Prognostic Significance of EGFR, HER2, and c-Met Overexpression in Surgically Treated Patients with Adenocarcinoma of the Ampulla of Vater
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Data Acquisition
2.2. Tissue Microarray and Immunohistochemistry
2.3. Histologic Subtypes
2.4. Immunohistochemical Analysis
2.5. Treatment and Surveillance
2.6. Statistical Analysis
3. Results
3.1. Patients Characteristics
3.2. Characteristics of Patients Stratified by EGFR, HER2, and c-Met Expression
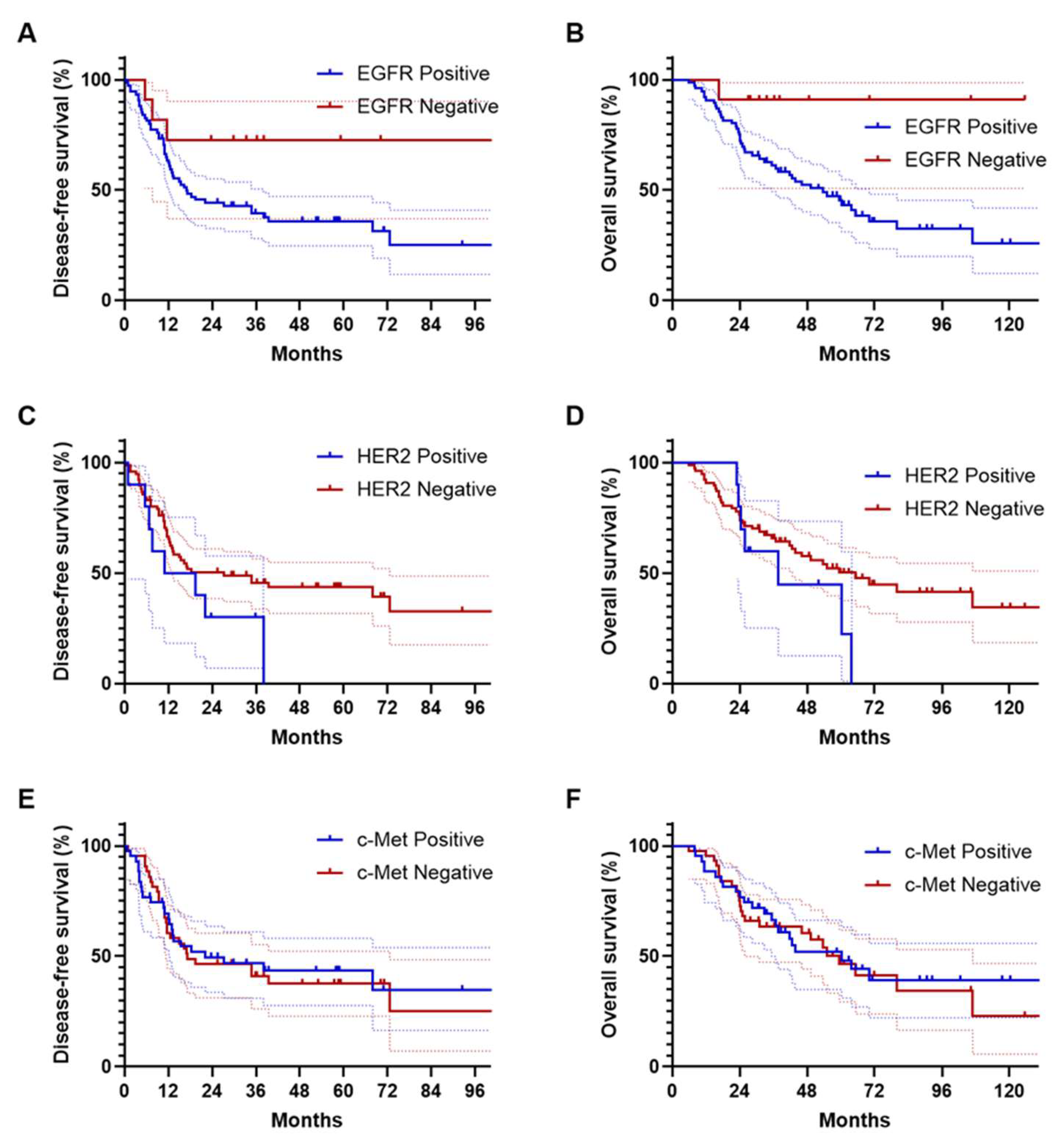
3.3. Survival Outcomes
3.4. Survival Analyses Based on EGFR Expression
3.5. Survival Outcomes in Relation to HER2 and c-Met Expression
3.6. Multivariate Analysis of Survival Outcomes
3.7. Survival Outcomes after Recurrence
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ahn, D.H.; Bekaii-Saab, T. Ampullary cancer: An overview. Am. Soc. Clin. Oncol. Educ. Book 2014, 34, 112–115. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Wu, R.; Zhang, G.; Yang, Z.; Zhang, L. Prognostic importance of numbers of retrieved lymph nodes and positive lymph nodes for ampulla of vater cancer (AVC) in 2347 patients from the Surveillance, Epidemiology, and End Results (SEER) database. PLoS ONE 2021, 16, e0244987. [Google Scholar] [CrossRef] [PubMed]
- Valle, J.; Wasan, H.; Palmer, D.H.; Cunningham, D.; Anthoney, A.; Maraveyas, A.; Madhusudan, S.; Iveson, T.; Hughes, S.; Pereira, S.P. Cisplatin plus gemcitabine versus gemcitabine for biliary tract cancer. N. Engl. J. Med. 2010, 362, 1273–1281. [Google Scholar] [CrossRef] [PubMed]
- Overman, M.J.; Varadhachary, G.R.; Kopetz, S.; Adinin, R.; Lin, E.; Morris, J.S.; Eng, C.; Abbruzzese, J.L.; Wolff, R.A. Phase II study of capecitabine and oxaliplatin for advanced adenocarcinoma of the small bowel and ampulla of Vater. J. Clin. Oncol. 2009, 27, 2598–2603. [Google Scholar] [CrossRef] [PubMed]
- Ang, D.C.; Shia, J.; Tang, L.H.; Katabi, N.; Klimstra, D.S. The utility of immunohistochemistry in subtyping adenocarcinoma of the ampulla of vater. Am. J. Surg. Pathol. 2014, 38, 1371–1379. [Google Scholar] [CrossRef] [PubMed]
- Chang, D.K.; Jamieson, N.B.; Johns, A.L.; Scarlett, C.J.; Pajic, M.; Chou, A.; Pinese, M.; Humphris, J.L.; Jones, M.D.; Toon, C. Histomolecular phenotypes and outcome in adenocarcinoma of the ampulla of vater. J. Clin. Oncol. 2013, 31, 1348–1356. [Google Scholar] [CrossRef] [PubMed]
