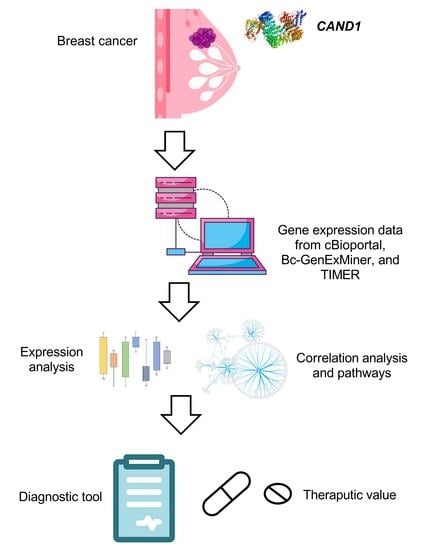
Bioinformatics Analysis of the Prognostic Significance of CAND1 in ERα-Positive Breast Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Investigating CAND1 mRNA Expression in Breast Cancer Tissue and Normal Breast Tissue
2.2. Kaplan–Meier Survival Curve Analysis
2.3. The Infiltration of Immune Cells
2.4. The Correlation between CAND1 mRNA and Neoplasm Histologic Grades, Hormone Therapy, and Lymph Nodes in ERα-Positive Breast Cancer Patients
2.5. Identification of Genes That Correlate with CAND1 in ERα-Positive Breast Cancer Patients
2.6. Association of Genes That Correlate with CAND1 in ERα-Positive Breast Cancer with Signaling Pathways
2.7. Statistical Analysis
3. Results
3.1. CAND1 mRNA Is Upregulated in ERα-Positive Breast Cancer Patients Compared to Tumor-Adjacent and Normal Breast Tissue
3.2. CAND1 mRNA Expression Correlates with Poor Prognosis in ERα-Positive Breast Cancer Patients
3.3. CAND1 Correlates Negatively with Various Gene Markers of Immune Cells in ERα-Positive Breast Cancer Patients
3.4. CAND1 mRNA Positively Correlates with Neoplasm Histologic Grades, Hormone Therapy, and Lymph Nodes in ERα-Positive Breast Cancer Patients
3.5. Identifying Genes That Positively Correlate with CAND1 in ERα-Positive Breast Cancer Patients
3.6. Genes That Correlate with CAND1 in ERα-Positive Breast Cancer Patients Are Involved in the Activation of the Androgen and Estrogen Signaling Pathways
4. Discussion
5. Conclusions
Supplementary Materials
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chua, Y.; Boh, B.; Ponyeam, W.; Hagen, T. Regulation of cullin RING E3 ubiquitin ligases by CAND1 in vivo. PLoS ONE 2011, 6, 16071. [Google Scholar] [CrossRef] [PubMed]
- Bosu, D.; Kipreos, T. Cullin-RING ubiquitin ligases: Global regulation and activation cycles. Cell Div. 2008, 3, 7. [Google Scholar] [CrossRef] [PubMed]
- Helmstaedt, K.; Schwier, E.; Christmann, M.; Nahlik, K.; Westermann, M.; Harting, R.; Grond, S.; Busch, S.; Braus, G. Recruitment of the inhibitor Cand1 to the cullin substrate adaptor site mediates interaction to the neddylation site. Mol. Biol. Cell 2011, 22, 153–164. [Google Scholar] [CrossRef] [PubMed]
- Bennett, E.; Rush, J.; Gygi, S.; Harper, J. Dynamics of Cullin-RING Ubiquitin Ligase Network Revealed by Systematic Quantitative Proteomics. Cell 2010, 143, 951–965. [Google Scholar] [CrossRef]
- Lydeard, J.; Schulman, B.; Harper, J. Building and remodelling Cullin–RING E3 ubiquitin ligases. EMBO Rep. 2013, 14, 1050–1061. [Google Scholar] [CrossRef]
- Soucy, T.; Smith, P.; Rolfe, M. Targeting NEDD8-Activated Cullin-RING Ligases for the Treatment of Cancer. Clin. Cancer Res. 2009, 15, 3912–3916. [Google Scholar] [CrossRef]
