Effect of Adhesion Conditions on the Shear Bond Strength of 3D Printing Resins after Thermocycling Used for Definitive Prosthesis
Abstract
1. Introduction
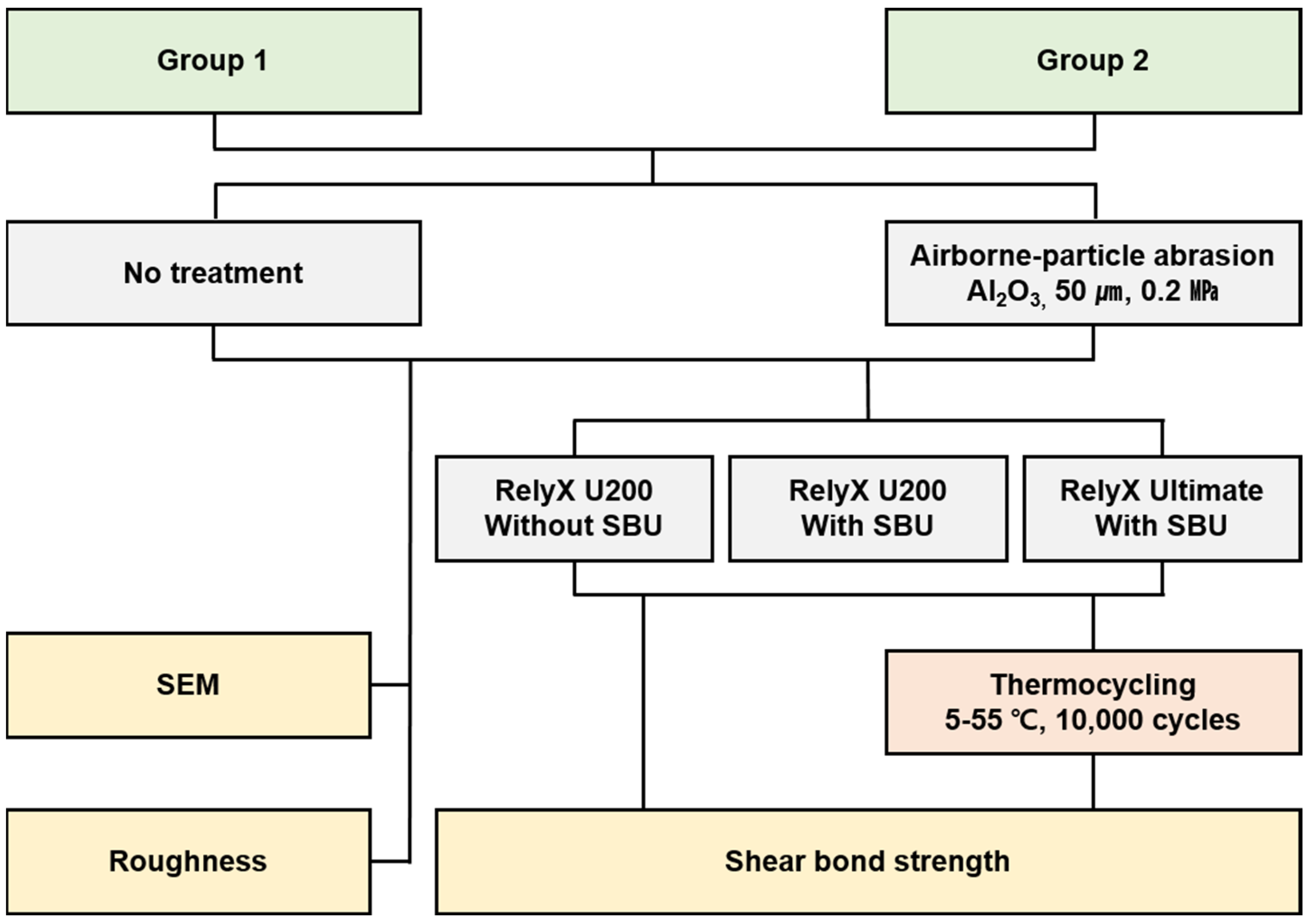
2. Materials and Methods
2.1. Preparation of Specimens
2.2. Shear Bond Strength
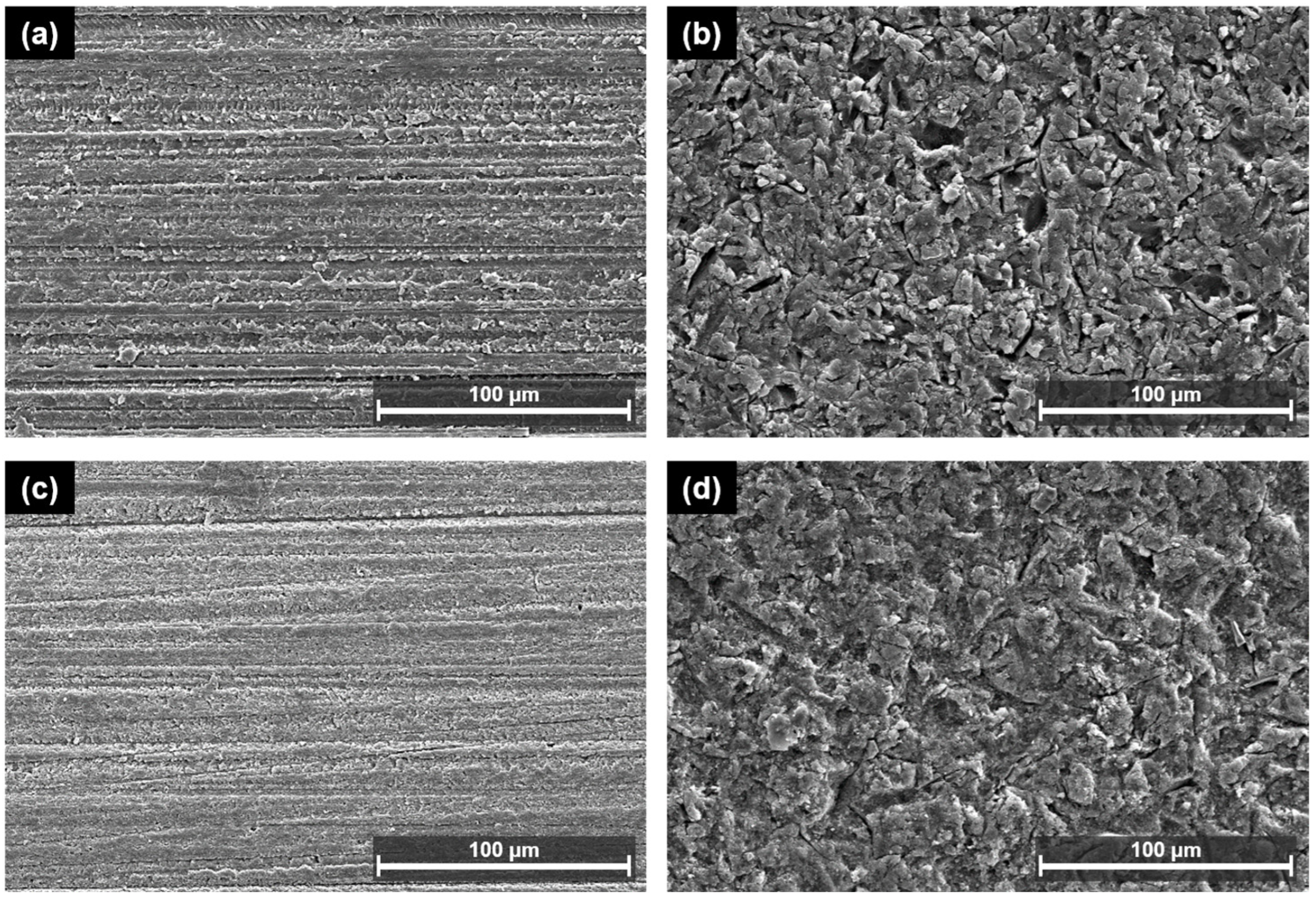
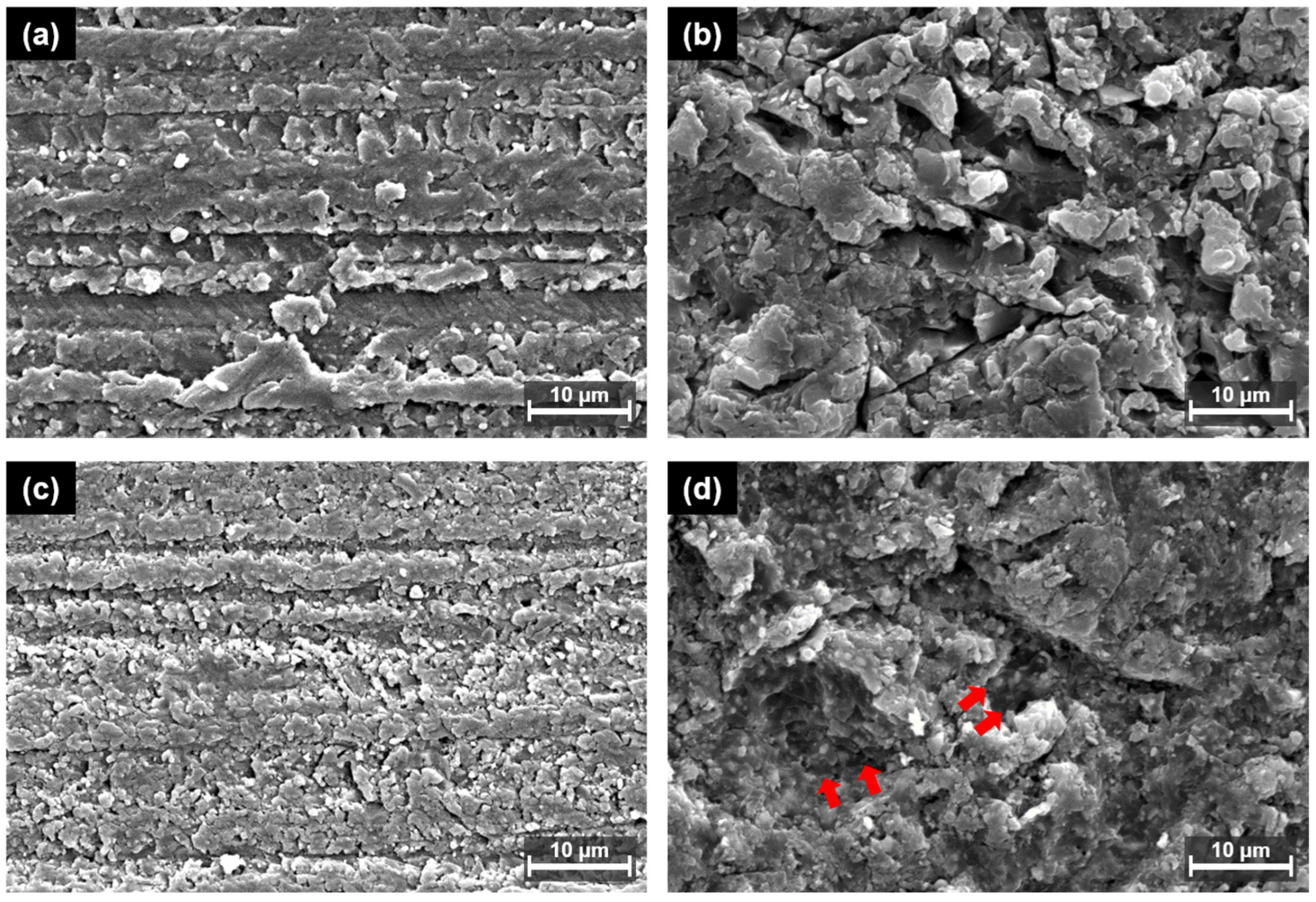
2.3. Scanning Electron Microscopy
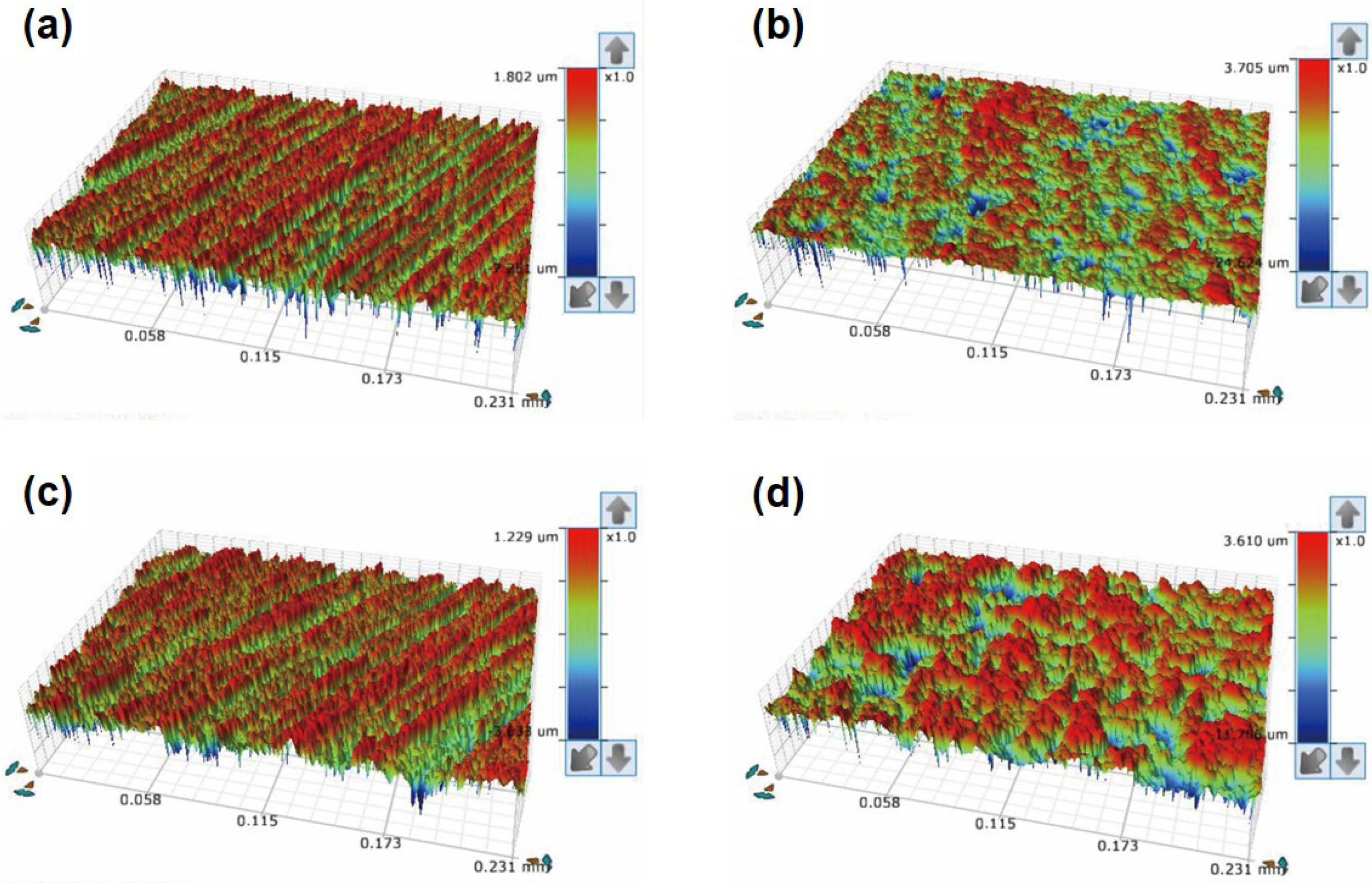
2.4. Roughness
2.5. Statistical Analysis
3. Results
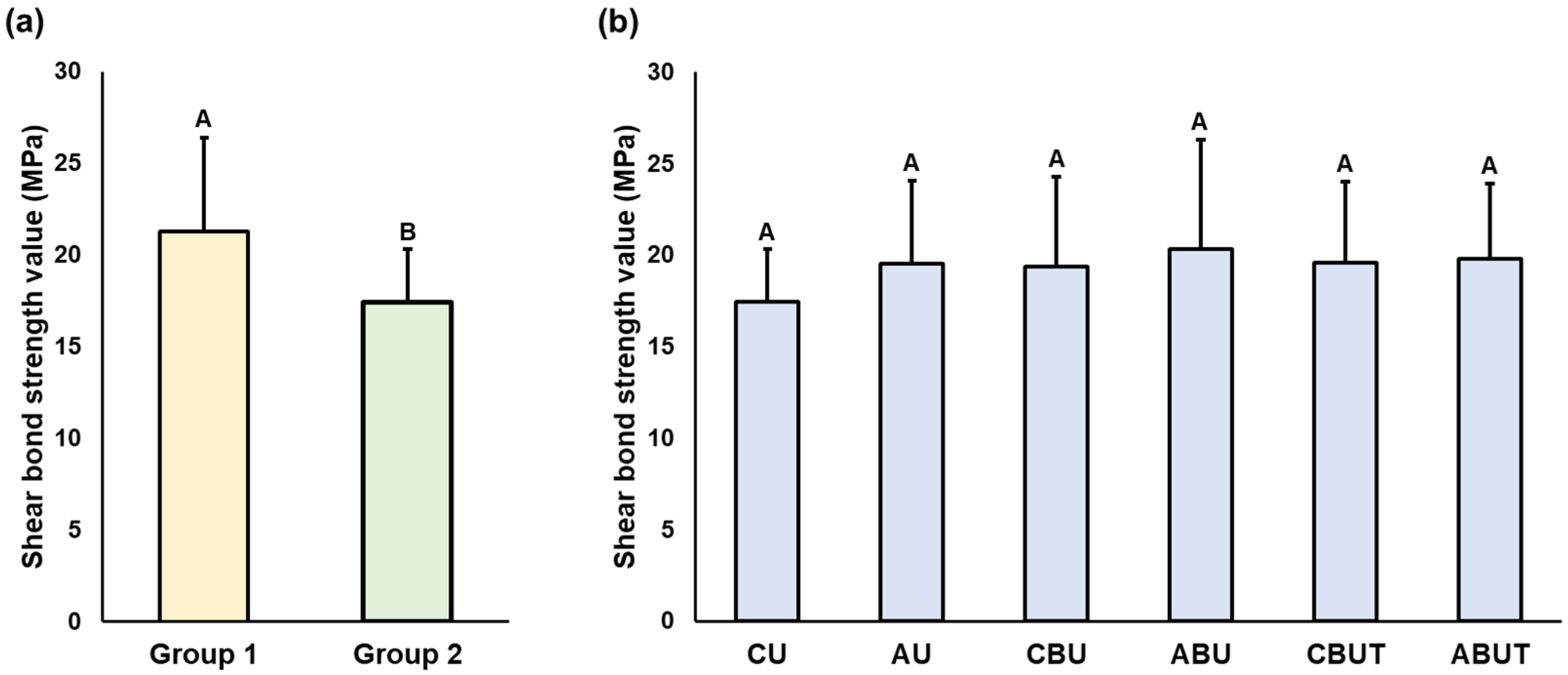
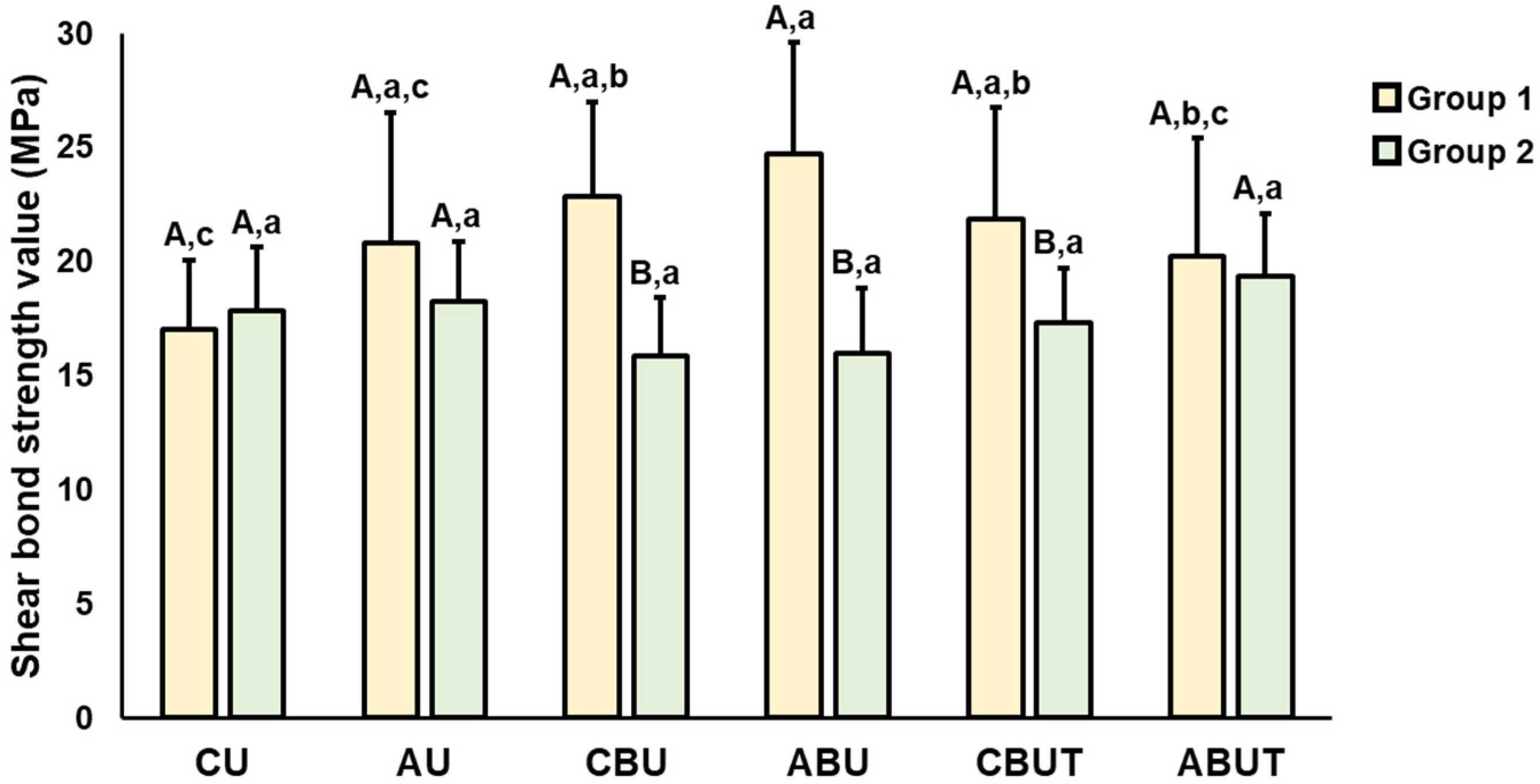
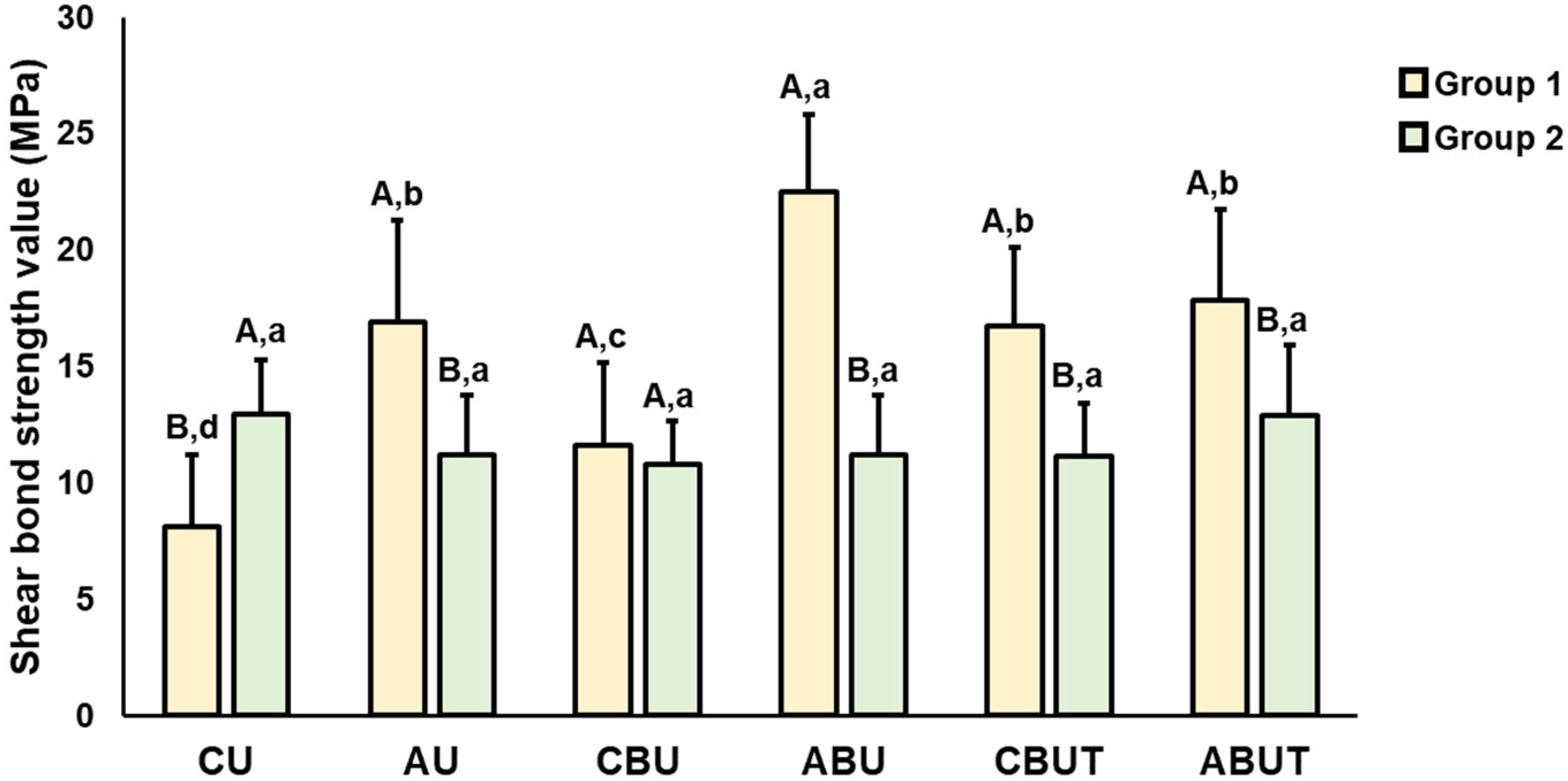
3.1. Shear Bond Strength
3.2. Scanning Electron Microscopy
3.3. Roughness
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Della Bona, A.; Cantelli, V.; Britto, V.T.; Collares, K.F.; Stansbury, J.W. 3D printing restorative materials using a stereolithographic technique: A systematic review. Dent. Mater. 