), and “government” (15). The purple cluster encompasses keywords particularly in the field of decentralization and local government. In turn, the blue cluster includes keywords mainly related to health policies. The green cluster, on the other hand, is associated with keywords focusing especially on the financing of health systems, while the red cluster centers mainly on the provision of healthcare, accessibility to care, and equity. Lastly, the yellow cluster’s keywords concentrate on the organization and management of health services. Concerning the links between the clusters, multiple interconnections exist among all of them. However, the purple cluster exhibits the strongest connections, followed by the blue and red clusters.
3.2.6. Type of Decentralized Healthcare
Of the included studies, 49 (77.8%) pertained to the general scope of decentralized healthcare. In terms of specific healthcare provision, nine articles (14.3%) focused on primary healthcare, four articles (6.3%) on hospital healthcare, and one article (1.6%) simultaneously addressed both primary and hospital healthcare (Table 7).

Table 7.
Number of publications by type of decentralized healthcare.
3.2.7. Entities to Which Decentralization Occurred
Concerning the entities affected by decentralization, most studies (49.2%, n = 31) analyzed decentralization to regional health authorities, followed by municipalities (42.9%, n = 27). Approximately 6.3% (n = 4) examined decentralization to regions, and 3.2% (n = 2) simultaneously investigated decentralization to both municipalities and regions (Table 8).

Table 8.
Number of publications based on the nature of entities affected by decentralization.
3.2.8. Type of Decentralization
Table 9 indicates that the authors primarily focused on fiscal decentralization (65.1%, n = 41) and administrative decentralization (44.4%, n = 28). Political decentralization was less prevalent, with only twelve articles (19.0%).

Table 9.
Number of publications by main types of decentralization.
A closer examination reveals that while authors often concentrated on a single type of decentralization, broader decentralization processes occurred in the countries under study, encompassing other type(s) of decentralization. The types of decentralization evaluated in the articles are presented in Table 10.

Table 10.
Number of publications by type of decentralization in country and evaluated in article.
3.2.9. Outcomes
The primary focus of the publications under review was on the impact of decentralized governance on health, with an emphasis on equity (n = 28, 44.4%) and efficiency (n = 24, 38.1%). Less attention was given in the literature to the impact on effectiveness (n = 19, 30.2%). Concerning equity, the attention was on access to healthcare, efficiency in health spending, and effectiveness in implementing decentralization policies (Table 11).

Table 11.
Number of publications by type of outcomes.
3.2.10. Decentralization Variables
Among the five decentralization variables, the literature placed greater emphasis on functions and economic weight (n = 27, 42.9%) and the organization of political processes (n = 13, 20.6%), as illustrated in Table 12. Subsequently, 11 studies focused on the decentralization variables of geography and sociodemographics (17.5%) and steering (17.5%), while only six studies concentrated on the decentralization variable of evaluation (9.5%).

Table 12.
Type of decentralization variables found in the articles.
3.2.11. Instruments of Data Collection
The predominant methodology in most studies was quantitative, with 33 articles using aggregated macro data about the country, regions, or municipalities, primarily derived from longitudinal analyses (n = 25, 39.7%). In contrast, a significantly smaller number, six articles, adopted a qualitative approach, employing interviews and document analysis (9.5%). Notably, the most used method involved a combination of interviews and document analysis, indicating the adoption of a mixed methodology, incorporating both qualitative and quantitative methods (Table 13).

Table 13.
Instruments of data collection.
Appendix A presents more detailed information on the data collection instruments used in each study.
3.2.12. Impact of Decentralization on Outcomes
Table 14 highlights the varied impacts of decentralization in health on equity, efficiency, and effectiveness. The results tended to be more positive than negative in terms of efficiency (n = 15, 23.8%), in contrast to equity (n = 17, 27.0%) and effectiveness (n = 10, 15.9%).

Table 14.
Number of publications by impact of decentralization on outcomes.
4. Discussion
In this section, we discuss the results and delve into the hypotheses formulated initially to understand the impacts of decentralization on the equity, efficiency, and effectiveness of the health system. While this theme exhibits some consensus in the literature, verified by the confirmation of some hypotheses, or parts of them, it also introduces ambiguous evidence for some of the decentralization variables under study.
The literature retrieved from the two databases echoed the growing importance of the health decentralization topic. There was a noticeable increase in the number of publications after 2019, in particular in the years following the COVID-19 pandemic. It is worth noticing that this context highlighted the leading role that local governments can play in the field of public health, revealing their capacity to assume competencies in this area.
Among the studies analyzed, research held in countries historically with high levels of decentralization stood out, and more than half of the articles focused on fiscal decentralization. These results may be attributed to the fact that this type of decentralization grants greater decision-making autonomy to local governments. They are responsible for decisions regarding revenues and expenses, allowing them to use resources as they see fit. In terms of decentralization variables, although such results can be expected, with functions, economic weight, and organization of political processes being the most preponderant, the remaining variables, despite their inherent complexity, require careful attention to perceive their impacts.
4.1. Equity in Access and Use
The EQ.GEO1 hypothesis finds support in the literature reviewed. These studies revealed that decentralization yields heterogeneous and differentiated responses, with more favorable effects in regions with higher development compared to less developed ones. The impacts varied based on the level of development of subnational governments, their available resources, population characteristics, the organization and management of health systems, and the resources redistributed in the decentralization process itself [41,56]. In this regard, Assis [41], focusing on Brazil, concluded that fiscal decentralization reduced infant mortality rates. However, the impacts varied across regions, contingent upon existing territorial and economic development. More significant effects were observed in the more developed regions (south), while the northern regions, characterized by disadvantaged cities lacking basic infrastructure and fewer resources, experienced less pronounced effects of decentralization. In turn, according to the findings in article [52], decentralization exacerbated existing geographic disparities in access to healthcare among Italian regions. Challenges related to healthcare accessibility, such as cost or transport issues, were more prevalent in the south, particularly in less developed regions. This evidence underscores the critical nature of healthcare accessibility, encompassing factors like the distance required to travel for care and the corresponding travel time.
The subsequent hypothesis, EQ.OPP1, also finds validation in the literature. The included studies indicated that designing policies without central government regulation and citizen involvement exacerbates inequalities between regions, resulting in adverse effects on the health of the population. The fragmentation of the health system in terms of financing and service provision, along with the standardization of the use of health services without consideration of local needs, generates inequities in healthcare [67,76]. Taking a governance perspective, [72] asserted that various attempts at decentralization in the Greek health system failed due to a lack of state support and political will. The limited transfer of administrative powers and constant discontinuity in health policies during political changes influenced the performance of regional health services, failing to reduce inequalities between local governments or improve the quality of services provided.
Thirteen articles report on equity in healthcare financing, presenting mixed results regarding the EQ.FE1 hypothesis, which was partially confirmed. Some studies indicated that the redistribution of responsibilities and financial resources did not lead to an increase in health inequalities or disparities in healthcare access; instead, it reduced them. These studies argued that prevailing inequalities stem from income disparities among the population rather than differences in health financing [24] and variations in the management of health systems [25]. Additionally, refs. [21,55] concluded that while decentralization can be a means to achieve a more equitable allocation of resources, it requires specific political conditions and mechanisms tailored to existing contexts.
