Diagnostic Potential of Endometrial Cancer DNA from Pipelle, Pap-Brush, and Swab Sampling
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
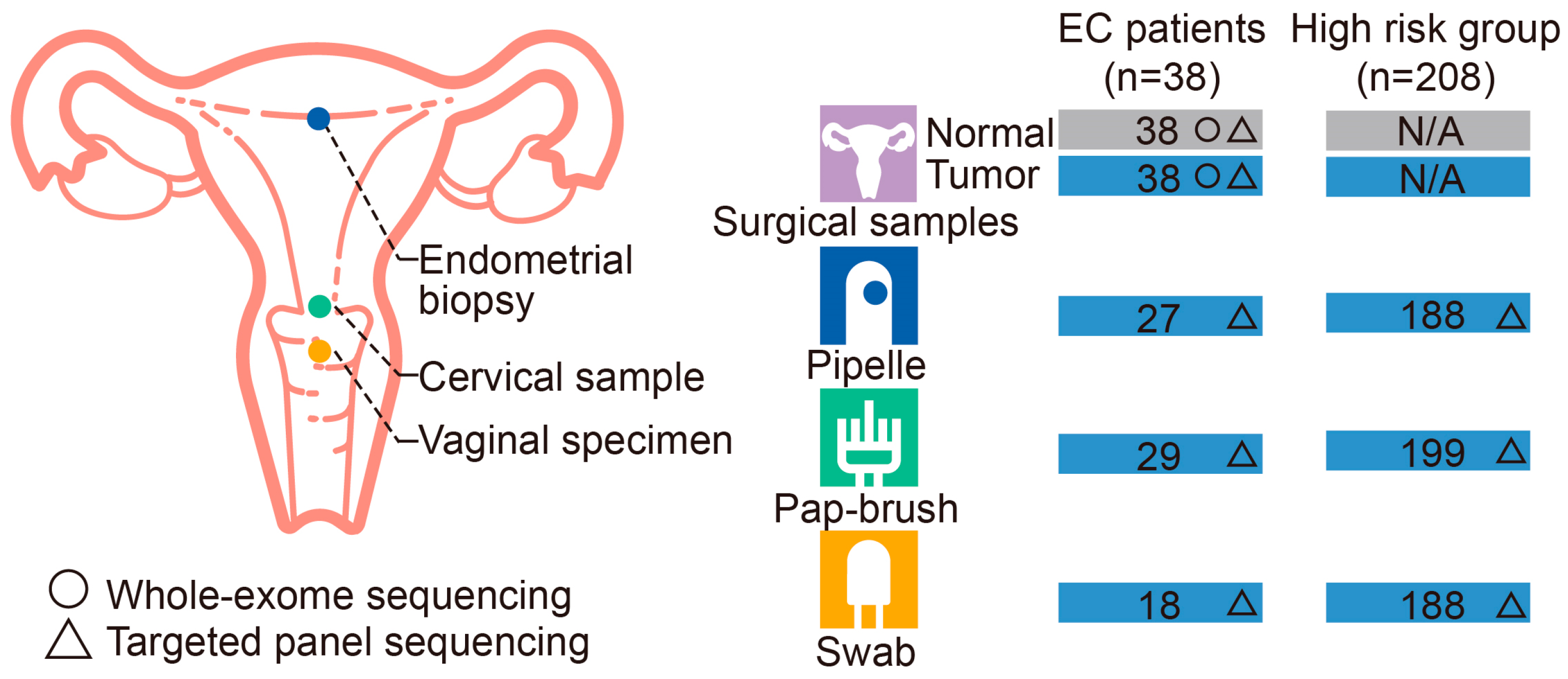
2.1. Patients and Sample Collection
2.2. WES and Data Analysis
2.3. Targeted NGS Panel Customization, Sequencing, and Analysis
2.4. Statistical Analysis
3. Results
3.1. Cohort Characteristics of Study Participants
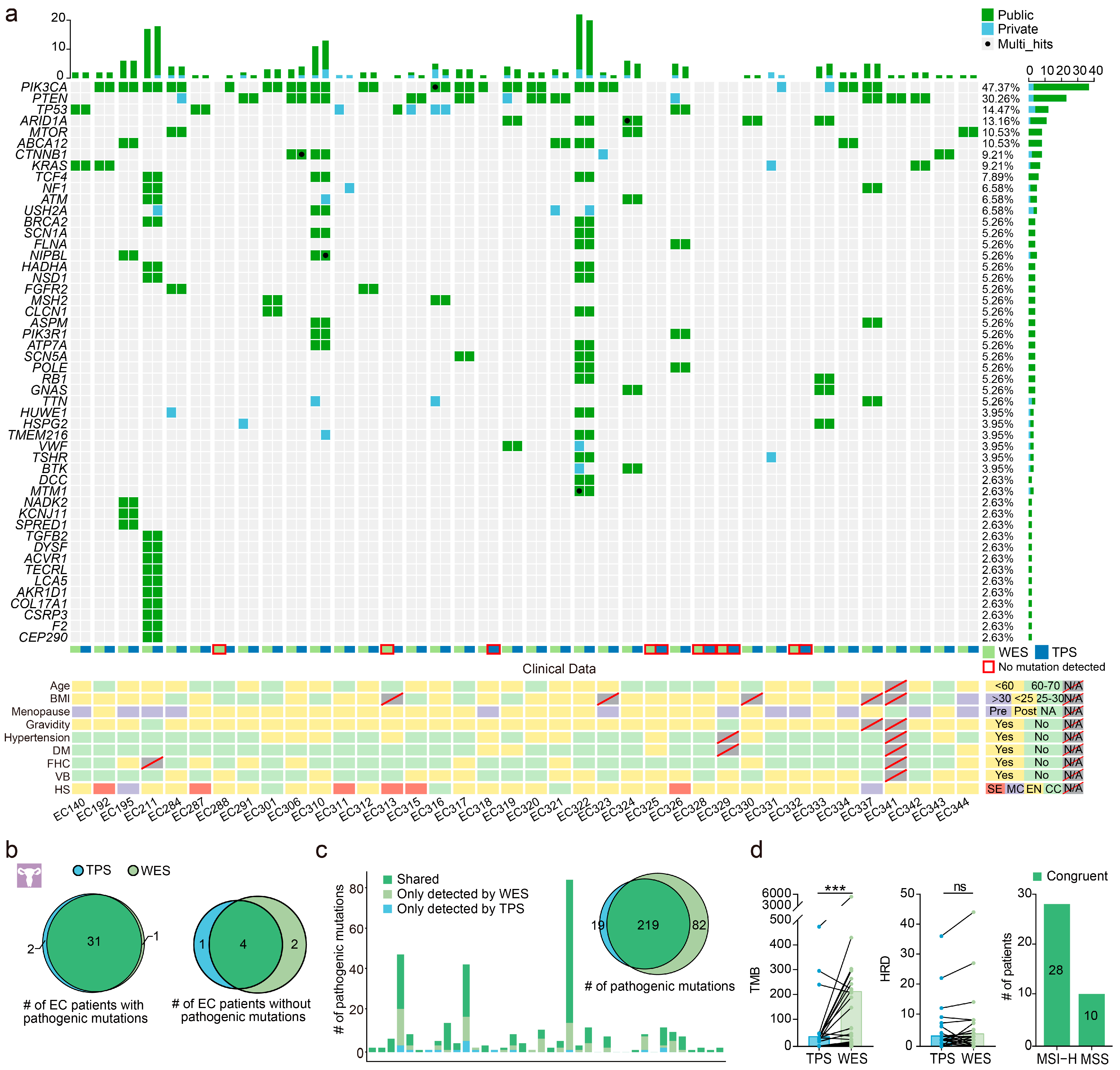
3.2. Performance of the Custom Panel in Surgical Specimens
3.3. TPS Data Quality of Endometrial, Cervical, and Vaginal Samples
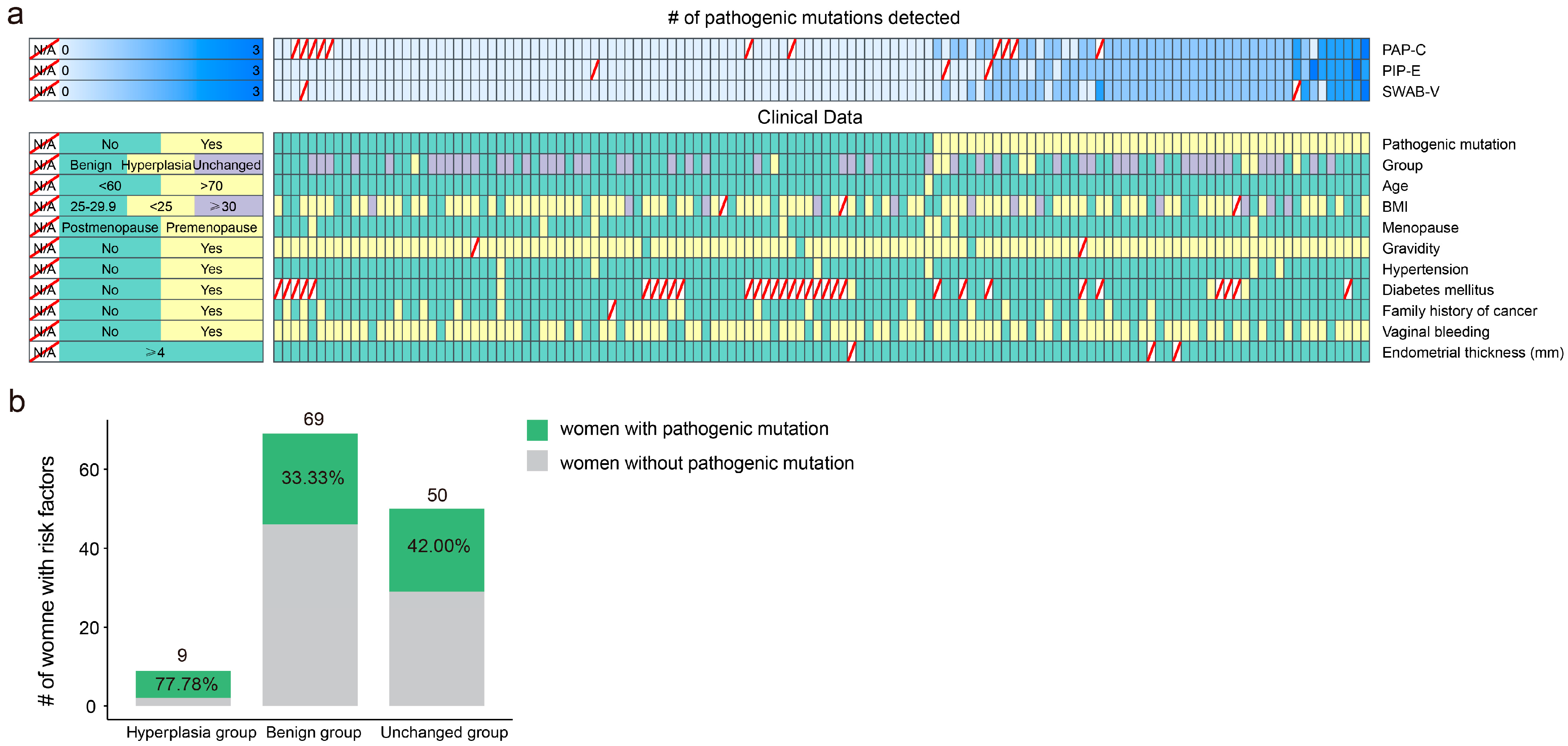
3.4. Early Detection Effectiveness of Endometrial, Cervical, and Vaginal Samples for EC Patients and Women with Risk Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Henley, S.J.; Ward, E.M.; Scott, S.; Ma, J.; Anderson, R.N.; Firth, A.U.; Thomas, C.C.; Islami, F.; Weir, H.K.; Lewis, D.R.; et al. Annual report to the nation on the status of cancer, part I: National cancer statistics. Cancer 2020, 126, 2225–2249. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.J.; Mann, C.H.; Shah, N.; Khan, K.S.; Song, F.; Gupta, J.K. Accuracy of outpatient endometrial biopsy in the diagnosis of endometrial cancer: A systematic quantitative review. BJOG Int. J. Obstet. Gynaecol. 2002, 109, 313–321. [Google Scholar] [CrossRef]
- Van Hanegem, N.; Prins, M.M.; Bongers, M.Y.; Opmeer, B.C.; Sahota, D.S.; Mol, B.W. Timmermans A: The accuracy of endometrial sampling in women with postmenopausal bleeding: A systematic review and meta-analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 197, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Costas, L.; Frias-Gomez, J.; Guardiola, M.; Benavente, Y.; Pineda, M.; Pavón, M.Á.; Martínez, J.M.; Climent, M.; Barahona, M.; Canet, J.; et al. New perspectives on screening and early detection of endometrial cancer. Int. J. Cancer 2019, 145, 3194–3206. [Google Scholar] [CrossRef] [PubMed]