- Bosman, F.T. WHO classification of tumors of the digestive system. In Adenocarcinoma of the Appendix; WHO: Geneva, Switzerland, 2010; pp. 120–125. [Google Scholar]
- Pea, A.; Riva, G.; Bernasconi, R.; Sereni, E.; Lawlor, R.T.; Scarpa, A.; Luchini, C. Ampulla of Vater carcinoma: Molecular landscape and clinical implications. World J. Gastrointest. Oncol. 2018, 10, 370. [Google Scholar] [CrossRef]
- Lamarca, A.; Edeline, J.; Goyal, L. How I treat biliary tract cancer. ESMO Open 2022, 7, 100378. [Google Scholar] [CrossRef]
- Stefani, C.; Miricescu, D.; Stanescu-Spinu, I.-I.; Nica, R.I.; Greabu, M.; Totan, A.R.; Jinga, M. Growth factors, PI3K/AKT/mTOR and MAPK signaling pathways in colorectal cancer pathogenesis: Where are we now? Int. J. Mol. Sci. 2021, 22, 10260. [Google Scholar] [CrossRef]
- Cohen, R.B. Epidermal growth factor receptor as a therapeutic target in colorectal cancer. Clin. Color. Cancer 2003, 2, 246–251. [Google Scholar] [CrossRef]
- Valsecchi, M.E.; McDonald, M.; Brody, J.R.; Hyslop, T.; Freydin, B.; Yeo, C.J.; Solomides, C.; Peiper, S.C.; Witkiewicz, A.K. Epidermal growth factor receptor and insulinlike growth factor 1 receptor expression predict poor survival in pancreatic ductal adenocarcinoma. Cancer 2012, 118, 3484–3493. [Google Scholar] [CrossRef] [PubMed]
- Mikhitarian, K.; Pollen, M.; Zhao, Z.; Shyr, Y.; Merchant, N.B.; Parikh, A.; Revetta, F.; Washington, M.K.; Vnencak-Jones, C.; Shi, C. Epidermal growth factor receptor signaling pathway is frequently altered in ampullary carcinoma at protein and genetic levels. Mod. Pathol. 2014, 27, 665–674. [Google Scholar] [CrossRef] [PubMed]
- Moasser, M.M. The oncogene HER2: Its signaling and transforming functions and its role in human cancer pathogenesis. Oncogene 2007, 26, 6469–6487. [Google Scholar] [CrossRef] [PubMed]
- Cooke, T.; Reeves, J.; Lanigan, A.; Stanton, P. HER2 as a prognostic and predictive marker for breast cancer. Ann. Oncol. 2001, 12, S23–S28. [Google Scholar] [CrossRef] [PubMed]
- Grávalos, C.; Jimeno, A. HER2 in gastric cancer: A new prognostic factor and a novel therapeutic target. Ann. Oncol. 2008, 19, 1523–1529. [Google Scholar] [CrossRef] [PubMed]