Conversely, an understanding of what municipalities perceive as their needs is crucial to comprehend how they allocate resources. In this context, the study on Colombia and Chile [21] asserted that employing an intergovernmental transfer allocation formula, based on population, facilitated the equitable distribution of national resources among local governments during the health decentralization process. Consequently, in terms of financial resource distribution, the interests of the recipient (local government) took precedence over those of the donor (national level interests) [83].
Other studies, nonetheless, suggested that decentralization had adverse effects on resource availability and healthcare access, leading to increased inequalities among population groups. Inappropriately redistributed financial resources resulted in a fragmented and unequal health system, where the levels of resource availability, utilization, and accessibility, as well as the extent of cost containment, matched with the wealth of the region [23]. Wealthier regions fared better, possessing greater capacity to expand their own sources of financing, thereby widening the gap between prosperous and impoverished regions [22].
Although some studies noted that the decentralization of financial resources contributed to reducing infant mortality rates [32,41], strengthened the decision-making capabilities of subnational governments [78], and did not affect inequalities between regions [56], they emphasized that the varied responses observed were influenced by the developmental level of each region and how financial resources were allocated. For instance, the study on Italy [56] mentioned that the fiscal decentralization reform contributed to containing existing inequalities, but benefits were higher in richer than in less developed regions. In turn, the results of [32] regarding Colombia indicated that decentralization had a positive effect on reducing infant mortality, but these benefits were higher in richer regions.
Regarding the EQ.STRE1 hypothesis, studies emphasized that the central government’s attribution of more responsibilities and resources to municipalities did not mitigate existing inequalities [43,54]. The transfer of skills lacked accompanying guidelines, and there was no planning for resource use based on local needs. The absence of coordination between government levels resulted in policies’ heterogeneity compromising equity. In Sweden, for instance, a distinct decentralization model in terms of regulations gave rise to reforms, such as the patient choice reform, without a national standard in practice. Consequently, with only recommendations in place, a soft governance, and a lack of guidelines for policy adoption, inequities arose between regions in terms of patients’ access to health services [80]. These results underscore the importance of having guidelines at various stages of the decentralization process.
The last hypothesis (EQ.EVAL1) was confirmed by two articles under study asserting that the adoption of evaluation mechanisms promoted the performance of decentralized health systems [50,77]. In the case of Italy, for example, the use of these mechanisms revealed notable regional disparities between the south and the north, with the former exhibiting poorer performance both in the provision of health services and in health outcomes [50]. Moreover, this knowledge empowered local governments to gauge whether the implemented measures were achieving the intended results and identify influencing factors. Consequently, local governments can formulate and implement measures to minimize identified problems.
4.2. Efficiency
In terms of efficiency, the hypothesis EFIC.GEO2 could not be validated due to evidence limited to a single article. Ferrario and Zanardi [57] argued that smaller regions with fewer resources had limited capacity to invest in adequate services, incurring unnecessary health expenditures and having resources only to cover basic expenses. Conversely, affluent regions could allocate resources to meet existing needs but, in some cases, may have spent more than necessary. Despite finding that larger regions incurred higher expenditures, there is insufficient evidence regarding efficiency; the data do not determine whether the expenses aligned with actual needs.
Considering hypothesis EFIC.OPP2, the studies disclosed that citizens’ preferences differed both between and within regions. Decentralizing decisions to levels closer to citizens was deemed more efficient. The proximity between governing bodies and citizens enables subnational governments to identify and comprehend citizens’ preferences for health services. This understanding is crucial in resource allocation, maximizing the overall well-being of the population [27]. Policymakers play a pivotal role in developing policies, and when the average cost of providing care aligns with population characteristics and healthcare structures, regions can enhance the efficiency of their healthcare system [26,66]. Thus, the aforementioned hypothesis was confirmed.
Fourteen articles related to the decentralization regarding functions and economic weight displayed controversial results, partially validating the EFIC.FE2 hypothesis. Some articles asserted that allocating financial resources to local governments contributed to efficient service provision. This was achieved through the judicious use of resources to enhance population health, reinforcing policy viability, and promoting transparency and responsibility in expense allocation [30,48]. Sun and Andrews [68] added that increased efficiency in using financial resources may be more apparent in more developed regions thanks to their capacity to develop mechanisms motivating proper resource use. Regarding this matter, [30] noted that fiscal decentralization in Spain increased regions’ accountability for resource allocation, leading to a decrease in infant mortality rates. Conversely, in regions where the transfer of financial resources did not take place, the observed effects were of a lower magnitude.
In contrast, other studies argued that the autonomy granted to subnational governments in using financial resources did not necessarily reflect efficient utilization [28,35]. Three studies posited that, given the diverse conditions among local governments, including varying population groups, socioeconomic conditions, and geographic locations, the general trend was a decrease in efficiency [40,46]. According to Machado and Guim [35], less developed local governments in Brazil incurred higher per capita expenses on personnel and the acquisition of medicines, leading to inefficiencies inherent in scale loss. Regional variations in per capita expenditures among local governments rendered the system more vulnerable. Others mentioned that resource allocation led to an increase in health spending. Local governments, aiming to improve existing services or implement diversified policies, might not allocate financial resources in the most efficient way [65,73,75].
Focusing the analysis on the EFIC.STRE2 hypothesis, studies corresponding to this decentralization variable substantiated its validity. Considering the intricate nature of the decentralization process, certain conditions were highlighted: (i) the involvement of all stakeholders with an awareness of the necessity for changes; (ii) the presence of strategies tailored to address existing issues; and (iii) the coordination of the entire process, clear and precise, aimed at developing an integrated healthcare supply network specific to achieving efficiency in health services. These conditions, which affect the structural components of the system, influencing the behavior of organizations and individuals, are an example of an innovative case from the Marche region in Italy [54]. One factor that can influence the attainment of efficiency is the existence of excessive impositions by the central government, restricting the role of subnational governments in resource utilization and allocation based on their specificities [44].
The EFIC.EVAL2 hypothesis was not corroborated by the literature, as no study measured the impact of the existence of efficiency evaluation mechanisms. Three studies highlighted that the existence of these mechanisms assisted local governments in understanding the effects of implemented reforms and could guide considerations for future interventions [70,82]. However, despite some countries having monitoring systems for the execution of decentralized tasks, it remains unclear whether their existence contributes to improving efficiency.
4.3. Effectiveness
Concerning effectiveness, literature related to the EFET.GEO3 hypothesis suggested that the decentralization process impacts less developed local governments, presenting a primary challenge in fulfilling proposed objectives [36]. The level of development was deemed a fundamental condition for achieving better results. Unlike more developed subnational governments, those with less development exhibited fewer technical, administrative, and managerial capabilities, along with inadequate financial capacity to address the challenges of managing health services. Consequently, they found themselves in a situation of greater vulnerability, requiring the implementation of measures to enhance health services, as studies [32,36] concluded with respect to Brazil and Colombia. Thus, the hypothesis under examination was confirmed.
In the decentralization variable of the organization of political processes (EFET.OPP3), refs. [60,81] underscored that local governments, conscious of their electoral accountability, promoted the enactment of policies aligned with the preferences and needs of their citizens, confirming the hypothesis. In the case of the Spanish system, the existence of autonomous communities and the consequent decentralization of the health system entitled citizens with more flexibility in choosing local government representatives. In this sense, a need emerged among political decision makers to guarantee a structure that reconciled the objectives of management and health policy with the preferences of individuals [60]. The definition of policies by subnational governments, particularly when leveraging their own resources significantly, enhanced accountability in resource utilization toward citizens [63]. Consequently, with this autonomy and accountability for their actions, governments allocated resources with the goal of developing effective policies [47,71].
