Abstract
The integration of Green Lean Six Sigma (GLSS) within healthcare systems presents an opportunity to improve operational efficiency, environmental sustainability, and the quality of patient care. This study examines healthcare professionals’ initial perceptions of GLSS adoption in their work environments, especially in the context of Industry 4.0, the COVID-19 pandemic, and economic constraints. Through semi-structured interviews with healthcare workers and academics, the study reveals a cautious yet optimistic outlook. Participants recognize the potential for significant efficiency gains and waste reduction but also voice concerns about resource limitations and the need for comprehensive training. These preliminary findings provide important insights into the opportunities and challenges associated with implementing GLSS in healthcare, laying a foundation for future research and practical applications aimed at enhancing hospital operations through sustainable practices.
1. Introduction
Healthcare is pivotal to societal well-being and economic development, yet achieving the United Nations’ Sustainable Development Goal (SDG) of Good Health and Well-Being remains a considerable challenge, particularly in regions where inadequate care disproportionately impacts vulnerable populations. This challenge is further compounded by the demands of Industry 4.0, the ongoing repercussions of the COVID-19 pandemic, and economic constraints. These factors place significant pressure on hospitals to maintain high standards of care while simultaneously improving operational efficiency, reducing costs, and adhering to environmental regulations.
While sustainable Lean practices like Green Lean Six Sigma (GLSS) hold promise for enhancing hospital operations, there is a notable gap in empirical research concerning their implementation in healthcare settings. Although Lean Thinking and Six Sigma have demonstrated success in improving efficiency and quality across various industries, their combined application with green technologies (GLSS) in the healthcare sector remains underexplored [1,2,3]. This gap is particularly significant, as understanding healthcare professionals’ perceptions and preparedness for GLSS adoption can provide crucial insights for facilitating successful implementation [4,5,6].
This study seeks to address this research gap by investigating the initial perceptions and insights of healthcare providers and academics regarding GLSS. Through qualitative interviews with a diverse range of healthcare professionals, this research aims to answer the following key questions: How do healthcare professionals perceive and understand GLSS? What benefits and concerns do they anticipate regarding its implementation? How prepared are they to adopt these practices, and what challenges do they foresee?
In addressing these questions, this study evaluates the readiness of healthcare workers and academics to embrace GLSS, identifying potential gains in efficiency and sustainability, while also highlighting challenges such as resource limitations and the need for training. This research makes a significant contribution by filling an empirical gap in the existing literature and offering practical guidance to healthcare administrators and policymakers.
The following sections will discuss the application of Lean Thinking in healthcare, outline the benefits of GLSS, and explain the research methodology used in this study. The findings from the interviews will then be presented, analyzed, and used to offer recommendations for the successful implementation of GLSS. Finally, the article will conclude by summarizing the key findings and offering suggestions for future research, advancing both the practical and academic understanding of sustainable healthcare practices.
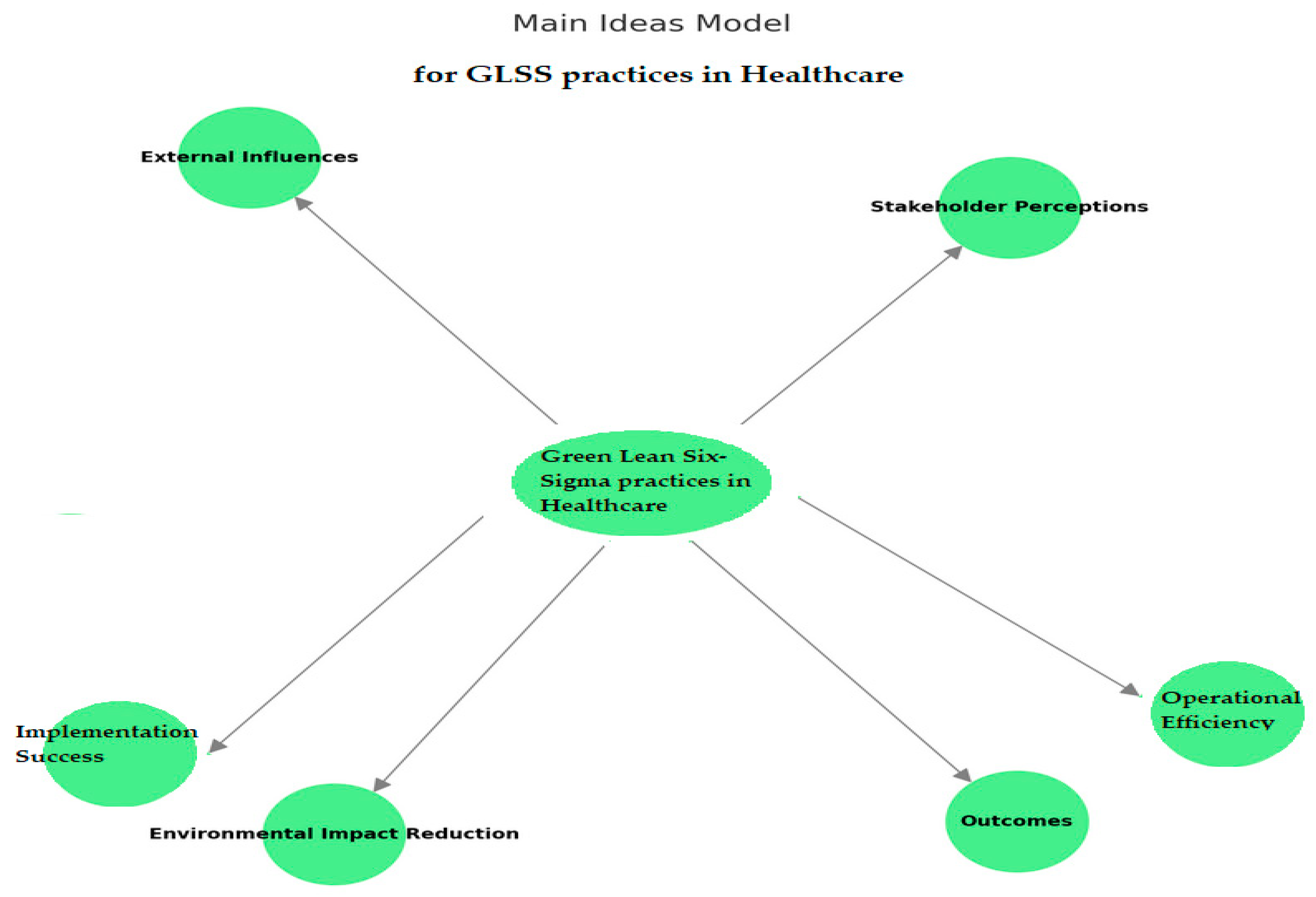
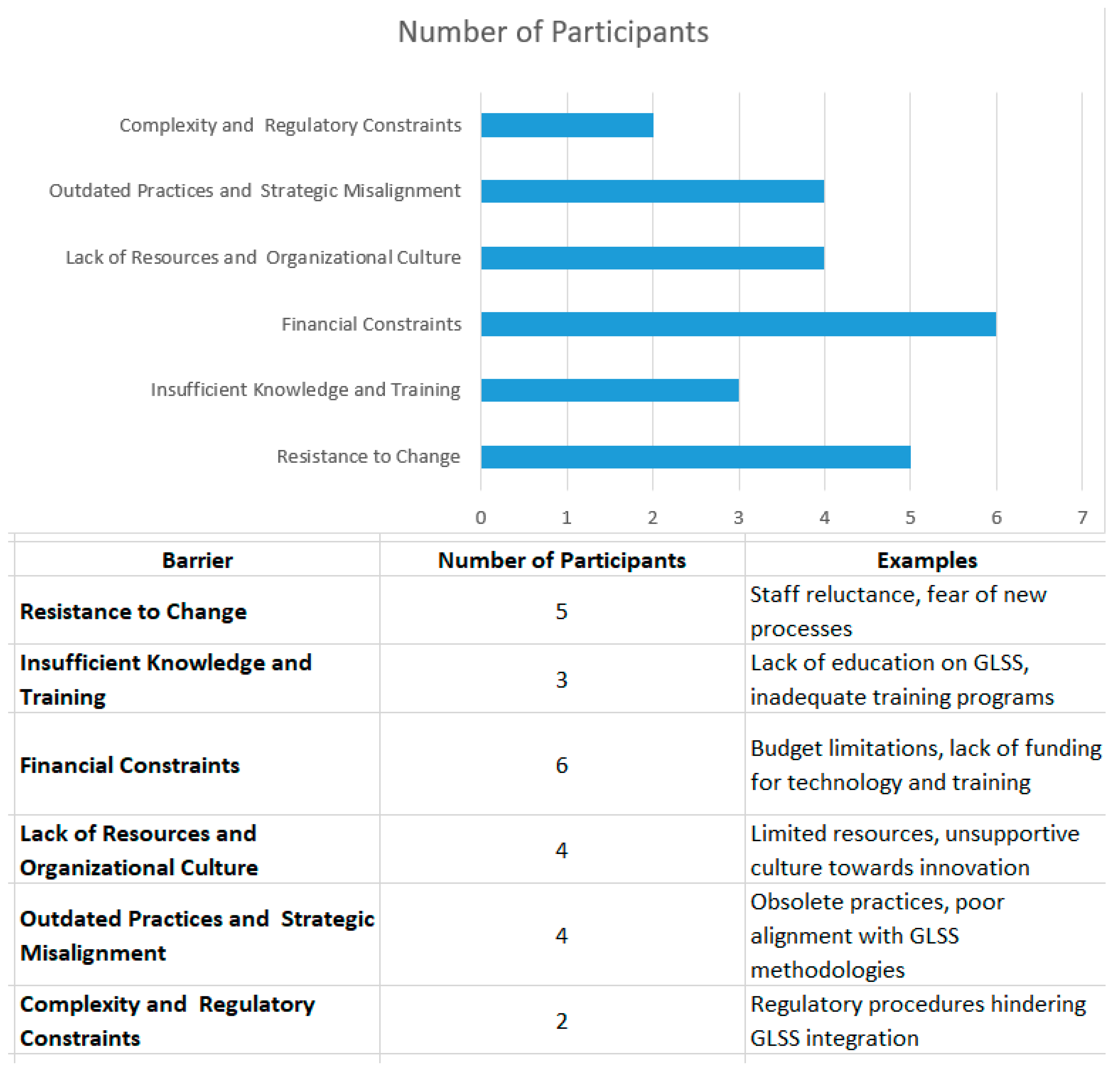
Main Ideas Model: GLSS Practices in Healthcare
The Main Ideas Model for GLSS Practices in Healthcare (Figure 1) centers around the integration of Lean methodologies to enhance the efficiency and sustainability of healthcare operations. The central idea is supported by key components, such as operational efficiency, environmental impact reduction, and implementation success. Operational efficiency focuses on process optimization and waste reduction, while environmental impact reduction emphasizes the use of green technology to minimize the healthcare sector’s environmental footprint.
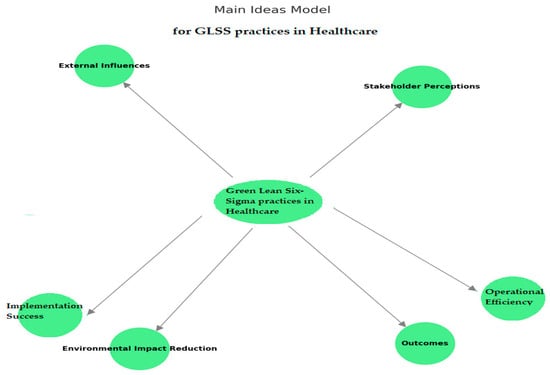
Figure 1.
Main Ideas Model. This figure was created by the authors of the article.
Successful implementation hinges on organizational readiness and leadership commitment, both of which are essential for overcoming challenges related to stakeholder perceptions, such as awareness, attitudes, and support needs. The model outlines expected outcomes, including improved efficiency, enhanced sustainability, and successful adoption of GLSS practices. External influences, such as Industry 4.0 technologies and the ongoing impact of COVID-19, play a significant role in shaping the implementation and effectiveness of these practices.
Explanation of the Diagram’s Elements:
Key components:
- Operational efficiency.
- ○
- Process optimization.
- ○
- Waste reduction.
- Environmental Impact Reduction.
- ○
- Green technology.
- ○
- Reduced environmental footprint.
- Implementation success.
- ○
- Organizational readiness.
- ○
- Leadership commitment.
- Stakeholder perceptions.
- ○
- Awareness and understanding.
- ○
- Attitudes and readiness.
- ○
- Challenges and support needs.
Outcomes:
- Improved efficiency.
- Enhanced sustainability.
- Successful GLSS adoption.
External influences:
- Industry 4.0 technologies.
- The impact of COVID-19.
The ideas in the model interact closely to achieve improved efficiency, sustainability, and successful GLSS adoption:
- Operational efficiency (process optimization and waste reduction) directly supports Environmental impact reduction by minimizing the environmental footprint through green technology.
- Implementation success relies on organizational readiness and leadership commitment, ensuring that both operational and environmental goals are met.
- Stakeholder perceptions (awareness, attitudes, and readiness) are crucial, as they influence the ease of GLSS adoption. Positive perceptions and adequate support help stakeholders overcome challenges.
- External influences like Industry 4.0 technologies and COVID-19 impact shape and sometimes accelerate these interactions, affecting the overall outcomes.
In summary, this model illustrates a holistic approach in which each component influences the others, creating a balanced system that drives the successful adoption of GLSS while achieving efficiency and sustainability goals. External influences further shape how these components interact and evolve.
2. Enhancing Hospital Performance through Green Lean Six-Sigma
Healthcare systems are among the most vital infrastructures in any society, playing a fundamental role not only in enhancing individual well-being but also in driving societal progress, contributing significantly to both economic and social development. The critical importance of healthcare cannot be overstated, as it is directly linked to the health, prosperity, and development of nations and communities. Access to quality healthcare is also globally recognized as a fundamental right, enshrined within the framework of the 17 Sustainable Development Goals (SDGs) set by the United Nations. Specifically, the third SDG focuses on “Good Health and Well-Being” and emphasizes the importance of ensuring that individuals across all demographics have access to equitable, affordable, and high-quality healthcare services [7,8,9,10].
While this goal highlights the significance of healthcare access, it also reflects the global challenges faced with regard to consistently delivering high-quality care. Despite the centrality of healthcare in fostering societal welfare, the quality of services delivered often falls short of expectations. Inadequate healthcare persists as a widespread issue, particularly in lower-income settings or among vulnerable populations who frequently bear the brunt of substandard services. The quality disparities in healthcare provision lead to significant health inequities, with disadvantaged groups disproportionately affected. Thus, addressing these gaps is critical for ensuring more equitable health outcomes and fostering sustainable development, as outlined in global development frameworks [11,12]. Addressing these challenges is essential for ensuring equitable health outcomes and promoting sustainable development [13,14].
In recent years, the rapidly evolving healthcare landscape has been further complicated by the emergence of Industry 4.0, the COVID-19 pandemic, and a continuously challenging economic climate. These factors have introduced new levels of complexity for healthcare organizations, especially hospitals, which now face the daunting task of maintaining high standards of patient care while simultaneously improving operational efficiency, reducing costs, and responding to the ever-increasing expectations of stakeholders [15,16].
Amid these challenges, there is growing pressure for hospitals to reduce waste, streamline their processes, and remain competitive, all while adhering to stringent environmental regulations. In this regard, it is increasingly evident that hospitals must not only focus on the quality of patient care but also their environmental footprint. The adoption of sustainable practices that prioritize eco-friendliness is thus essential. Hospitals must evolve to meet environmental regulations and public expectations for sustainability, integrating eco-friendly initiatives into their core operational strategies to ensure both their competitiveness and long-term viability [17,18].
Sustainable development has emerged as a key organizational strategy across various sectors and is driven by the need to address both present and future demands. It is increasingly recognized that sustainable practices not only enable organizations to meet ethical and regulatory requirements but also fuel innovation, driving growth and fostering a competitive edge [19,20]. For hospitals, the strategic incorporation of sustainability is particularly critical. Not only does it ensure compliance with environmental and health regulations, but it also positions hospitals as leaders in areas such as corporate social responsibility, environmental stewardship, and community engagement [21,22]. In this context, the integration of sustainable methodologies such as Green Lean Six Sigma (GLSS) has gained widespread recognition as an effective strategy for achieving both operational excellence and sustainability objectives [23,24].