- Vivaldi, C.; Fornaro, L.; Ugolini, C.; Niccoli, C.; Musettini, G.; Pecora, I.; Cacciato Insilla, A.; Salani, F.; Pasquini, G.; Catanese, S. HER2 overexpression as a poor prognostic determinant in resected biliary tract cancer. Oncologist 2020, 25, 886–893. [Google Scholar] [CrossRef] [PubMed]
- Oh, D.-Y.; Bang, Y.-J. HER2-targeted therapies—A role beyond breast cancer. Nat. Rev. Clin. Oncol. 2020, 17, 33–48. [Google Scholar] [CrossRef] [PubMed]
- Olson, E.M. Maximizing human epidermal growth factor receptor 2 inhibition: A new oncologic paradigm in the era of targeted therapy. J. Clin. Oncol. 2012, 30, 1712–1714. [Google Scholar] [CrossRef]
- Hechtman, J.F.; Liu, W.; Sadowska, J.; Zhen, L.; Borsu, L.; Arcila, M.E.; Won, H.H.; Shah, R.H.; Berger, M.F.; Vakiani, E. Sequencing of 279 cancer genes in ampullary carcinoma reveals trends relating to histologic subtypes and frequent amplification and overexpression of ERBB2 (HER2). Mod. Pathol. 2015, 28, 1123–1129. [Google Scholar] [CrossRef]
- Hiraoka, N.; Nitta, H.; Ohba, A.; Yoshida, H.; Morizane, C.; Okusaka, T.; Nara, S.; Esaki, M.; Kishi, Y.; Shimada, K. Details of human epidermal growth factor receptor 2 status in 454 cases of biliary tract cancer. Hum. Pathol. 2020, 105, 9–19. [Google Scholar] [CrossRef]
- Sierra, J.R.; Tsao, M.-S. c-MET as a potential therapeutic target and biomarker in cancer. Ther. Adv. Med. Oncol. 2011, 3, S21–S35. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, M.; Ojima, H.; Iwasaki, M.; Shimizu, H.; Kokubu, A.; Hiraoka, N.; Kosuge, T.; Yoshikawa, D.; Kono, T.; Furukawa, H. Prognostic significance of overexpression of c-Met oncoprotein in cholangiocarcinoma. Br. J. Cancer 2011, 105, 131–138. [Google Scholar] [CrossRef] [PubMed]
- Rizwani, W.; Allen, A.E.; Trevino, J.G. Hepatocyte growth factor from a clinical perspective: A pancreatic cancer challenge. Cancers 2015, 7, 1785–1805. [Google Scholar] [CrossRef] [PubMed]
- Kwon, M.J.; Kim, J.W.; Jeon, J.Y.; Nam, E.S.; Cho, S.J.; Park, H.-R.; Min, S.K.; Seo, J.; Min, K.-W.; Choe, J.-Y. Concurrent MET copy number gain and KRAS mutation is a poor prognostic factor in pancreatobiliary subtype ampullary cancers. Pathol.-Res. Pract. 2017, 213, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Shin, K.; Hong, T.H.; Lee, S.H.; Kim, I.-H.; Kim, Y.; Lee, M. Histologic subtype-based evaluation of recurrence and survival outcomes in patients with adenocarcinoma of the ampulla of Vater. Sci. Rep. 2023, 13, 16547. [Google Scholar] [CrossRef] [PubMed]
