Hip Preservation Surgery in Osteoarthritis Prevention: Potential Benefits of the Radiographic Angular Correction
Abstract
:1. Introduction
2. Materials and Methods
- -
- Group 1 (n = 147): Group corresponding to younger patients aged 60 or less;
- -
- Group 2 (n = 155): Group corresponding to patients aged between 61 and 74 years;
- -
- Group 3 (n = 98): Group corresponding to elderly patients aged 75 years or more.
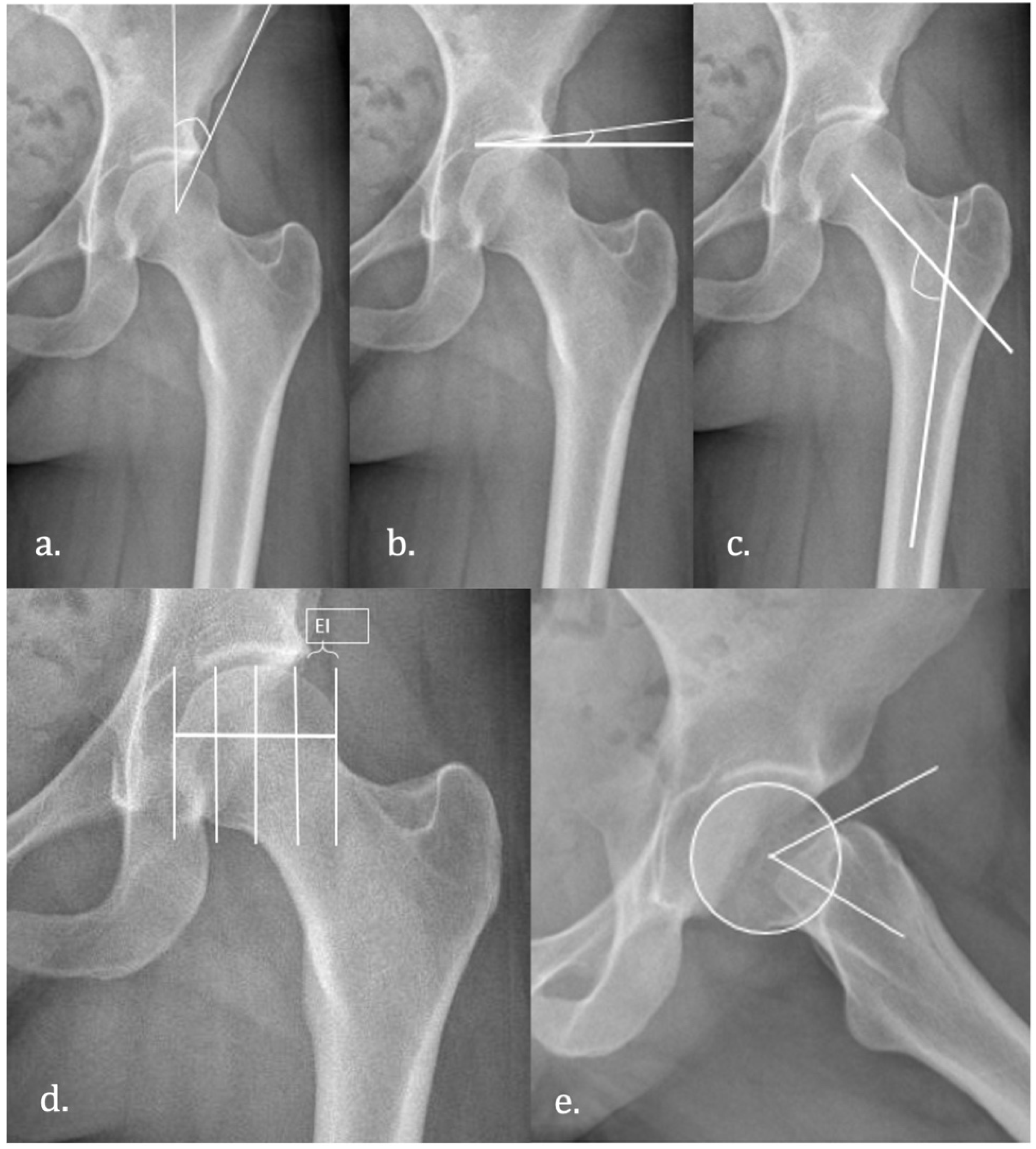
Radiological Measurements
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Bedi, A.; Dolan, M.; Leunig, M.; Kelly, B.T. Static and dynamic mechanical causes of hip pain. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2011, 27, 235–251. [Google Scholar] [CrossRef] [PubMed]
- Chegini, S.; Beck, M.; Ferguson, S.J. The effects of impingement and dysplasia on stress distributions in the hip joint during sitting and walking: A finite element analysis. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2009, 27, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Doherty, M.; Courtney, P.; Doherty, S.; Jenkins, W.; Maciewicz, R.A.; Muir, K.; Zhang, W. Nonspherical femoral head shape (pistol grip deformity), neck shaft angle, and risk of hip osteoarthritis: A case-control study. Arthritis Rheum. 2008, 58, 3172–3182. [Google Scholar] [CrossRef] [PubMed]
- Freeman, C.R.; Azzam, M.G.; Leunig, M. Hip preservation surgery: Surgical care for femoroacetabular impingement and the possibility of preventing hip osteoarthritis. J. Hip Preserv. Surg. 2014, 1, 46–55. [Google Scholar] [CrossRef] [Green Version]
- Ganz, R.; Parvizi, J.; Beck, M.; Leunig, M.; Nötzli, H.; Siebenrock, K.A. Femoroacetabular impingement: A cause for osteoarthritis of the hip. Clin. Orthop. 2003, 417, 112–120. [Google Scholar] [CrossRef]
- Nicholls, A.S.; Kiran, A.; Pollard, T.C.B.; Hart, D.J.; Arden, C.P.A.; Spector, T.; Gill, H.S.; Murray, D.W.; Carr, A.J.; Arden, N.K. The association between hip morphology parameters and nineteen-year risk of end-stage osteoarthritis of the hip: A nested case-control study. Arthritis Rheum. 2011, 63, 3392–3400. [Google Scholar] [CrossRef] [Green Version]
- Ng, V.Y.; Ellis, T.J. More than just a bump: Cam-type femoroacetabular impingement and the evolution of the femoral neck. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2011, 21, 1–8. [Google Scholar] [CrossRef]
- Siebenrock, K.A.; Fiechter, R.; Tannast, M.; Mamisch, T.C.; von Rechenberg, B. Experimentally induced cam impingement in the sheep hip. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2013, 31, 580–587. [Google Scholar] [CrossRef]
