Micropulse Transscleral Cyclophotocoagulation for Glaucoma after Penetrating Keratoplasty
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Initial Characteristics
3.2. Follow-Up
3.3. Primary Outcome—IOP Evolution
3.4. Secondary Outcomes
3.4.1. Antiglaucoma Medication
3.4.2. Visual Acuity
3.4.3. Corneal Graft Status
3.4.4. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hemanth Raj, M.N.; Bhanushree, G.; Hlinaykor, R.M.; Vijayanath, V. Preoperative Risk Factors and Incidence of Glaucoma after Penetrating Keratoplasty. Int. J. Clin. Trails 2014, 1, 55–61. [Google Scholar]
- Franea, E.T.; Araeri, E.S.; Roche, F.J. A Study of Glaucoma after Penetrating Keratoplasty. Cornea 2002, 21, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Zemba, M.; Stamate, A.C. Glaucoma after Penetrating Keratoplasty. Rom. J. Ophthalmol. 2017, 61, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, K.; Price, M.O.; Feng, M.T.; Price, W.P. Micropulse Transscleral Cyclophotocoagulation in Keratoplasty Eyes. Cornea 2019, 38, 542–545. [Google Scholar] [CrossRef] [PubMed]
- Baltaziak, M.; Chew, H.F.; Podbielski, D.W.; Ahmed, I.I.K. Glaucoma after Corneal Replacement. Surv. Ophthalmol. 2018, 63, 135–148. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Vu, V.; Lazcano-Gomez, G.; Han, K.; Suvannachart, P.; Rose-Nussbaumer, J.; Schallhorn, J.; Hwang, D.; Han, Y. Clinical Outcomes of Micropulse Transscleral Cyclophotocoagulation in Patients with a History of Keratoplasty. J. Ophthalmol. 2020, 2020, 6147248. [Google Scholar] [CrossRef]
- Hau, S.; Barton, K. Corneal Complications of Glaucoma Surgery. Curr. Opin. Ophtalmol. 2009, 20, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.; Yu, S.; Wong, J. Micropulse Laser for the Treatment of Glaucoma: A Literature Review. Surv. Ophthalmol. 2019, 64, 486–497. [Google Scholar] [CrossRef]
- Amoozgar, B.; Phan, E.N.; Lin, S.C.; Han, Y. Update on Ciliary Body Laser Procedures. Curr. Opin. Ophtalmol 2017, 28, 181–186. [Google Scholar] [CrossRef]
- Williams, A.; Moster, M.; Rahmatnejad, K.; Resende, A.; Horan, T.; Reynolds, M.; Yung, E.; Abramowitz, B.; Kuchar, S.; Waisbourd, M. Clinical Efficacy and Safety Profile of Micropulse Transscleral Cyclophotocoagulation in Refractory Glaucoma. J. Glaucoma 2018, 27, 445–449. [Google Scholar] [CrossRef]
- Stanca, H.; Munteanu, M.; Jianu, D.; Motoc, A.; Tăbăcaru, B.; Stanca, S.; Ungureanu, E.; Boruga, V.; Preda, M. New Perspectives in the Use of Laser Diode Transscleral Cyclophotocoagulation. A Prospective Single Center Observational Cohort Study. Rom. J. Morphol. Embryol. 2018, 59, 869–872. [Google Scholar] [PubMed]
- Robinson, C.H. Indications, Complications and Prognosis for Repeat Penetrating Keratoplasty. Ophthalmic Surg. 1979, 10, 27–34. [Google Scholar] [PubMed]
- Olson, R.; Kaufman, H. Prognostic Factors of Intraocular Pressure after Aphakic Keratoplasty. Am. J. Ophthalmol. 1975, 86, 510–515. [Google Scholar] [CrossRef]
- Dumitrescu, O.M.; Istrate, S.; Macovei, M.L.; Gheorghe, A.G. Intraocular Pressure Measurement after Penetrating Keratoplasty. Diagnostics 2022, 12, 234. [Google Scholar] [CrossRef]
- Garcia, G.A.; Nguyen, C.V.; Yelenskiy, A.; Akiyama, G.; McKnight, B.; Chopra, V.; Lu, K.; Huang, A.; Tan, J.C.H.; Francis, B.A. Micropulse Transscleral Diode Laser Cyclophotocoagulation in the Treatment of Refractory Glaucoma. Clin. Exp. Ophthalmol. 2010, 38, 266–272. [Google Scholar]
- Aquino, M.C.; Barton, K.; Tan, A.M.; Sng, C.; Li, X.; Loon, S.C.; Chew, P.T. Micropulse versus Continuous Wave Transscleral Diode Cyclophotocoagulation in Refractory Glaucoma: A Randomized Exploratory Study. Clin. Exp. Ophthalmol. 2015, 43, 40–46. [Google Scholar] [CrossRef]
- Zaarour, K.; Abdelmassih, Y.; Arej, N.; Cherfan, G.; Tomey, K.F.; Khoueir, Z. Outcomes of Micropulse Transscleral Cyclophotocoagulation in Uncontrolled Glaucoma Patients. J. Glaucoma 2019, 82, 270–275. [Google Scholar] [CrossRef]