2021, 37, 336–350. [Google Scholar] [CrossRef]
- Alshamrani, A.A.; Raju, R.; Ellakwa, A. Effect of printing layer thickness and postprinting conditions on the flexural strength and hardness of a 3d-printed resin. BioMed. Res. Int. 2022, 2022, 8353137. [Google Scholar] [CrossRef]
- Park, S.M.; Park, J.M.; Kim, S.K.; Heo, S.J.; Koak, J.Y. Flexural strength of 3d-printing resin materials for provisional fixed dental prostheses. Materials 2020, 13, 3970. [Google Scholar] [CrossRef]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3d printing technique and its challenges. Bioact. Mater. 2020, 5, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Abduo, J.; Lyons, K.; Bennamoun, M. Trends in computer-aided manufacturing in prosthodontics: A review of the available streams. Int. J. Dent. 2014, 2014, 783948. [Google Scholar] [CrossRef] [PubMed]
- Goodacre, B.J.; Goodacre, C.J. Additive manufacturing for complete denture fabrication: A narrative review. J. Prosthodont. 2022, 31, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Sayed, M.E.; Shetty, M.; Alqahtani, S.M.; Al Wadei, M.H.D.; Gupta, S.G.; Othman, A.A.A.; Alshehri, A.H.; Alqarni, H.; Mobarki, A.H.; et al. Physical and mechanical properties of 3d-printed provisional crowns and fixed dental prosthesis resins compared to cad/cam milled and conventional provisional resins: A systematic review and meta-analysis. Polymers 2022, 14, 2691. [Google Scholar] [CrossRef]
- Jeong, K.W.; Kim, S.H. Influence of surface treatments and repair materials on the shear bond strength of cad/cam provisional restorations. J. Adv. Prosthodont. 2019, 11, 95–104. [Google Scholar] [CrossRef]