Green Lean Six Sigma (GLSS) combines the principles of Lean Thinking and Six Sigma with sustainable practices, offering a comprehensive approach to improving hospital operations while reducing environmental impact. The GLSS framework enables healthcare settings to streamline processes, minimize waste, and reduce resource consumption, thus enhancing both operational efficiency and environmental responsibility [25,26]. By adopting this approach, hospitals can not only improve their internal processes and patient care delivery but also contribute to broader sustainability goals, aligning their operations with global environmental standards and promoting long-term, sustainable growth.
2.1. Lean Thinking in Healthcare
Lean Thinking (LT) is a methodology that focuses on optimizing organizational processes, reducing waste, and continuously improving service delivery. Rooted in the Toyota Production System, LT emphasizes the efficient use of resources, enhancing customer satisfaction, and fostering a culture of continuous improvement (CI) across organizations [27,28,29]. Although it originated in the manufacturing sector, LT has since been widely adopted in various industries, including healthcare, where it is used to streamline processes and create agile, customer-focused systems [30,31,32,33].
In healthcare, Lean Thinking empowers leaders and managers to identify inefficiencies in service delivery, reduce waste and errors, and focus on adding value to patient care. This, in turn, enhances staff productivity and satisfaction, while also improving the overall patient experience [32,34,35]. Over the past two decades, hospitals have increasingly embraced Lean methodologies, recognizing their potential to optimize care delivery and resource management. The adoption of Lean Thinking and Six Sigma techniques has transformed the healthcare sector by introducing industrial process reorganization methods that improve efficiency and outcomes [36,37,38].
A key element of Lean Thinking in hospitals is the concept of “flow” and “pull.” These principles are particularly relevant to healthcare, where the timely and efficient delivery of services is essential to patient care. “Flow” refers to the smooth progression of tasks and services without unnecessary delays, while “pull” ensures that resources are allocated based on real-time demand, rather than stockpiling supplies or over-preparing for uncertain needs [39,40]. By applying these principles, hospitals can significantly improve their operational processes, ensuring that patient care is delivered more efficiently, effectively, and in a manner that minimizes waste.
In addition to Lean Thinking, several complementary methodologies have been integrated into hospital operations to enhance customer value and improve service delivery. These approaches include quality management systems, demand variability controls, and resource availability strategies, all of which align with the core objectives of Lean Thinking. Together, these strategies create a cohesive operational framework that maximizes hospital efficiency while maintaining a focus on high-quality patient care [41,42]. Although these concepts were not originally part of Lean Thinking, they have been successfully incorporated to extend their impact in healthcare environments [43,44].
Lean Thinking, Six Sigma, and Lean Six Sigma (LSS) have emerged as the most frequently published and applied continuous improvement (CI) methodologies in healthcare, particularly in hospitals. These approaches are regularly cited in academic and professional publications as effective methods for improving hospital operations and enhancing patient care [45,46]. According to Henrique et al. (2021) [39], Lean Thinking, Six Sigma, and LSS are the most commonly employed CI techniques in hospitals, as evidenced by their frequent use in both research and practice. These methodologies not only improve operational efficiency but also foster a culture of continuous improvement, adaptability, and excellence within healthcare institutions, ensuring that hospitals can effectively respond to evolving patient and stakeholder needs.
Although GLSS has the potential to improve efficiency and reduce waste, many healthcare facilities face substantial obstacles in its implementation. Resource constraints, particularly in low-income settings, limit the ability of hospitals to allocate necessary funds for training and technological upgrades. Additionally, institutional resistance to change presents a significant hurdle. Employees accustomed to established routines often exhibit hesitance toward adopting new practices, particularly when the perceived benefits of GLSS are not immediately clear [42,46,47].
In any case, by incorporating these strategies into their operations, hospitals can establish a solid foundation for continuous improvement, leading to better patient outcomes, enhanced operational performance, and a sustainable competitive advantage in the healthcare sector.
2.2. The Role of Green Lean Six-Sigma
Green Lean Six Sigma (GLSS) is an innovative methodology that merges the principles of Lean Six Sigma (LSS) with green, environmentally sustainable practices. Traditionally, LSS focuses on eliminating waste, reducing process defects, and optimizing organizational performance [48]. However, while LSS excels at improving efficiency, it does not fully address the environmental impacts of operations. Recent research has shown that integrating green practices into the LSS framework significantly enhances environmental performance, making operations more eco-friendly and resource-efficient [49,50,51,52,53].
The gap between LSS and environmental responsibility is bridged by incorporating green technology into the process improvement strategies of LSS. This integration results in a comprehensive GLSS methodology, which balances operational improvements with sustainability objectives. By implementing GLSS, organizations can optimize their processes while also reducing their environmental footprint, thus aligning their operations with broader sustainability goals [54,55,56,57].
In healthcare settings, the adoption of GLSS is particularly beneficial. Hospitals are tasked with providing high-quality patient care while also reducing their carbon footprint and complying with environmental regulations. Through GLSS, healthcare institutions can enhance process efficiency, minimize waste, and reduce their environmental impact, all while maintaining a focus on delivering high-quality care [54,58]. This dual focus on operational excellence and sustainability enables hospitals to meet the evolving demands of both patients and regulatory bodies, ensuring long-term viability and community well-being.
This gap is addressed by incorporating green technology, which adds a sustainability dimension to LSS, resulting in the comprehensive GLSS strategy which effectively balances process improvement with environmental responsibility [59,60].
In healthcare, GLSS is particularly beneficial, as hospitals must deliver high-quality patient care while complying with environmental regulations and reducing their carbon footprint. By implementing GLSS, healthcare institutions can improve process efficiency, reduce waste, and minimize environmental impact, aligning with sustainable development goals that promote both regulatory compliance and community well-being [61,62].
The adoption of GLSS in hospitals aligns with the increasing focus on sustainable development, which integrates economic, social, and environmental considerations into organizational strategies [63]. As more hospitals embrace industrial process reorganization, GLSS provides a solid framework for continuous improvement, fostering innovation and sustainability in healthcare operations [17,64].
Overall, GLSS represents a strategic advancement in improvement methodologies, combining the strengths of LSS with the sustainability benefits of green technology. This integrated approach not only enhances hospital operations but also ensures that healthcare providers can meet the evolving needs of patients and stakeholders while contributing to a sustainable future [65,66,67,68,69].
2.2.1. Implementing GLSS in Healthcare
GLSS exemplifies a holistic approach to healthcare that effectively minimizes patient stays, optimizes space utilization, reduces medical errors, and expedites the delivery of medical services. By applying GLSS tools, healthcare facilities can efficiently manage patient treatment areas, maintain workplace hygiene, and improve ward management, leading to enhanced operational efficiency and patient care quality [68,69].
During the COVID-19 pandemic, the implementation of Lean practices proved invaluable. It maximized healthcare facility capacity utilization and managed hospital supply chains effectively to meet the unprecedented demands across regions. GLSS facilitated the rapid adaptation of healthcare services, ensuring that hospitals could handle surges in patient numbers while maintaining high standards of care [70,71,72].
Furthermore, GLSS enhances operating room safety, patient well-being, and cleanliness through the systematic application of its tools. This model embodies a sustainable approach to patient care, emphasizing the 3Rs: reduce, reuse, and recycle [39]. In the hospital context, “reduce” translates to shorter patient stays, reduced inventory levels, and cost-efficient patient care processes. “Reuse” involves the sustainable management of resources such as linen, wastewater, and other reusable items. “Recycle” pertains to the responsible handling of materials like paper, water, glass, cardboard, plastic, metal, and medical waste.
Despite its extensive industrial applications, the adoption of GLSS in hospitals remains limited. This gap presents a significant opportunity for the healthcare sector to leverage GLSS’s full potential. By integrating GLSS principles, hospitals can achieve a balanced approach to high-quality patient care and environmental sustainability [59,73,74].
The strategic integration of GLSS in healthcare aligns with broader sustainable development goals. It supports both present and future needs by embedding economic, social, and environmental considerations into hospital operations [60,63,64]. As more hospitals adopt industrial process reorganization methods, GLSS offers a robust framework for continuous improvement, fostering innovation and sustainability within healthcare operations [17,48,75,76].
In summary, GLSS represents a significant advancement in continuous improvement methodologies for healthcare. It combines the efficiency and waste reduction benefits of Lean Six Sigma with the sustainability advantages of green technology. This integrated approach not only enhances hospital operations but also ensures that healthcare providers can meet evolving patient and stakeholder expectations while contributing to a sustainable future. By reducing patient stays, optimizing space, managing resources efficiently, and emphasizing the 3Rs, GLSS positions hospitals to achieve both operational excellence and environmental stewardship.
2.2.2. Project Selection and Success Factors
GLSS begins with the critical phase of project selection, which involves identifying practical projects, selecting appropriate indicators, and ensuring proficiency with the necessary tools for execution [77,78,79]. This initial step sets the stage for the entire GLSS process. Success factors are pivotal for effective GLSS implementation, and these include clear project goals, stakeholder engagement, and continuous monitoring [3,23]. Understanding the interrelationships among these factors is crucial for establishing a robust and sustainable implementation framework.
Notably, there is a scarcity of research focusing on GLSS in hospital settings. The limited scholarly literature addressing comprehensive frameworks for long-term implementation exacerbates the issue. Most existing publications are theoretical rather than empirical, offering minimal insights into real-world applications and outcomes. This research gap heightens the risk of unsuccessful GLSS implementation in hospitals, as the lack of practical guidance and case studies leaves healthcare institutions without a clear roadmap [80].
Furthermore, hospitals face unique challenges that differ from those in other industries, making the adaptation of GLSS more complex in the era of the fourth industrial revolution. The dynamic and sensitive nature of healthcare environments requires tailored approaches that account for patient safety, regulatory compliance, and the need for uninterrupted services. This complexity underscores the importance of developing and sharing empirical research and best practices specifically focused on GLSS in healthcare [81,82].
To bridge these gaps, it is essential to conduct more empirical studies that document the implementation process, challenges, and successes of GLSS in hospital settings. Such research should aim to develop comprehensive, practical frameworks that can guide healthcare institutions through the intricacies of GLSS adoption. These frameworks should ideally include detailed case studies, step-by-step guidelines, and performance metrics that reflect the unique requirements of the healthcare sector.
Additionally, fostering collaboration among hospitals, academic institutions, and industry experts can facilitate the exchange of knowledge and experiences [70,83], contributing to a deeper understanding of GLSS implementation in healthcare. This collaborative approach can lead to the development of standardized best practices and training programs that equip healthcare professionals and academics with the skills and knowledge needed to execute GLSS effectively.
In summary, while GLSS offers significant potential benefits for hospitals, its successful implementation requires a thorough understanding of critical success factors, practical application, and a robust empirical foundation. Addressing the current research gaps through focused studies and collaborative efforts will be crucial for enabling healthcare institutions to harness the full potential of GLSS, ultimately leading to improved patient care, operational efficiency, and environmental sustainability.
2.3. Research Questions (RQ)
Based on the preceding analysis of the literature, the following research questions are derived to explore healthcare workers’ perspectives on GLSS. This connection to the literature is justified as it highlights the significance of understanding healthcare professionals’ awareness, attitudes, readiness, and perceived challenges regarding GLSS implementation. The specific research questions aim to gather detailed insights that are crucial for addressing the gaps identified in the literature, particularly in the context of applying GLSS in healthcare settings. These questions are as follows:
- RQ1: What is healthcare workers’ level of awareness of, understanding of, and familiarity with GLSS, including Lean Thinking, Six Sigma, and sustainability practices?
- RQ2: What are the general attitudes, perceptions, and initial reactions of healthcare professionals towards the concept of GLSS?
- RQ3: How ready are healthcare professionals to adopt GLSS in their work environment, and what factors influence their readiness?
- RQ4: What key challenges, barriers, and concerns do healthcare professionals anticipate regarding the implementation of GLSS, particularly related to resource constraints and training needs?
- RQ5: What types of support, including leadership and organizational strategies, do healthcare professionals believe are necessary for the successful adoption and sustainability of GLSS initiatives?
3. Materials and Methods
This study explores the adoption of GLSS in healthcare by examining healthcare workers’ perceptions, readiness for change, and the challenges associated with implementation. It aims to assess awareness, attitudes, and barriers while identifying support needs for effective GLSS integration. Using an exploratory qualitative approach, the study employs semi-structured interviews with healthcare professionals and academics to capture detailed insights into their views. This method allows for a deep understanding of the factors influencing the successful adoption of GLSS practices in complex healthcare settings.
3.1. Objectives
The objectives of this study are centered on gaining a deep understanding of the initial perceptions and practical implications of implementing GLSS in healthcare settings. These objectives guide the research process and inform the development of research questions to capture comprehensive insights. The specific objectives are as follows:
- Assessing Awareness and Understanding:
To evaluate the awareness and understanding of GLSS among healthcare workers and stakeholders.
- 2.
- Exploring Attitudes and Perceptions:
To capture the initial reactions, enthusiasm, skepticism, or hesitancy regarding the adoption of GLSS methodologies in healthcare environments.
- 3.
- Evaluating Readiness for Change:
To identify the factors influencing healthcare professionals’ readiness to embrace and engage with GLSS initiatives, including organizational culture and personal motivation.
- 4.
- Uncovering Challenges and Barriers:
To identify the primary challenges and barriers healthcare professionals foresee in adopting and implementing GLSS practices, such as resource limitations, training gaps, or resistance to change.
- 5.
- Determining Support Needs:
To determine the specific support, such as leadership guidance, training programs, and resource allocation, that healthcare workers need to effectively implement GLSS practices in their respective institutions.
3.2. Qualitative Research Design
This study adopts a qualitative research design with an exploratory framework to understand the perceptions and attitudes of healthcare professionals and academics regarding the adoption of GLSS in healthcare settings. The qualitative approach is particularly well suited for exploring complex, subjective experiences, which quantitative methods may not adequately capture. This design allows the researcher to delve deeply into the participants’ perspectives and gather insights that are contextual, nuanced, and rich in detail [84,85].
Qualitative research, especially with an exploratory design, is ideal for this study because it allows for flexibility in capturing emerging ideas and themes during the research process. In contrast to fixed, hypothesis-driven research, this approach enables the researcher to remain open to new patterns of thought that may arise during the data collection phase, thus providing a more holistic view of the phenomena under investigation [86,87].
The use of semi-structured interviews was chosen as the primary data collection method. This interview format provides a balance between structure and flexibility, ensuring that key research questions are addressed while also allowing the participants to share their experiences freely. The semi-structured format enables the interviewer to ask follow-up or probing questions based on the participants’ responses, thus facilitating a deeper exploration of certain topics or themes [86,87].
The following key advantages of semi-structured interviews justify their use in this study:
- Flexibility: Semi-structured interviews allow for adaptability during the interview process. If participants raise unexpected topics relevant to the research, the interviewer can explore these areas further without deviating from the core objectives of the study.
- Depth: The open-ended nature of the questions provides an opportunity for participants to explain their thoughts in their words, giving researchers deeper insights into their perceptions of GLSS implementation.
- Emerging Themes: As the interviews progressed, certain themes and ideas emerged that had not been anticipated during the research design phase. Semi-structured interviews are well suited for capturing such emerging themes, which were further explored in subsequent interviews [88,89].
Additionally, the qualitative design of this study prioritizes the contextual understanding of GLSS practices in healthcare. This is important, as the adoption of GLSS principles, which combine lean management strategies and environmental sustainability, depends heavily on organizational culture, staff perceptions, and the unique challenges of the healthcare environment. By employing qualitative methods, this study captures these subjective and context-dependent factors, which quantitative approaches may overlook [88,89].
Bias Consideration in Research Design: One important issue in qualitative research design is the potential for bias. Researchers need to be aware of how their own views and interpretations might influence the study. To mitigate this, interview protocols were designed with neutral language to avoid leading questions. Moreover, the inclusion of a diverse group of participants—both in terms of their professional backgrounds and levels of familiarity with GLSS—helped reduce selection bias and ensured a more balanced representation of opinions [87,89].
In summary, the qualitative research design, combined with semi-structured interviews, enabled this study to capture comprehensive and nuanced insights into healthcare professionals’ perceptions of GLSS. This approach ensured that emerging themes were identified and explored while maintaining a structured focus on the key research objectives.
3.3. Sampling and Participant Selection
This study utilizes purposive sampling to select 16 participants, which is a common strategy in qualitative research aimed at selecting individuals with relevant experience or expertise in a particular area. This sample includes healthcare workers and academics who are either directly involved in or have an understanding of the processes surrounding GLSS [90,91,92].
Purposive sampling was chosen for its ability to ensure a targeted and meaningful participant pool, focusing on healthcare professionals from diverse roles, including clinical, administrative, and support services. The selection process aimed to gather insights from participants at different levels of familiarity with Lean, green, and Six Sigma principles to provide a comprehensive overview of perspectives regarding GLSS adoption.