- Fouad, S.; Wells, O.; Hill, M.; D’Angiolella, V. Cullin Ring Ubiquitin Ligases (CRLs) in Cancer: Responses to Ionizing Radiation (IR) Treatment. Front. Physiol. 2019, 10, 1144. Available online: https://www.frontiersin.org/articles/10.3389/fphys.2019.01144 (accessed on 1 September 2022). [CrossRef]
- Genschik, P.; Sumara, I.; Lechner, E. The emerging family of CULLIN3-RING ubiquitin ligases (CRL3s): Cellular functions and disease implications. EMBO J. 2013, 17, 2307–2320. [Google Scholar] [CrossRef]
- Diaz, S.; Wang, K.; Sjögren, B.; Liu, X. Roles of Cullin-RING Ubiquitin Ligases in Cardiovascular Diseases. Biomolecules 2022, 12, 416. [Google Scholar] [CrossRef]
- Qi, J.; Ronai, Z. Dysregulation of ubiquitin ligases in cancer. Drug Resist. Updat. Rev. Comment. Antimicrob. Anticancer Chemother. 2015, 23, 1–11. [Google Scholar] [CrossRef]
- Wang, Y.; Dai, J.; Zeng, Y.; Guo, J.; Lan, J. E3 Ubiquitin Ligases in Breast Cancer Metastasis: A Systematic Review of Pathogenic Functions and Clinical Implications. Front. Oncol. 2021, 11, 752604. [Google Scholar] [CrossRef] [PubMed]
- Iskandar, A.; Zulkifli, N.; Ahmad, M.; Das, K.; Zulkifle, N. OTUB1 expression and interaction network analyses in MCF-7 breast cancer cells. Gene Rep. 2021, 24, 101273. [Google Scholar] [CrossRef]
- Murata, T.; Takayama, K.; Urano, T.; Horie-Inoue, K.; Ikeda, K.; Takahashi, S.; Kawazu, C.; Hasegawa, A.; Ouchi, Y.; Homma, Y.; et al. miR-148a is an androgen-responsive microRNA that promotes LNCaP prostate cell growth by repressing its target CAND1 expression. Prostate Cancer Prostatic Dis. 2010, 13, 356–361. [Google Scholar] [CrossRef] [PubMed]
- Korzeniewski, N.; Hohenfellner, M.; Duensing, S. CAND1 Promotes PLK4-Mediated Centriole Overduplication and Is Frequently Disrupted in Prostate Cancer. Neoplasia 2012, 14, 799–806. [Google Scholar] [CrossRef] [PubMed]
- Eigentler, A.; Tymoszuk, P.; Zwick, J.; Schmitz, A.; Pircher, A.; Kocher, F.; Schlicker, A.; Lesche, R.; Schafer, G.; Theurl, I.; et al. The Impact of Cand1 in Prostate Cancer. Cancers 2020, 12, 428. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.; Li, Y.; Zhao, Y.; He, S.; Shi, J. miR-33a inhibits cell proliferation and invasion by targeting CAND1 in lung cancer. Clin. Transl. Oncol. 2018, 20, 457–466. [Google Scholar] [CrossRef] [PubMed]
- Che, Z.; Liu, F.; Zhang, W.; Mcgrath, M.; Hou, D.; Chen, P.; Song, C.; Yang, D. Targeting CAND1 promotes caspase-8/RIP1-dependent apoptosis in liver cancer cells. Am. J. Transl. Res. 2018, 10, 1357–1372. [Google Scholar]
- Lv, Z.; Bao, B.; Liang, P. Screening and Authentication of Key Genes and Prognostic Value Analysis in Oligodendroglial Tumor. Res. Square 2020. [Google Scholar] [CrossRef]
- Qian, T.; Zhao, L.; Wang, J.; Li, P.; Qin, J.; Liu, Y.; Yu, B.; Ding, F.; Gu, X.; Zhou, S. miR-148b-3p promotes migration of Schwann cells by targeting cullin-associated and neddylation-dissociated 1. Neural Regen. Res. 2016, 11, 1001–1005. [Google Scholar] [CrossRef]