- Tannast, M.; Wolfer, N.; Ryan, M.K.; Nuss, K.M.; von Rechenberg, B.; Steppacher, S.D. Vascular supply of the femoral head in sheep-Implications for the ovine femoroacetabular impingement model. J. Orthop. Res. Off. Publ. Orthop. Res. Soc. 2018, 36, 2340–2348. [Google Scholar] [CrossRef] [Green Version]
- Yépez, A.K.; Abreu, M.; Germani, B.; Galia, C.R. Prevalence of femoroacetabular impingement morphology in asymptomatic youth soccer players: Magnetic resonance imaging study with clinical correlation. Rev. Bras. Ortop. 2017, 52, 14–20. [Google Scholar] [CrossRef]
- Diesel, C.V.; Ribeiro, T.A.; Scheidt, R.B.; de Souza Macedo, C.A.; Galia, C.R. The prevalence of femoroacetabular impingement in radiographs of asymptomatic subjects: A cross-sectional study. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2015, 25, 258–263. [Google Scholar] [CrossRef]
- Frank, J.M.; Harris, J.; Erickson, B.J.; Slikker, W.; Bush-Joseph, C.A.; Salata, M.J.; Nho, S.J. Prevalence of Femoroacetabular Impingement Imaging Findings in Asymptomatic Volunteers: A Systematic Review. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2015, 31, 1199–1204. [Google Scholar] [CrossRef]
- Johnson, A.C.; Shaman, M.A.; Ryan, T.G. Femoroacetabular impingement in former high-level youth soccer players. Am. J. Sports Med. 2012, 40, 1342–1346. [Google Scholar] [CrossRef]
- Philippon, M.J.; Ho, C.P.; Briggs, K.K.; Stull, J.; LaPrade, R.F. Prevalence of increased alpha angles as a measure of cam-type femoroacetabular impingement in youth ice hockey players. Am. J. Sports Med. 2013, 41, 1357–1362. [Google Scholar] [CrossRef]
- Thier, S.; Gerisch, D.; Weiss, C.; Fickert, S.; Brunner, A. Prevalence of Cam and Pincer Deformities in the X-rays of Asymptomatic Individuals. BioMed. Res. Int. 2017, 2017, 8562329. [Google Scholar] [CrossRef] [Green Version]
- Domb, B.G.; Chaharbakhshi, E.O.; Rybalko, D.; Close, M.R.; Litrenta, J.; Perets, I. Outcomes of Hip Arthroscopic Surgery in Patients with Tönnis Grade 1 Osteoarthritis at a Minimum 5-Year Follow-up: A Matched-Pair Comparison with a Tönnis Grade 0 Control Group. Am. J. Sports Med. 2017, 45, 2294–2302. [Google Scholar] [CrossRef]
- Domb, B.G.; Philippon, M.J.; Giordano, B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthrosc. J. Arthrosc. Relat. Surg. Off. Publ. Arthrosc. Assoc. N. Am. Int. Arthrosc. Assoc. 2013, 29, 162–173. [Google Scholar] [CrossRef]
- Fujii, M.; Nakashima, Y.; Jingushi, S.; Yamamoto, T.; Noguchi, Y.; Suenaga, E.; Iwamoto, Y. Intraarticular findings in symptomatic developmental dysplasia of the hip. J. Pediatr. Orthop. 2009, 29, 9–13. [Google Scholar] [CrossRef]