Several studies suggested that when existing financing mechanisms proved insufficient to cover expenses, and local governments resorted to their own resources, only the most developed governments had the capacity to implement appropriate policies [48,49]. Other articles indicated that in regions where a substantial portion of expenses was financed through their own revenues, politicians were more accountable, delivering services that better aligned with existing needs. Conversely, less developed regions heavily dependent on central government funds faced limitations, resulting in more constrained governance [22]. The Italian case highlighted these two impacts resulting from the decentralization of financial resources to the regions. While the objective was to foster regional development, the impacts varied among regions due to the pre-existing capabilities of this reform [56]. Thus, the EFET.FE3 hypothesis was validated.
Studies analyzed within the scope of the EFET.STRE3 hypothesis substantiated it, concluding that the existence of central coordination in defining guidelines for planning, resource utilization, and evaluation of implemented measures, combined with favorable local conditions for decentralization, contributed to improved policy performance [20,39]. In Italy [20] and Spain [62], given the pandemic context, differences emerged between the regions of the two countries in their capacity to respond to this phenomenon, which may be related to regional variations in the organization and provision of services and/or to different policies. However, in both contexts, planning and coordination linked to the decentralized model were fundamental in responding effectively to this phenomenon. Guidelines between the central government and the regions were crucial in addressing emerging needs. However, when subnational governments primarily implemented policies dictated by the central government, guidelines were defined and were useful for local-level actions but limited their capacity to implement policies [38].
Lastly, the EFET.EVAL3 hypothesis could not be thoroughly evaluated due to the existence of a single article [34]. However, it suggested that through the evaluation of implemented policies, it is possible to understand which measures were most successful, identify parameters for improvement and innovative practices, and recognize that municipalities have assumed a leadership role in the development and implementation of health policies.
Overall, the studies revealed several crucial insights. Firstly, asymmetries between municipalities were apparent based on the variable of geography and sociodemographics, with smaller municipalities, lower population density, and lower development levels being more susceptible to inefficiency, ineffectiveness, and inequities. Secondly, the presence of autonomy and accountability in local governments, coupled with effective regulation by the central administration and citizen involvement, enhanced their understanding of local needs and improvement potential. This collective understanding contributed significantly to advancements in equity, efficiency, and effectiveness in the organization of political processes. Thirdly, the allocation of financial resources to cover costs associated with transferred skills produced ambiguous impacts on equity and efficiency. The existing literature failed to distinctly demonstrate whether the inadequate redistribution of these resources contributed to an increase in health inequities or, conversely, if their allocation enhanced greater efficiency in utilization. Lastly, the successful implementation of more effective policies was contingent upon the socioeconomic capabilities of local governments. These findings underscore the complex dynamics inherent in decentralization processes, emphasizing the necessity for nuanced considerations in local-level policy formulation and implementation.
5. Conclusions
The process of decentralization in the health sector has generated concerns at various levels, including central governments, local administrations, and even among citizens. Numerous questions have emerged regarding the potential impacts stemming from the adoption and execution of such processes. Research findings indicate that the effects of decentralizing health policies to municipalities do not uniformly yield multiple benefits to health systems. Rather, the outcomes vary significantly based on socioeconomic contexts, access to financing, and the specifics of the implementation process.
While decentralization holds promise for enhancing health outcomes by fostering proximity to citizens, it introduces additional expenses that can compromise overall efficiency. Moreover, it tends to create disparities among municipalities, disproportionately affecting those with fewer resources and placing them in vulnerable situations. On a positive note, the close proximity between governance structures and individuals facilitates the exchange of information and enhances the adaptability of implemented measures to local realities. In turn, decentralization can contribute to achieving equity, particularly if smaller municipalities receive resources in proportion to their larger counterparts.
The potential for efficiency gains is a key aspect of decentralization, as it can mitigate information asymmetries and enable tailored responses to existing needs. However, the management of financial resources by local governments lacks conclusive evidence supporting guaranteed efficiency gains. Nevertheless, it is imperative to clearly define their responsibilities in terms of health service expenditures, ensuring that allocated resources are effectively used to improve healthcare services. In terms of effectiveness, decentralization can contribute to the formulation of more impactful policies, provided local governments are granted autonomy and held accountable for their actions.
The institutional capacity of local governments, coupled with clear guidelines on resource allocation processes, emerges as a pivotal factor for achieving equity, efficiency in health services, and the effectiveness of policies. These findings offer valuable insights for policymakers regarding the implementation of decentralization processes to maximize potential benefits and mitigate possible consequences once these initiatives are in place.
Moreover, these findings highlight the close relationship between the variables and the three decentralization theories. Regarding the “voting with your feet” theory, the possibility of citizens moving based on potential tax benefits or services requires that the decentralization process guarantees an efficient allocation of resources. Concerning the “close to ground” theory, intrinsically related to the variable organization of political processes, it is emphasized that the involvement of citizens and the existence of autonomy and political accountability for the actions of policymakers contribute to achieving the effectiveness of policies. Finally, concerning the theory “watching the watchers”, mutual accountability and support among all those involved in the process are key to the success of decentralization. This relationship shows that the impacts of the decentralization variables are strongly influenced by the existing geographic, socioeconomic, and institutional contexts.
Nevertheless, it is crucial to acknowledge certain limitations in the existing literature on this topic. The focus on a limited number of countries and the absence of comparative studies between nations pose challenges in drawing universal conclusions. Additionally, the narrow selection of outcome indicators, such as mortality rather than quality of life, limits the comprehensive understanding of the impact of decentralization. Despite theoretical references emphasizing the relevance of evaluation and monitoring capacity in this context, the connection between decentralization variables and their outcomes remains underexplored in the current body of literature. Addressing these gaps will be instrumental to advancing our understanding of the complex dynamics surrounding decentralization in the health sector.
Decentralization in the health sector dictates substantial changes that hinge upon a cohesive institutional and organizational structure, accompanied by adequate human, physical, and material resources to ensure successful execution. Additionally, not only is political will paramount in fostering improved health conditions for individuals, but local governments are also in a privileged position to integrate a network of partners and agents that enhance the development and sustainability of health systems [84]. The results underscore that the success of health decentralization relies on ensuring specific parameters. These parameters aim to secure an equitable regional/local distribution of health services and resources, facilitate the wise use of resources, and foster the implementation of effective policies.
While this scoping review adhered to rigorous methodological procedures in study selection and data extraction, it bears certain limitations that warrant consideration in future research. Firstly, the review focused on only five decentralization variables, overlooking others such as technical capacity at the local level to design policies, the institutional framework, the country’s governance model, and public awareness regarding local government accountability in health matters. These additional variables may influence the impacts of decentralization on healthcare. Secondly, the quality of the selected articles was not assessed due to the heterogeneous nature of the studies. Thirdly, the exclusion of gray literature in this scoping review is noteworthy, considering the likelihood of numerous reports and studies being unpublished in scientific articles. However, the decision to include only published studies was deliberate, guided by the criterion of ensuring quality through peer review.