- Dai, W.; He, J.; Zheng, L.; Bi, M.; Hu, F.; Chen, M.; Niu, H.; Yang, J.; Luo, Y.; Tang, W.; et al. miR-148b-3p, miR-190b, and miR-429 Regulate Cell Progression and Act as Potential Biomarkers for Breast Cancer. J. Breast Cancer 2019, 22, 219–236. [Google Scholar] [CrossRef]
- Dorraki, N.; Ghale-Noie, Z.; Ahmadi, N.; Keyvani, V.; Bahadori, R.; Nejad, A.; Aschner, M.; Pourghadamya, H.; Mollazadeh, S.; Mirzaei, H. miRNA-148b and its role in various cancers. Epigenomics 2021, 13, 1939–1960. [Google Scholar] [CrossRef] [PubMed]
- Jézéquel, P.; Gouraud, W.; Azzouz, F.; Guerin-Charbonnel, C.; Juin, P.; Lasla, H.; Campone, M. Bc-GenExMiner 4.5: New mining module computes breast cancer differential gene expression analyses. Database 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Li, T.; Fu, J.; Zeng, Z.; Cohen, D.; Li, J.; Chen, Q.; Liu, X. TIMER2.0 for analysis of tumor-infiltrating immune cells. Nucleic Acids Res. 2020, 48, W509–W514. [Google Scholar] [CrossRef] [PubMed]
- Győrffy, B. Survival analysis across the entire transcriptome identifies biomarkers with the highest prognostic power in breast cancer. Comput. Struct. Biotechnol. J. 2021, 19, 4101–4109. [Google Scholar] [CrossRef]
- Li, Q.; Birkbak, N.; Gyorffy, B.; Szallasi, Z.; Eklund, A. Jetset: Selecting the optimal microarray probe set to represent a gene. BMC Bioinform. 2011, 12, 474. [Google Scholar] [CrossRef]
- Tang, Z.; Kang, B.; Li, C.; Chen, T.; Zhang, Z. GEPIA2: An enhanced web server for large-scale expression profiling and interactive analysis. Nucleic Acids Res. 2019, 47, W556–W560. [Google Scholar] [CrossRef]
- Cerami, E.; Gao, J.; Dogrusoz, U.; Gross, B.; Sumer, S.; Aksoy, B.; Jacobsen, A.; Byrne, C.; Heuer, M.; Larsson, E.; et al. The cBio Cancer Genomics Portal: An Open Platform for Exploring Multidimensional Cancer Genomics Data. Cancer Discov. 2017, 7, 736–740. [Google Scholar] [CrossRef]
- Cereda, M.; Gambardella, G.; Benedetti, L.; Iannelli, F.; Patel, D.; Basso, G.; Guerra, R.; Mourikis, T.; Puccio, I.; Sinha, S.; et al. Patients with genetically heterogeneous synchronous colorectal cancer carry rare damaging germline mutations in immune-related genes. Nat. Commun. 2016, 7, 12072. [Google Scholar] [CrossRef]
- Liu, C.; Hu, F.; Xia, M.; Han, L.; Zhang, Q.; Guo, A. GSCALite: A web server for gene set cancer analysis. Bioinformatics 2018, 34, 3771–3772. [Google Scholar] [CrossRef]
- Manuel, M.; Tredan, O.; Bachelot, T.; Clapisson, G.; Courtier, A.; Parmentier, G.; Rabeony, T.; Grives, A.; Perez, S.; Mouret, J.; et al. Lymphopenia combined with low TCR diversity (divpenia) predicts poor overall survival in metastatic breast cancer patients. Oncoimmunology 2012, 1, 432–440. [Google Scholar] [CrossRef]