- Luo, G.; Long, J.; Qiu, L.; Liu, C.; Xu, J.; Yu, X. Role of epidermal growth factor receptor expression on patient survival in pancreatic cancer: A meta-analysis. Pancreatology 2012, 11, 595–600. [Google Scholar] [CrossRef] [PubMed]
- Ayasun, R.; Ozer, M.; Sahin, I. The role of HER2 status in the biliary tract cancers. Cancers 2023, 15, 2628. [Google Scholar] [CrossRef] [PubMed]
- Ahcene Djaballah, S.; Daniel, F.; Milani, A.; Ricagno, G.; Lonardi, S. HER2 in colorectal cancer: The long and winding road from negative predictive factor to positive actionable target. Am. Soc. Clin. Oncol. Educ. Book 2022, 42, 219–232. [Google Scholar] [CrossRef]
- Stintzing, S.; Modest, D.P.; Rossius, L.; Lerch, M.M.; von Weikersthal, L.F.; Decker, T.; Kiani, A.; Vehling-Kaiser, U.; Al-Batran, S.-E.; Heintges, T. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab for metastatic colorectal cancer (FIRE-3): A post-hoc analysis of tumour dynamics in the final RAS wild-type subgroup of this randomised open-label phase 3 trial. Lancet Oncol. 2016, 17, 1426–1434. [Google Scholar] [CrossRef]
- Karapetis, C.S.; Khambata-Ford, S.; Jonker, D.J.; O’Callaghan, C.J.; Tu, D.; Tebbutt, N.C.; Simes, R.J.; Chalchal, H.; Shapiro, J.D.; Robitaille, S. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N. Engl. J. Med. 2008, 359, 1757–1765. [Google Scholar] [CrossRef]
- Harding, J.J.; Fan, J.; Oh, D.-Y.; Choi, H.J.; Kim, J.W.; Chang, H.-M.; Bao, L.; Sun, H.-C.; Macarulla, T.; Xie, F. Zanidatamab for HER2-amplified, unresectable, locally advanced or metastatic biliary tract cancer (HERIZON-BTC-01): A multicentre, single-arm, phase 2b study. Lancet Oncol. 2023, 24, 772–782. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Mizuno, N.; Sunakawa, Y.; Hamilton, E.P.; Hayashi, H.; Kim, S.T.; Lee, K.-W.; Monk, B.J.; Nguyen, D.; Okines, A.F.C. Tucatinib and trastuzumab for previously treated HER2-positive metastatic biliary tract cancer (SGNTUC-019): A phase 2 basket study. 2023.