Given that qualitative research prioritizes depth over breadth, a sample size of 16 was deemed sufficient for achieving data saturation—where new data cease to add novel insights. Although relatively small, this sample captures a wide range of perspectives from different departments and professional levels within the healthcare sector, reflecting a diverse range of experiences and expertise necessary for addressing the study’s objectives [93,94].
3.4. Data Collection Procedures
Data were collected through semi-structured interviews conducted with each participant. The semi-structured format allowed for flexibility with regard to probing deeper into emerging themes while maintaining focus on the key research questions. The interview questions were designed to be open-ended to promote an open dialogue and to elicit detailed responses [86,94,95]. This structure allowed participants to elaborate on their experiences with GLSS, contributing to a rich understanding of their perceptions and attitudes [95,96,97].
Interviews were conducted at the convenience of the participants, either in person or through video conferencing platforms, depending on the participants’ availability and preference. Each interview lasted approximately 20 to 30 min. To ensure consistency, all interviews followed a prepared interview protocol, which included questions on the participants’ understanding of GLSS, perceived benefits, challenges, and suggestions for effective implementation. These interviews were recorded with participants’ consent, and detailed notes were taken.
In line with the request for increased transparency, possible biases in participant selection were considered. Although purposive sampling is designed to select those with relevant expertise, there is an inherent risk of selection bias, as participants are chosen based on the researcher’s judgment of their relevance to the study. To mitigate this, efforts were made to include a diverse group of healthcare professionals from various roles and departments, thereby reducing the influence of any single perspective or bias [90,91,92]. Additionally, participants with differing levels of familiarity with Lean and GLSS practices were included to ensure the data captured a range of viewpoints, reducing the risk of homogeneity in responses [98].
3.5. Data Analysis Techniques
The study employed a thematic analysis approach to interpret and identify patterns within the qualitative data. This method is particularly useful for organizing complex datasets, allowing researchers to highlight significant ideas and link them to broader themes within the research context [99,100,101]. Thematic analysis is not only flexible but also systematic, ensuring a structured exploration of qualitative insights.
Key Steps in the Data Analysis:
- ▪
- Transcription: All interviews were recorded and transcribed verbatim to ensure the accuracy of the data. Verbatim transcription was essential for capturing the nuances of the participants’ responses and facilitated detailed analysis.
- ▪
- Familiarization: The research team reviewed the transcripts multiple times to become thoroughly familiar with the data, noting key phrases, emerging themes, and significant ideas. This step was crucial for understanding the depth of the participants’ responses and identifying recurring patterns.
- ▪
- Initial Coding: NVivo 14 software was used to assist in coding the data. Codes were generated to capture essential features related to participants’ perceptions, including perceived benefits, barriers, and overall views on GLSS practices [102,103]. The use of NVivo facilitated the efficient organization and retrieval of data related to specific topics, enhancing the rigor and transparency of the analysis process.
- ▪
- Theme Development: Following the coding process, NVivo was also used to cluster similar codes into broader themes. These themes were analyzed to identify patterns and connections, helping researchers understand the underlying trends in the data. Examples of key themes developed are as follows:
- ○
- Efficiency gains perceived by participants.
- ○
- Concerns about environmental sustainability.
- ○
- Identified training and educational needs for healthcare workers.
- ○
- Anticipated barriers to successful implementation, such as organizational resistance or limited resources.
- ▪
- Refining Themes: Through an iterative process, the identified themes were reviewed and refined to accurately represent the participants’ views. This step also involved identifying discrepancies or contrasting opinions within the data, ensuring that the analysis provided a nuanced and comprehensive understanding of the findings [102,103].
The thematic analysis was essential for managing the large volume of qualitative data, allowing the researchers to systematically code and interpret the data and to revisit and refine themes as necessary. NVivo software played a critical role in ensuring the credibility of the findings by offering structured, transparent, and rigorous data management tools. This method enabled the researchers to develop a clear understanding of the participants’ perspectives on GLSS practices while also addressing complex and evolving themes.
3.6. Addressing Biases
The study recognized potential biases that may arise from the purposive sampling technique and researcher influence during interviews. These biases are listed below.
- Selection Bias: Given the purposive nature of participant selection, there is a potential bias in the representation of views, as the sample may over-represent individuals more favorable to or familiar with Lean and green methodologies. To counter this, participants from a wide range of healthcare roles and experiences were included, ensuring a broader spectrum of opinions [95,97].
- Researcher Bias: Interviewers may inadvertently introduce bias during the data collection process through their assumptions or by leading questions. To reduce this risk, interviewers followed a structured protocol and conducted mock interviews to ensure neutrality and consistency [96,97].
3.7. Ethical Considerations
Ethical considerations were central to the research design and implementation. Before conducting the interviews, participants were provided with detailed information about the study’s objectives, the nature of their participation, and how their data would be used. Informed consent was obtained from all participants to ensure that they were aware of their right to withdraw from the study at any point [104,105].
Confidentiality was maintained throughout the research process. Participants’ identities were anonymized in the transcripts, and any identifying information was removed to protect their privacy. The data were securely stored and accessible only to the research team.
4. Results
4.1. Participant Demographics
This section provides an overview of the demographics of the healthcare providers and professors who participated in the study. A total of 16 participants were interviewed, representing a diverse range of roles within the healthcare sector. The participants included frontline clinical staff, such as medical doctors and nurses, as well as other healthcare personnel. University professors with experience in teaching healthcare-related subjects also took part. The sample varied in terms of years of experience in the healthcare field, with some participants having experience implementing or interacting with Lean and green practices, while others were relatively new to these concepts.
The demographic breakdown of the participants is as follows:
- -
- Gender: 50% female, 50% male.
- -
- Age Range: Participants ranged from 30 to 62 years old, with the majority (64%) falling within the 45.73 bracket.
- -
- Years of Experience: Participants had between 9 years and 30 years of experience in healthcare, with a mean of 21.38.
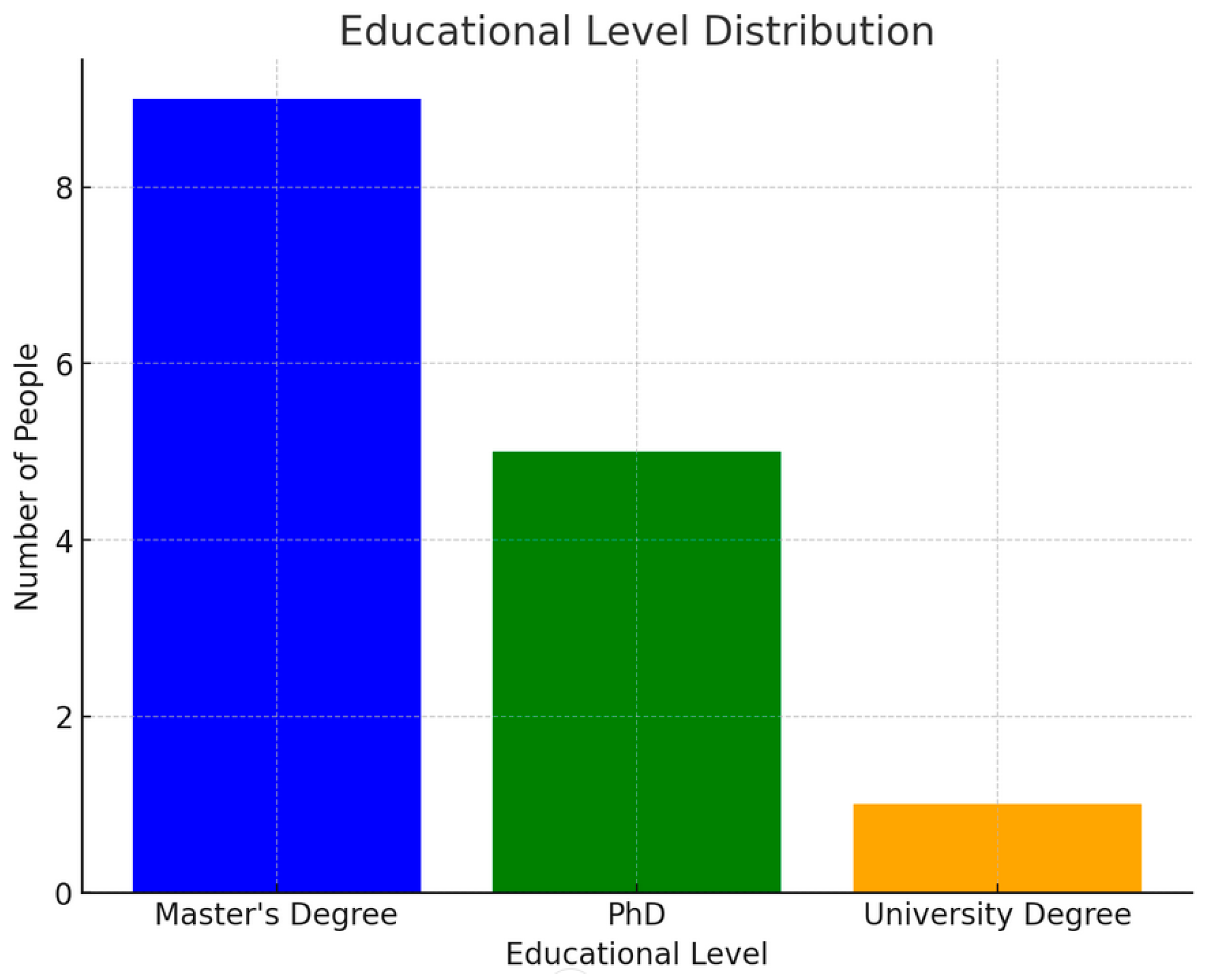
The bar chart labeled Chart 1 illustrates the distribution of educational levels among a group of 16 individuals. This chart provides a visual representation of how many people fall into each educational category. Specifically, it highlights the number of individuals who have attained a Master’s Degree, a PhD, or a University Degree. By breaking down the group according to these educational levels, the chart offers a clear comparison of how many people are represented in each category.
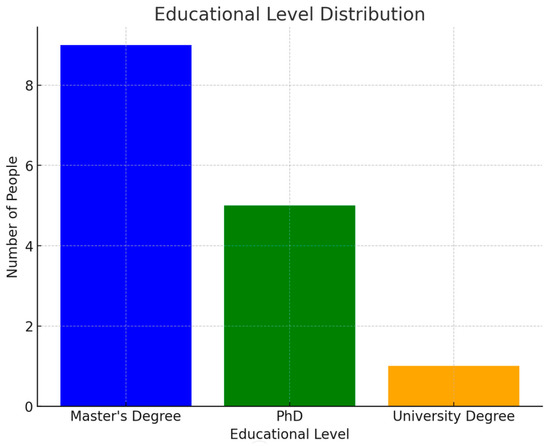
Chart 1.
Educational Level Distribution. The chart was created by the authors of the article.
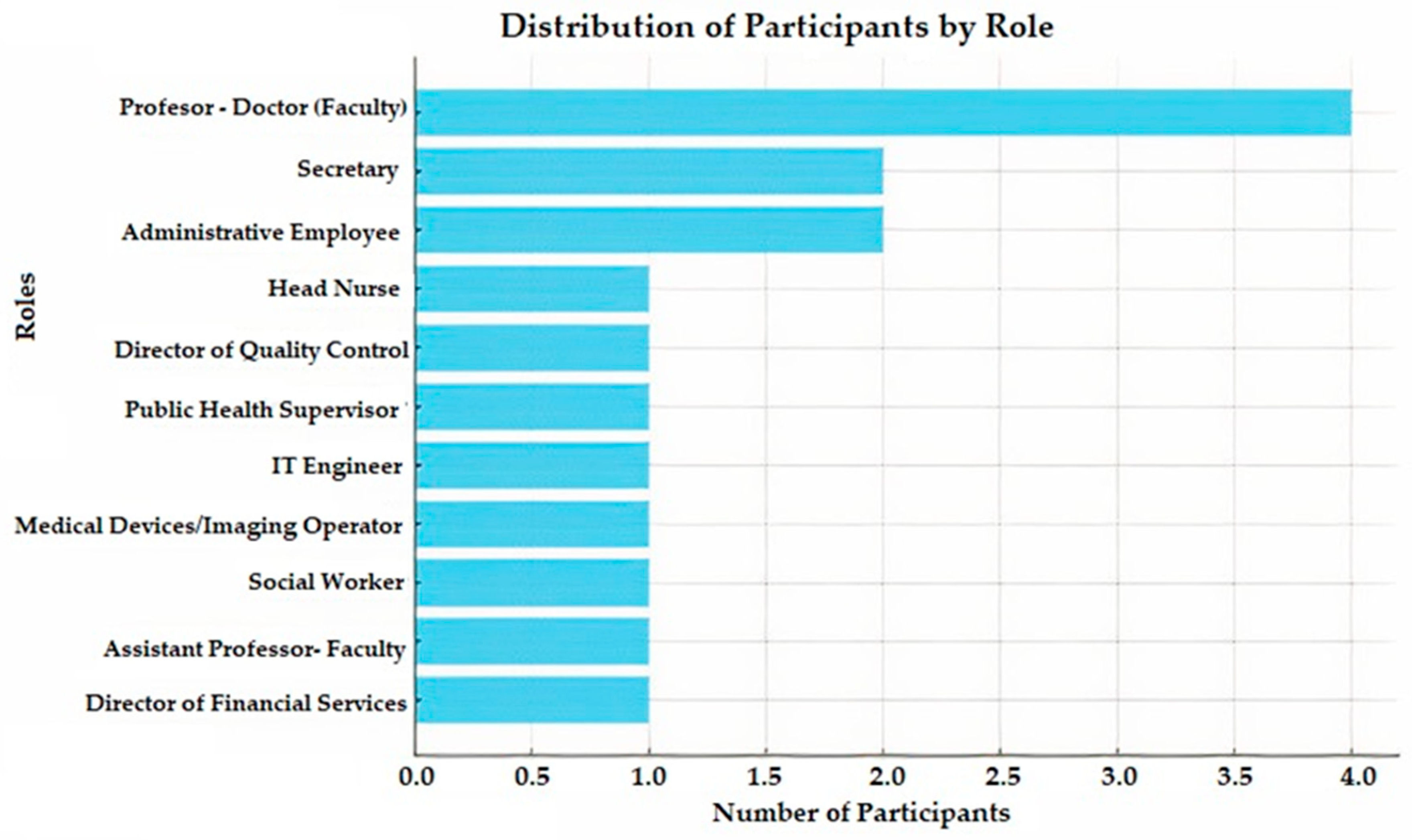
Moreover, Chart 2 displays the distribution of participants by their professional roles in the research related to GLSS for hospitals. It provides a detailed breakdown of the 16 individuals, each with a unique position within the healthcare or academic sectors. Moreover, of the 16 participants, 44% were healthcare providers, 38% were administrative staff, and 31% were academics. Some individuals held dual roles, such as academic medical doctors who worked in hospitals while simultaneously serving as faculty members at universities.
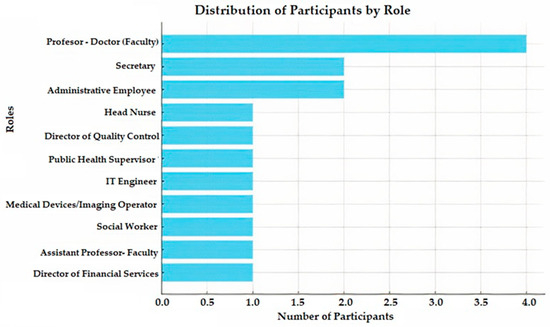
Chart 2.
Distribution of Participants by Role. This chart was created by the authors of the article.
The chart includes a range of roles that reflect the diverse functions involved in the research. These roles include a Head Nurse, a Director of Quality Control in Business Administration, and a Public Health Supervisor, with each bringing distinct perspectives from healthcare management and oversight. Additionally, there is representation from the field of technology, as an IT Engineer is also part of the group, emphasizing the role of technical support in hospital operations.
Administrative roles are well represented in the chart, which features two Secretaries and two Administrative Employees, highlighting the importance of organizational support in the healthcare system. The graph also includes a Medical Devices/Imaging Operator, whose role is crucial for handling and maintaining diagnostic equipment in hospitals, and a Social Worker, reflecting the focus on patient care beyond medical treatment.
The academic side is depicted by an Assistant Professor and four professors holding Doctorate degrees (faculty), indicating significant involvement from the educational sector. Their expertise likely contributes to the research from a theoretical and analytical standpoint.
Lastly, the chart captures the participation of senior-level management, represented by the Director of Financial Services, underscoring the importance of financial oversight and budgeting in hospital operations.