For future research endeavors, given the vast unexplored landscape in this domain, it is recommended, based on insights into the impacts of decentralization on healthcare, to contemplate the capabilities, tasks, and competencies required in governance. These considerations are essential for ensuring that decentralization contributes to achieving greater equity, efficiency, and effectiveness. In light of the dearth of studies accurately measuring the evaluation variable and the outcomes of decentralization, there is a critical need to develop studies in this area. Finally, exploring whether the decentralization of skills has taken on new dimensions amid the challenges posed by the COVID-19 pandemic and understanding the emergent changes would be an intriguing avenue for further investigation.
Author Contributions
Conceptualization, R.O., T.S.M. and G.S.; methodology, R.O. and G.S.; writing—original draft preparation, R.O.; results, R.O. and G.S.; writing—review and editing, R.O., T.S.M. and G.S.; Supervision, T.S.M. and G.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Fundação para a Ciência e Tecnologia, grant number 2022.13288.BD, and partially funded by Programa Operacional Centro 2020 through Fundo Social Europeu.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
This review used existing research data.
Acknowledgments
Gonçalo Santinha would like to acknowledge the contribution of the research unit on Governance, Competitiveness, and Public Policies (UIDB/04058/2020) + (UIDP/04058/2020), funded by national funds through FCT—Portuguese Foundation for Science and Technology. The authors would like to acknowledge the contribution of Julian Perelman (NOVA National School of Public Health) for his helpful contribution to the development of the study.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A

Table A1.
Overview of studies on the instruments of data collection by type of methodology.
Table A1.
Overview of studies on the instruments of data collection by type of methodology.
| Number | Macro/Micro Analysis | Interviews | Document Analysis | Instruments of Data Collection | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size | Years | Dependent Variable | Independent Variable | Data Source | Sample Size | Typology | Years | |||
| 20 | Documents with responses to COVID-19 | Document analysis | ||||||||
| 21 | 318 municipalities (Chile); 1058 municipalities (Colombia) | Chile: 1991–96; Colombia: 1994–97 | Per capita expenditures at the municipal level; Use of health services | Key informants | Semi-structured interviews | Government documents | Longitudinal macro analysis + interviews + document analysis | |||
| 22 | Chile: 2001–13; Colombia: 2005–13 | Equity | Average per capita income; average per capita municipal income (Chile); supply-side resources; demand-side resources; total health resources (Colombia) | Colombia: National Planning Agency; Chile: Ministry of Interior (SEDERE) | Longitudinal macro analysis + interviews | |||||
| 23 | 1990–2010 | Equity | Maternal mortality rate; child mortality rate; public spending on health per capita; amongst others | National and subnational databases of the National Health Service of China | Government officials | Longitudinal macro analysis + interviews | ||||
| 24 | 21,120 interviews | May–June 2001 | Intra-regional inequalities in health | Self-declared health status; age; sex; income; inequalities in the health service; amongst others | Spanish National Health Survey; Spanish Household Budget Continuous Survey | Longitudinal micro analysis | ||||
| 25 | Italian and Spanish regions | 1998–2009 | Health spending per capita and the quality of services | Health; GDP per capita; proportion of people over 65 years of age; political alignment between regional and central government | Ministry of Health and the National Institute of Statistics | Longitudinal macro analysis | ||||
| 26 | 101 regions | 2004–2005 | Healthcare efficiency | Number of paid nurses; number of beds; number of total patients and case mix index; amongst others | Italian Ministry of Health; Health for All database | Longitudinal macro analysis | ||||
| 27 | 95% of Colombian municipalities | 1994–2004 | Variation in the poor population covered by public health insurance | Decentralization variables; resources; socioeconomic and geographic variables; amongst others | Agustín Codazzi Geography Institute; National Administrative Department of Statistics; National Electoral Office; amongst others | Longitudinal macro analysis | ||||
| 28 | 20 Italian regions | 1980–1995 | Real per capita spending on public health | GDP per capita; aging population; number of beds per hospital; number of medical and non-medical staff per hospital | Longitudinal macro analysis | |||||
| 29 | 19 Italian regions; 2 autonomous provinces | 2001–2017 | Fiscal decentralization of health spending | Density of general practitioners per 10,000 people; density of hospital beds per 10,000 people; amongst others | Health for All | Longitudinal macro analysis | ||||
| 30 | 50 Spanish regions | 1980–2010 | Infant mortality rate; neonatal mortality | Female employment rate; percentage of adult population with tertiary education; amongst others | Longitudinal macro analysis | |||||
| 31 | 20 regions | 2007 | Regional efficiency | Hospitalization rate for long-term complication diabetes; hospitalization rate for congestive heart failure; flu vaccination rate | Italian National Observatory on Health Status; Italian National Institute of Statistics | Cross-sectional macro analysis | ||||
| 32 | 1080 municipalities | 1998–2007 | Infant mortality rate | Locally controlled health expenditure as a proportion of total health expenditure; amongst others | National census and statistics; National Planning Department; National Administrative Department of Statistics | Longitudinal macro analysis | ||||
| 33 | 66 microregions | 2006 | Efficiency in the use of resources | DATASUS official website | Cross-sectional macro analysis | |||||
| 34 | Municipal health plan for 2014–2017; annual management reports for 2013–2016; epidemiologic bulletins | Document analysis | ||||||||
| 35 | 6626 Brazilian municipalities | 2010 | Health income and expenses | Propensity of managers to adhere to strategies for primary healthcare; ability of local managers to adhere to federal strategies for structuring primary healthcare; amongst others | Information System on Public Health Budgets; National Health Fund; Brazilian Institute of Geography and Statistics; amongst others | Cross-sectional macro analysis | ||||
| 36 | 55 key informants from health regions | Semi-structured | Interviews | |||||||
| 37 | 1 database with 424 municipalities until the end of 1998; 1 database with 523 municipalities until the end of 2000 | 1998–2000 | Performance and results of municipal health management | % of admissions to hospitals under municipal management in the total number of admissions carried out; number of admissions to hospitals under municipal management per inhabitants; amongst others | Public Health Budget Information System; Brazilian Institute of Geography and Statistics Foundation | Longitudinal macro analysis | ||||