- Cho, B.C.; Simi, A.; Sabari, J.; Vijayaraghavan, S.; Moores, S.; Spira, A. Amivantamab, an epidermal growth factor receptor (EGFR) and mesenchymal-epithelial transition factor (MET) bispecific antibody, designed to enable multiple mechanisms of action and broad clinical applications. Clin. Lung Cancer 2023, 24, 89–97. [Google Scholar] [CrossRef] [PubMed]
- El-Zammar, O.A.; Zhang, S.; Katzenstein, A.-L.A. Comparison of FISH, PCR, and immunohistochemistry in assessing EGFR status in lung adenocarcinoma and correlation with clinicopathologic features. Diagn. Mol. Pathol. 2009, 18, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Bhargava, R.; Gerald, W.L.; Li, A.R.; Pan, Q.; Lal, P.; Ladanyi, M.; Chen, B. EGFR gene amplification in breast cancer: Correlation with epidermal growth factor receptor mRNA and protein expression and HER-2 status and absence of EGFR-activating mutations. Mod. Pathol. 2005, 18, 1027–1033. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Lee, H.E.; Kim, M.A.; Jang, B.G.; Lee, H.S.; Kim, W.H. Analysis of MET mRNA expression in gastric cancers using RNA in situ hybridization assay: Its clinical implication and comparison with immunohistochemistry and silver in situ hybridization. PLoS ONE 2014, 9, e111658. [Google Scholar] [CrossRef]
- Guo, R.; Berry, L.D.; Aisner, D.L.; Sheren, J.; Boyle, T.; Bunn, P.A., Jr.; Johnson, B.E.; Kwiatkowski, D.J.; Drilon, A.; Sholl, L.M. MET IHC is a poor screen for MET amplification or MET exon 14 mutations in lung adenocarcinomas: Data from a tri-institutional cohort of the lung cancer mutation consortium. J. Thorac. Oncol. 2019, 14, 1666–1671. [Google Scholar] [CrossRef]

| Variables | Total (n = 87) | PB Type (n = 54) | Intestinal Type (n = 33) | p Value |
|---|---|---|---|---|
| Age, Median (range) | 65 (39–87) | 66 (39–87) | 65 (42–87) | 0.789 |
| Gender, n (%) | ||||
| Male | 49 (56.3) | 29 (53.7) | 20 (60.6) | 0.529 |
| Female | 38 (43.7) | 25 (46.3) | 13 (39.4) | |
| Tumor size, cm, mean ± SD | 2.5 ± 1.1 | 2.4 ± 1.0 | 2.5 ± 1.1 | 0.691 |
| Histologic grading, n (%) | ||||
| Grade 1 | 15 (17.2) | 7 (13.0) | 8 (24.2) | 0.177 |
| Grade 2/3 | 72 (82.8) | 47 (87.0) | 25 (75.8) | |
| Tumor Category, n (%) | ||||
| T1–2 | 47 (54.0) | 25 (46.3) | 22 (66.7) | 0.064 |
| T3–4 | 40 (46.0) | 29 (53.7) | 11 (33.3) | |
| Node Category, n (%) | ||||
| N0 | 37 (42.5) | 21 (38.9) | 16 (48.5) | 0.380 |
| N1–2 | 50 (57.5) | 33 (61.1) | 17 (51.5) | |
| TNM Stage *, n (%) | ||||
| Stage I–II | 38 (43.7) | 22 (40.7) | 16 (48.5) | 0.480 |
| Stage III–IV | 49 (56.3) | 32 (59.3) | 17 (51.5) | |
| EGFR expression, n (%) | ||||
| Positive | 76 (87.4) | 51 (94.4) | 25 (75.8) | 0.018 |
| Negative | 11 (12.6) | 3 (5.6) | 8 (24.2) | |
| HER2 expression, n (%) | ||||
| Positive | 10 (11.5) | 6 (11.1) | 4 (12.1) | 0.571 |
| Negative | 77 (88.5) | 48 (88.9) | 29 (87.9) | |
