Comparison of Bulk Polymeric Resin Composite and Hybrid Glass Ionomer Cement in Adhesive Class I Dental Restorations: A 3D Finite Element Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Generation of Solid Models
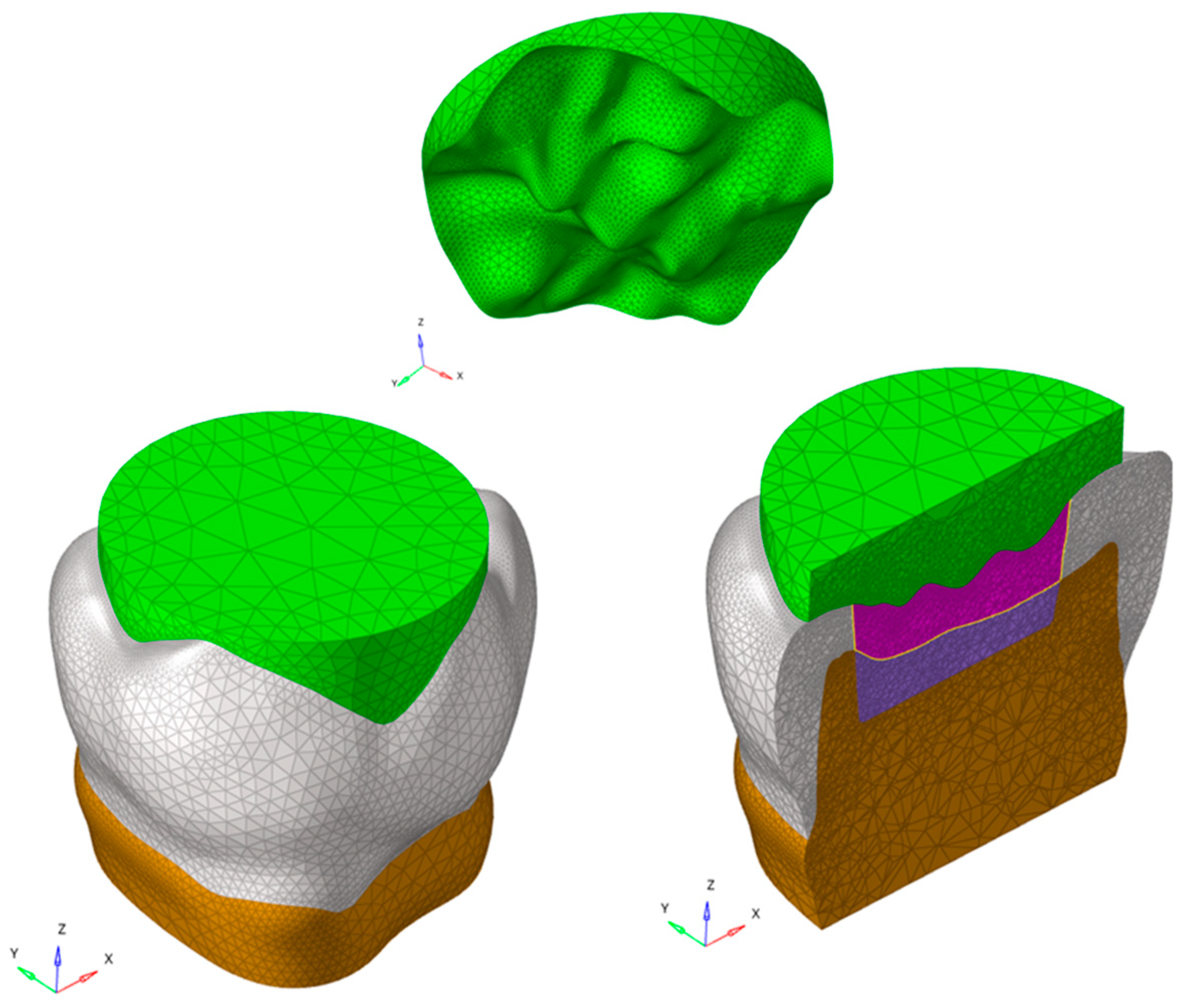
2.2. Numerical Simulation
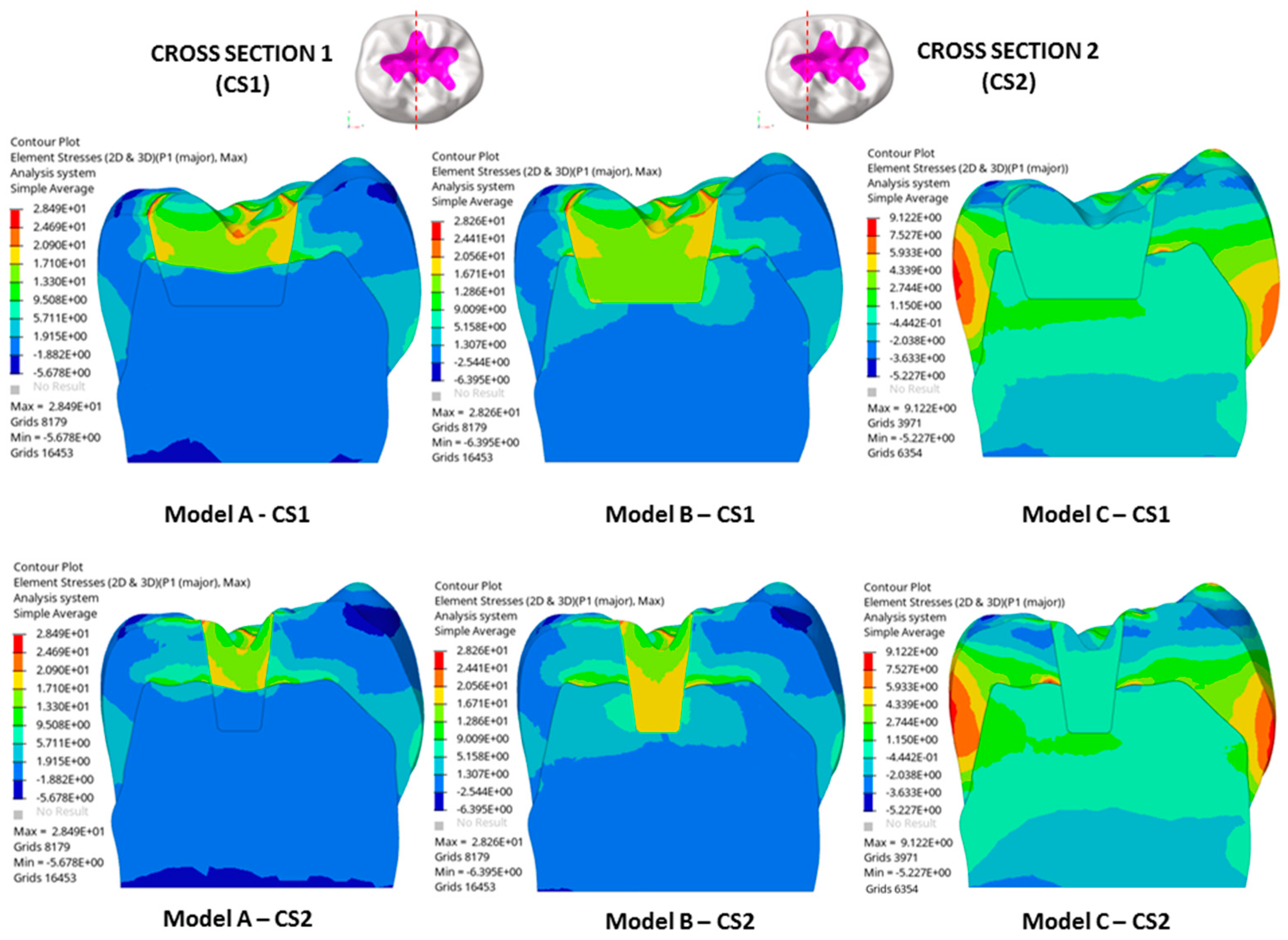
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Osiewicz, M.A.; Werner, A.; Roeters, F.J.M.; Kleverlaan, C.J. Wear of bulk-fill resin composites. Dent. Mater. 2022, 38, 549–553. [Google Scholar] [CrossRef] [PubMed]
- Heintze, S.D.; Loguercio, A.D.; Hanzen, T.A.; Reis, A.; Rousson, V. Clinical efficacy of resin-based direct posterior restorations and glass-ionomer restorations—An updated meta-analysis of clinical outcome parameters. Dent. Mater. 2022, 38, e109–e135. [Google Scholar] [CrossRef]
- Van Ende, A.; De Munck, J.; Lise, D.P.; Van Meerbeek, B. Bulk-fill composites: A review of the current literature. J. Adhes. Dent. 2017, 19, 95–109. [Google Scholar]
- Ausiello, P.; Dal Piva, A.M.d.O.; Borges, A.L.S.; Lanzotti, A.; Zamparini, F.; Epifania, E.; Mendes Tribst, J.P. Effect of Shrinking and No Shrinking Dentine and Enamel Replacing Materials in Posterior Restoration: A 3D-FEA Study. Appl. Sci. 2021, 11, 2215. [Google Scholar] [CrossRef]
- Gonçalves, F.; Campos, L.M.d.P.; Rodrigues-Júnior, E.C.; Costa, F.V.; Marques, P.A.; Francci, C.E.; Braga, R.R.; Boaro, L.C.C. A comparative study of bulk-fill composites: Degree of conversion, post-gel shrinkage and cytotoxicity. Braz. Oral Res. 2018, 32, e17. [Google Scholar] [CrossRef]
- Schneider, T.R.; Hakami-Tafreshi, R.; Tomasino-Perez, A.; Tayebi, L.; Lobner, D. Effects of dental composite resin monomers on dental pulp cells. Dent. Mater. J. 2019, 38, 579–583. [Google Scholar] [CrossRef]