By visualizing the frequency of these roles, the graph offers a comprehensive view of the varied expertise and professional backgrounds that contribute to the research on GLSS in hospitals. This diversity is crucial for a holistic approach to the study, ensuring that multiple aspects of hospital functioning are considered.
This diverse representation ensures that the findings reflect a wide range of perspectives and experiences, providing a comprehensive understanding of the attitudes towards GLSS in healthcare.
4.2. Key Themes
The analysis of the interviews revealed several key themes that offer insights into healthcare professionals’ and academics’ awareness, perceptions, and concerns regarding the adoption of GLSS practices in their work environment.
4.2.1. General Awareness and Initial Impressions of Potential Impact of GLSS in Hospitals
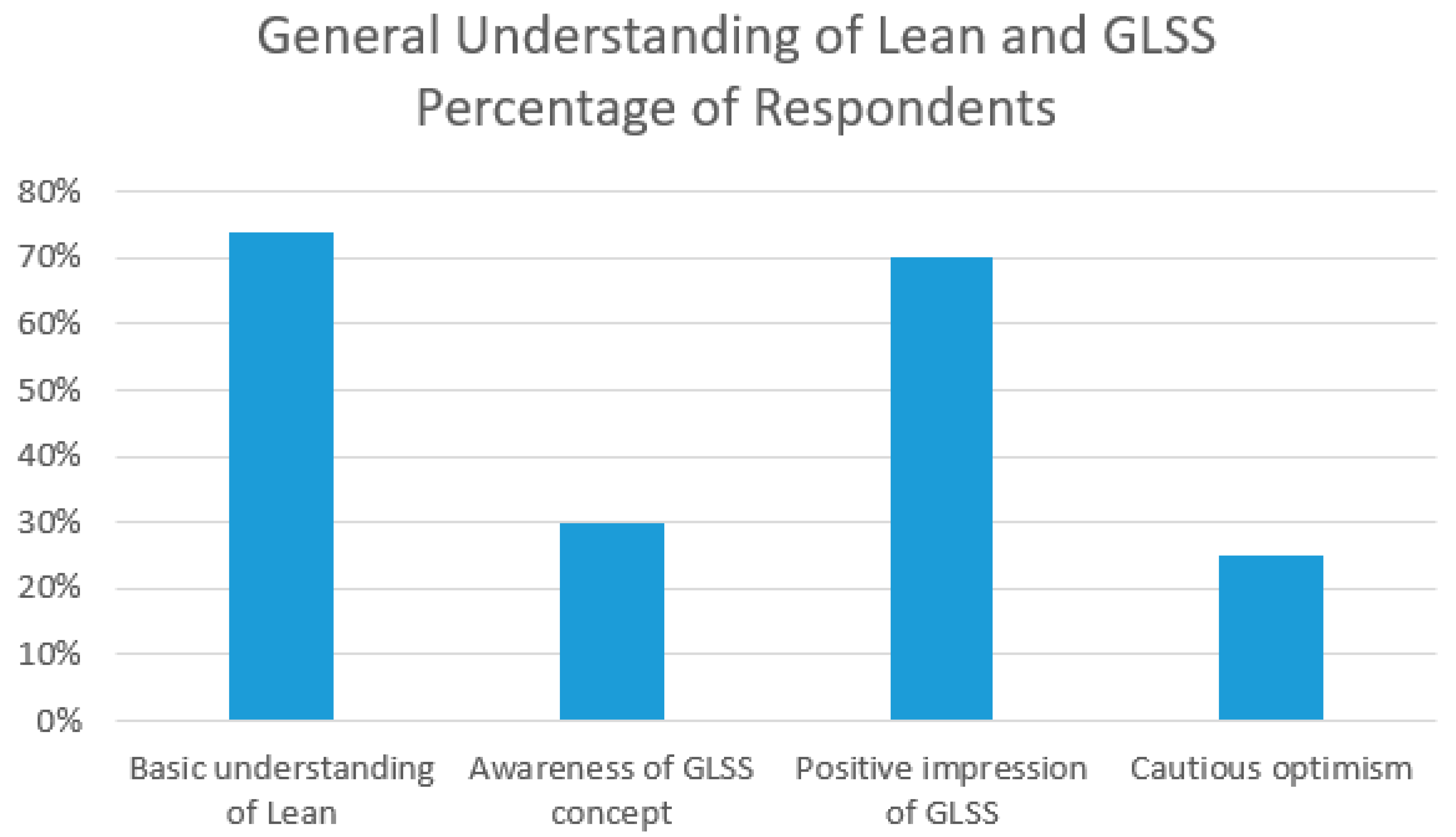
Overall, 74% of participants (see Chart 3) expressed a basic understanding of Lean practices, particularly in process optimization and waste reduction. However, awareness of the specific GLSS concept was limited (30%), with many (70%) expressing unfamiliarity with integrating green practices into Lean methodologies. Those who were aware of GLSS generally encountered it through workplace initiatives or professional development courses, suggesting that awareness is still emerging in the healthcare sector. Despite this, the introduction of GLSS in hospitals has generated a range of positive initial impressions (75%) among healthcare professionals and academics. However,25% of respondents expressed cautious optimism, noting that while GLSS shows promise, its success will depend on careful implementation and sustained commitment. This section explores these impressions, highlighting the most significant themes that emerge from their perspectives and reflecting the collective thoughts of hospital staff on GLSS’s potential impact:
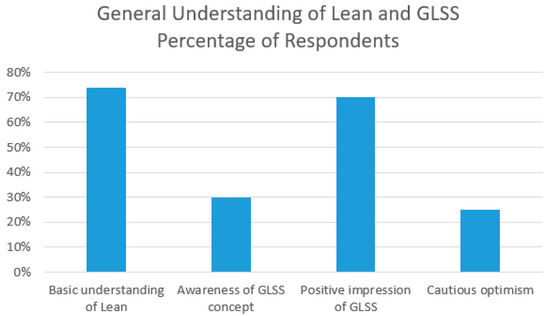
Chart 3.
General Understanding of Lean and GLSS. This chart was created by the authors of the article.
- Social, Economic, and Environmental Benefits:
- A predominant theme among the respondents is the anticipation of substantial social, economic, and environmental benefits as a result of implementing “GLSS. Several individuals noted that the methodology would lead to better resource management, which in turn could yield significant improvements in the hospital’s social and environmental impact. They foresee a waste reduction, lower operational costs, and enhanced sustainability practices, all of which contribute to a positive societal influence.
- Improvement in Healthcare Quality and Efficiency:
- Another critical area highlighted by the respondents is the potential for GLSS to enhance the quality and efficiency of healthcare services. The methodology is seen as a tool for refining hospital processes, leading to improved patient care. By streamlining operations and optimizing resource use, GLSS can help hospitals deliver higher-quality services while minimizing unnecessary expenditure and resource consumption. This focus on efficiency aligns closely with the overarching goals of healthcare institutions to provide the best possible outcomes for patients with the most efficient use of resources.
- Environmental Sustainability:
- Environmental protection is a significant concern in the healthcare sector, and GLSS is perceived as a method that can directly address this issue. Many respondents expressed optimism about the methodology’s ability to reduce the hospital’s environmental footprint. By focusing on reducing waste and pollution, GLSS can help hospitals operate more sustainably, which is increasingly important in a world facing environmental challenges.
- Improved Working Conditions:
- Several professionals mentioned that the implementation of GLSS could lead to improved working conditions within hospitals. The methodology’s emphasis on process improvement is expected to create a more organized and efficient work environment, which can enhance staff satisfaction and productivity. This improvement in the workplace not only benefits the employees but also contributes to better overall hospital performance.
- Positive Expectations with Cautious Optimism:
- While the majority of initial impressions are overwhelmingly positive, there is a note of cautious optimism. Some respondents recognize the potential benefits but emphasize that the effectiveness of GLSS will ultimately depend on its practical application. They are hopeful that the methodology will live up to its promises but acknowledge that successful implementation will require careful planning, commitment, and continuous evaluation.
In summation, the initial impressions of GLSS in hospitals are largely positive, with healthcare professionals and academics recognizing its potential to significantly improve resource management, service quality, environmental sustainability, and working conditions. Despite varying levels of familiarity with GLSS, participants consistently highlighted its potential benefits, particularly its potential to enhance operational efficiency by reducing waste and streamlining processes. Furthermore, GLSS is seen as a means to improve patient care by allowing healthcare professionals to focus more on patient-centered activities rather than administrative tasks. The integration of green practices is also viewed as a positive step toward meeting environmental regulations and reducing the carbon footprint of healthcare facilities. However, there is an acknowledgment that the true impact of GLSS will only be realized through effective and sustained implementation, as hospitals continue to explore and adopt these practices, building on the strong foundation of these initial expectations.
4.2.2. Potential Barriers, Concerns, and Challenges Related to Implementing GLSS Principles in Hospital Settings
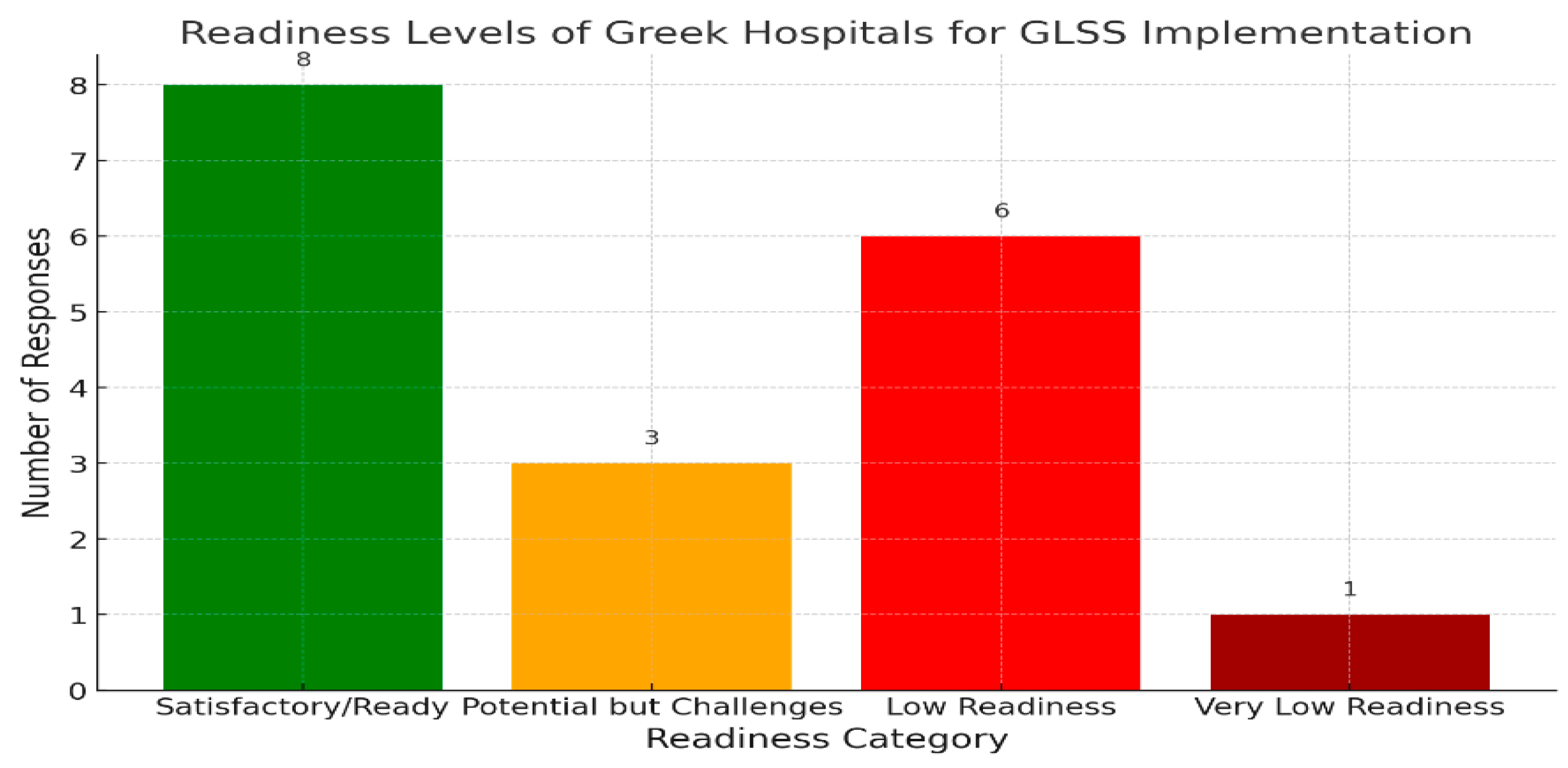
A total of 45% percent of participants identified resource constraints, including the time and financial investment required for staff training and the adoption of new practices, as a major challenge (see Chart 4). They also noted potential cultural resistance, with some healthcare workers being hesitant to adopt new methodologies due to a lack of understanding or fear of change. Emphasizing the importance of ongoing support and leadership commitment, participants warned that without such backing, GLSS initiatives might struggle over time. This section examines these significant obstacles, grouping them into key themes for a comprehensive analysis to aid in overcoming barriers and ensuring effective adoption.
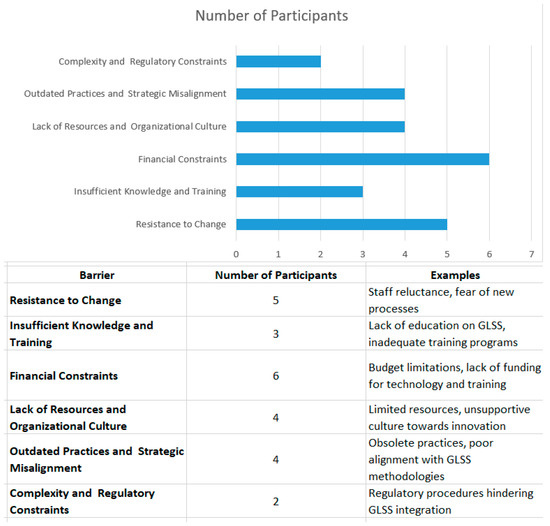
Chart 4.
Key Barriers to GLSS Implementation in Healthcare. This chart was created by the authors of the article.
- Resistance to Change:
- One of the most frequently cited barriers is resistance to change. Five participants have highlighted that both staff and management often resist altering established routines and practices. This resistance can stem from a lack of understanding, fear of the unknown, or simple inertia. Overcoming this barrier requires targeted strategies, including change management programs and active engagement with all levels of staff to foster a culture of adaptability.
- Insufficient Knowledge and Training:
- A related issue is the lack of sufficient knowledge and training about GLSS principles. According to three participants, inadequate training and a lack of understanding of the benefits of GLSS contribute to ineffective implementation. This can be compounded by an overall deficiency in communication and education about the methodologies. Addressing this barrier involves investing in comprehensive training programs and ensuring that educational resources are available to all relevant personnel.
- Financial Constraints:
- Financial constraints represent a significant hurdle as well. As noted by six participants, hospitals often face budget limitations that impede their ability to invest in the necessary resources for implementing GLSS principles. These constraints can affect both the acquisition of new technologies and the funding for training programs. Solutions may include seeking alternative funding sources, optimizing existing resources, and demonstrating the long-term cost benefits of GLSS to secure financial support.
- Lack of Resources and Organizational Culture:
- The lack of resources and an unsupportive organizational culture also pose challenges. Limited resources can hinder the implementation of GLSS practices, while an entrenched organizational culture that does not prioritize continuous improvement can obstruct progress. Developing a supportive culture requires leadership commitment, clear communication about the benefits of GLSS, and the creation of an environment that encourages innovation and process improvement.
- Outdated Practices and Strategic Misalignment:
- Some individuals have pointed out that outdated practices and strategic misalignment within hospital management can also be barriers. Anachronistic practices and resistance to adopting modern methodologies can slow down the implementation process. To address these issues, it is essential to align organizational strategies with GLSS principles and update practices to reflect current best practices.
- Complexity and Regulatory Constraints:
- Finally, complex and strictly regulated procedures present additional challenges. The rigid nature of some hospital procedures can complicate the integration of GLSS practices. To mitigate this, it is necessary to work within regulatory constraints while gradually introducing GLSS principles in a way that complements existing procedures and compliance requirements.
Chart 4 shows the key barriers identified by participants with regard to implementing GLSS principles in healthcare institutions. These challenges can be grouped into several themes for a comprehensive analysis, as summarized in the table below:
Moreover, many respondents expressed high expectations for GLSS, particularly regarding its potential social, economic, and environmental benefits. However, discussions also highlighted various concerns and challenges, suggesting that while the potential of this approach is clear, achieving these outcomes will require overcoming significant obstacles. The comparative Table 1 offers a balanced overview of both the anticipated benefits and the practical challenges, such as financial constraints, staff resistance, and integration issues, illustrating the complexities that must be managed to facilitate successful implementation.