- Kinde, I.; Bettegowda, C.; Wang, Y.; Wu, J.; Agrawal, N.; Shih Ie, M.; Kurman, R.; Dao, F.; Levine, D.A.; Giuntoli, R.; et al. Evaluation of DNA from the Papanicolaou test to detect ovarian and endometrial cancers. Sci. Transl. Med. 2013, 5, 167ra164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reijnen, C.; van der Putten, L.J.M.; Bulten, J.; Snijders, M.P.L.M.; Küsters-Vandevelde, H.V.N.; Sweegers, S.; Vos, M.C.; van der Wurff, A.A.M.; Ligtenberg, M.J.L.; Massuger, L.F.A.G.; et al. Mutational analysis of cervical cytology improves diagnosis of endometrial cancer: A prospective multicentre cohort study. Int. J. Cancer 2020, 146, 2628–2635. [Google Scholar] [CrossRef]
- Wang, Y.; Li, L.; Douville, C.; Cohen, J.D.; Yen, T.T.; Kinde, I.; Sundfelt, K.; Kjær, S.K.; Hruban, R.H.; Shih, I.M.; et al. Evaluation of liquid from the Papanicolaou test and other liquid biopsies for the detection of endometrial and ovarian cancers. Sci. Transl. Med. 2018, 10, eaap8793. [Google Scholar] [CrossRef] [Green Version]
- Makker, V.; MacKay, H.; Ray-Coquard, I.; Levine, D.A.; Westin, S.N.; Aoki, D.; Oaknin, A. Endometrial cancer. Nat. Rev. Dis. Primers 2021, 7, 88. [Google Scholar] [CrossRef]
- BGI: Extraction of Animal DNA BGI-NGS-TQ-DNA-003 A0; BGI: Shenzhen, China, 2022.
- BGI: Whole Exome Sequencing Library Preparation (DNBSEQ) BGI-NGS-JK-DNA-002 A0; BGI: Shenzhen, China, 2022.
- Chen, Y.; Chen, Y.; Shi, C.; Huang, Z.; Zhang, Y.; Li, S.; Li, Y.; Ye, J.; Yu, C.; Li, Z.; et al. SOAPnuke: A MapReduce acceleration-supported software for integrated quality control and preprocessing of high-throughput sequencing data. GigaScience 2018, 7, gix120. [Google Scholar] [CrossRef] [Green Version]
- Ewels, P.; Magnusson, M.; Lundin, S.; Käller, M. MultiQC: Summarize analysis results for multiple tools and samples in a single report. Bioinformatics 2016, 32, 3047–3048. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, H. Durbin R: Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 2009, 25, 1754–1760. [Google Scholar] [CrossRef] [Green Version]