- Treglia, A.S.; Turco, S.; Ulianich, L.; Ausiello, P.; Lofrumento, D.D.; Nicolardi, G.; Miele, C.; Garbi, C.; Beguinot, F.; Di Jeso, B. Cell fate following ER stress: Just a matter of "quo ante" recovery or death? Histol. Histopathol. 2012, 27, 1–12. [Google Scholar]
- Tou, G.A.; dos A Gomes, J.M.; Rinco, L.S.d.O.; Yamauti, M.; Diniz, I.M.A.; Pires, F.; Schmidt, M.E.P.; Menezes, H.C.; Cardeal, Z.L.; Bottoli, C.B.G.; et al. Release of leachable products from resinous compounds in the saliva of children with anterior open bite treated with spur. J. Appl. Oral. Sci. 2022, 30, e20220227. [Google Scholar] [CrossRef] [PubMed]
- Marzouk, T.; Sathyanarayana, S.; Kim, A.S.; Seminario, A.L.; McKinney, C.M. A systematic review of exposure to bisphenol A from dental treatment. JDR Clin. Trans. Res. 2019, 4, 106–115. [Google Scholar] [CrossRef]
- De Nys, S.; Duca, R.C.; Vervliet, P.; Covaci, A.; Boonen, I.; Elskens, M.; Vanoirbeek, J.; Godderis, L.; Van Meerbeek, B.; Van Landuyt, K.L. Bisphenol A as degradation product of monomers used in resin-based dental materials. Dent. Mater. 2021, 37, 1020–1029. [Google Scholar] [CrossRef]
- Ausiello, P.; Dal Piva, A.M.d.O.; di Lauro, A.E.; Garcia-Godoy, F.; Testarelli, L.; Tribst, J.P.M. Mechanical behavior of Alkasite posterior restorations in comparison to polymeric materials: A 3D-FEA study. Polymers 2022, 14, 1502. [Google Scholar] [CrossRef] [PubMed]
- Moshaverinia, M.; de Almeida Queiroz Ferreira, L.; Smidt, G.; Shah, K.C.; Ansari, S.; Moshaverinia, A. Evaluation of mechanical, optical, and fluoride-releasing properties of a translucent bulk fill glass hybrid restorative dental material. J. Esthet. Restor. Dent. 2024, 36, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Giordano, M.; Ausiello, P.; Martorelli, M.; Sorrentino, R. Reliability of computer designed surgical guides in six implant rehabilitations with two years follow-up. Dent. Mater. 2012, 28, e168–e177. [Google Scholar] [CrossRef]