Table 1.
Comparative Analysis Table: Anticipated Benefits vs. Potential Challenges.
It must also be highlighted that several participants expressed concerns over the financial investment required for the successful integration of GLSS. For instance, one hospital administrator cited the high cost of upgrading equipment and providing comprehensive training to staff, noting that without external funding or government subsidies, it is difficult to justify the immediate expenditure. Another common issue raised was the reluctance of senior staff to change established practices. A senior nurse remarked that many of their senior doctors are resistant to process changes, as they believe it disrupts the workflow and does not directly improve patient outcomes.
Cultural resistance to change is another challenge frequently mentioned by participants. One healthcare professional noted that GLSS may require changing long-established hierarchical structures, which can cause discomfort among staff who are used to traditional processes. This resistance is particularly prevalent in larger, public hospitals where systemic inertia and the complexity of operations further hinder the adoption of new methodologies.
Regardless, the implementation of GLSS principles in hospital settings encounters numerous barriers, including resistance to change, insufficient training, financial constraints, and lack of resources, outdated practices, and regulatory complexities. Respondents have emphasized the significant social, economic, and environmental benefits that GLSS can offer, yet practical challenges such as staff resistance, integration issues, and the need for strategic alignment remain. Addressing these obstacles requires a multifaceted approach, which involves targeted investments in training, fostering a culture of support and adaptability, securing necessary financial resources, and aligning organizational strategies with GLSS principles. A clear understanding of these complexities, paired with proactive solutions, will enable hospitals to successfully adopt GLSS methodologies and unlock their potential for improvement.
4.2.3. Key Factors for the Successful Implementation of GLSS in Hospitals
Implementing GLSS principles in hospital settings can significantly enhance operational efficiency and patient care. However, success in this implementation depends on several critical factors. These factors include adequate resource allocation, effective staff training, and the ability to navigate potential resistance to change [61,62]. This section synthesizes the most important elements identified by various experts, categorizing them into key themes that contribute to the effective adoption of GLSS in healthcare environments. By examining these elements, this section aims to provide a comprehensive framework for overcoming common barriers and ensuring the successful integration of GLSS methodologies in hospitals (Table 2):

Table 2.
Key Factors for the Successful Implementation of GLSS in Hospitals.
- Leadership Commitment
- A recurring theme among experts is the crucial role of leadership commitment. Effective implementation of GLSS principles requires strong support from hospital management. This includes not only endorsing the GLSS initiative but also actively participating in and promoting its objectives. Leadership commitment ensures that resources are allocated appropriately and that necessary organizational changes are made to facilitate the adoption of GLSS practices.
- Comprehensive Training and Education
- Training and education are essential for the successful application of GLSS principles. Properly educating staff on GLSS methodologies and their benefits is fundamental to overcoming resistance and ensuring that all team members are aligned with the initiative’s goals. Training should be continuous and hands-on, integrating practical application with theoretical knowledge to enhance understanding and competency.
- Incentives and Motivation
- Incentives and motivation are critical for encouraging staff engagement and adherence to GLSS practices. Providing appropriate rewards and recognition for contributions to process improvements can drive positive behavior and foster a culture of excellence. Incentives also help overcome resistance to change and maintain momentum throughout the implementation process.
- Resource Allocation
- The availability of necessary resources is another key factor for the successful implementation of GLSS. This includes financial resources, technology, and human capital. Adequate funding is required to cover the costs of new tools, training programs, and any additional expenses associated with the transition to GLSS practices. Ensuring that resources are used efficiently will help to achieve the desired outcomes of the GLSS initiative.
- Continuous Improvement and Innovation
- Fostering a culture of continuous improvement and innovation is essential for the long-term success of GLSS in hospitals. This involves regularly assessing and refining processes, encouraging innovative solutions to problems, and adapting strategies based on performance results. A commitment to ongoing improvement helps maintain the relevance and effectiveness of GLSS practices over time.
- Clear Communication and Transparency
- Clear communication and transparency are vital for ensuring that all stakeholders are informed and engaged. Effective communication strategies help clarify the goals of the GLSS initiative, outline expectations, and provide updates on progress. Transparency in reporting results and challenges also builds trust and facilitates collaborative problem-solving.
- Integration with Existing Protocols
- Integrating GLSS principles with existing hospital protocols and procedures can enhance the effectiveness of implementation. This involves aligning GLSS practices with current standards and workflows to ensure that they complement, rather than disrupt, existing processes. Proper integration helps achieve a seamless transition and maximize the benefits of GLSS.
In summary, the successful implementation of GLSS principles in hospital settings hinges on several key factors: strong leadership commitment, comprehensive training and education, effective incentives and motivation, adequate resource allocation, a focus on continuous improvement, clear communication and transparency, and the integration of GLSS with existing protocols. By addressing these factors, hospitals can better position themselves to achieve the benefits of GLSS, leading to improved efficiency, enhanced patient care, and a culture of excellence.
4.2.4. Readiness of Greek Public and Private Hospitals for the Implementation of GLSS Principles
This part explores Greek public and private hospitals’ current levels of readiness to implement these principles, based on qualitative insights from healthcare professionals. The findings reveal a spectrum of perspectives, reflecting both optimism and concern regarding the preparedness of these institutions.
- -
- Overview of Readiness Levels:
- The responses indicate a varied level of readiness across Greek hospitals, with certain institutions, particularly in the private sector, perceived as more prepared than others. There is general acknowledgment of the modernization efforts in hospitals and adherence to hygiene and safety protocols. However, significant concerns remain regarding the overall preparedness for the implementation of GLSS principles, particularly regarding organizational and managerial capabilities.
- -
- High-Readiness Institutions:
- Some healthcare professionals expressed confidence in their hospitals’ readiness, particularly at institutions where similar policies and quality assurance measures were already in place. For example, the modernization of public hospitals was cited as contributing to a satisfactory level of readiness. In these cases, existing infrastructure and the integration of quality assurance principles are seen as strong foundations for implementing GLSS. This confidence is further supported by widespread knowledge among healthcare professionals regarding hygiene and safety rules, which are already being followed in many hospitals.
- Additionally, there is recognition that certain public hospitals are structurally equipped to adopt GLSS principles, thanks to their adherence to established protocols and processes. These hospitals have already embraced modernization efforts, and as such are closely aligned with the goals of GLSS.
- -
- Challenges in Readiness:
- Despite the positive assessments, a significant portion of healthcare professionals expressed concerns about the readiness of Greek hospitals overall. A key issue that has been identified is weaknesses in management, particularly at the upper levels, where there is a lack of effective organization, communication, and staff motivation. These managerial shortcomings are seen as major obstacles to the successful implementation of GLSS principles.
- Another common concern is the difficulty many Greek hospitals face in adapting to innovations and changing work methods. This resistance to change contributes to the perception of low readiness, particularly in institutions that are not as advanced in their modernization efforts. Several healthcare professionals pointed out that, while there are exceptions, the overall readiness of both public and private hospitals remains low.
- The gap between intent and execution is also highlighted, with the Ministry of Health and the Greek Government showing a positive inclination toward adopting GLSS and other best practices. However, the lack of coordinated initiatives and necessary resources is a significant barrier to progress. This disconnect underscores broader systemic issues that hinder the widespread adoption of GLSS principles in the healthcare sector.
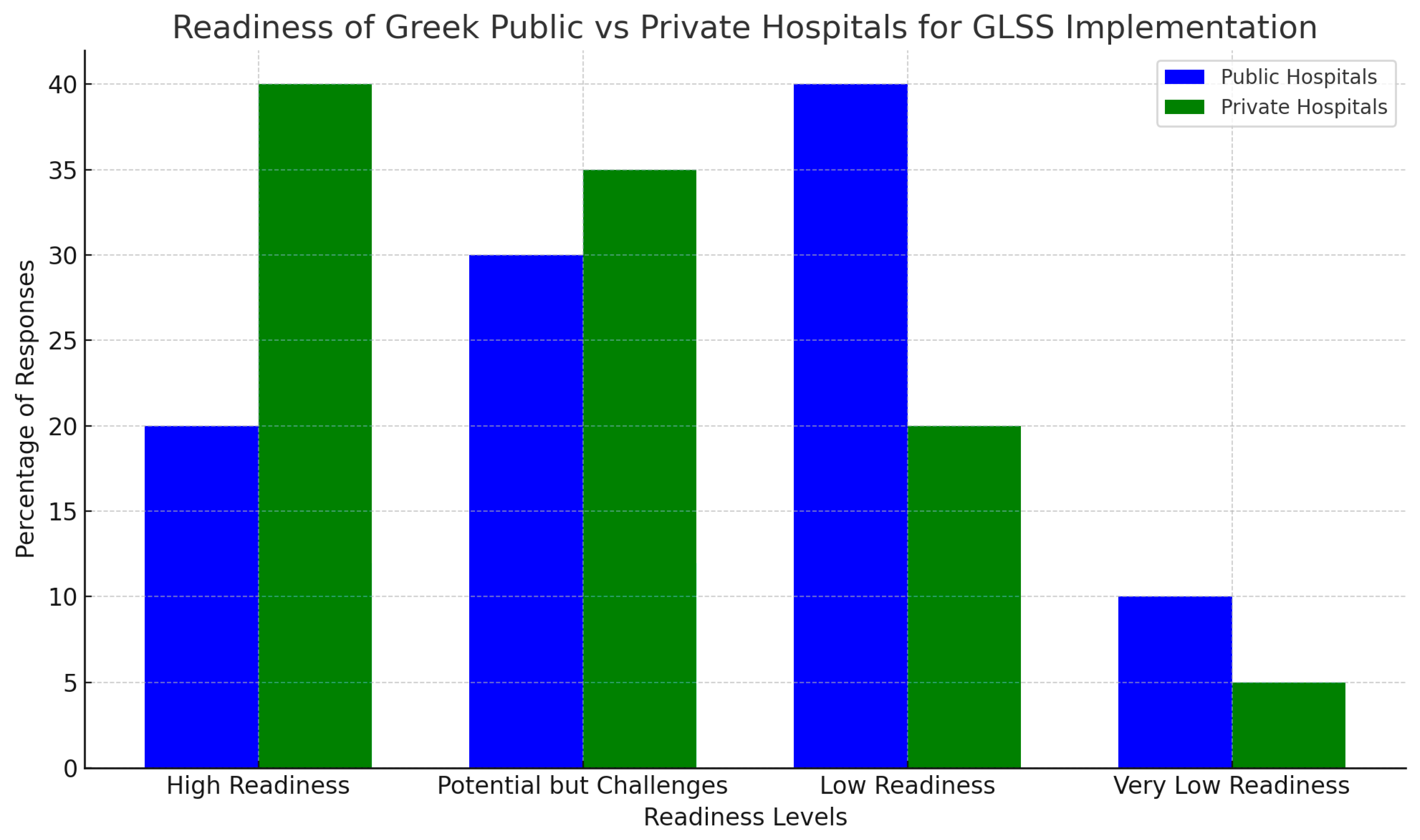
Chart 5 summarizes the responses regarding the readiness levels of Greek public and private hospitals for implementing GLSS principles. The chart categorizes the responses into four main groups:
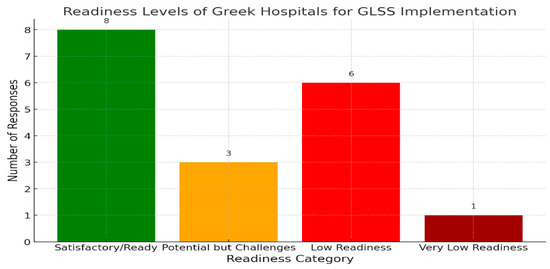
Chart 5.
Readiness Levels of Greek Hospitals for GLSS Implementation. The chart was created by the authors of the article.
- Satisfactory/Ready: eight responses indicated that certain hospitals are ready or have satisfactory levels of readiness.
- Potential Challenges: three responses acknowledged the potential for implementation but highlighted significant challenges, particularly with regard to management.
- Low Readiness: six responses described the readiness levels as low, with some noting exceptions or specific challenges.
- Very Low Readiness: one response indicated a very low level of readiness.
In summary, public and private Greek hospitals’ readiness to implement GLSS principles is mixed. While some institutions, particularly those that have already engaged in modernization and quality assurance initiatives, show a higher level of preparedness, significant challenges remain. Managerial weaknesses, resource constraints, and resistance to change are key barriers that need to be addressed. Although private hospitals may have certain advantages, the overall readiness across the healthcare system is inconsistent. To bridge the gap between intent and execution, targeted interventions and coordinated efforts are essential for the successful adoption of GLSS principles in Greek hospitals.
4.2.5. Readiness Differences between Public and Private Hospitals in Greece
The healthcare landscape in Greece comprises both public and private institutions, with each playing a critical role in the healthcare system. Understanding the differences in readiness between these hospitals, particularly regarding the implementation of quality assurance and improvement processes, is essential for policymakers and healthcare administrators. The findings in this section (Chart 5) are based on qualitative responses from various stakeholders, highlighting the perceived differences and similarities between public and private hospitals.
- Perceived Similarities in Readiness
A minority of respondents believed that there were no significant differences in readiness between public and private hospitals. They emphasized that public hospitals have increasingly adopted management practices and certifications similar to private institutions. Key insights from respondents include the following:
Adoption of Management Practices: “Management and certifications have also been introduced in public hospitals,” said one respondent, suggesting that standardization is bridging the gap.
Implementation of Quality Assurance: Respondents noted that all hospitals, regardless of type, implement the necessary quality assurance processes, although public hospitals often face challenges due to outdated equipment.
This perspective highlights that, while public hospitals are catching up in terms of processes, their technological resources may still be lacking.
- 2.
- Perceived Differences in Readiness
The majority of respondents reported significant differences between public and private hospitals, with private hospitals perceived as more prepared. The key factors contributing to this difference were as follows:
Reputation and Resource Management: Private hospitals were seen to prioritize their reputation and resource management, driving continuous improvement. One respondent noted, “Private hospitals prioritize their reputation and resource management, unlike public hospitals.”
Resource Availability: Several respondents highlighted that private hospitals have more resources at their disposal, enabling greater flexibility and responsiveness to changes. For instance, respondents observed that private hospitals have better access to newer technologies and skilled staff.
Bureaucracy and Flexibility: Public hospitals face bureaucratic hurdles, making it harder for them to adapt quickly. “Private hospitals are more equipped to adopt methodologies quickly, while public hospitals are slowed by bureaucracy,” noted one respondent.
- 3.
- Role of Staff and Management
Differences in staff demographics and management structures further contribute to the perceived readiness gap:
Younger, More Adaptable Staff: Private hospitals tend to employ younger staff who are more open to adopting new practices and technologies, and this contributes to higher readiness levels.
Flexible Management Structures: Respondents highlighted that private hospitals’ reliance on private decision-making processes, as opposed to the state-dependent processes employed in public hospitals, allows for quicker decision-making and better resource allocation.
- 4.
- Counterexamples: Public Sector Potential
Despite the consensus favoring private hospitals, some respondents acknowledged exceptions in the public sector. Pioneering public hospitals that focus on specific departments (e.g., emergency, oncology) and implement methodologies like Lean Six Sigma (LSS) were cited as examples of successful quality improvement.
Chart 6 compares the readiness of Greek public vs. private hospitals for GLSS implementation. The chart segments the responses into groups such as “High Readiness”, “Potential but Challenges”, “Low Readiness”, and “Very Low Readiness”. It clearly shows that private hospitals have higher perceived readiness, while public hospitals face more challenges with regard to readiness levels.
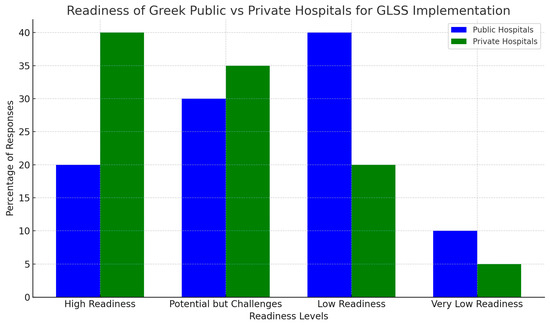
Chart 6.
Readiness Levels of Greek Public vs. Private Hospitals for GLSS Implementation. This chart was created by the authors of the article.
In summary, the findings indicate clear differences in readiness between public and private hospitals in Greece. Private hospitals are generally better equipped and more agile, thanks to their superior resource management and flexibility. However, public hospitals, especially those pioneering quality improvement initiatives, show that they too can achieve high levels of readiness with the right strategies and investments.