- McKenna, A.; Hanna, M.; Banks, E.; Sivachenko, A.; Cibulskis, K.; Kernytsky, A.; Garimella, K.; Altshuler, D.; Gabriel, S.; Daly, M.; et al. The Genome Analysis Toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010, 20, 1297–1303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Niu, B.; Ye, K.; Zhang, Q.; Lu, C.; Xie, M.; McLellan, M.D.; Wendl, M.C.; Ding, L. MSIsensor: Microsatellite instability detection using paired tumor-normal sequence data. Bioinformatics 2014, 30, 1015–1016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sztupinszki, Z.; Diossy, M.; Krzystanek, M.; Reiniger, L.; Csabai, I.; Favero, F.; Birkbak, N.J.; Eklund, A.C.; Syed, A.; Szallasi, Z. Migrating the SNP array-based homologous recombination deficiency measures to next generation sequencing data of breast cancer. NPJ Breast Cancer 2018, 4, 16. [Google Scholar] [CrossRef] [Green Version]
- Auton, A.; Brooks, L.D.; Durbin, R.M.; Garrison, E.P.; Kang, H.M.; Korbel, J.O.; Marchini, J.L.; McCarthy, S.; McVean, G.A.; Abecasis, G.R. A global reference for human genetic variation. Nature 2015, 526, 68–74. [Google Scholar]
- Urick, M.E.; Bell, D.W. Clinical actionability of molecular targets in endometrial cancer. Nat. Rev. Cancer 2019, 19, 510–521. [Google Scholar] [CrossRef]
- Jia, W.; Li, H.; Li, S.; Chen, L.; Li, S.C. Oviz-Bio: A web-based platform for interactive cancer genomics data visualization. Nucleic Acids Res. 2020, 48, W415–W426. [Google Scholar] [CrossRef]
- Maritschnegg, E.; Wang, Y.; Pecha, N.; Horvat, R.; Van Nieuwenhuysen, E.; Vergote, I.; Heitz, F.; Sehouli, J.; Kinde, I.; Diaz, L.A., Jr.; et al. Lavage of the Uterine Cavity for Molecular Detection of Müllerian Duct Carcinomas: A Proof-of-Concept Study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 4293–4300. [Google Scholar] [CrossRef]
- Nair, N.; Camacho-Vanegas, O.; Rykunov, D.; Dashkoff, M.; Camacho, S.C.; Schumacher, C.A.; Irish, J.C.; Harkins, T.T.; Freeman, E.; Garcia, I.; et al. Genomic Analysis of Uterine Lavage Fluid Detects Early Endometrial Cancers and Reveals a Prevalent Landscape of Driver Mutations in Women without Histopathologic Evidence of Cancer: A Prospective Cross-Sectional Study. PLoS Med. 2016, 13, e1002206. [Google Scholar] [CrossRef] [Green Version]