- Romanyk, D.L.; Vafaeian, B.; Addison, O.; Adeeb, S. The use of finite element analysis in dentistry and orthodontics: Critical points for model development and interpreting results. Semin. Orthodontics 2020, 26, 162–173. [Google Scholar] [CrossRef]
- Tribst, J.P.M.; de Morais, D.C.; de Matos, J.D.M.; Martorelli, M.; Ausiello, P. Influence of Framework Material and Posterior Implant Angulation in Full-Arch All-on-4 Implant-Supported Prosthesis Stress Concentration. Dent. J. 2022, 10, 12. [Google Scholar] [CrossRef]
- Williams, S.H.; Wright, B.W.; den Truong, V.; Daubert, C.R.; Vinyard, C.J. Mechanical properties of foods used in experimental studies of primate masticatory function. Am. J. Primatol. 2005, 67, 329–346. [Google Scholar] [CrossRef] [PubMed]
- Kowalczyk, P. Influence of the shape of the layers in photo-cured dental restorations on the shrinkage stress peaks-FEM study. Dent. Mater. 2009, 25, e83–e91. [Google Scholar] [CrossRef]
- Juloski, J.; Apicella, D.; Ferrari, M. The effect of ferrule height on stress distribution within a tooth restored with fiber posts and ceramic crown: A finite element analysis. Dent. Mater. 2014, 30, 1304–1315. [Google Scholar] [CrossRef]
- Natali, A.N.; Carniel, E.L.; Pavan, P.G. Modelling of mandible bone properties in the numerical analysis of oral implant biomechanics. Comput. Methods Programs Biomed. 2010, 100, 158–165. [Google Scholar] [CrossRef]
- Burke, F.T.; Mackenzie, L.; Sands, P. Are the latest GICs suitable for restoring back teeth. Dent. Update 2023, 50, 437–446. [Google Scholar] [CrossRef]