| 38 | 5 municipalities | 1980–1999 (mortality) and 1995–2001 (morbidity) | Effectiveness | Preventable infant mortality rate; proportion of preventable child deaths; infant mortality from diarrhea; infant mortality due to acute respiratory infection; amongst others | Hospital Information System of the Unified Health System; Mortality Information System of the Unified Health System | 101 individuals | Semi-structured | Health plans 1998–2001; management reports 1999 and 2000 and federal transfers to municipalities between 1997 and 2001 | Longitudinal macro analysis + interviews + document analysis | |
| 39 | 3 key informants | Not structured | Decrees; resolutions; documents prepared by regional teams | Interviews + document analysis | ||||||
| 40 | 5526 municipalities | 2010 | Per capita expenditure on healthcare from municipal governments | Health services; the size of the installed healthcare network; population size; socioeconomic conditions of the municipalities | Information System on Public Health Budgets; Medical and Sanitary Car and Census; Brazilian Institute of Geography and Statistics; Atlas of Human Development in Brazil | Cross-sectional macro analysis | ||||
| 41 | 26 Brazilian states and the federal district | 2000–2013 | Infant mortality | Fiscal decentralization of health | Brazilian Ministry of Health; Brazilian Institute of Geography and Statistics | Longitudinal macro analysis | ||||
| 42 | 14 municipalities | 2003–2005 | Health system financing | Total expenditure with the municipality; expenditure with own resources; SUS transfers; primary care spending | SIOPS—data collection and processing system on total revenues and expenditures on public health actions and services across the three spheres of government | 14 municipal secretaries and representatives of the Municipal Health Fund and 42 municipal councilors | Semi-structured, individual and group with selected people | Municipal Health Plan, Multi-Year Plan; Budget Guidelines Law; Annual Budget Law; amongst others | Longitudinal macro analysis + interviews + document analysis | |
| 43 | 8 actors who occupy relevant roles in health management | Interviews | ||||||||
| 44 | 853 municipalities | 2006–2014 | Federal costs for medium and high complexity hospital and outpatient care | Resident population; total area (Km2); covered municipalities; health regions covered by socioeconomic and health conditions category; amongst others | National Health Fund | Longitudinal macro analysis | ||||
| 45 | 6 health specialists | In depth | February and March 2017 | Constitution of 1988; health policies; debates and decisions of the National Congress; amongst others | Interviews + document analysis | |||||
| 46 | 20 regions | 2007 | Regional efficiency | Hospitalization rate for long-term complication diabetes; hospitalization rate for congestive heart failure; flu vaccination rate; amongst others | Italian National Observatory on Health Status; Italian National Institute of Statistics | Longitudinal macro analysis | ||||
| 47 | 3 elements responsible for the PROREDE project | Semi-structured | 2008 | Interviews | ||||||
| 48 | Brazilian municipalities | 1998–2006 | Total health spending | Outpatient production of basic care; number of visits carried out by family health teams; community health agents; number of families supported by the programs | Finbra (Brazilian Finance); National Treasury Secretariat; Ministries of Health | Institutional reforms implemented | Longitudinal macro analysis + document analysis | |||
| 49 | Brazilian municipalities | 2000–2006 | Total health spending | Own resources; PAB transfers and total transfers from the Unified Health Service | Information System on Public Health Budgets | Longitudinal macro analysis | ||||
| 50 | 19 Italian regions and 2 autonomous provinces of Trento and Bolzano | 2015 | Performance of regional health systems | Accessibility; cost-expenditure; quality; effectiveness; safety; responsiveness/patient-centeredness | Health for All; National Health Observatory; Data provided by the “Passi”; SDO Report by the Italian Health Ministry | Cross-sectional macro analysis | ||||
| 51 | Documents with responses to COVID-19 | Document analysis | ||||||||
| 52 | 45,175 individuals | 2006 | Unmet health needs | Predisposing variables (age, sex, education); enabling variables (personal, family); need variables (self-assessment of general health status; presence of limitations in daily activities due to health problems) | European Union Statistics on Income and Living Conditions | Cross-sectional micro analysis | ||||
| 53 | 120,00 individuals | 2013 | Waiting time to access healthcare | Demographic (sex; age); socioeconomic (education; professional qualification); health conditions (self-perceived health status); type of structure (public or private); areas/regions (location) | Italian Health Interview Survey 2013 | Cross-sectional micro analysis | ||||
| 54 | People who occupy key positions in all the main organizations operating in the system | Semi-structured | Laws; files; historical data; organizational plans provided by organizations operating in the healthcare system | Interviews + document analysis | ||||||
| 55 | 20 regions | 1996–2012 | Infant mortality rate | Evolution of the degree of fiscal decentralization; evolution of vertical fiscal imbalance; GDP per capita; regional health expenditures as a share of total regional expenditures; amongst others | Health For All | Longitudinal macro analysis | ||||
| 56 | 20,000 Italian households (60,000 individuals) | 1994–2007 | Self-assessed health | Per capita spending on public health; GDP of the regions | Survey on the Daily Life of Italian Households—Italian Institute of Statistics | Longitudinal micro analysis | ||||
| 57 | 15 Italian regions | 1999–2006 | Per capita regional income | GDP; expense: revenue (regional government taxes; central government taxes; fees); fiscal balance | Longitudinal macro analysis of 21 Italian regions | |||||
| 58 | 21 Italian regions | 1991–2005 | Efficiency | Inputs (current public expenditure) and outputs (infant mortality rate; neonatal mortality rate in 1 day); policy variables (1995 electoral reform); control/environmental variables (intergovernmental subsidies for the health sector); amongst others | Longitudinal macro analysis | |||||
| 59 | 8400 individuals | 1997 | Self-perceived health inequality | Health spending | Spanish National Health Survey | Cross-sectional micro analysis | ||||
| 60 | 114–153 hospitals | 1996–2006 | Hospital capacity and production | Non-intensive care discharges; outpatient consultations; discharges from intensive care; donation of beds; graduated professionals; assistance technicians; amongst others | Spanish National Health System; Ministry of Health | Longitudinal macro analysis | ||||
| 61 | 119 regions | 1998–2005 | Per capita healthcare expenditure | Gross domestic product per capita; number of beds; population by region; region with political responsibilities; region with fiscal responsibilities | Website of the Ministry of Health and Social Policy and the Spanish Ministry of Education; Spanish Institute of National Statistics | Longitudinal macro analysis | ||||
| 62 | Documents with responses to COVID-19 | Document analysis | ||||||||
| 63 | 20 key officials | Semi-structured | Official documents | Interviews + document analysis | ||||||
| 64 | 10,409 individuals | January and March 2010 | Citizens’ perception of decentralization | Perception of efficiency gains through decentralization; way of assigning responsibility to regions; education level; age; job; political concern | Barometer CIS nº2.829 | Longitudinal micro analysis | ||||