- Klaue, K.; Durnin, C.W.; Ganz, R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J. Bone Jt. Surg. Br. 1991, 73, 423–429. [Google Scholar] [CrossRef]
- Nozawa, M.; Shitoto, K.; Matsuda, K.; Maezawa, K.; Kurosawa, H. Rotational acetabular osteotomy for acetabular dysplasia. A follow-up for more than ten years. J. Bone Jt. Surg. Br. 2002, 84, 59–65. [Google Scholar] [CrossRef]
- Clohisy, J.C.; Nunley, R.M.; Curry, M.C.; Schoenecker, P.L. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J. Bone Jt. Surg. Am. 2007, 89, 1417–1423. [Google Scholar] [CrossRef] [Green Version]
- Clohisy, J.C.; Beaulé, P.E.; O’Malley, A.; Safran, M.R.; Schoenecker, P. AOA symposium. Hip disease in the young adult: Current concepts of etiology and surgical treatment. J. Bone Jt. Surg. Am. 2008, 90, 2267–2281. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adler, K.L.; Cook, P.C.; Yen, Y.-M.; Giordano, B.D. Current Concepts in Hip Preservation Surgery: Part I. Sports Health 2015, 7, 518–526. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Campbell, S.E. Radiography of the hip: Lines, signs, and patterns of disease. Semin. Roentgenol. 2005, 40, 290–319. [Google Scholar] [CrossRef] [Green Version]
- Gosvig, K.K.; Jacobsen, S.; Palm, H.; Sonne-Holm, S.; Magnusson, E. A new radiological index for assessing asphericity of the femoral head in cam impingement. J. Bone Jt. Surg. Br. 2007, 89, 1309–1316. [Google Scholar] [CrossRef] [Green Version]
- Tönnis, D.; Heinecke, A. Acetabular and femoral anteversion: Relationship with osteoarthritis of the hip. J. Bone Jt. Surg. Am. 1999, 81, 1747–1770. [Google Scholar] [CrossRef]
- Bardakos, N.V.; Villar, R.N. Predictors of progression of osteoarthritis in femoroacetabular impingement: A radiological study with a minimum of ten years follow-up. J. Bone Jt. Surg. Br. 2009, 91, 162–169. [Google Scholar] [CrossRef]
- Li, P.L.S.; Ganz, R. Morphologic features of congenital acetabular dysplasia: One in six is retroverted. Clin. Orthop. 2003, 416, 245–253. [Google Scholar] [CrossRef]
- Agricola, R.; Heijboer, M.; Roze, R.; Reijman, M.; Bierma-Zeinstra, S.; Verhaar, J.; Weinans, H.; Waarsing, J. Pincer deformity does not lead to osteoarthritis of the hip whereas acetabular dysplasia does: Acetabular coverage and development of osteoarthritis in a nationwide prospective cohort study (CHECK). Osteoarthr. Cartil. 2013, 21, 1514–1521. [Google Scholar] [CrossRef] [Green Version]