- Tavangar, M.; Sadeghi, Y.; Mihandoust, S.; Darabi, F.; Monir, A.S.; Soltani, S.; Davalloo, R.T. Comparison of Stress Distribution in MOD Premolars Restored with Two Low Shrinkage Resin Composites Using Finite Element Analysis. J. Dentomaxillofacial Radiol. 2023, 12, 9–17. [Google Scholar]
- Aregawi, W.A.; Fok, A.S.L. Shrinkage stress and cuspal deflection in MOD restorations: Analytical solutions and design guidelines. Dent. Mater. 2021, 37, 783–795. [Google Scholar] [CrossRef] [PubMed]
- Matuda, A.G.N.; Silveira, M.P.M.; de Andrade, G.S.; Piva, A.M.d.O.D.; Tribst, J.P.M.; Borges, A.L.S.; Testarelli, L.; Mosca, G.; Ausiello, P. Computer aided design modelling and finite element analysis of premolar proximal cavities restored with resin composites. Materials 2021, 14, 2366. [Google Scholar] [CrossRef] [PubMed]
- Justen, M.; Scheck, D.; Münchow, E.A.; Jardim, J.J. Is Cention-N comparable to other direct dental restorative materials? A systematic review with network meta-analysis of in vitro studies. Dent. Mater. 2024, 40, 1341–1352. [Google Scholar] [CrossRef]
- Alsari, A.; Ghilotti, J.; Sanz, J.L.; Llena, C.; Folguera, S.; Melo, M. Comparative evaluation of the microleakage of glass ionomers as restorative materials: A Systematic Review of in vitro studies. Appl. Sci. 2024, 14, 1729. [Google Scholar] [CrossRef]
- Zheng, L.; Zhang, Y.; Bai, Y.; Zhang, Z.; Wu, Q. Study on the mechanical and aging properties of an antibacterial composite resin loaded with fluoride-doped nano-zirconia fillers. Front. Bioeng. Biotechnol. 2024, 12, 1397459. [Google Scholar] [CrossRef]
- Mulgaonkar, A.; De Ataide, I.D.; Fernandes, M.; Lambor, R. Shear bond strength evaluation of an alkasite restorative material to three different liners with and without using adhesive system: An: In vitro: Study. J. Conserv. Dent. Endod. 2021, 24, 278–282. [Google Scholar] [CrossRef]