| c-Met expression, n (%) | ||||
| Positive | 43 (49.4) | 26 (48.1) | 17 (51.5) | 0.467 |
| Negative | 44 (50.6) | 28 (51.9) | 16 (48.5) | |
| Adjuvant chemotherapy, n (%) | ||||
| No | 44 (50.6) | 26 (48.1) | 18 (54.5) | 0.563 |
| Yes | 43 (49.4) | 28 (51.9) | 15 (45.5) | |
| Preoperative CA19-9 level, n (%) | ||||
| Within normal (<40 U/mL) | 39 (44.8) | 20 (37.0) | 19 (57.6) | 0.151 |
| Above normal (≥40 U/mL) | 40 (46.0) | 29 (53.7) | 11 (33.3) | |
| Missing data | 8 (9.2) | 5 (9.3) | 3 (9.1) |
| DFS | ||||
|---|---|---|---|---|
| Variables | Univariate Analysis | Multivariate Analysis | ||
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age ≥ 70 (vs. <70 year) | 1.33 (0.76–2.32) | 0.319 | ||
| Histologic grade 2–3 (vs. grade 1) | 2.60 (1.03–6.55) | 0.043 | 1.94 (0.75–4.99) | 0.171 |
| Tumor stage 3 or 4 (vs. Stage 1 or 2) | 2.49 (1.43–4.34) | 0.001 | 2.20 (1.23–3.92) | 0.008 |
| Nodal metastasis (vs. none) | 2.01 (1.12–3.61) | 0.019 | 1.13 (0.61–2.09) | 0.702 |
| Pancreatobiliary type (vs. intestinal) | 1.74 (0.95–3.17) | 0.072 | 1.20 (0.62–2.32) | 0.588 |
| EGFR expression (vs. none) | 2.89 (1.35–6.20) | 0.061 | 2.38 (0.69–8.23) | 0.172 |
| Received AC (vs. none) | 1.04 (0.60–1.79) | 0.899 | ||
| OS | ||||
|---|---|---|---|---|
| Variables | Univariate Analysis | Multivariate Analysis | ||
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age ≥ 70 (vs. <70 year) | 1.75 (0.96–3.18) | 0.069 | 1.74 (0.95–3.20) | 0.074 |
| Histologic grade 2–3 (vs. grade 1) | 1.98 (0.70–5.55) | 0.197 | ||
| Tumor stage 3 or 4 (vs. Stage 1 or 2) | 2.60 (1.42–4.76) | 0.002 | 2.44 (1.30–4.58) | 0.006 |
| Nodal metastasis (vs. none) | 1.70 (0.92–3.14) | 0.088 | 1.46 (0.77–2.75) | 0.243 |
| Pancreatobiliary type (vs. intestinal) | 2.09 (1.06–4.14) | 0.034 | 1.15 (0.56–2.39) | 0.706 |
| EGFR expression (vs. none) | 6.89 (2.94–16.2) | 0.026 | 6.26 (0.81–48.4) | 0.079 |
| Received AC (vs. none) | 0.96 (0.53–1.72) | 0.877 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, S.J.; Shin, K.; Hong, T.H.; Lee, S.H.; Kim, I.-H.; Kim, Y.; Lee, M. Prognostic Significance of EGFR, HER2, and c-Met Overexpression in Surgically Treated Patients with Adenocarcinoma of the Ampulla of Vater. Cancers 2024, 16, 2756. https://doi.org/10.3390/cancers16152756
Park SJ, Shin K, Hong TH, Lee SH, Kim I-H, Kim Y, Lee M. Prognostic Significance of EGFR, HER2, and c-Met Overexpression in Surgically Treated Patients with Adenocarcinoma of the Ampulla of Vater. Cancers. 2024; 16(15):2756. https://doi.org/10.3390/cancers16152756
Chicago/Turabian StylePark, Se Jun, Kabsoo Shin, Tae Ho Hong, Sung Hak Lee, In-Ho Kim, Younghoon Kim, and MyungAh Lee. 2024. "Prognostic Significance of EGFR, HER2, and c-Met Overexpression in Surgically Treated Patients with Adenocarcinoma of the Ampulla of Vater" Cancers 16, no. 15: 2756. https://doi.org/10.3390/cancers16152756