- Adams, S.; Gray, R.; Demaria, S.; Goldstein, L.; Perez, E.; Shulman, L.; Martino, S.; Wang, M.; Jones, V.; Saphner, T.; et al. Prognostic value of tumor-infiltrating lymphocytes in triple-negative breast cancers from two phase III randomized adjuvant breast cancer trials: ECOG 2197 and ECOG 1199. J. Clin. Oncol. Off. J. Am. Soc. 2014, 32, 2959–2966. [Google Scholar] [CrossRef] [PubMed]
- Ali, H.; Chlon, L.; Pharoah, P.; Markowetz, F.; Caldas, C. Patterns of Immune Infiltration in Breast Cancer and Their Clinical Implications: A Gene-Expression-Based Retrospective Study. PLoS Med. 2016, 13, e1002194. [Google Scholar] [CrossRef]
- Rezaul, K.; Thumar, J.; Lundgren, D.; Eng, J.; Claffey, K.; Wilson, L.; Han, D. Differential Protein Expression Profiles in Estrogen Receptor–Positive and –Negative Breast Cancer Tissues Using Label-Free Quantitative Proteomics. Genes Cancer 2010, 1, 251–271. [Google Scholar] [CrossRef] [PubMed]
- Mamoor, S. A single nucleotide variant on chromosome 12 residing within CAND1 distinguishes patients with luminal B breast cancer. OSF Preprints 2022. [Google Scholar] [CrossRef]
- Reichermeier, K.; Straube, R.; Reitsma, J.; Sweredoski, M.; Rose, C.; Moradian, A.; Besten, W.; Hinkle, T.; Verschueren, E.; Petzold, G.; et al. PIKES Analysis Reveals Response to Degraders and Key Regulatory Mechanisms of the CRL4 Network. Mol. Cell. 2020, 77, 1092–1106.e9. [Google Scholar] [CrossRef]
- Liu, A.; Zhang, S.; Shen, Y.; Lei, R.; Wang, Y. Association of mRNA expression levels of Cullin family members with prognosis in breast cancer: An online database analysis. Medicine 2019, 98, e16625. [Google Scholar] [CrossRef] [PubMed]
- Feng, M.; Wang, Y.; Bi, L.; Wang, H.; Mao, Z.; Wei, G. CRL4ADTL degrades DNA-PKcs to modulate NHEJ repair and induce genomic instability and subsequent malignant transformation. Oncogene 2021, 40, 2096–2111. [Google Scholar] [CrossRef]
- Alhammad, R. Bioinformatics Identification of TUBB as Potential Prognostic Biomarker for Worse Prognosis in ERα-Positive and Better Prognosis in ERα-Negative Breast Cancer. Diagnostics 2022, 12, 2067. [Google Scholar] [CrossRef]
- Wang, G.; Zhao, M.; Li, G.; Zheng, F.; Xu, G.; Hong, X. m7G-Associated subtypes, tumor microenvironment, and validation of prognostic signature in lung adenocarcinoma. Front. Genet. 2022, 13, 954840. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, X.; Tian, Y.; Liu, L.; Su, P. Decreased Expression of circ_0000160 in Breast Cancer With Axillary Lymph Node Metastasis. Front. Mol. Biosci. 2022, 8, 690826. Available online: https://www.frontiersin.org/articles/10.3389/fmolb.2021.690826 (accessed on 19 September 2022). [CrossRef]