- Ipach, I.; Rondak, I.-C.; Sachsenmaier, S.; Buck, E.; Syha, R.; Mittag, F. Radiographic signs for detection of femoroacetabular impingement and hip dysplasia should be carefully used in patients with osteoarthritis of the hip. BMC Musculoskelet. Disord. 2014, 15, 150. [Google Scholar] [CrossRef] [Green Version]
- Hartofilakidis, G.; Bardakos, N.V.; Babis, G.C.; Georgiades, G. An examination of the association between different morphotypes of femoroacetabular impingement in asymptomatic subjects and the development of osteoarthritis of the hip. J. Bone Jt. Surg. Br. 2011, 93, 580–586. [Google Scholar] [CrossRef] [Green Version]
- Wyles, C.C.; Heidenreich, M.J.; Jeng, J.; Larson, D.R.; Trousdale, R.T.; Sierra, R.J. The John Charnley Award: Redefining the Natural History of Osteoarthritis in Patients with Hip Dysplasia and Impingement. Clin. Orthop. 2017, 475, 336–350. [Google Scholar] [CrossRef] [Green Version]
- Byrd, J.W.T. Femoroacetabular impingement in athletes: Current concepts. Am. J. Sports Med. 2014, 42, 737–751. [Google Scholar] [CrossRef]
- Blankenstein, T.; Grainger, A.; Dube, B.; Evans, R.; Robinson, P. MRI hip findings in asymptomatic professional rugby players, ballet dancers, and age-matched controls. Clin. Radiol. 2020, 75, 116–122. [Google Scholar] [CrossRef]
- Byers, P.D.; Contepomi, C.A.; Farkas, T.A. A post mortem study of the hip joint. Including the prevalence of the features of the right side. Ann. Rheum. Dis. 1970, 29, 15–31. [Google Scholar] [CrossRef] [Green Version]
- Farrell, G.; McGrath, F.; Hogan, B.; Logan, M.; Denvir, K.; O’Connell, B.; Irwin, E.; Gissane, C.; Wilson, F. 95% prevalence of abnormality on hip MRI in elite academy level rugby union: A clinical and imaging study of hip disorders. J. Sci. Med. Sport 2016, 19, 893–897. [Google Scholar] [CrossRef] [Green Version]
- Seldes, R.M.; Tan, V.; Hunt, J.; Katz, M.; Winiarsky, R.; Fitzgerald, R.H. Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin. Orthop. 2001, 382, 232–240. [Google Scholar] [CrossRef]
- Gosvig, K.K.; Jacobsen, S.; Sonne-Holm, S.; Gebuhr, P. The prevalence of cam-type deformity of the hip joint: A survey of 4151 subjects of the Copenhagen Osteoarthritis Study. Acta Radiol. 2008, 49, 436–441. [Google Scholar] [CrossRef]
- Allen, D.; Beaulé, P.E.; Ramadan, O.; Doucette, S. Prevalence of associated deformities and hip pain in patients with cam-type femoroacetabular impingement. J. Bone Jt. Surg. Br. 2009, 91, 589–594. [Google Scholar] [CrossRef]
- Kang, A.C.L.; Gooding, A.J.; Coates, M.H.; Goh, T.D.; Armour, P.; Rietveld, J. Computed tomography assessment of hip joints in asymptomatic individuals in relation to femoroacetabular impingement. Am. J. Sports Med. 2010, 38, 1160–1165. [Google Scholar] [CrossRef]