- Levine, D.A.; Getz, G.; Gabriel, S.B.; Cibulskis, K.; Lander, E.; Sivachenko, A.; Sougnez, C.; Lawrence, M.; Kandoth, C.; Dooling, D.; et al. Integrated genomic characterization of endometrial carcinoma. Nature 2013, 497, 67–73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McConechy, M.K.; Ding, J.; Cheang, M.C.; Wiegand, K.; Senz, J.; Tone, A.; Yang, W.; Prentice, L.; Tse, K.; Zeng, T.; et al. Use of mutation profiles to refine the classification of endometrial carcinomas. J. Pathol. 2012, 228, 20–30. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byron, S.A.; Gartside, M.; Powell, M.A.; Wellens, C.L.; Gao, F.; Mutch, D.G.; Goodfellow, P.J.; Pollock, P.M. FGFR2 point mutations in 466 endometrioid endometrial tumors: Relationship with MSI, KRAS, PIK3CA, CTNNB1 mutations and clinicopathological features. PLoS ONE 2012, 7, e30801. [Google Scholar] [CrossRef]
- Le Gallo, M.; O’Hara, A.J.; Rudd, M.L.; Urick, M.E.; Hansen, N.F.; O’Neil, N.J.; Price, J.C.; Zhang, S.; England, B.M.; Godwin, A.K.; et al. Exome sequencing of serous endometrial tumors identifies recurrent somatic mutations in chromatin-remodeling and ubiquitin ligase complex genes. Nat. Genet. 2012, 44, 1310–1315. [Google Scholar] [CrossRef] [Green Version]
- Schultheis, A.M.; Martelotto, L.G.; De Filippo, M.R.; Piscuglio, S.; Ng, C.K.; Hussein, Y.R.; Reis-Filho, J.S.; Soslow, R.A.; Weigelt, B. TP53 Mutational Spectrum in Endometrioid and Serous Endometrial Cancers. Int. J. Gynecol. Pathol. Off. J. Int. Soc. Gynecol. Pathol. 2016, 35, 289–300. [Google Scholar] [CrossRef] [Green Version]
- van der Putten, L.J.M.; van Hoof, R.; Tops, B.B.J.; Snijders, M.P.L.M.; van den Berg-van Erp, S.H.; van der Wurff, A.A.M.; Bulten, J.; Pijnenborg, J.M.A.; Massuger, L.F.A.G. Molecular profiles of benign and (pre)malignant endometrial lesions. Carcinogenesis 2017, 38, 329–335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latta, E.; Chapman, W.B. PTEN mutations and evolving concepts in endometrial neoplasia. Curr. Opin. Obstet. Gynecol. 2002, 14, 59–65. [Google Scholar] [CrossRef]