- Hua, W.; Li, J.; Zhu, Z.; Li, A.; Huang, J.; Gan, Z.; Dong, S. A review of mixed mode I-II fracture criteria and their applications in brittle or quasi-brittle fracture analysis. Theor. Appl. Fract. Mech. 2023, 124, 103741. [Google Scholar] [CrossRef]
- Ibrahim, H.A.; Abdalla, A.I.; El-Sayed, H.Y. Clinical study of different composite resin systems in Class I cavities (an 18-month randomized clinical trial). Braz. Dent. Sci. 2023, 26, e3737. [Google Scholar] [CrossRef]
- Sengupta, A.; Naka, O.; Mehta, S.B.; Banerji, S. The clinical performance of bulk-fill versus the incremental layered application of direct resin composite restorations: A systematic review. Evid. Based Dent. 2023, 24, 143. [Google Scholar] [CrossRef]
- Francesco, P.; Gabriele, C.; Fiorillo, L.; Giuseppe, M.; Antonella, S.; Giancarlo, B.; Mirta, P.; Mendes Tribst, J.P.; Lo Giudice, R. The use of bulk fill resin-based composite in the sealing of cavity with margins in radicular cementum. Eur. J. Dent. 2022, 16, 1–13. [Google Scholar] [CrossRef]
- Rosado, L.P.; Münchow, E.A.; De Oliveira, E.L.; Lacerda-Santos, R.; Freitas, D.Q.; Carlo, H.L.; Verner, F.S. Translucency and Radiopacity of Dental Resin Composites-Is There a Direct Relation. Oper. Dent. 2023, 48, e61–e69. [Google Scholar] [CrossRef]
- Furtado, M.D.; Immich, F.; Da Rosa, W.L.; Piva, E.; Da Silva, A.F. Repair of aged restorations made in direct resin composite—A systematic review. Int. J. Adhes. Adhes. 2023, 124, 103367. [Google Scholar] [CrossRef]