4.2.6. Recommendations for Developing and Implementing GLSS Principles in Healthcare Processes
The adoption of GLSS principles in healthcare processes has the potential to greatly enhance the quality and efficiency of hospital operations. This section presents recommendations for the successful development and implementation of GLSS methodologies in hospitals, based on insights gathered from participants in a qualitative survey. These participants, who were selected from various levels of healthcare organizations, provided valuable perspectives on critical areas such as management support, stakeholder engagement, and continuous improvement.
- Senior Management Support:
- One of factors most frequently cited by survey participants for the successful implementation of GLSS was strong support from senior management. Participants emphasized that effective leadership is crucial for creating the vision and providing the necessary resources for GLSS initiatives. Specific recommendations were as follows:
- Strategic Endorsement: Participants stressed the importance of senior management actively endorsing GLSS principles. They highlighted that a clear and visible commitment from leadership, integrated into the hospital’s strategic goals, is essential for driving GLSS adoption.
- Resource Provision: Several participants noted that allocating sufficient resources, including financial, technological, and human resources, is a critical enabler for GLSS projects. Without these, initiatives are likely to struggle.
- Motivation and Incentives: Participants suggested the development of incentive programs to motivate staff. They found that recognizing and rewarding contributions to GLSS initiatives fosters a culture of continuous improvement and engagement.
- Continuous Training and Education:
- Ongoing training and education emerged as a key theme in the survey responses. Participants highlighted the necessity of equipping healthcare professionals with the skills needed to implement GLSS effectively. Recommendations include:
- Stakeholder Education: Participants advocated for comprehensive training programs for all stakeholders, including clinical and administrative staff. They emphasized that understanding GLSS principles across the organization is crucial for coherent implementation.
- Knowledge Updates: Survey participants recommended that training programs be regularly updated to incorporate the latest advancements in GLSS methodologies. Keeping staff informed of new tools and practices is vital for maintaining efficiency.
- Practical Implementation: Participants also highlighted the importance of practical, hands-on training. They suggested that training be closely aligned with real-world applications, making it more relevant and impactful for staff.
- Process Improvement and Waste Reduction:
- Improving processes and reducing waste was another significant area highlighted by survey participants. Their responses offered the following strategies:
- Waste Management: Participants identified waste reduction in the supply chain as a critical area for GLSS application. They recommended techniques such as Value Stream Mapping (VSM) to identify and eliminate inefficiencies.
- Infection Control: Participants working in clinical settings emphasized the importance of using GLSS to enhance infection control practices. Standardized procedures and reduced variability are crucial, especially in high-risk areas.
- Ongoing Monitoring: Many participants stressed the need for continuous monitoring of processes to identify areas for improvement. They suggested that regular audits and performance reviews are essential for sustaining high standards.
- Engaging and Motivating Staff:
- The engagement and motivation of hospital staff were frequently mentioned as critical to the success of GLSS implementation. Based on their feedback, the following strategies are recommended:
- Staff Involvement: Participants strongly advocated for involving staff in decision-making processes. They emphasized that engaging in problem-solving fosters ownership and commitment to GLSS initiatives.
- Cultural Change: The need for cultural change was another recurring theme in the responses. Participants suggested fostering a culture of continuous improvement where innovation is encouraged and change is welcomed. Success stories should be shared to reinforce this culture.
- Feedback Mechanisms: Survey participants recommended establishing robust feedback channels. These mechanisms allow staff to voice concerns and suggest improvements, enhancing morale and refining GLSS practices.
- Overcoming Legislative and Organizational Barriers:
- Participants also identified various legislative and organizational barriers to GLSS implementation. Their responses led to the following recommendations:
- Navigating Legislation: Participants highlighted the need for healthcare organizations to work within existing regulations while advocating for policy changes that support GLSS principles. Collaboration with regulatory bodies was seen as a key strategy.
- Identifying Challenges: Survey responses emphasized the importance of proactively identifying organizational barriers. Participants suggested conducting surveys and interviews to uncover potential challenges and develop strategies to address them.
- Cost Management: Although the initial cost of GLSS was a concern for some participants, they recommended careful financial planning and focusing on long-term sustainability to ensure that GLSS initiatives are financially viable.
- Practical Implementation and Project Management:
- Treating the implementation of GLSS as a structured project was another key recommendation that emerged from the survey responses. Participants provided the following insights:
- Project Management: Participants underscored the importance of applying project management principles to GLSS initiatives. They suggested setting clear objectives, timelines, and milestones to ensure that projects are well planned and executed effectively.
- Role Assignment: The survey responses highlighted the need for clearly defined roles and responsibilities within GLSS projects. Having clearly defined roles is crucial for smooth execution and accountability.
- Evaluation and Adjustment: Regular evaluation of GLSS initiatives was a common recommendation. Participants stressed the importance of using feedback and performance metrics to make necessary adjustments and improvements.
In summary, the successful development and implementation of GLSS principles in healthcare settings require a multifaceted approach informed by industry insights. The qualitative survey responses underscore the importance of support from senior management, continuous training, staff engagement, and overcoming organizational barriers. By addressing these areas, hospitals can enhance operational efficiency, improve patient care, and achieve sustainable cost reductions. A collaborative effort by all stakeholders, combined with a commitment to continuous improvement, will be crucial for realizing the full benefits of GLSS methodologies in the healthcare sector.
5. Discussion
5.1. Interpretation of Findings
The findings of this study provide critical insights into healthcare workers’ perceptions of adopting Green Lean Six Sigma (GLSS) practices within healthcare institutions. This study is particularly timely given the increasing emphasis on environmental sustainability and operational efficiency in healthcare, a trend driven by growing concerns over health, environmental impacts, and resource constraints [106,107,108]. While there is a foundational awareness of Lean and Six Sigma practices among healthcare professionals, this research reveals that the integration of these methodologies with green practices under the GLSS framework remains largely unfamiliar to many in the sector. This observation aligns with previous studies that suggest healthcare has been slower to adopt GLSS practices compared to other industries like manufacturing and construction [60,109].
This study contributes to the broader literature by both affirming and challenging existing theories regarding the adoption of operational improvement methodologies in healthcare. On the one hand, the results reinforce the potential of Lean and Six Sigma methodologies to enhance efficiency, reduce waste, and improve patient care—outcomes that have been extensively documented in the literature [57,58]. However, the study also challenges the assumption that these methodologies can be easily transferred to healthcare. The unfamiliarity with GLSS observed here suggests that healthcare organizations face unique barriers to adopting such integrated practices, including a lack of clear frameworks tailored to the complexities of healthcare environments. This points to a critical gap in the literature and a need for sector-specific strategies for the implementation of GLSS in healthcare [110,111].
The challenges identified by healthcare workers in this study—such as resource limitations, training deficits, and cultural resistance—are consistent with the readiness factors (RFs) commonly discussed in the literature. Successful implementation of GLSS, as noted in prior research, requires addressing these RFs, which include organizational, cultural, and operational dimensions [27,112,113]. The findings reinforce the idea that leadership commitment, adequate resource allocation, and continuous staff engagement are essential for overcoming these barriers [45,114]. These insights are crucial in the ongoing debate on the effectiveness of Lean practices in healthcare, highlighting the importance of organizational readiness in ensuring successful outcomes [115,116,117].
One of the significant contributions of this study is the identification of a gap in empirical evidence regarding GLSS adoption in healthcare. Although GLSS frameworks have been applied and studied in other sectors, the healthcare industry lacks sufficient empirical data on their implementation. This supports Narayanamurthy and Gurumurthy (2018), who called for the development of structured assessment techniques to evaluate hospitals’ readiness for GLSS adoption [118]. Without sector-specific empirical insights, the risk of ineffective implementation increases, as organizations may struggle to adapt existing frameworks to their unique operational needs [119,120,121,122].
Moreover, this study draws attention to the role of organizational behavior (OB) and hospital organizational behavior (HOB) in facilitating or hindering the adoption of GLSS practices. While some research acknowledges the relationship between OB and Lean practices, empirical evidence in healthcare settings remains limited [123,124,125]. This study suggests that understanding the specific HOB factors that influence GLSS adoption is critical for developing targeted strategies to overcome the identified barriers. This could serve as the basis for future research aimed at creating more effective and contextually relevant frameworks for GLSS implementation in healthcare [126,127,128,129].
Additionally, it is important to emphasize that Swarnakar et al. (2021) [17] evaluated the critical failure factors associated with GLSS in healthcare, providing contemporary evidence that highlights specific barriers such as insufficient training and resistance to change. These findings resonate with the current study, reinforcing the importance of leadership commitment and the development of comprehensive training programs to support healthcare workers in adopting GLSS practices.
Similarly, Kaswan et al. (2022) [19] explore sustainable healthcare practices through an integrated GRA-Fuzzy TOPSIS application, focusing on how GLSS can help healthcare institutions improve operational efficiency and patient safety while adhering to environmental regulations. Their findings support the argument that GLSS can drive sustainable health practices, particularly in waste reduction and resource efficiency. This highlights the evolving role of GLSS in aligning healthcare operations with sustainability mandates, which is especially crucial in the post-COVID era of healthcare reform [13].
In addition, as healthcare systems adopt more and more sustainability goals, the integration of GLSS into operational frameworks becomes more relevant. Haleem et al. (2022) [13] emphasize the role of Industry 4.0 and its intersection with healthcare sustainability initiatives, noting that the incorporation of technology and sustainability is a key aspect of healthcare reform. GLSS practices can help healthcare institutions align with these goals by promoting continuous improvement strategies that enhance patient outcomes while also reducing environmental footprints. This connection between GLSS and sustainability further emphasizes the importance of adopting such practices in modern healthcare institutions.
In this context, Graban (2018) [18] highlights updated methodologies on Lean thinking in hospitals, demonstrating how continuous improvement strategies can align with sustainability goals to optimize healthcare delivery. The integration of GLSS practices not only improves operational efficiency but also contributes to broader sustainability goals, such as reducing carbon footprints and promoting eco-friendly healthcare practices.
Regarding the broader implications for sustainable healthcare practices, the implications of this study extend beyond the operational improvements associated with GLSS. As more healthcare systems adopt Industry 4.0 technologies, the need for efficient, patient-centered, and sustainable practices becomes even more pressing. GLSS offers a practical framework for achieving these objectives, as demonstrated in recent studies on its impact on both operational and environmental performance. Incorporating advanced technologies into GLSS practices not only enhances operational efficiency but also supports sustainability goals by reducing resource consumption and minimizing waste [18].
This is particularly relevant in light of emerging trends in healthcare sustainability. Kaswan et al. (2022) [19] identified GLSS as a critical enabler for healthcare institutions striving to meet stringent environmental regulations while maintaining operational efficiency. Their research supports the argument that GLSS is not only beneficial but increasingly necessary for hospitals seeking to remain competitive and sustainable in the evolving healthcare landscape. As healthcare institutions face mounting pressures to improve efficiency and reduce environmental impacts, GLSS offers a structured approach to addressing these challenges.
In conclusion, the findings of this study both confirm and extend the existing knowledge on the potential benefits of GLSS in healthcare. While there is growing recognition of its advantages, significant barriers—particularly in relation to organizational readiness and the integration of green practices—persist. The study emphasizes the need for further research to develop tailored frameworks that address the unique challenges of healthcare institutions. By doing so, healthcare organizations will be better positioned to adopt GLSS practices effectively, leading to improved sustainability and efficiency in healthcare delivery.
5.2. Practical Recommendations
Based on the study’s findings, several practical recommendations can be made for healthcare administrators considering the implementation of GLSS in their organizations:
- Leadership Commitment and Vision: To overcome cultural resistance and ensure sustained engagement, healthcare leaders must demonstrate a strong commitment to new initiatives [70,71] This includes communicating the vision and benefits of GLSS to all staff members, ensuring that they understand the value of these practices not only in terms of efficiency and cost savings but also in improving patient care and contributing to environmental sustainability.
- Comprehensive Training Programs: Given concerns about resource constraints and the need for specialized knowledge, healthcare organizations should invest in comprehensive training programs that equip staff with the necessary skills to implement new practices effectively [72,73]. Training should not only cover the technical aspects of Lean and green practices but should also emphasize their importance in achieving broader organizational goals, such as sustainability and patient-centered care.
- Continuous Engagement and Feedback: To foster a culture of continuous improvement, it is important to maintain ongoing engagement with staff throughout the implementation process [59,74]. This can be achieved through regular feedback sessions, workshops, and team meetings where employees can share their experiences, challenges, and suggestions for improvement. Continuous engagement helps build a sense of ownership among staff, making them more likely to support the success of GLSS initiatives.
- Resource Allocation and Support: Addressing concerns about resource constraints requires careful planning and resource allocation. This includes not only financial investment in training and infrastructure but also providing sufficient time and support for staff to adapt to new practices [75,76]. Phased implementations, in which GLSS practices are introduced gradually, allow staff to adjust and provide opportunities for continuous learning and process refinement.
To mitigate resource constraints, hospitals could explore partnerships with government programs or non-governmental organizations to secure funding for training and equipment upgrades. Leadership plays a crucial role in reducing cultural resistance by fostering a culture of continuous improvement. Clear communication about the long-term benefits of GLSS, along with involving staff in decision-making processes, can help alleviate fears of disruption and encourage broader adoption of these practices. By maintaining an open dialogue and emphasizing the positive outcomes of GLSS, healthcare organizations can further reduce resistance and facilitate the successful integration of these methodologies.
All in all, the findings of this study contribute to the ongoing discourse on the adoption of operational improvement methodologies in healthcare by highlighting the potential of GLSS to drive both operational and environmental sustainability. While healthcare organizations recognize the advantages of GLSS, significant barriers remain, particularly regarding organizational readiness and the integration of green practices. Future research should focus on developing tailored frameworks that address the unique challenges of healthcare institutions, enabling them to adopt GLSS practices effectively. By doing so, healthcare organizations will be better positioned to improve sustainability and efficiency in healthcare delivery.
6. Conclusions
6.1. Summary of Key Findings and Their Significance
This study explored healthcare professionals’ and academics’ perspectives on adopting GLSS practices in healthcare, focusing on their awareness, perceived benefits, and the challenges associated with its implementation. While there is general awareness of Lean practices, integrating these practices with green technologies remains relatively unfamiliar within the sector. Nevertheless, participants recognized the significant potential of GLSS in improving operational efficiency, reducing waste, and enhancing patient care. These benefits align with the existing literature, which supports the positive impact of Lean methodologies on healthcare delivery, with the added advantage of green practices promoting sustainability.
Despite the recognized benefits, this study also identified several barriers to the successful adoption of GLSS in healthcare institutions. Key challenges include resource constraints, such as limited time, financial investment, and the need for comprehensive staff training. Healthcare professionals noted that comprehensive training programs in both leadership and technical GLSS methodologies are essential for overcoming the readiness gap. By equipping staff with the necessary skills, hospitals can enhance their capacity to adopt GLSS successfully. Additionally, cultural resistance to change and the critical need for strong leadership commitment were highlighted as major factors that influence the success of GLSS initiatives.
The insights gained emphasize that successful GLSS implementation requires a holistic approach that combines top management involvement, an adaptive organizational culture, and continuous staff education. Addressing these factors not only fosters a supportive environment for GLSS adoption but also helps healthcare institutions contribute to broader sustainability goals, aligning with initiatives like the United Nations’ Sustainable Development Goals (SDGs).
By providing a nuanced understanding of both the opportunities and challenges of integrating GLSS, this study offers valuable guidance for healthcare administrators and policymakers. Future research should focus on expanding empirical evidence of GLSS implementation, particularly with regard to assessing its long-term impact on healthcare outcomes, and exploring how it can be applied to other pressing sustainability issues such as energy management and carbon reduction in healthcare settings.
6.2. Limitations and Future Research
This study provides valuable insights into healthcare workers’ perceptions of GLSS adoption, highlighting both its potential benefits and the significant challenges to its successful implementation. While the findings shed light on the opportunities for improved efficiency, waste reduction, and enhanced patient care, several limitations must be acknowledged. The relatively small sample size and limited geographic focus may restrict the generalizability of the results. Additionally, the study primarily captures initial perceptions, lacking a detailed exploration of the long-term impact of GLSS on healthcare outcomes and sustainability.
Future research should build on these initial findings by conducting larger, more comprehensive studies that include a broader range of healthcare institutions and diverse geographical contexts. Longitudinal studies will be particularly important for assessing the sustained effects of GLSS on healthcare performance, patient outcomes, and environmental sustainability. In addition to examining the broader impact of GLSS, future studies should explore critical sustainability issues such as energy consumption, waste management, and carbon reduction in healthcare settings.