- Laborie, L.B.; Lehmann, T.G.; Engesæter, I.Ø.; Eastwood, D.M.; Engesæter, L.B.; Rosendahl, K. Prevalence of radiographic findings thought to be associated with femoroacetabular impingement in a population-based cohort of 2081 healthy young adults. Radiology 2011, 260, 494–502. [Google Scholar] [CrossRef] [Green Version]
- Morales-Avalos, R.; Leyva-Villegas, J.I.; Sánchez-Mejorada, G.; Reynaga-Obregón, J.; León, S.G.-D.; Vílchez-Cavazos, F.; Espinosa-Uribe, A.G.; Acosta-Olivo, C.; De La Garza-Castro, O.; Guzmán-Avilan, R.I.; et al. Prevalence, topographic and morphometric features of femoral cam-type deformity: Changes in relation to age and gender. Anat. Sci. Int. 2016, 91, 391–397. [Google Scholar] [CrossRef]
- Briggs, K.K.; Soares, E.; Bhatia, S.; Philippon, M.J. Postoperative alpha angle not associated with patient-centered midterm outcomes following hip arthroscopy for FAI. Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2019, 27, 3105–3109. [Google Scholar] [CrossRef]
- Femoroacetabular Impingement Randomized Controlled Trial (FIRST) Investigators; Ayeni, O.R.; Karlsson, J.; Heels-Ansdell, D.; Thabane, L.; Musahl, V.; Simunovic, N.; Duong, A.; Bhandari, M.; Bedi, A.; et al. Osteochondroplasty and Labral Repair for the Treatment of Young Adults with Femoroacetabular Impingement: A Randomized Controlled Trial. Am. J. Sports Med. 2020, 49, 25–34. [Google Scholar] [CrossRef]
- Griffin, D.R.; Dickenson, E.J.; Wall, P.; Achana, F.; Donovan, J.L.; Griffin, J.; Hobson, R.; Hutchinson, C.E.; Jepson, M.; Parsons, N.; et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): A multicentre randomised controlled trial. Lancet 2018, 391, 2225–2235. [Google Scholar] [CrossRef]
- Mansell, N.S.; Rhon, D.I.; Meyer, J.; Slevin, J.M.; Marchant, B.G. Arthroscopic Surgery or Physical Therapy for Patients with Femoroacetabular Impingement Syndrome: A Randomized Controlled Trial with 2-Year Follow-up. Am. J. Sports Med. 2018, 46, 1306–1314. [Google Scholar] [CrossRef]
- Kemp, J.L.; Crossley, K.M.; Agricola, R.; Geuskens, F.; van Middelkoop, M. Radiographic Hip Osteoarthritis Is Prevalent, and Is Related to Cam Deformity 12–24 Months Post-Hip Arthroscopy. Int. J. Sports Phys. Ther. 2018, 13, 177–184. [Google Scholar] [CrossRef] [Green Version]