- Kazazian, K.; Go, C.; Wu, H.; Brashavitskaya, O.; Xu, R.; Dennis, J.; Gringras, A.; Swallow, C. Plk4 Promotes Cancer Invasion and Metastasis through Arp2/3 Complex Regulation of the Actin Cytoskeleton. Cancer Res. 2017, 77, 434–447. [Google Scholar] [CrossRef] [PubMed]
- Iacopetta, D.; Rechoum, Y.; Fuqua, S. The Role of Androgen Receptor in Breast Cancer. Drug Discov. Today Dis. Mech. 2012, 9, e19–e27. [Google Scholar] [CrossRef] [PubMed]
- Michmerhuizen, A.; Spratt, D.; Pierce, L.; Speers, C. Are we there yet? Understanding androgen receptor signaling in breast cancer. NPJ Breast Cancer 2020, 6, 47. [Google Scholar] [CrossRef] [PubMed]
- Bleach, R.; McIlroy, M. The Divergent Function of Androgen Receptor in Breast Cancer; Analysis of Steroid Mediators and Tumor Intracrinology. Front. Endocrinol. 2018, 9, 594. [Google Scholar] [CrossRef] [PubMed]
- Khatun, A.; Shimozawa, M.; Kito, H.; Kawaguchi, M.; Fujimoto, M.; Ri, M.; Kajikuri, J.; Niwa, S.; Fujii, M.; Ohya, S. Transcriptional Repression and Protein Degradation of the Ca2+-Activated K+ Channel KCa1.1 by Androgen Receptor Inhibition in Human Breast Cancer Cells. Front. Physiol. 2018, 9, 312. Available online: https://www.frontiersin.org/articles/10.3389/fphys.2018.00312 (accessed on 30 August 2022). [CrossRef] [PubMed]
- Roy, S.; Vadlamudi, R. Role of Estrogen Receptor Signaling in Breast Cancer Metastasis. Int. J. Breast Cancer. 2012, 2012, 654698. [Google Scholar] [CrossRef]
- Cheng, R.; Qi, L.; Kong, X.; Wang, Z.; Fang, Y.; Wang, J. Identification of the Significant Genes Regulated by Estrogen Receptor in Estrogen Receptor-Positive Breast Cancer and Their Expression Pattern Changes When Tamoxifen or Fulvestrant Resistance Occurs. Front. Genet. 2020, 11, 538734. [Google Scholar] [CrossRef]
- Venz, S.; Junker, H.; Ultsch, E.; Hetke, F.; Kruger, E.; Burchardt, M.; Caetano-Pinto, P.; Roennau, C. Identification of the Regulatory Targets of miR-3687 and miR-4417 in Prostate Cancer Cells Using a Proteomics Approach. Int. J. Mol. Sci. 2022, 23, 10565. [Google Scholar] [CrossRef]
- Jalava, S.; Urbanucci, A.; Latonen, L.; Waltering, K.; Sahu, B.; Janne, O.; Seppala, J.; Lahdesmaki, H.; Tammela, T.; Visakorpi, T. Androgen-regulated miR-32 targets BTG2 and is overexpressed in castration-resistant prostate cancer. Oncogene 2012, 31, 4460–4471. [Google Scholar] [CrossRef]
- Koundal, D.; Sharma, B. Challenges and future directions in neutrosophic set-based medical image analysis. In Neutrosophic Set in Medical Image Analysis; Academic Press: Cambridge, MA, USA, 2019; pp. 313–343. [Google Scholar] [CrossRef]
- Koundal, D.; Sharma, B.; Guo, Y. Intuitionistic based segmentation of thyroid nodules in ultrasound images. Comput. Biol. Med. 2020, 121, 103776. [Google Scholar] [CrossRef]