- Ruz-Caracuel, I.; López-Janeiro, Á.; Heredia-Soto, V.; Ramón-Patino, J.L.; Yébenes, L.; Berjón, A.; Hernández, A.; Gallego, A.; Ruiz, P.; Redondo, A.; et al. Clinicopathological features and prognostic significance of CTNNB1 mutation in low-grade, early-stage endometrial endometrioid carcinoma. Virchows Arch. Int. J. Pathol. 2021, 479, 1167–1176. [Google Scholar] [CrossRef]
- Peremiquel-Trillas, P.; Paytubi, S.; Pelegrina, B.; Frias-Gomez, J.; Carmona, Á.; Martínez, J.M.; de Francisco, J.; Benavente, Y.; Barahona, M.; Briansó, F.; et al. An Integrated Approach for the Early Detection of Endometrial and Ovarian Cancers (Screenwide Study): Rationale, Study Design and Pilot Study. J. Pers. Med. 2022, 12, 1074. [Google Scholar] [CrossRef]
- Mutter, G.L.; Monte, N.M.; Neuberg, D.; Ferenczy, A.; Eng, C. Emergence, involution, and progression to carcinoma of mutant clones in normal endometrial tissues. Cancer Res. 2014, 74, 2796–2802. [Google Scholar] [CrossRef] [Green Version]
- Mota, A.; Colás, E.; García-Sanz, P.; Campoy, I.; Rojo-Sebastián, A.; Gatius, S.; García, Á.; Chiva, L.; Alonso, S.; Gil-Moreno, A.; et al. Genetic analysis of uterine aspirates improves the diagnostic value and captures the intra-tumor heterogeneity of endometrial cancers. Mod. Pathol. 2017, 30, 134–145. [Google Scholar] [CrossRef] [Green Version]
- Kinde, I.; Wu, J.; Papadopoulos, N.; Kinzler, K.W.; Vogelstein, B. Detection and quantification of rare mutations with massively parallel sequencing. Proc. Natl. Acad. Sci. USA 2011, 108, 9530–9535. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, M.W.; Kennedy, S.R.; Salk, J.J.; Fox, E.J.; Hiatt, J.B.; Loeb, L.A. Detection of ultra-rare mutations by next-generation sequencing. Proc. Natl. Acad. Sci. USA 2012, 109, 14508–14513. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.R.; Chen, S.X.; Wu, Y.; Patel, A.A.; Zhang, D.Y. Multiplexed enrichment of rare DNA variants via sequence-selective and temperature-robust amplification. Nat. Biomed. Eng. 2017, 1, 714–723. [Google Scholar] [CrossRef] [PubMed]
- Xu, C. A review of somatic single nucleotide variant calling algorithms for next-generation sequencing data. Comput. Struct. Biotechnol. J. 2018, 16, 15–24. [Google Scholar] [CrossRef]