- Lafrance, R.; Williams, R.; Madsen, W.; Maloney, M.; Drinkwater, C.; Giordano, B. The prevalence of radiographic criteria of femoral acetabular impingement in patients undergoing hip arthroplasty surgery. Geriatr. Orthop. Surg. Rehabil. 2014, 5, 21–26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haneda, M.; Rai, M.F.; Cai, L.; Brophy, R.; O’Keefe, R.J.; Clohisy, J.C.; Pascual-Garrido, C. Distinct Pattern of Inflammation of Articular Cartilage and the Synovium in Early and Late Hip Femoroacetabular Impingement. Am. J. Sports Med. 2020, 48, 2481–2488. [Google Scholar] [CrossRef] [PubMed]
- Chinzei, N.; Hashimoto, S.; Fujishiro, T.; Hayashi, S.; Kanzaki, N.; Uchida, S.; Kuroda, R.; Kurosaka, M. Inflammation and Degeneration in Cartilage Samples from Patients with Femoroacetabular Impingement. J. Bone Jt. Surg. Am. 2016, 98, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Bedi, A.; Lynch, E.B.; Enselman, E.R.S.; Davis, M.E.; DeWolf, P.D.; Makki, T.A.; Kelly, B.T.; Larson, C.M.; Henning, P.T.; Mendias, C.L. Elevation in circulating biomarkers of cartilage damage and inflammation in athletes with femoroacetabular impingement. Am. J. Sports Med. 2013, 41, 2585–2590. [Google Scholar] [CrossRef] [Green Version]
- Malahias, M.-A.; Gu, A.; Richardson, S.S.; De Martino, I.; Sculco, P.K.; McLawhorn, A.S. Hip arthroscopy for hip osteoarthritis is associated with increased risk for revision after total hip arthroplasty. Hip Int. J. Clin. Exp. Res. Hip Pathol. Ther. 2020, 31, 656–662. [Google Scholar] [CrossRef]
- Hunter, D.J.; Eyles, J.; Murphy, N.J.; Spiers, L.; Burns, A.; Davidson, E.; Dickenson, E.; Fary, C.; Foster, N.E.; Fripp, J.; et al. Multi-centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapist-led care for femoroacetabular impingement (FAI) syndrome on hip cartilage metabolism: The Australian FASHIoN trial. BMC Musculoskelet. Disord. 2021, 22, 697. [Google Scholar] [CrossRef]
- Schmaranzer, F.; Haefeli, P.C.; Hanke, M.S.; Liechti, E.F.; Werlen, S.F.; Siebenrock, K.A.; Tannast, M. How Does the dGEMRIC Index Change After Surgical Treatment for FAI? A Prospective Controlled Study: Preliminary Results. Clin. Orthop. 2017, 475, 1080–1099. [Google Scholar] [CrossRef] [Green Version]

| Age | 64.75 (11.1) |
|---|---|
| Sex (M:F) | 236:164 |
| Size (R:L) | 222:178 |
| BMI | 28.12 (4.42) |
| Wiberg angle (°) | 38.2 (14.21) |
| Acetabular Angle (°) | 10.86 (9.81) |
| Extrusion Index (%) | 18.02 (12.07) |
| Alpha Angle (°) | 68.59 (18.66) |
| Cervical–Diaphyseal angle (°) | 131.45 (8.83) |
| Group 1 (n = 147) | Group 2 (n = 155) | Group 3 (n = 98) | |
|---|---|---|---|
| Sex (M:F) | 98:49 | 87:68 | 50:48 |
| Size (R:L) | 84:63 | 84:71 | 54:44 |
| BMI | 27.65 (4.54) | 28.77 (4.29) | 27.83 (4.36) |
| Wiberg angle (°) | 30.54 (14.63) | 41.73 (11.20) | 44.77 (12.02) |