- Sonkaya, E.; Kürklü, G.B. The effect of different surface treatments on the repair of 3d permanent resin restorations by composite resin different surface treatments and repair of 3d permanent resin. Res. Square 2022, 1–15. [Google Scholar] [CrossRef]
- Alharbi, N.; Alharbi, A.; Osman, R. Stain susceptibility of 3d-printed nanohybrid composite restorative material and the efficacy of different stain removal techniques: An in vitro study. Materials 2021, 14, 5621. [Google Scholar] [CrossRef]
- Berli, C.; Thieringer, F.M.; Sharma, N.; Müller, J.A.; Dedem, P.; Fischer, J.; Rohr, N. Comparing the mechanical properties of pressed, milled, and 3d-printed resins for occlusal devices. J. Prosthet. Dent. 2020, 124, 780–786. [Google Scholar] [CrossRef] [PubMed]
- Reymus, M.; Fabritius, R.; Keßler, A.; Hickel, R.; Edelhoff, D.; Stawarczyk, B. Fracture load of 3d-printed fixed dental prostheses compared with milled and conventionally fabricated ones: The impact of resin material, build direction, post-curing, and artificial aging-an in vitro study. Clin. Oral Investig. 2020, 24, 701–710. [Google Scholar] [CrossRef] [PubMed]
- Albahri, R.; Yoon, H.I.; Lee, J.D.; Yoon, S.; Lee, S.J. Shear bond strength of provisional repair materials bonded to 3d printed resin. J. Dent. Sci. 2021, 16, 261–267. [Google Scholar] [CrossRef]
- Lim, N.K.; Shin, S.Y. Bonding of conventional provisional resin to 3d printed resin: The role of surface treatments and type of repair resins. J. Adv. Prosthodont. 2020, 12, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Çulhaoğlu, A.K.; Özkır, S.E.; Şahin, V.; Yılmaz, B.; Kılıçarslan, M.A. Effect of various treatment modalities on surface characteristics and shear bond strengths of polyetheretherketone-based core materials. J. Prosthodont. 2020, 29, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Önöral, Ö.; Ongun, S.; Günal, B. Evaluation of surface characterization and mechanical features of resin-matrix ceramics before and after different surface treatments. J. Prosthet. Dent. 2022, 127, 928.e1–928.e8. [Google Scholar] [CrossRef]
- Sinha, N. Shear Bond Strength Characteristics on Surface Treatment Modalities of Cad-Cam Resin Based Core Materials. Master’s Thesis, Marquette University, Milwaukee, WI, USA, 2009. Volume 2021. p. 656. Available online: https://epublications.marquette.edu/theses_open/656 (accessed on 20 May 2021).