- Pai, S.; Bhat, V.; Patil, V.; Naik, N.; Awasthi, S.; Nayak, N. Numerical three-dimensional finite element modeling of cavity shape and optimal material selection by analysis of stress distribution on class V cavities of mandibular premolars. J. Int. Soc. Prev. Community Dent. 2020, 10, 279–285. [Google Scholar] [PubMed]
- Miletić, I.; Baraba, A.; Basso, M.; Pulcini, M.G.; Marković, D.; Perić, T.; Ozkaya, C.A.; Turkun, L.S. Clinical performance of a glass-hybrid system compared with a resin composite in the posterior region: Results of a 2-year multicenter study. J. Adhes. Dent. 2020, 22, 235–247. [Google Scholar]
- Asadian, F.; Shahidi, Z.; Moradi, Z. Evaluation of wear properties of four bulk-fill composites: Attrition, erosion, and abrasion. Biomed. Res. Int. 2021, 2021, 8649616. [Google Scholar] [CrossRef] [PubMed]
- Santos, M.J.M.C.; Leon, L.; Siddique, I.; Butler, S. Retrospective clinical evaluation of RMGIC/GIC Class V restorations. Dent. J. 2023, 11, 225. [Google Scholar] [CrossRef] [PubMed]
- Crins, L.A.M.J.; Opdam, N.J.M.; Huysmans, M.C.D.N.J.M.; Zhang, Y.; Loomans, B.A.C. An in vitro evaluation of the fatigue behavior of resin composite materials as part of a translational research cycle. Dent. Mater. 2024, 40, 1409–1416. [Google Scholar] [CrossRef]
- Chang, Y.; Tambe, A.A.; Maeda, Y.; Wada, M.; Gonda, T. Finite element analysis of dental implants with validation: To what extent can we expect the model to predict biological phenomena? A literature review and proposal for classification of a validation process. Int. J. Implant. Dent. 2018, 4, 7. [Google Scholar] [CrossRef]
- Kang, K.S.; Park, K.M.; Ahn, J.W.; Jo, M.Y.; Oh, Y.R.; Youn, J.H.; Lee, J.W.; Je, D.Y.; Jung, T.G. Validation of the Finite Element Model versus Biomechanical Assessments of Dental Implants and Total Knee Replacements. Bioengineering 2023, 10, 1365. [Google Scholar] [CrossRef]
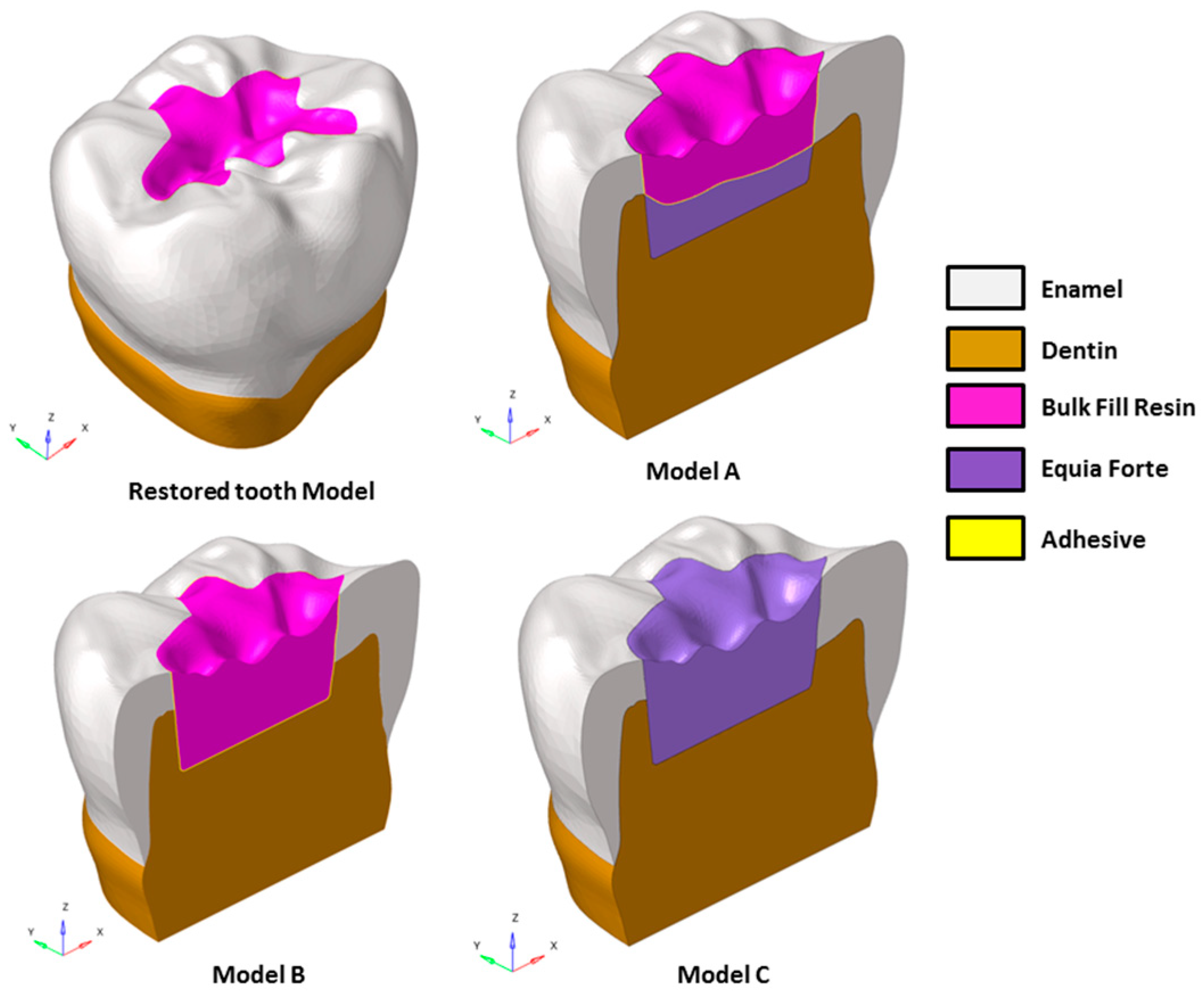