| Tönnis angle (°) | 15.35 (8.77) | 8.94 (8.63) | 7.11 (10.57) |
| Extrusion Index (%) | 22.12 (4.54) | 16.73 (11.47) | 13.89(11.03) |
| Alpha angle (°) | 61.78 (12.87) | 71.34 (17.15) | 73.64 (19.46) |
| Cervical–Diaphyseal angle (°) | 133.17 (8.96) | 130.60 (8.61) | 130.28 (9.34) |
| Group | Difference | IC (95%) | p | |
|---|---|---|---|---|
| Wiberg angle (°) | ≤60 vs. 61–74 | −11.39 | −15.036–(−7.75) | <0.01 |
| ≤60 vs. ≥75 | −14.43 | −18.58–(−10.2) | <0.01 | |
| 60–74 vs. ≥75 | −3.04 | −6.69–0.61 | 0.133 | |
| Tönnis angle (°) | ≤60 vs. 61–74 | 6.41 | 4.00–8.8 | <0.01 |
| ≤60 vs. ≥75 | 8.24 | 5.12–11.36 | <0.01 | |
| 60–74 vs. >75 | 1.82 | −1.23–4.9 | 0.395 | |
| Extrusion index (%) | ≤60 vs. 61–74 | 5.39 | 2.12–8.66 | <0.01 |
| ≤60 vs. ≥75 | 8.23 | 4.61–11.85 | <0.01 | |
| 61–74 vs. >75 | 2.83 | −0.62–6.2 | 0.65 | |
| Alpha angle (°) | ≤60 vs. 61–74 | −9.55 | −14.65–(−4.46) | <0.01 |
| ≤60 vs. ≥75 | −11.86 | −18.00–(−5.71) | <0.01 | |
| 61–74 vs. ≥75 | −2.3 | −8.23–3.62 | 0.726 | |
| Cervical–Diaphyseal angle (°) | ≤60 vs. 61–74 | −1.11 | −6.83–4.61 | 0.954 |
| ≤60 vs. ≥75 | −0.29 | −6.75–6.16 | 0.999 | |
| 61–74 vs. ≥75 | 0.81 | −3.90–5.53 | 0.966 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamo-Espinosa, J.M.; Alfonso, A.; Pascual, E.; García-Ausín, J.; Sánchez-Gordoa, M.; Blanco, A.; Gómez-Álvarez, J.; San-Julián, M. Hip Preservation Surgery in Osteoarthritis Prevention: Potential Benefits of the Radiographic Angular Correction. Diagnostics 2022, 12, 1128. https://doi.org/10.3390/diagnostics12051128
Lamo-Espinosa JM, Alfonso A, Pascual E, García-Ausín J, Sánchez-Gordoa M, Blanco A, Gómez-Álvarez J, San-Julián M. Hip Preservation Surgery in Osteoarthritis Prevention: Potential Benefits of the Radiographic Angular Correction. Diagnostics. 2022; 12(5):1128. https://doi.org/10.3390/diagnostics12051128
Chicago/Turabian StyleLamo-Espinosa, José M., Adrián Alfonso, Elena Pascual, Jorge García-Ausín, Miguel Sánchez-Gordoa, Asier Blanco, Jorge Gómez-Álvarez, and Mikel San-Julián. 2022. "Hip Preservation Surgery in Osteoarthritis Prevention: Potential Benefits of the Radiographic Angular Correction" Diagnostics 12, no. 5: 1128. https://doi.org/10.3390/diagnostics12051128
APA StyleLamo-Espinosa, J. M., Alfonso, A., Pascual, E., García-Ausín, J., Sánchez-Gordoa, M., Blanco, A., Gómez-Álvarez, J., & San-Julián, M. (2022). Hip Preservation Surgery in Osteoarthritis Prevention: Potential Benefits of the Radiographic Angular Correction. Diagnostics, 12(5), 1128. https://doi.org/10.3390/diagnostics12051128