| 65 | 17 Spanish regions | 1992–2005 | Per capita health spending | Logarithm of healthcare expenditure per capita; logarithm of real per capita income; acute care beds per 1000 people; amongst others | Spanish National Health Service | Longitudinal macro analysis | ||||
| 66 | 50 individuals from the Basque country and 146 from the Canary Islands | Simple random sampling in 2012 and 2016 (Islands) | Interviews | |||||||
| 67 | 23 Chinese provinces | 2002–2012 | Income inequalities; fiscal decentralization; public health | Ratio of per capita disposable income of urban residents to per capita disposable income of rural residents; ratio of provincial consolidated expenditure per capita to national consolidated expenditure per capita; amongst others | Chinese Fiscal Statistical Yearbooks | Longitudinal macro analysis | ||||
| 68 | 22 regions + 4 of China’s five provincial autonomous regions | 2006–2017 | Efficiency | Decentralization of health expenditure; revenue decentralization; GDP | Finance Yearbooks of China; China Statistical Yearbooks for Regional Economy; Provincial governments’ yearly budgetary reports; China Population and Employment Statistics Yearbooks | Longitudinal macro analysis | ||||
| 69 | 30 regions and 4 municipalities | 2008–2019 | Population mortality and public health expenditure | Decentralization of tax revenue; decentralization of fiscal expenditure; real GDP per capita; economic development; scientific and technological advancement; amongst others | China Statistical Year book—Finance Year book of China and the China Statistical Year book on Environment | Longitudinal macro analysis | ||||
| 70 | 51 hospitals | 2000 and 2003 | Efficiency | Inputs: annual numbers of full-time medical staff; all other staff; staffed hospital beds. Outputs: case-mix-adjusted inpatient cases; outpatient visits; surgical operations performed | Longitudinal micro analysis | |||||
| 71 | Legislative acts and official reports regarding regional health policy | Document analysis | ||||||||
| 72 | 37 directors of health regions | Semi-structured interviews | 2009 and 2012 | Interviews | ||||||
| 73 | 20 OECD countries | 1990–2000 | Per-capita total health expenditure | Per-capita GDP; density of physicians per 1000 inhabitants; density of acute beds per 1000 inhabitants; percentage of population below 19 years of age; amongst others | OECD Health Data | Longitudinal macro analysis of 20 OECD countries | ||||
| 74 | 20 OECD countries | 1970–2001 | Infant mortality | Infant mortality; total healthcare expenditure; GDP per capita; healthcare expenditure/GDP; alcohol consumption, liters per capita; amongst others | International Monetary Fund Government Finance Statistics; OECD Stat Extracts; Economic Performance-OCDE Political Institutions | Longitudinal macro analysis | ||||
| 75 | 110 regions in 8 OECD countries | 1997 | Health spending and per capita income | GDP per capita; population aged 65 or over; total health spending | Macro analysis cross-section | Cross-sectional macro analysis | ||||
| 76 | 32,365 people 18 years of age or older | 2013 | Use of healthcare services | Predisposing factors (sex; age in ranges, married or united); enabling factors (type of health coverage; currently employed); need factors (self-perceived health status; problems with mobilization; level of physical activity) | Third National Survey of Risk Factors 2013 | Cross-sectional micro analysis | ||||
| 77 | 17 autonomous regions—Spain; 26 states and 5579 municipalities—Brazil | 1980–2015 | Decentralization | Total spending on health (% of GDP); public spending on health (% of GDP) | Economic Commission for Latin America and the Caribbean; World Health Organization | Laws; normative acts; official documents | Longitudinal macro analysis + document analysis | |||
| 78 | 20 interviews with key health system officials and political leaders | In-depth interviews | Documents related to changes in financing policies and community participation after decentralization | Interviews + document analysis | ||||||
| 79 | 28 EU countries | 2014 | Local public spending | Fiscal decentralization | Eurostat data | Cross-sectional macro analysis | ||||
| 80 | 2006 | Patient Choice Index | Economic result (excluding government grants); running net profit; net purchase of healthcare; governing majorities; population; amongst others | Cross-sectional macro analysis | ||||||
| 81 | In-depth individual interviews (local officials from each community); focus group interviews | In depth | Interviews + document analysis of 81 regions | |||||||
| 82 | 81 regions | 2014 and 2017 | Efficiency | INPUTS: number of beds per 10,000 people; intensive care beds per 10,000 people; OUTPUTS: number of examinations; total birth parturition; amongst others | Public Hospitals Statistics Yearbook | Longitudinal macro analysis | ||||
References
- Saltman, R.B.; Bankauskaite, V.; Vrangbæk, K. Decentralization in Health Care: Strategies and outcomes. In European Observatory on Health Systems and Policies Series; McGraw-Hill: Maidenhead, UK; New York, NY, USA, 2007. [Google Scholar]
- Sumah, A.M.; Baatiema, L.; Abimbola, S. The impacts of decentralisation on health-related equity: A systematic review of the evidence. Health Policy 2016, 120, 1183–1192. [Google Scholar] [CrossRef] [PubMed]
- OECD. Decentralisation and Regionalisation in Portugal: What Reform Scenarios? In OECD Multi-Level Governance Studies; OECD Publishing: Paris, France, 2020. [Google Scholar] [CrossRef]
- Teles, F. Descentralização e Poder Local em Portugal; Fundação Francisco Manuel dos Santos: Lisboa, Portugal, 2021; ISBN 978-989-9004-85-6. [Google Scholar]
- Abimbola, S.; Baatiema, L.; Bigdeli, M. The impacts of decentralization on health system equity, efficiency and resilience: A realist synthesis of the evidence. Health Policy Plan. 2019, 34, 605–617. [Google Scholar] [CrossRef] [PubMed]
- Santinha, G.; Fernandes, A.; Oliveira, R.; Rocha, N. Designing a Health Strategy at Local Level: A Conceptual Framework for Local Governments. Int. J. Environ. Res. Public Health 2023, 20, 6250. [Google Scholar] [CrossRef] [PubMed]
- Tiebout, C. A pure theory of local expenditures. J. Political Econ. 1956, 64, 416–424. [Google Scholar] [CrossRef]
- Arrow, K.J. Uncertainty and the welfare economics of medical care. Am. Econ. Rev. 1963, 53, 941–973. [Google Scholar]
- Hurwicz, L. But who will guard the guardians? Am. Econ. Rev. 2008, 98, 577–585. [Google Scholar] [CrossRef]
- Dougherty, S.; Lorenzoni, L.; Marino, A.; Murtin, F. The impact of decentralisation on the performance of health care systems: A non-linear relationship. Eur. J. Health Econ. 2022, 23, 705–715. [Google Scholar] [CrossRef]
- Cadham, C.; Prosser, L. Eliciting Trade-Offs Between Equity and Efficiency: A Methodological Scoping Review. Jou Int. Soc. Phar. Out Res. 2023, 26, 943–952. [Google Scholar] [CrossRef]
- Gocke, D.; Johnston-Webber, C.; McGuire, A.; Wharton, G. Building Sustainable and Resilient Health Systems: Key Findings. The Partnership for Health System Sustainability and Resilience. LSE Consulting. 2023. Available online: https://www3.weforum.org/docs/WEF_PHSSR_Building_Sustainable_and_Resilient_Health_Systems_2023.pdf (accessed on 21 December 2023).