- Lahoura, V.; Singh, H.; Aggarwal, A.; Sharma, B.; Mohammed, M.; Damasevicius, R.; Kadry, S.; Cengiz, K. Cloud Computing-Based Framework for Breast Cancer Diagnosis Using Extreme Learning Machine. Diagnostics 2021, 11, 241. [Google Scholar] [CrossRef] [PubMed]
- Varga, A.; Marton, E.; Markovics, A.; Penyige, A.; Balogh, I.; Nagy, B.; Szilagyi, M. Suppressing the PI3K/AKT Pathway by miR-30d-5p Mimic Sensitizes Ovarian Cancer Cells to Cell Death Induced by High-Dose Estrogen. Biomedicines 2022, 10, 2060. [Google Scholar] [CrossRef]
- Gao, C.; Wei, J.; Tang, T.; Huang, Z. Role of microRNA-33a in malignant cells (Review). Oncol. Lett. 2020, 20, 2537–2556. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Chen, Z.; Wang, Y.; Wang, X.; Chen, L.; Yuan, T.; Tang, X.; Lu, Y.; Chen, H.; Chen, M.; et al. Several circulating miRNAs related to hyperlipidemia and atherosclerotic cardiovascular diseases. Lipids Health Dis. 2019, 18, 104. [Google Scholar] [CrossRef] [PubMed]






| Gene Symbol | Correlation Coefficient 1 | p-Value | Number of Patients |
|---|---|---|---|
| CCT2 | 0.6541 | <0.0001 | 3685 |
| LEMD3 | 0.6339 | <0.0001 | 3685 |
| NUP107 | 0.6324 | <0.0001 | 3685 |
| XPOT | 0.6155 | <0.0001 | 3685 |
| TBK1 | 0.6058 | <0.0001 | 3685 |
| PCBP2P2 | 0.5962 | <0.0001 | 530 |
| CNOT2 | 0.5901 | <0.0001 | 3685 |
| ANKRD18EP | 0.5863 | <0.0001 | 530 |
| XPOTP1 | 0.5848 | <0.0001 | 530 |
| YEATS4 | 0.5838 | <0.0001 | 3685 |
| CPSF6 | 0.5686 | <0.0001 | 3685 |
| RAB21 | 0.5648 | <0.0001 | 3685 |
| FRS2 | 0.5577 | <0.0001 | 3685 |
| LARP4 | 0.5474 | <0.0001 | 3685 |
| YWHAZP4 | 0.5464 | <0.0001 | 530 |
| MDM2 | 0.5444 | <0.0001 | 3685 |
| MDM1 | 0.5387 | <0.0001 | 3685 |
| SUDS3P1 | 0.5379 | <0.0001 | 530 |
| LRRC37A16P | 0.5342 | <0.0001 | 530 |
| PTGES3P3 | 0.5318 | <0.0001 | 530 |
| SCYL2 | 0.5234 | <0.0001 | 3685 |
| PTGES3 | 0.5193 | <0.0001 | 3685 |
| NUS1P1 | 0.5097 | <0.0001 | 530 |
| FAM3C2P | 0.5081 | <0.0001 | 530 |
| XPO1 | 0.5045 | <0.0001 | 3685 |
| TCAF1P1 | 0.5041 | <0.0001 | 530 |
| RBM12 | 0.5014 | <0.0001 | 3685 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhammad, R. Bioinformatics Analysis of the Prognostic Significance of CAND1 in ERα-Positive Breast Cancer. Diagnostics 2022, 12, 2327. https://doi.org/10.3390/diagnostics12102327
Alhammad R. Bioinformatics Analysis of the Prognostic Significance of CAND1 in ERα-Positive Breast Cancer. Diagnostics. 2022; 12(10):2327. https://doi.org/10.3390/diagnostics12102327
Chicago/Turabian StyleAlhammad, Rashed. 2022. "Bioinformatics Analysis of the Prognostic Significance of CAND1 in ERα-Positive Breast Cancer" Diagnostics 12, no. 10: 2327. https://doi.org/10.3390/diagnostics12102327
APA StyleAlhammad, R. (2022). Bioinformatics Analysis of the Prognostic Significance of CAND1 in ERα-Positive Breast Cancer. Diagnostics, 12(10), 2327. https://doi.org/10.3390/diagnostics12102327