- Zhou, L.; Qian, Y.; Zhu, Y.; Liu, H.; Gan, K.; Guo, J. The effect of different surface treatments on the bond strength of peek composite materials. Dent. Mater. 2014, 30, e209–e215. [Google Scholar] [CrossRef]
- Uhrenbacher, J.; Schmidlin, P.R.; Keul, C.; Eichberger, M.; Roos, M.; Gernet, W.; Stawarczyk, B. The effect of surface modification on the retention strength of polyetheretherketone crowns adhesively bonded to dentin abutments. J. Prosthet. Dent. 2014, 112, 1489–1497. [Google Scholar] [CrossRef]
- Kömürcüoğlu, M.B.; Sağırkaya, E.; Tulga, A. Influence of different surface treatments on bond strength of novel cad/cam restorative materials to resin cement. J. Adv. Prosthodont. 2017, 9, 439–446. [Google Scholar] [CrossRef]
- Blatz, M.B.; Phark, J.H.; Ozer, F.; Mante, F.K.; Saleh, N.; Bergler, M.; Sadan, A. In vitro comparative bond strength of contemporary self-adhesive resin cements to zirconium oxide ceramic with and without air-particle abrasion. Clin. Oral Investig. 2010, 14, 187–192. [Google Scholar] [CrossRef]
- Cekic-Nagas, I.; Ergun, G.; Egilmez, F.; Vallittu, P.K.; Lassila, L.V. Micro-shear bond strength of different resin cements to ceramic/glass-polymer cad-cam block materials. J. Prosthodont. Res. 2016, 60, 265–273. [Google Scholar] [CrossRef]
- ISO 10477:2020; Dentistry—Polymer-Based Crown and Bridge Materials. 4th ed. International Standard Organization: Geneva, Switzerland, 2020.
- Stawarczyk, B.; Basler, T.; Ender, A.; Roos, M.; Özcan, M.; Hämmerle, C. Effect of surface conditioning with airborne-particle abrasion on the tensile strength of polymeric cad/cam crowns luted with self-adhesive and conventional resin cements. J. Prosthet. Dent. 2012, 107, 94–101. [Google Scholar] [CrossRef]
- Moon, J.-E.; Kim, S.-H.; Lee, J.-B.; Han, J.-S.; Yeo, I.-S.; Ha, S.-R. Effects of airborne-particle abrasion protocol choice on the surface characteristics of monolithic zirconia materials and the shear bond strength of resin cement. Ceram. Int. 2016, 42, 1552–1562. [Google Scholar] [CrossRef]
- Kurtulmus-Yilmaz, S.; Cengiz, E.; Ongun, S.; Karakaya, I. The effect of surface treatments on the mechanical and optical behaviors of cad/cam restorative materials. J. Prosthodont. 2019, 28, e496–e503. [Google Scholar] [CrossRef] [PubMed]
- Yoshihara, K.; Nagaoka, N.; Maruo, Y.; Nishigawa, G.; Irie, M.; Yoshida, Y.; Van Meerbeek, B. Sandblasting may damage the surface of composite cad-cam blocks. Dent. Mater. 2017, 33, e124–e135. [Google Scholar] [CrossRef]
- Blatz, M.B.; Chiche, G.; Holst, S.; Sadan, A. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 2007, 38, 745–753. [Google Scholar]
- Wolfart, M.; Lehmann, F.; Wolfart, S.; Kern, M. Durability of the resin bond strength to zirconia ceramic after using different surface conditioning methods. Dent. Mater. 2007, 23, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, M.; Vallittu, P.K. Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent. Mater. 2003, 19, 725–731. [Google Scholar] [CrossRef] [PubMed]
- Keul, C.; Liebermann, A.; Roos, M.; Uhrenbacher, J.; Stawarczyk, B. The effect of ceramic primer on shear bond strength of resin composite cement to zirconia: A function of water storage and thermal cycling. J. Am. Dent. Assoc. 2013, 144, 1261–1271. [Google Scholar] [CrossRef]
- Román-Rodríguez, J.L.; Fons-Font, A.; Amigó-Borrás, V.; Granell-Ruiz, M.; Busquets-Mataix, D.; Panadero, R.A.; Solá-Ruiz, M.F. Bond strength of selected composite resin-cements to zirconium-oxide ceramic. Med. Oral Patol. Oral Cir. Bucal. 2013, 18, e115–e123. [Google Scholar] [CrossRef]
- Amaral, R.; Ozcan, M.; Valandro, L.F.; Balducci, I.; Bottino, M.A. Effect of conditioning methods on the microtensile bond strength of phosphate monomer-based cement on zirconia ceramic in dry and aged conditions. J. Biomed. Mater. Res. B 2008, 85, 1–9. [Google Scholar] [CrossRef]
- Blank, J.T. Scientifically based rationale and protocol for use of modern indirect resin inlays and onlays. J. Esthet. Dent. 2000, 12, 195–208. [Google Scholar] [CrossRef] [PubMed]
- Fouquet, V.; Lachard, F.; Abdel-Gawad, S.; Dursun, E.; Attal, J.P.; François, P. Shear bond strength of a direct resin composite to cad-cam composite blocks: Relative contribution of micromechanical and chemical block surface treatment. Materials 2022, 15, 5018. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.-J.; Park, J.-K.; Son, S.-A. Shear bond strength between universal adhesives with various pH and dual-cured resin cements. Kor. J. Dent. Mater. 2018, 45, 301–309. [Google Scholar] [CrossRef]