- Whitehead, M. The concepts and principles of equity and health. Int. J. Health Serv. 1992, 22, 429–445. [Google Scholar] [CrossRef]
- Santana, P.; Freitas, Â.; Stefanik, I.; Costa, C.; Oliveira, M.; Rodrigues, T.; Vieira, A.; Ferreira, P.; Borrell, C.; Dimitroulopoulou, S.; et al. Advancing tools to promote health equity across European Union regions: The EURO-HEALTHY project. Health Res. Policy Syst. 2020, 18, 18. [Google Scholar] [CrossRef]
- Palmer, S.; Torgerson, D.J. Economic notes: Definitions of efficiency. BMJ 1999, 318, 1136. [Google Scholar] [CrossRef] [PubMed]
- Patel, P. Efficacy, Effectiveness, and Efficiency. Natl. J. Community Med. 2021, 12, 33–39. [Google Scholar]
- Peters, M.; Marnie, C.; Colquhoun, H.; Garritty, C.; Hempel, S.; Horsley, T.; Langlois, E.; Lillie, E.; O’Brien, K.; Tunçalp, O.; et al. Scoping reviews: Reinforcing and advancing the methodology and application’. Syst. Rev. 2021, 10, 263. [Google Scholar] [CrossRef] [PubMed]
- Migchelbrink, K.; Van de Walle, S. A systematic review of the literature on determinants of public managers’ attitudes toward public participation. Local Gov. Stud. 2021, 48, 1–22. [Google Scholar] [CrossRef]
- Heise, T.; Seidler, A.; Girbig, M.; Freiberg, A.; Alayli-Goebbels, A.; Fischer, M.; Haß, W.; Zeeb, H. CAT HPPR: A critical appraisal tool to assess the quality of systematic, rapid, and scoping reviews investigating interventions in health promotion and prevention. BMC Med. Res. Methodol. 2022, 22, 334. [Google Scholar] [CrossRef]
- Bosa, I.; Castelli, A.; Castelli, M.; Ciani, O.; Compagni, A.; Galizzi, M.; Garofano, M.; Ghislandi, S.; Giannoni, M.; Marini, G.; et al. Corona-regionalism? Differences in regional responses to COVID-19 in Italy. Health Policy 2021, 125, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Bossert, T.; Larrañaga, O.; Giedion, U.; Arbelaez, J.; Bowser, D. Decentralization and equity of resource allocation: Evidence from Colombia and Chile. Bull. World Health Organ 2003, 81, 95–100. [Google Scholar]
- Bossert, T.; Lenz, R.; Guerrero, R.; Miranda, R.; Soto Rojas, V.; Vargas, N. Decentralization Can Improve Equity, but Can It Be Sustained? Health Syst. Reform 2022, 8, e2064793. [Google Scholar] [CrossRef]
- Brixi, H.; Um, Y.; Targa, B.; Hipgrave, D. Engaging sub-national governments in addressing health equities: Challenges and opportunities in China’s health system reform. Health Policy Plan. 2013, 28, 809–824. [Google Scholar] [CrossRef]
- Costa-Font, J.; Gil, J. Exploring the pathways of inequality in health, health care access and financing in decentralized Spain. J. Eur. Soc. Policy 2009, 19, 446–458. [Google Scholar] [CrossRef]
- Costa-Font, J.; Turati, G. Regional healthcare decentralization in unitary states: Equal spending, equal satisfaction? Reg. Stud. 2018, 52, 974–985. [Google Scholar] [CrossRef]
- De Nicola, A.; Gitto, S.; Mancuso, P.; Valdmanis, V. Healthcare reform in Italy: An analysis of efficiency based on nonparametric methods. Int. J. Health Plan. Manag. 2014, 29, e48–e63. [Google Scholar] [CrossRef] [PubMed]
- Faguet, J.; Sánchez, F. Decentralization and access to social services in Colombia. Public Choice 2014, 160, 227–249. [Google Scholar] [CrossRef]
- Giannoni, M.; Hitiris, T. The regional impact of health care expenditure: The case of Italy. Appl. Econ. 2002, 34, 1829–1836. [Google Scholar] [CrossRef]
- Rótulo, A.; Paraskevopoulou, C.; Kondilis, E. The Effects of Health Sector Fiscal Decentralisation on Availability, Accessibility, and Utilisation of Healthcare Services: A Panel Data Analysis. Int. J. Health Plan. Manag. 2022, 12, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Rubio, D.; García-Gómez, P. Decentralization of health care systems and health outcomes: Evidence from a natural experiment. Soc. Sci. Med. 2017, 188, 69–81. [Google Scholar] [CrossRef] [PubMed]
- Pelone, F.; Kringos, D.S.; Valerio, L.; Romaniello, A.; Lazzari, A.; Ricciardi, W.; Giulio de Belvis, A. The measurement of relative efficiency of general practice and the implications for policy makers. Health Policy 2012, 107, 258–268. [Google Scholar] [CrossRef]
- Soto, V.; Farfan, M.; Lorant, V. Fiscal decentralisation and infant mortality rate: The Colombian case. Soc. Sci. Med. 2012, 74, 1426–1434. [Google Scholar] [CrossRef]
- Fonseca, P.; Ferreira, M. Investigation of efficiency levels in the use of resources in the health sector: An analysis of the micro-regions of Minas Gerais. Saúde Soc. 2009, 18, 199–213. [Google Scholar] [CrossRef][Green Version]
- Massuda, A.; Titton, C.; Poli, P. Remembering Alma-Ata: Challenges and innovations in primary health care in a middle-income city in Latin America. Rev. Panam. Salud Pública 2018, 42, e157. [Google Scholar] [CrossRef]
- Machado, J.; Guim, L. Decentralization and equality in access to health services: The case of Brazil. Rev. Serviço Público 2017, 68, 37–64. [Google Scholar] [CrossRef][Green Version]
- Pinafo, E.; Nunes, E.; Carvalho, B.; Mendonça, F.; Domingos, C.; Silva, C. Management problems and strategies: The vulnerability of small-sized municipalities. Ciência Saúde Coletiva 2020, 25, 1619–1628. [Google Scholar] [CrossRef] [PubMed]
- Viana, A.; Heimann, L.; de Lima, L.; de Oliveira, R.; Rodrigues, S. Significant changes in the health system decentralization process in Brazil. Cad. Saúde Pública 2002, 18, S139–S151. [Google Scholar] [CrossRef]
- Vieira-da-Silva, L.; Hartz, Z.; Chave, S.; da Silva, G.; Paim, J. The implementation of decentralized health systems: A comparative study of five cases in Bahia, Brazil. Cad. Saude Publica 2007, 23, 355–370. [Google Scholar] [CrossRef]
- Spedo, S.; Tanaka, O.; Pinto, N. The challenge of decentralization of the Unified National Health System in large cities: The case of São Paulo, Brazil. Cad. Saude Publica 2009, 25, 1781–1790. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Araújo, C.; Gonçalves, G.; Machado, J. Os municípios brasileiros e os gastos próprios com saúde: Algumas associações. Cienc Saude Coletiva 2017, 22, 953–963. [Google Scholar] [CrossRef]
- Assis, D. Descentralização e resultados na saúde infantil no Brasil. Estud. Económicos 2020, 50, 447–484. [Google Scholar] [CrossRef]
- Leite, V.; Lima, K.; de Vasconcelos, C. Funding, public spending and management of health resources: The current situation in a Brazilian state. Cienc Saude Coletiva 2012, 17, 1849–1856. [Google Scholar] [CrossRef]
- Miranda, G.; Mendes, A.; Silva, A. The challenge of organizing a universal and efficient National Health System in the Brazilian federal pact. Saude Soc. 2017, 26, 329–335. [Google Scholar] [CrossRef]
- Moreira, L.; Ferré, F.; Andrade, E. Healthcare financing, decentralization and regional health planning: Federal transfers and the healthcare networks in Minas Gerais, Brazil. Cienc Saude Coletiva 2017, 22, 1245–1256. [Google Scholar] [CrossRef][Green Version]
- Segatto, C.; Béland, D. Federalism and decision making in health care: The influence of subnational governments in Brazil. Policy Stud. 2021, 42, 308–326. [Google Scholar] [CrossRef]
- Vasconcelos, M.; Silva, C. An Evaluation of the Unified Health System in Brazilian Capital: Suggestions for the Creation of Public Polices. J. Glob. Compet. Governability 2018, 12, 49–63. [Google Scholar] [CrossRef]
- Valdebenito, M.; Capucci, P.; Brandalise, D.; Moreira, R. Health Decentralization Resources (PROREDE): Consolidating citizenship and popular participation. Saude Soc. 2012, 21, 278–285. [Google Scholar] [CrossRef]