- Xu, H.; DiCarlo, J.; Satya, R.V.; Peng, Q.; Wang, Y. Comparison of somatic mutation calling methods in amplicon and whole exome sequence data. BMC Genom. 2014, 15, 244. [Google Scholar] [CrossRef] [Green Version]
- Shih, I.M.; Wang, Y.; Wang, T.L. The Origin of Ovarian Cancer Species and Precancerous Landscape. Am. J. Pathol. 2021, 191, 26–39. [Google Scholar] [CrossRef]


| Variable | EC Group (n = 38) | Potential Risk Group (n = 208) | All (n = 246) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Age at diagnosis, median (range) | 56 (33–65) | 45 (23–75) | 46 (23–75) |
| <60 years | 22 (57.89) | 199 (95.67) | 221 (89.84) |
| 60–70 years | 15 (39.47) | 6 (2.88) | 21 (8.54) |
| >70 years | 0 (0) | 1 (0.48) | 1 (0.41) |
| Missing data | 1 (2.63) | 2 (0.96) | 3 (1.22) |
| BMI (kg/m2) | |||
| <25 | 23 (60.53) | 130 (62.50) | 153 (62.20) |
| 25–29.9 | 9 (23.68) | 52 (25.00) | 61 (24.80) |
| ≥30 | 1 (2.63) | 18 (8.65) | 19 (7.72) |
| Missing data | 5 (13.16) | 8 (3.85) | 13 (5.28) |
| Histological subtype | |||
| Endometrioid | 27 (71.05) | 0 (0) | 27 (10.98) |
| Serous | 6 (15.79) | 0 (0) | 6 (2.44) |
| Clear cell | 3 (7.89) | 0 (0) | 3 (1.22) |
| Mixed carcinomas | 2 (5.26) | 0 (0) | 2 (0.81) |
| Atypical endometrial hyperplasia | 0 (0) | 1 (0.48) | 1 (0.41) |
| Endometrial hyperplasia | 0 (0) | 8 (3.85) | 8 (3.25) |
| Cystic endometrial atrophy | 0 (0) | 1 (0.48) | 1 (0.41) |
| Endometrial polyp | 0 (0) | 4 (1.92) | 4 (1.63) |
| Benign cystic glandular hyperplasia | 0 (0) | 41 (19.71) | 41 (16.67) |
| Chronic endometritis | 0 (0) | 23 (11.06) | 23 (9.35) |
| Proliferative phase | 0 (0) | 28 (13.46) | 28 (11.38) |
| Secretory phase | 0 (0) | 22 (10.58) | 22 (8.94) |
| Others | 0 (0) | 10 (4.81) | 10 (4.07) |
| Missing data | 0 (0) | 70 (33.65) | 70 (28.46) |
| Menopausal state | |||
| Premenopausal | 12 (31.58) | 182 (77.12) | 194 (78.86) |
| Postmenopausal | 25 (65.79) | 24 (10.17) | 49 (19.92) |
| Missing data | 1 (2.63) | 2 (0.85) | 3 (1.22) |
| Vaginal bleeding | |||