Moreover, a key avenue for future research lies in developing and refining tailored GLSS frameworks that cater to the specific needs of different healthcare organizations, from small clinics to large hospitals. Investigating the influence of organizational culture, leadership styles, and resource availability in various healthcare environments will be essential for creating adaptable, effective GLSS models. While the upfront costs of implementing GLSS are a significant barrier, particularly in resource-constrained settings, the long-term savings from reduced waste and optimized processes can offset initial investments. Hospitals should focus on demonstrating these long-term benefits to secure necessary financial support. By advancing research in these areas, GLSS can be better positioned to contribute to the development of more sustainable, efficient, and resilient healthcare systems.
Another key limitation of this study is its focus on the Greek health system, which may not fully capture the variability of outcomes associated with GLSS in different international contexts. Our findings, which suggest that private hospitals in Greece benefit from GLSS, may not hold in other countries with differing healthcare system structures. Health systems vary widely in terms of regulations, funding mechanisms, and institutional frameworks, which can significantly influence the effectiveness and impact of policies like GLSS. Consequently, the generalizability of our conclusions to other countries should be approached with caution. Future research should aim to examine GLSS in diverse health systems to better understand its broader applicability and identify potential variations in its impact across different national contexts.
6.3. Call to Action for Further Exploration and Adoption of GLSS in Healthcare Settings
Given the potential benefits and challenges identified in this study, further exploration and adoption of GLSS in clinical settings are both necessary and timely. Healthcare administrators and policymakers are encouraged to consider these findings and take proactive steps toward integrating GLSS into their organizational practices. Although GLSS offers significant potential for improving efficiency and sustainability in healthcare, its success depends on overcoming key challenges such as the high training demands and the financial costs of implementation. Addressing these barriers will be critical for the broader adoption of GLSS methodologies.
Moreover, to facilitate the adoption of GLSS, healthcare organizations should prioritize leadership commitment, invest in comprehensive training programs, and engage staff throughout the implementation process. When the challenges highlighted in this study are addressed, the likelihood of successful GLSS adoption increases, leading to more efficient, sustainable, and high-quality healthcare services.
In conclusion, the adoption of GLSS presents a promising opportunity for the healthcare industry to address the dual challenges of improving efficiency and enhancing sustainability. The insights gained from this study provide a foundation for future research and practical applications, paving the way for a more sustainable and effective healthcare system. Healthcare leaders are urged to take action by exploring and implementing GLSS practices to ensure their organizations are well-prepared to meet future demands.
Author Contributions
Conceptualization, E.S. and A.V.; methodology, A.V.; software, A.V.; validation, E.S. and G.T.; formal analysis, A.V.; investigation, A.V. and E.S.; resources, A.V. and E.S.; data curation, A.V. and E.S.; writing—original draft preparation, A.V.; writing—review and editing, A.V. and E.S.; visualization, G.T.; supervision, E.S.; project administration, A.V.; funding acquisition, G.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Kovacevic, M.; Jovicic, M.; Djapan, M.; Zivanovic-Macuzic, I. Lean thinking in healthcare: Review of implementation results. Int. J. Qual. Res. 2016, 10, 219. [Google Scholar]
- Tsekouropoulos, G.; Gkouna, O.; Theocharis, D.; Gounas, A. Innovative sustainable tourism development and entrepreneurship through sports events. Sustainability 2022, 14, 4379. [Google Scholar] [CrossRef]
- Antony, J.; Sunder, M.V.; Sreedharan, R.; Chakraborty, A.; Gunasekaran, A. A systematic review of Lean in healthcare: A global prospective. Int. J. Qual. Reliab. Manag. 2019, 36, 1370–1391. [Google Scholar] [CrossRef]
- Daultani, Y.; Chaudhuri, A.; Kumar, S. A decade of lean in healthcare Current state and future directions. Glob. Bus. Rev. 2015, 16, 1082–1099. [Google Scholar] [CrossRef]
- Lima, R.M.; Azevedo, V.; Costa, M.F.; Soares, A.L. Implementation of lean in health care environments: An update of systematic reviews. Int. J. Lean Six Sigma 2021, 12, 399–431. [Google Scholar] [CrossRef]
- Nnamuchi, O. The Sustainable Development Goals (SDGS) and the Right to Health Is There a Nexus? Fla. J. Int. Law 2020, 32, 147. [Google Scholar]
- United Nations. Transforming Our World. The 2030 Agenda for Sustainable Development; United Nations, Department of Economic and Social Affairs: New York, NY, USA, 2015; pp. 1–41. [Google Scholar]
- World Health Organization. A Vision for Primary Health Care in the 21st Century Towards Universal Health Coverage and the Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Dyakova, M.; Hamelmann, C.; Bellis, M.A.; Grey, C.N.; Ashton, K.; Schwappach, A.; Christine, C. Investment for Health and Well-Being: A Review of the Social Return on Investment from Public Health Policies to Support Implementing the Sustainable Development Goals by Building on Health 2020; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- World Health Organization, Small Countries Initiative. Building Resilience: A Key Pillar of Health 2020 and the Sustainable Development Goals Examples from the WHO Small Countries Initiative; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V.; et al. High-quality health systems in the Sustainable Development Goals era Time for a revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef]
- Barron, G.C.; Laryea-Adjei, G.; Vike-Freiberga, V.; Abubakar, I.; Dakkak, H.; Devakumar, D.; Johnsson, A.; Karabey, S.; Labonté, R.; Legido-Quigley, H.; et al. Safeguarding people living in vulnerable conditions in the COVID-19 era through universal health coverage and social protection. Lancet Public Health 2022, 7, e86–e92. [Google Scholar] [CrossRef]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R. Medical 4.0 technologies for healthcare: Features, capabilities, and applications. Internet Things Cyber Phys. Syst. 2022, 2, 12–30. [Google Scholar] [CrossRef]
- Yaqub, M.Z.; Alsabban, A. Industry-4.0-Enabled digital transformation: Prospects, instruments, challenges, and implications for business strategies. Sustainability 2023, 15, 8553. [Google Scholar] [CrossRef]
- National Academies of Sciences; Medicine Division; Board on Global Health; Committee on Improving the Quality of Health Care Globally. Crossing the Global Quality Chasm Improving Health Care Worldwide; National Academies Press: Washington, DC, USA, 2018. [Google Scholar]
- Duek, I.; Fliss, D.M. The COVID-19 pandemic-from great challenge to unique opportunity: Perspective. Ann. Med. Surg. 2020, 59, 68–71. [Google Scholar] [CrossRef] [PubMed]
- Swarnakar, V.; Singh, A.R.; Tiwari, A.K. Evaluating the effect of critical failure factors associated with sustainable Lean Six-sigma framework implementation in healthcare organization. Int. J. Qual. Reliab. Manag. 2021, 38, 1149–1477. [Google Scholar] [CrossRef]
- Graban, M. Lean hospitals Improving Quality, Patient Safety, and Employee Engagement; Productivity Press: New York, NY, USA, 2018. [Google Scholar]
- Kaswan, M.S.; Rathi, R.; Singh, M.; Garza-Reyes, J.A.; Antony, J. Exploration and prioritization of just in time enablers for sustainable health care: An integrated GRA-Fuzzy TOPSIS application. World J. Eng. 2022, 19, 402–417. [Google Scholar] [CrossRef]
- Beynaghi, A.; Moztarzadeh, F.; Mobini-Dehkordi, M.; Maknoon, R.; Waasmaier, S.; Leal Filho, W. Future sustainability scenarios for universities: Moving beyond the United Nations Decade of Education for Sustainable Development. J. Clean. Prod. 2016, 112, 3464–3478. [Google Scholar] [CrossRef]
- Afeltra, G.; Alerasoul, S.A.; Strozzi, F. The evolution of sustainable innovation: From the past to the future. Eur. J. Innov. Manag. 2023, 26, 386–421. [Google Scholar] [CrossRef]
- Voegtlin, C.; Scherer, A.G. Responsible innovation and the innovation of responsibility Governing sustainable development in a globalized world. J. Bus. Ethics 2017, 143, 227–243. [Google Scholar] [CrossRef]
- Chugani, N.; Kumar, V.; Garza-Reyes, J.A.; Rocha-Lona, L.; Upadhyay, A. Investigating the green impact of Lean, Six Sigma and Lean Six Sigma A systematic literature review. Int. J. Lean Six Sigma 2017, 8, 7–32. [Google Scholar] [CrossRef]
- Qadri, Y.A.; Naeem, M.; Al-Turjman, F.; Al-Fuqaha, A.; Guizani, M. The future of healthcare internet of things A survey of emerging technologies. IEEE Commun. Surv. Tutor 2020, 22, 1121–1167. [Google Scholar] [CrossRef]
- Kasemsap, K. Applying Lean Production and Six Sigma in Global Operations. In Operations and Service Management: Concepts, Methodologies, Tools, and Applications; IGI Global: Hershey, PA, USA, 2018; pp. 582–612. [Google Scholar]
- Simeli, I.; Tsekouropoulos, G.; Vasileiou, A.; Hoxha, G. Benefits and Challenges of Teleworking for a Sustainable Future Knowledge Gained through Experience in the Era of COVID-19. Sustainability 2023, 15, 11794. [Google Scholar] [CrossRef]
- Al-Balushi, S.; Sohal, A.S.; Singh, P.J.; Al Hajri, A.; Al Farsi, Y.M.; AlAbri, R. Readiness factors for lean implementation in healthcare settings–a literature review. J. Health Organ. Manag. 2014, 28, 135–153. [Google Scholar] [CrossRef]
- Saini, M. A Framework for Transferring and Sharing Tacit Knowledge in Construction Supply Chains within Lean and Agile Processes. Ph.D. Thesis, University of Salford, Salford, UK, 2015. [Google Scholar]
- Raja Sreedharan, V.; Raju, R. A systematic literature review of Lean Six Sigma in different industries. Int. J. Lean Six Sigma 2016, 7, 430–466. [Google Scholar] [CrossRef]
- Iqbal, T.; Huq, F.; Bhutta, M.K. Agile manufacturing relationship building with TQM, JIT, and firm performance: An exploratory study in apparel export industry of Pakistan. Int. J. Prod. Econ. 2018, 203, 24–37. [Google Scholar] [CrossRef]
- Khan, S.A.; Kaviani, M.A.; Galli, J.B.; Ishtiaq, P. Application of continuous improvement techniques to improve organization performance: A case study. Int. J. Lean Six Sigma 2019, 10, 542–565. [Google Scholar] [CrossRef]
- Wickramasinghe, N.; Al-Hakim, L.; Gonzalez, C.; Tan, J. (Eds.) Lean Thinking for Healthcare; Springer: New York, NY, USA, 2014. [Google Scholar]
- Kakouris, A.; Sfakianaki, E.; Tsioufis, M. Lean thinking in lean times for education. Ann. Oper. Res. 2022, 316, 657–697. [Google Scholar] [CrossRef]
- Tsekouropoulos, G.; Vasileiou, A.; Hoxha, G.; Dimitriadis, A.; Zervas, I. Sustainable Approaches to Medical Tourism: Strategies for Central Macedonia/Greece. Sustainability 2023, 16, 121. [Google Scholar] [CrossRef]
- Hines, P.; Holweg, M.; Rich, N. Learning to evolve A review of contemporary lean thinking. Int. J. Oper. Prod. Manag. 2004, 24, 994–1011. [Google Scholar] [CrossRef]
- Stanton, P.; Gough, R.; Ballardie, R.; Bartram, T.; Bamber, G.J.; Sohal, A. Implementing lean management/Six Sigma in hospitals Beyond empowerment or work intensification? Int. J. Hum. Resour. Manag. 2014, 25, 2926–2940. [Google Scholar] [CrossRef]
- Alshurideh, M.; Gasaymeh, A.; Ahmed, G.; Alzoubi, H.; Kurd, B. Loyalty program effectiveness Theoretical reviews and practical proofs. Uncertain Supply Chain Manag. 2020, 8, 599–612. [Google Scholar] [CrossRef]
- Sohal, A.; De Vass, T.; Vasquez, T.; Bamber, G.J.; Bartram, T.; Stanton, P. Success factors for lean six sigma projects in healthcare. J. Manag. Control. 2022, 33, 215–240. [Google Scholar] [CrossRef]
- Henrique, D.B.; Filho, M.G.; Marodin, G.; Jabbour, A.B.; Chiappetta Jabbour, C.J. A framework to assess sustaining continuous improvement in lean healthcare. Int. J. Prod. Res. 2021, 59, 2885–2904. [Google Scholar] [CrossRef]
- Bell, S.C.; Orzen, M.A. Lean IT Enabling and Sustaining Your Lean Transformation; CRC Press: Boca Raton, FL, USA, 2016. [Google Scholar]
- Teeling, S.P.; Dewing, J.; Baldie, D. A discussion of the synergy and divergence between Lean Six Sigma and person-centred improvement sciences. Int. J. Res. Nurs. 2020, 11, 10–23. [Google Scholar] [CrossRef]
- Valamede, L.S.; Akkari, A.C.S. Lean 4.0: A new holistic approach for the integration of lean manufacturing tools and digital technologies. Int. J. Math. Eng. Manag. Sci. 2020, 5, 851. [Google Scholar] [CrossRef]
- Ahmed, A.; Page, J.; Olsen, J. Enhancing Six Sigma methodology using simulation techniques: Literature review and implications for future research. Int. J. Lean Six Sigma 2020, 14, 211–232. [Google Scholar] [CrossRef]
- Yahya, S.; Khan, A.; Farooq, M.; Irfan, M. Integrating green business strategies and green competencies to enhance green innovation Evidence from manufacturing firms of Pakistan. Environ. Sci. Pollut. Res. 2022, 29, 39500–39514. [Google Scholar] [CrossRef]
- D’Andreamatteo, A.; Ianni, L.; Lega, F.; Sargiacomo, M. Lean in healthcare: A comprehensive review. Health Policy 2015, 119, 1197–1209. [Google Scholar] [CrossRef]
- Parmar, P.S.; Desai, T.N. A systematic literature review on Sustainable Lean Six Sigma: Current status and future research directions. Int. J. Lean Six Sigma 2020, 11, 429–461. [Google Scholar] [CrossRef]
- Van Rossum, L.; Aij, K.H.; Simons, F.E.; Van Der Eng, N.; Ten Have, W. Lean healthcare from a change management perspective the role of leadership and workforce flexibility in an operating theatre. J. Health Organ. Manag. 2016, 30, 475–493. [Google Scholar] [CrossRef]
- Farrukh, A.; Mathrani, S.; Taskin, N. Investigating the theoretical constructs of a green lean six sigma approach towards environmental sustainability A systematic literature review and future directions. Sustainability 2020, 12, 8247. [Google Scholar] [CrossRef]
- Ruben, R.B.; Vinodh, S.; Asokan, P. Lean Six Sigma with environmental focus: Review and framework. Int. J. Adv. Manuf. Technol. 2018, 94, 4023–4037. [Google Scholar] [CrossRef]
- Costa, L.B.M.; Godinho Filho, M.; Fredendall, L.D.; Ganga, G.M.D. Lean six-sigma in the food industry: Construct development and measurement validation. Int. J. Prod. Econ. 2021, 231, 107843. [Google Scholar] [CrossRef]
- Adeodu, A.; Kanakana-Katumba, M.G.; Maladzhi, R. Implementation of Lean Six Sigma for production process optimization in a paper production company. J. Ind. Eng. Manag. 2021, 14, 661–680. [Google Scholar] [CrossRef]
- Jones, E. Quality Management for Organizations Using Lean Six Sigma Techniques; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Singh, A.; Ravi, P. Lean six-sigma (LSS) applications in hospitals A decade (2011–2020) bibliometric analysis. Int. J. Prod. Perform. Manag. 2023, 72, 2270–2291. [Google Scholar] [CrossRef]