- Kiomarsi, N.; Saburian, P.; Chiniforush, N.; Karazifard, M.J.; Hashemikamangar, S.S. Effect of thermocycling and surface treatment on repair bond strength of composite. J. Clin. Exp. Dent. 2017, 9, e945–e951. [Google Scholar] [CrossRef] [PubMed]
- Elsaka, S.E. Bond strength of novel cad/cam restorative materials to self-adhesive resin cement: The effect of surface treatments. J. Adhes. Dent. 2014, 16, 531–540. [Google Scholar] [CrossRef] [PubMed]
- Barutcigil, K.; Barutcigil, Ç.; Kul, E.; Özarslan, M.M.; Buyukkaplan, U.S. Effect of different surface treatments on bond strength of resin cement to a cad/cam restorative material. J. Prosthodont. 2019, 28, 71–78. [Google Scholar] [CrossRef]

| Product Name | Manufacturer | Composition |
|---|---|---|
| Tera Harz TC-80DP (A2) | Graphy, Seoul, Korea | Urethane dimethacrylate-based dental resin, phosphine oxides, and pigment |
| Permanent Crown (A2) | Formlabs, Somerville, MA, USA | Esterification products of 4,4′-isopropylidiphenol, ethoxylated and 2-methylprop-2enoic acid; ethoxylated bisphenol A dimethacrylate (Bis-EMA, methacrylate polymer), silanized dental glass, methyl benzoylformate, diphenyl (2,4,6-trimethylbenzoyl) phosphine oxide (TPO, photoinitiator), 30–50 wt.%—inorganic fillers (particle size 0.7 μm) |
| Single Bond Universal | 3M ESPE, St. Paul, MN, USA | MDP, dimethacrylate resins, HEMA, Vitrebond copolymer, filler, ethanol, water, initiators, and silane |
| RelyX U200 | 3M ESPE, St. Paul, MN, USA | Base: methacrylate monomers containing phosphoric acid groups, methacrylate monomers, silanated fillers, initiator components, stabilizers, and rheological additives Catalyst: methacrylate monomers, alkaline fillers, silanated fillers, initiator components, stabilizers, pigments, and rheological additives |
| RelyX Ultimate | 3M ESPE, St. Paul, MN, USA | Base: methacrylate monomers, silanated fillers, initiator components, stabilizers, rheological additives Catalyst: methacrylate monomers, alkaline fillers, silanated fillers, initiator components, stabilizers, pigments, rheological additives, fluorescence dye, and dark cure activator for Scotchbond Universal adhesive |
| Cobra Aluoxyd | Renfert GmbH, Hilzinger, Germany | 50 µm aluminum oxide |
| Group | Procedure |
|---|---|
| CU | Control + U200 |
| AU | APA + U200 |
| CBU | Control + SBU + U200 |
| ABU | APA + SBU + U200 |
| CBUT | Control + SBU + Ultimate |
| ABUT | APA + SBU + Ultimate |
| CU | AU | CBU | ABU | CBUT | ABUT | ||
|---|---|---|---|---|---|---|---|
| Group 1 | Before thermocycling | 17.0 ± 3.0 A | 20.8 ± 5.7 A | 22.9 ± 4.2 A | 24.7 ± 4.9 A | 21.9 ± 4.9 A | 20.2 ± 5.2 A |
| After thermocycling | 8.1 ± 3.1 B | 16.9 ± 4.3 A | 11.6 ± 3.6 B | 22.5 ± 3.3 A | 16.8 ± 3.3 B | 17.8 ± 3.9 A | |
| Group 2 | Before thermocycling | 17.9 ± 2.8 A | 18.2 ± 2.6 A | 15.9 ± 2.6 A | 16.0 ± 2.8 A | 17.3 ± 2.4 A | 19.4 ± 2.7 A |
| After thermocycling | 12.9 ± 2.3 B | 11.2 ± 2.6 B | 10.8 ± 1.8 B | 11.2 ± 2.6 B | 11.2 ± 2.3 B | 12.9 ± 3.0 B |
| Control | APA | |
|---|---|---|
| Group 1 | 0.41 ± 0.04 A,a | 0.79 ± 0.05 A,b |
| Group 2 | 0.40 ± 0.04 A,a | 1.00 ± 0.06 B,b |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kang, Y.-J.; Park, Y.; Shin, Y.; Kim, J.-H. Effect of Adhesion Conditions on the Shear Bond Strength of 3D Printing Resins after Thermocycling Used for Definitive Prosthesis. Polymers 2023, 15, 1390. https://doi.org/10.3390/polym15061390
Kang Y-J, Park Y, Shin Y, Kim J-H. Effect of Adhesion Conditions on the Shear Bond Strength of 3D Printing Resins after Thermocycling Used for Definitive Prosthesis. Polymers. 2023; 15(6):1390. https://doi.org/10.3390/polym15061390
Chicago/Turabian StyleKang, You-Jung, Yeseul Park, Yooseok Shin, and Jee-Hwan Kim. 2023. "Effect of Adhesion Conditions on the Shear Bond Strength of 3D Printing Resins after Thermocycling Used for Definitive Prosthesis" Polymers 15, no. 6: 1390. https://doi.org/10.3390/polym15061390
APA StyleKang, Y.-J., Park, Y., Shin, Y., & Kim, J.-H. (2023). Effect of Adhesion Conditions on the Shear Bond Strength of 3D Printing Resins after Thermocycling Used for Definitive Prosthesis. Polymers, 15(6), 1390. https://doi.org/10.3390/polym15061390