| Yes | 34 (89.47) | 149 (71.63) | 183 (74.39) |
| No | 2 (5.26) | 57 (27.40) | 59 (23.98) |
| Missing data | 2 (5.26) | 2 (0.96) | 4 (1.63) |
| Endometrial thickness | |||
| <4 mm | 0 (0) | 3 (1.44) | 3 (1.22) |
| ≥4 mm | 20 (52.63) | 194 (93.27) | 214 (86.99) |
| Missing data | 18 (47.37) | 11 (5.29) | 29 (11.79) |
| Gravidity | |||
| Yes | 34 (89.47) | 196 (94.23) | 230 (93.50) |
| No | 2 (5.26) | 7 (3.3652) | 9 (3.66) |
| Missing data | 2 (5.26) | 5 (2.40) | 7 (2.84) |
| Hypertension | |||
| Yes | 10 (26.32) | 16 (7.69) | 26 (10.57) |
| No | 26 (68.42) | 190 (91.35) | 216 (87.80) |
| Missing data | 2 (5.26) | 2 (0.96) | 4 (1.63) |
| Diabetes | |||
| Yes | 4 (10.53) | 9 (4.33) | 13 (5.28) |
| No | 32 (84.21) | 138 (66.35) | 170 (69.11) |
| Missing data | 2 (5.26) | 61 (29.33) | 63 (25.61) |
| Family history of cancer | |||
| Yes | 8 (21.05) | 25 (12.02) | 33 (13.41) |
| No | 28 (73.68) | 179 (86.06) | 207 (84.15) |
| Missing data | 2 (5.26) | 4 (1.92) | 6 (2.44) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Du, H.; Dai, W.; Bao, C.; Zhang, X.; Hu, Y.; Xie, Z.; Zhao, X.; Li, C.; Zhang, W.; et al. Diagnostic Potential of Endometrial Cancer DNA from Pipelle, Pap-Brush, and Swab Sampling. Cancers 2023, 15, 3522. https://doi.org/10.3390/cancers15133522
Wang Y, Du H, Dai W, Bao C, Zhang X, Hu Y, Xie Z, Zhao X, Li C, Zhang W, et al. Diagnostic Potential of Endometrial Cancer DNA from Pipelle, Pap-Brush, and Swab Sampling. Cancers. 2023; 15(13):3522. https://doi.org/10.3390/cancers15133522
Chicago/Turabian StyleWang, Yinan, Hui Du, Wenkui Dai, Cuijun Bao, Xi Zhang, Yan Hu, Zhiyu Xie, Xin Zhao, Changzhong Li, Wenyong Zhang, and et al. 2023. "Diagnostic Potential of Endometrial Cancer DNA from Pipelle, Pap-Brush, and Swab Sampling" Cancers 15, no. 13: 3522. https://doi.org/10.3390/cancers15133522
APA StyleWang, Y., Du, H., Dai, W., Bao, C., Zhang, X., Hu, Y., Xie, Z., Zhao, X., Li, C., Zhang, W., & Wu, R. (2023). Diagnostic Potential of Endometrial Cancer DNA from Pipelle, Pap-Brush, and Swab Sampling. Cancers, 15(13), 3522. https://doi.org/10.3390/cancers15133522