| Model | Adhesive Layer | Restorative Lower Layer | Restorative Upper Layer | Single Restorative Material |
|---|---|---|---|---|
| A | 10 µm thick (only around restorative upper layer) | Equia Forte HT (about 1.45 mm thick and 20 mm3 volume) | Bulk fill resin composite (about 2.5 mm thick and 33 mm3 volume) | - |
| B | 10 µm thick | - | - | Bulk fill resin composite (about 4 mm and 53 mm3 volume) |
| C | - | - | - | Equia Forte HT (about 4 mm and 53 mm3 volume) |
| Material | Young’s Modulus (GPa) | Poisson’s Ratio | Linear Shrinkage Ratio (%) |
|---|---|---|---|
| Dentin | 18.00 | 0.23 | -- |
| Enamel | 80.00 | 0.30 | -- |
| Food (apple pulp) | 3.41 | 0.1 | -- |
| Adhesive layer | 4.00 | 0.30 | 1.0 |
| Bulk fill composite | 12.00 | 0.25 | 1.0 |
| Equia Forte HT | 6.27 | 0.25 | -- |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
di Lauro, A.E.; Ciaramella, S.; Tribst, J.P.M.; Aliberti, A.; Ausiello, P. Comparison of Bulk Polymeric Resin Composite and Hybrid Glass Ionomer Cement in Adhesive Class I Dental Restorations: A 3D Finite Element Analysis. Polymers 2024, 16, 2525. https://doi.org/10.3390/polym16172525
di Lauro AE, Ciaramella S, Tribst JPM, Aliberti A, Ausiello P. Comparison of Bulk Polymeric Resin Composite and Hybrid Glass Ionomer Cement in Adhesive Class I Dental Restorations: A 3D Finite Element Analysis. Polymers. 2024; 16(17):2525. https://doi.org/10.3390/polym16172525
Chicago/Turabian Styledi Lauro, Alessandro E., Stefano Ciaramella, João P. Mendes Tribst, Angelo Aliberti, and Pietro Ausiello. 2024. "Comparison of Bulk Polymeric Resin Composite and Hybrid Glass Ionomer Cement in Adhesive Class I Dental Restorations: A 3D Finite Element Analysis" Polymers 16, no. 17: 2525. https://doi.org/10.3390/polym16172525