- Belhadi, A.; Kamble, S.S.; Zkik, K.; Cherrafi, A.; Touriki, F.E. The integrated effect of big data analytics, lean six-sigma and green manufacturing on the environmental performance of manufacturing companies: The case of North Africa. J. Clean. Prod. 2020, 252, 119903. [Google Scholar] [CrossRef]
- Tasdemir, C.; Gazo, R. A systematic literature review for better understanding of lean driven sustainability. Sustainability 2018, 10, 2544. [Google Scholar] [CrossRef]
- De, D.; Chowdhury, S.; Dey, P.K.; Ghosh, S.K.; Ghosh, S.K. Impact of lean and sustainability oriented innovation on sustainability performance of small and medium sized enterprises: A data envelopment analysis-based framework. Int. J. Prod. Econ. 2020, 219, 416–430. [Google Scholar] [CrossRef]
- Ghaithan, A.M.; Alshammakhi, Y.; Mohammed, A.; Mazher, K.M. Integrated impact of circular economy, industry 4.0, and lean manufacturing on sustainability performance of manufacturing firms. Int. J. Environ. Res. Public Health 2023, 20, 5119. [Google Scholar] [CrossRef]
- Sony, M.; Naik, S. Green lean six-sigma implementation framework: A case of reducing graphite and dust pollution. Int. J. Sustain. Eng. 2019, 13, 184–193. [Google Scholar] [CrossRef]
- Gholami, H.; Jamil, N.; Mat Saman, M.Z.; Streimikiene, D.; Sharif, S.; Zakuan, N. The application of green lean six sigma. Bus. Strategy Environ. 2021, 30, 1913–1931. [Google Scholar] [CrossRef]
- Rathi, R.; Kaswan, M.S.; Garza-Reyes, J.A.; Antony, J.; Cross, J. Green lean six-sigma for improving manufacturing sustainability: Framework development and validation. J. Clean. Prod. 2022, 345, 131130. [Google Scholar] [CrossRef]
- Zhu, Q.; Johnson, S.; Sarkis, J. Lean six sigma and environmental sustainability: A hospital perspective. Supply Chain Forum Int. J. 2018, 19, 25–41. [Google Scholar] [CrossRef]
- Thomas, A.; Antony, J.; Francis, M.; Fisher, R. Green operation strategies in healthcare for enhanced quality of life. Healthcare 2022, 11, 37. [Google Scholar] [CrossRef] [PubMed]
- Kaswan, M.S.; Rathi, R. Green Lean Six-sigma for sustainable development. Integr. Framew. Environ. 2020, 83, 106396. [Google Scholar]
- Hoxha, G.; Simeli, I.; Theocharis, D.; Vasileiou, A.; Tsekouropoulos, G. Sustainable Healthcare Quality and Job Satisfaction through Organizational Culture: Approaches and Outcomes. Sustainability 2024, 16, 3603. [Google Scholar] [CrossRef]
- Shokri, A.; Li, G. Green implementation of Lean Six Sigma projects in the manufacturing sector. Int. J. Lean Six Sigma 2020, 11, 711–729. [Google Scholar] [CrossRef]
- Kaswan, M.S.; Rathi, R. An inclusive review of Green Lean Six Sigma for sustainable development: Readiness measures and challenges. Int. J. Adv. Oper. Manag. 2021, 13, 129–166. [Google Scholar] [CrossRef]
- Hussain, K.; Haq, A.N.; Kannan, S. Green, lean, six sigma barriers at a glance: A case from the construction sector of Pakistan. Build. Environ. 2019, 161, 106225. [Google Scholar] [CrossRef]
- Saceleanu, V.M.; Padureanu, V.; Baleanu, V.D.; Ungureanu, B.S.; Balasa, R. Integrative approaches in acute ischemic stroke: From symptom recognition to future innovations. Biomedicines 2023, 11, 2617. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A.; Singh, R.P.; Suman, R. Industry 4.0 and circular economy for bolstering healthcare sector: A comprehensive view on challenges, implementation, and futuristic aspects. Biomed. Anal. 2024, 1, 174–198. [Google Scholar] [CrossRef]
- Leite, H. The role of lean in healthcare during COVID-19 pandemic. Int. J. Qual. Reliab. Manag. 2023, 40, 1389–1411. [Google Scholar] [CrossRef]
- Kumar, P. Green service production in healthcare and role of value chain flexibility. Int. J. Product. Perform. Manag. 2020, 69, 1721–1742. [Google Scholar] [CrossRef]
- Morell-Santandreu, O.; Santandreu-Mascarell, C.; Garcia-Sabater, J.J. A model for the implementation of lean improvements in healthcare environments as applied in a primary care center. Int. J. Environ. Res. Public Health 2021, 18, 2876. [Google Scholar] [CrossRef] [PubMed]
- Farrukh, A.; Mathrani, S.; Sajjad, A. Managerial perspectives on green-lean-six sigma adoption in the flexible packaging industry Empirical evidence from an emerging economy. J. Manuf. Technol. Manag. 2022, 33, 1232–1255. [Google Scholar] [CrossRef]
- Yadav, V.; Singh, A.R.; Jain, R.; Rathore, A.P. Green Lean Six Sigma for sustainability improvement: A systematic review and future research agenda. Int. J. Lean Six Sigma 2023, 14, 759–790. [Google Scholar] [CrossRef]
- Patel, A.S.; Patel, K.M. Critical review of literature on Lean Six Sigma methodology. Int. J. Lean Six Sigma 2021, 12, 627–674. [Google Scholar] [CrossRef]
- Allum, P. Investigating Opportunities for Sustainability Behaviours Within Paramedic and Ambulance Service Practice. Ph.D. Thesis, University of Plymouth, Plymouth, UK, 2023. [Google Scholar]
- Sfakianaki, E.; Kaiseroglou, N.; Kakouris, A. An instrument for studying TQM implementation in primary education: Development and empirical investigation. Qual. Assur. Educ. 2023, 31, 452–468. [Google Scholar] [CrossRef]
- Pandey, H.; Garg, D.; Luthra, S. Identification and ranking of enablers of green lean Six Sigma implementation using AHP. Int. J. Product. Qual. Manag. 2018, 23, 187–217. [Google Scholar] [CrossRef]
- Garza-Reyes, J.A. Green lean and the need for Six Sigma. Int. J. Lean Six Sigma 2015, 6, 226–248. [Google Scholar] [CrossRef]
- Filip, R.; GheorghitaPuscaselu, R.; Anchidin-Norocel, L.; Dimian, M.; Savage, W.K. Global challenges to public health care systems during the COVID-19 pandemic: A review of pandemic measures and problems. J. Pers. Med. 2022, 12, 1295. [Google Scholar] [CrossRef]
- Lee, S.M.; Lee, D. Opportunities and challenges for contactless healthcare services in the post-COVID-19 Era. Technol. Forecast. Soc. Chang. 2021, 167, 120712. [Google Scholar] [CrossRef]
- Tortorella, G.L.; Fogliatto, F.S.; Mac Cawley Vergara, A.; Vassolo, R.; Sawhney, R. Healthcare 4.0 Trends, challenges and research directions. Prod. Plan. Control 2020, 31, 1245–1260. [Google Scholar] [CrossRef]
- Sors, T.G.; O’Brien, R.C.; Scanlon, M.L.; Bermel, L.Y.; Chikowe, I.; Gardner, A.; Kiplagat, J.; Lieberman, M.; Moe, S.M.; Morales-Soto, N.; et al. Reciprocal innovation: A new approach to equitable and mutually beneficial global health partnerships. Glob. Public Health 2023, 18, 2102202. [Google Scholar] [CrossRef]
- Tracy, S.J. Qualitative Research Methods: Collecting Evidence, Crafting Analysis, Communicating Impact; John Wiley & Sons: Hoboken, NJ, USA, 2019. [Google Scholar]
- Creswell, J.W.; Poth, C.N. Qualitative Inquiry and Research Design: Choosing Among Five Approaches; Sage Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- Adeoye-Olatunde, O.A.; Olenik, N.L. Research and scholarly methods: Semi-structured interviews. J. Am. Coll. Clin. Pharm. 2021, 4, 1358–1367. [Google Scholar] [CrossRef]
- Kallio, H.; Pietilä, A.M.; Johnson, M.; Kangasniemi, M. Systematic methodological review: Developing a framework for a qualitative semi-structured interview guide. J. Adv. Nurs. 2016, 72, 2954–2965. [Google Scholar] [CrossRef]
- Kvale, S. Interviews: Learning the Craft of Qualitative Research Interviewing; Sage Publications: Thousand Oaks, CA, USA, 2009. [Google Scholar]
- Casillas, A.; Cemballi, A.G.; Abhat, A.; Lemberg, M.; Portz, J.D.; Sadasivaiah, S.; Ratanawongsa, N.; Semere, W.; Brown, A.; Lyles, C.R. An untapped potential in primary care: Semi-structured interviews with clinicians on how patient portals will work for caregivers in the safety net. J. Med. Internet Res. 2020, 22, e18466. [Google Scholar] [CrossRef]
- Suri, H. Purposeful sampling in qualitative research synthesis. Qual. Res. J. 2011, 11, 63–75. [Google Scholar] [CrossRef]
- Campbell, S.; Greenwood, M.; Prior, S.; Shearer, T.; Walkem, K.; Young, S.; Bywaters, D.; Walker, K. Purposive sampling: Complex or simple? Research case examples. J. Res. Nurs. 2020, 25, 652–661. [Google Scholar] [CrossRef]
- Brennen, B.S. Qualitative Research Methods for Media Studies; Routledge: New York, NY, USA, 2021. [Google Scholar]
- Levitt, H.M. Qualitative generalization, not to the population but to the phenomenon: Reconceptualizing variation in qualitative research. Qual. Psychol. 2021, 8, 95. [Google Scholar] [CrossRef]
- Fossey, E.; Harvey, C.; McDermott, F.; Davidson, L. Understanding and evaluating qualitative research. Aust. N. Zealand J. Psychiatry 2002, 36, 717–732. [Google Scholar] [CrossRef]
- Gugiu, P.C.; Rodríguez-Campos, L. Semi-structured interview protocol for constructing logic models. Eval. Program Plan. 2007, 30, 339–350. [Google Scholar] [CrossRef]
- Brown, A.; Danaher, P.A. CHE principles: Facilitating authentic and dialogical semi-structured interviews in educational research. Int. J. Res. Method Educ. 2019, 42, 76–90. [Google Scholar] [CrossRef]
- Prior, M.T. Interviews and Focus Groups. In Palgrave Handbook of Applied Linguistics Research Methodology; Palgrave Macmillan: London, UK, 2018; pp. 225–248. [Google Scholar]
- Oumlil, R.; Faouzi, H.; Juiz, C. Uncovering two decades of open innovation benefits: A qualitative meta-analysis. Int. J. Innov. Technol. Manag. 2020, 17, 2030006. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Thematic Analysis; American Psychological Association: Washington, DC, USA, 2012. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Jones, J.; Turunen, H.; Snelgrove, S. Theme development in qualitative content analysis and thematic analysis. J. Nurs. Educ. Pract. 2016, 6, 5. [Google Scholar] [CrossRef]
- Maher, C.; Hadfield, M.; Hutchings, M.; De Eyto, A. Ensuring rigor in qualitative data analysis: A design research approach to coding combining NVivo with traditional material methods. Int. J. Qual. Methods 2018, 17, 1609406918786362. [Google Scholar] [CrossRef]
- Marathe, M.; Toyama, K. Semi-automated coding for qualitative research: A user-centered inquiry and initial prototypes. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems, Montreals, QC, Canada, 1–4 September 2018; pp. 1–12. [Google Scholar]
- Millum, J.; Bromwich, D. Informed consent: What must be disclosed and what must be understood? Am. J. Bioeth. 2021, 21, 46–58. [Google Scholar] [CrossRef] [PubMed]
- Sieber, J.E.; Tolich, M.B. Planning Ethically Responsible Research; Sage Publications: Thousand Oaks, CA, USA, 2012. [Google Scholar]
- Osorio-Gonz_alez, C.S.; Hegde, K.; Brar, S.K.; Avalos-Ramírez, A.; Surampalli, R.Y. Sustainable Healthcare Systems Sustainability: Fundamentals and Applications; John Wiley & Sons: Hoboken, NJ, USA, 2020; pp. 375–396. [Google Scholar]
- Lee, H.L.; Tang, C.S. Socially and environmentally responsible value chain innovations: New operations management research opportunities. Manag. Sci. 2018, 64, 983–996. [Google Scholar] [CrossRef]
- Gao, T.; Gurd, B. Organizational issues for the lean success in China: Exploring a change strategy for lean success. BMC Health Serv. Res. 2019, 19, 66. [Google Scholar] [CrossRef]
- Régis, T.K.; Santos, L.C.; Gohr, C.F. A case-based methodology for lean implementation in hospital operations. J. Health Organ. Manag. 2019, 33, 656–676. [Google Scholar] [CrossRef]
- Mazzocato, P.; Savage, C.; Brommels, M.; Aronsson, H.; Thor, J. Lean thinking in healthcare: A realist review of the literature. BMJ Qual. Saf. 2010, 19, 376–382. [Google Scholar] [CrossRef]
- Sfakianaki, E.; Kakouris, A. Lean thinking for education: Development and validation of an instrument. Int. J. Qual. Reliab. 2019, 36, 917–950. [Google Scholar] [CrossRef]
- Vaishnavi, V.; Suresh, M. Modelling of readiness factors for the implementation of Lean Six-sigma in healthcare organizations. Int. J. Lean Six Sigma 2020, 11, 597–633. [Google Scholar] [CrossRef]
- Dwekat, A.; Al-Tuwaijri, H.; Iqbal, N.; Khan, S.Z.; Sanni, A. Corporate governance and corporate social responsibility: Mapping the most critical drivers in the board academic literature. Meditari Account. Res. 2022, 30, 1705–1739. [Google Scholar] [CrossRef]
- Alnajem, M.; Garza-Reyes, J.A.; Antony, J. Lean readiness within emergency departments: A conceptual framework. Benchmarking Int. J. 2019, 26, 1874–1904. [Google Scholar] [CrossRef]
- Sfakianaki, E.; Matsiori, A.; Giannias, D.A.; Sevdali, I. Educational leadership and total quality management: Investigating teacher leadership styles. Int. J. Manag. Educ. 2018, 12, 375–392. [Google Scholar] [CrossRef]
- Cherrafi, A.; Elfezazi, S.; Govindan, K.; Garza-Reyes, J.A.; Benhida, K.; Mokhlis, A. A framework for the integration of Green and Lean Six Sigma for superior sustainability performance. Int. J. Prod. Res. 2017, 55, 4481–4515. [Google Scholar] [CrossRef]
- Mohan, J.; Rathi, R.; Kaswan, M.S.; Nain, S.S. Green lean six-sigma journey Conceptualization and realization. Mater. Today Proc. 2022, 50, 1991–1998. [Google Scholar] [CrossRef]
- Narayanamurthy Gurumurthy, A. Is the hospital lean? A mathematical model for assessing the implementation of lean thinking in healthcare institutions. Oper. Res. Health Care 2018, 18, 84–98. [Google Scholar] [CrossRef]
- Drotz, E.; Poksinska, B. Lean in healthcare from employees perspectives. J. Health Organ. Manag. 2018, 32, 444–460. [Google Scholar] [CrossRef] [PubMed]
- Radnor, Z.; Holweg, M.; Waring, J. Lean in healthcare: The unfilled promise? Soc. Sci. Med. 2019, 220, 60–67. [Google Scholar] [CrossRef]
- Frankel, A.S.; Leonard, M.W.; Denham, C.R. Fair and just culture, team behavior, and leadership engagement the tools to achieve high reliability. Health Serv. Res. 2006, 41, 1690–1709. [Google Scholar] [CrossRef]
- Daly, J.; Jackson, D.; Mannix, J.; Davidson, P.M.; Hutchinson, M. The importance of clinical leadership in the hospital setting. J. Healthc. Leadersh. 2014, 21, 75–83. [Google Scholar] [CrossRef]
- Karamitri, I.; Talias, M.A.; Bellali, T. Knowledge management practices in healthcare settings: A systematic review. Int. J. Health Plan. Manag. 2017, 32, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Li, S.A.; Jeffs, L.; Barwick, M.; Stevens, B. Organizational contextual features that influence the implementation of evidence-based practices across healthcare settings: A systematic integrative review. Syst. Rev. 2018, 7, 72. [Google Scholar] [CrossRef]
- Taneja, S.; Sewell, S.S.; Odom, R.Y. A culture of employee engagement: A strategic perspective for global managers. J. Bus. Strategy 2015, 36, 46–56. [Google Scholar] [CrossRef]
- Smith, M.; Bititci, U.S. Interplay between performance measurement and management, employee engagement and performance. Int. J. Oper. Prod. Manag. 2017, 37, 1207–1228. [Google Scholar] [CrossRef]
- Langenwalter, G.A. Enterprise Resources Planning and Beyond: Integrating Your Entire Organization; CRC Press: Boca Raton, FL, USA, 2020. [Google Scholar]
- Beşikci, U.; Bilge, Ü.; Ulusoy, G. Multi-mode resource constrained multi-project scheduling and resource portfolio problem. Eur. J. Oper. Res. 2015, 240, 22–31. [Google Scholar] [CrossRef]
- Awang, M.; Idris, M.R.; Zakaria, Z. Lean readiness index for Malaysian hospitals: An exploratory study. Int. J. Ind. Eng. Prod. Res. 2023, 33, 1–11. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).