- Vazquez, D. Institutional Mechanisms of Federal Regulation and its Results on Education and Health Policies. Rev. Bras. Cienc. Sociais 2014, 57, 969. [Google Scholar] [CrossRef][Green Version]
- Vazquez, D. The effects of Brazilian Federal regulation on health financing. Cad. Saude Publica 2011, 27, 1201–1212. [Google Scholar] [CrossRef]
- Bruzzi, S.; Ivaldi, E.; Santagata, M. Measuring Regional Performance in the Italian NHS: Are Disparities Decreasing? Social Indic Res. 2022, 159, 1057–1084. [Google Scholar] [CrossRef] [PubMed]
- Capano, G.; Lippi, A. Decentralization, policy capacities, and varieties of first health response to the COVID-19 outbreak: Evidence from three regions in Italy. J. Eur. Public Policy 2021, 28, 1197–1218. [Google Scholar] [CrossRef]
- Cavalieri, M. Geographical variation of unmet medical needs in Italy: A multivariate logistic regression analysis. Int. J. Health Geogr. 2013, 12, 27. [Google Scholar] [CrossRef]
- Landi, S.; Ivaldi, E.; Testi, A. The role of regional health systems on the waiting time inequalities in health care services: Evidences from Italy. Health Serv. Manag. 2021, 34, 136–147. [Google Scholar] [CrossRef]
- Villa, S.; Alesani, D.; Borgonovi, E. Getting health reforms right: What lessons from an Italian case? Health Serv. Manag. 2008, 21, 131–140. [Google Scholar] [CrossRef]
- Cavalieri, M.; Ferrante, L. Does fiscal decentralization improve health outcomes? Evidence from infant mortality in Italy. Soc. Sci. Med. 2016, 164, 74–88. [Google Scholar] [CrossRef] [PubMed]
- Novi, C.; Piacenza, M.; Robone, S.; Turati, G. Does fiscal decentralization affect regional disparities in health? Quasi-experimental evidence from Italy. Reg. Sci. Urban Econ. 2019, 78, 103465. [Google Scholar] [CrossRef]
- Ferrario, C.; Zanardi, A. Fiscal decentralization in the Italian NHS: What happens to interregional redistribution? Health Policy 2011, 100, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Porcelli, F. Electoral accountability and local government efficiency: Quasi-experimental evidence from the Italian health care sector reforms. Econ. Gov. 2014, 15, 221–251. [Google Scholar] [CrossRef]
- Costa-Font, J. Inequalities in self-reported health within Spanish Regional Health Services: Devolution re-examined? Int. J. Health Plan. Manag. 2005, 20, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Álvarez, A.; Roibás-Alonso, D.; Wall, A. The response of decentralized health services to demand uncertainty and the role of political parties in the Spanish public health system. J. Prod. Anal. 2013, 40, 357–365. [Google Scholar] [CrossRef]
- Costa-Font, J. Does Devolution Lead to Regional Inequalities in Welfare Activity? Environ. Plan. C 2010, 28, 435–449. [Google Scholar] [CrossRef]
- Erkoreka, M.; Hernando-Pérez, J. Decentralization: A handicap in fighting the COVID-19 pandemic? The response of the regional governments in Spain. Public Admin. Develop. 2022, 43, 129–140. [Google Scholar] [CrossRef]
- Gallego, R.; Barbieri, N.; Brosa, C.; González, S.; Ferrer, M. Constraints on political autonomy in decentralized Spain? Analysing the impact of territorial financing and governments’ ideology on regional policy-making. Rev. Estud. Políticos 2018, 180, 131–162. [Google Scholar] [CrossRef]
- Sauco, F.; Laborda, J. Attribution of regional responsibilities for public services and citizen support of decentralisation: Evidence from Spain. Rev. Esp. Investig. Soc. 2015, 152, 65–86. [Google Scholar] [CrossRef]
- Prieto, D.; Lago-Peñas, S. Decomposing the determinants of health care expenditure: The case of Spain. Eur. J. Health Econ. 2012, 13, 19–27. [Google Scholar] [CrossRef] [PubMed]
- Sigüenza, W.; Artabe, A. Do individuals’ health preferences validate the decentralisation of the public health system in Spain? Health Policy 2022, 126, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Hao, Y.; Liu, J.; Lu, Z.; Shig, R.; Wu, H. Impact of income inequality and fiscal decentralization on public health: Evidence from China. Econ. Model 2021, 94, 934–944. [Google Scholar] [CrossRef]
- Sun, S.; Andrews, R. Intra-provincial fiscal decentralization, relative wealth, and healthcare efficiency: Empirical evidence from China. Public Admin. 2022, 101, 973–992. [Google Scholar] [CrossRef]
- Xu, W.; Lin, J. Fiscal Decentralization, Public Health Expenditure and Public Health-Evidence From China. Front Public Health 2022, 10, 773728. [Google Scholar] [CrossRef] [PubMed]
- Aletras, V.; Kontodimopoulos, N.; Zagouldoudis, A.; Niakas, D. The short-term effect on technical and scale efficiency of establishing regional health systems and general management in Greek NHS hospitals. Health Policy 2007, 83, 236–245. [Google Scholar] [CrossRef] [PubMed]
- Athanasiadis, A.; Kostopoulou, S.; Philalithis, A. Regional Decentralisation in the Greek Health Care System: Rhetoric and Reality. Glob. J. Health Sci. 2015, 7, 55–67. [Google Scholar] [CrossRef]
- Athanasiadis, A.; Ratsika, N.; Trompoukis, C.; Philalithis, A. The health decentralization process in Greece: The insiders’ perspective. Int. J. Health Gov. 2018, 23, 316–329. [Google Scholar] [CrossRef]
- Mosca, I. Decentralization as a determinant of health care expenditure: Empirical analysis for OECD countries. Appl Econ Lett 2007, 14, 511–515. [Google Scholar] [CrossRef]
- Jiménez-Rubio, D. The impact of fiscal decentralization on infant mortality rates: Evidence from OECD countries. Soc. Sci. Med. 2011, 73, 1401–1407. [Google Scholar] [CrossRef]
- López-Casasnovas, G.; Saez, M. A multilevel analysis on the determinants of regional health care expenditure: A note. European J. Health Econ. 2007, 8, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Palacios, A.; Espinola, N.; Rojas-Roque, C. Need and inequality in the use of health care services in a fragmented and decentralized health system: Evidence for Argentina. Int. J. Equity Health 2020, 19, 67. [Google Scholar] [CrossRef] [PubMed]
- Pereira, A.; Lima, L.; Machado, C. Decentralization and regionalization of health policy: A historical-comparative approach between Brazil and Spain. Cienc. Saude Coletiva 2018, 23, 2239–2252. [Google Scholar] [CrossRef] [PubMed]
- Arredondo, A.; Orozco, E. Effects of health decentralization, financing and governance in Mexico. Rev. Saude Publica 2006, 40, 152–160. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Halásková, R.; Haláskova, M. Local governments in EU countries: Competences and financing of public services. Sci. Pap. Univ. Pardubic. 2017, 25, 49–60. [Google Scholar]
- Fredriksson, M.; Winblad, U. Consequences of a decentralized healthcare governance model: Measuring regional authority support for patient choice in Sweden. Soc. Sci. Med. 2008, 67, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Sudhipongpracha, T. Measuring community empowerment as a process and an outcome: Preliminary evaluation of the decentralized primary health care programs in northeast Thailand. Community Dev. J. 2013, 44, 551–566. [Google Scholar] [CrossRef]
- Manavgat, G.; Demirci, A. Decentralization Matter of Healthcare and Effect on Regional Healthcare Efficiency: Evidence from Turkey. Sosyoekonomi 2020, 28, 261–281. [Google Scholar] [CrossRef]
- Jancovic, P.; Zagorsekova, N.; Baleha, A. Geography of the European Union Development Aid Allocation. Folia Geographica 2021, 63, 5–18. [Google Scholar]
- Guha, J.; Chakrabarti, B. Achieving the Sustainable Development Goals (SDGs) through decentralisation and the role of local governments: A systematic review. Commonw. J. Local Gov. 2019, 22, 6855. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).