- Preda, M.; Karancsi, O.; Munteanu, M.; Stanca, H. Clinical Outcomes of Micropulse Transscleral Cyclophotocoagulation in Refractory Glaucoma-18 Months Follow-up. Lasers Med. Sci. 2020, 35, 1487–1491. [Google Scholar] [CrossRef]
- Ocakoglu, O.; Arslan, O.S.; Kayiran, A. Diode Laser Transscleral Cyclophotocoagulation for the Treatment of Refractory Glaucoma after Penetrating Keratoplasty. Curr. Eye Res. 2005, 30, 569–574. [Google Scholar] [CrossRef]
- Elhefney, E.; Mokbel, T.; Hagras, S.; AlNagdy, A.; Ellayeh, A.; Mohsen, T.; Gaafar, W. Micropulsed Diode Laser Cyclophotocoagulation in Recurrent Pediatric Glaucoma. Eur. J. Ophthalmol. 2020, 30, 1149–1155. [Google Scholar] [CrossRef]
- Threlkeld, A.B.; Shields, M.B. Noncontact Transscleral Nd:YAG Cyclophotocoagulation for Glaucoma after Penetrating Keratoplasty. Am. J. Ophthalmol. 1995, 120, 569–576. [Google Scholar] [CrossRef]
- Ayyala, R.S.; Pieroth, L.; Vinals, A.F.; Goldstein, M.H.; Schuman, J.S.; Netland, P.A.; Dreyer, E.B.; Cooper, M.L.; Mattox, C.; Frangie, J.P.; et al. Comparison of Mitomycin C Trabeculectomy, Glaucoma Drainage Device Implantation, and Laser Neodymium:YAG Cyclophotocoagulation in the Management of Intractable Glaucoma after Penetrating Keratoplasty. Ophthalmology 1998, 105, 1550–1556. [Google Scholar] [CrossRef]
- Cohen, E.J.; Schwartz, L.W.; Luskind, R.D.; Parker, A.V.; Spaeth, G.L.; Katz, L.J.; Arentsen, J.J.; Wilson, R.P.; Moster, M.D.; Laibson, P.R. Neodymium: YAG Laser Transscleral Cyclophotocoagulation for Glaucoma after Penetrating Keratoplasty. Ophthalmic Surg. 1989, 20, 713–716. [Google Scholar] [PubMed]
- Knape, R.M.; Szymarek, T.N.; Tuli, S.S.; Driebe, W.T., Jr.; Sherwood, M.B.; Smith, M.F. Five-Year Outcomes of Eyes With Glaucoma Drainage Device and Penetrating Keratoplasty. J. Glaucoma 2012, 21, 608–614. [Google Scholar] [CrossRef] [Green Version]
- Purtskhvanidze, K.; Saeger, M.; Frimpong-Boateng, A.; Rufer, F.; Roider, J.; Noelle, B. Ten-Year Outcome of Glaucoma Drainage Device Surgery After Penetrating Keratoplasty. J. Glaucoma 2021, 30, e108–e113. [Google Scholar] [CrossRef]
- Akdemir, M.O.; Acar, B.T.; Kokturk, F.; Acar, S. Clinical Outcomes of Trabeculectomy vs. Ahmed Glaucoma Valve Implantation in Patients with Penetrating Keratoplasty: (Trabeculectomy vs. Ahmed Glaucoma Valve in Patients with Penetrating Keratoplasty). Int. Ophthalmol. 2016, 36, 541–546. [Google Scholar] [CrossRef]
- Anders, L.-M.; Gatzioufas, Z.; Grieshaber, M.C. Challanges in the Complex Management of Post-Keratoplasty Glaucoma. Ther. Adv. Ophthalmol. 2021, 13, 25158414211031397. [Google Scholar]
- Panda, A.; Prakash, V.J.; Dada, T.; Gupta, A.K.; Khokhar, S.; Vanathi, M. Ahmed Glaucoma Valve in Post-Penetrating-Keratoplasty Glaucoma: A Critically Evaluated Prospective Clinical Study. Indian J. Ophthalmol. 2011, 59, 185–189. [Google Scholar] [CrossRef]
- Ates, H.; Palamar, M.; Yagci, A.; Egrilmez, S. Evaluation of Ex-PRESS Mini Glaucoma Shunt Implantation in Refractory Postpenetrating Keratoplasty Glaucoma. J. Glaucoma 2010, 19, 556–560. [Google Scholar] [CrossRef] [Green Version]


| Patient | Gender | Age (Years) | Reason for PK | Cause of IOP Rise | Previous Surgery | Lens Status | Graft Status (Clear) | Follow-Up Period (Months) |
|---|---|---|---|---|---|---|---|---|
| 1 | M | 72 | BK | PreG, PAS | CE, Trab | PC-IOL | No | 12 |
| 2 | M | 68 | BK | PreG, ST | CE | PC-IOL | Yes | 12 |
| 3 | F | 65 | FCD | PreG, ST | CE, Trab | PC-IOL | No | 15 |
| 4 | M | 49 | PTL | PAS | WC, CE | SF-IOL | Yes | 15 |
| 5 | F | 69 | BK | PB, PAS | CE, AV | SF-IOL | Yes | 12 |
| 6 | F | 71 | BK | PB, PAS | CE, AV | SF-IOL | Yes | 15 |
| 7 | M | 80 | BK | PAS | CE, Trab | PC-IOL | Yes | 18 |
| 8 | F | 73 | BK | PreG, ST | CE | PC-IOL | No | 12 |
| 9 | M | 25 | BK | ST | CE | PC-IOL | Yes | 12 |
| 10 | F | 64 | BK | PAS, ST | CE, Trab, AV | PC-IOL | Yes | 15 |
| 11 | M | 59 | BCU | PAS; Chr.Inf. | CE | PC-IOL | No | 18 |
| 12 | M | 55 | GCD | ST | None | Phakic | Yes | 24 |
| 13 | F | 78 | FCD | PreG, ST | None | Phakic | Yes | 12 |
| 14 | M | 31 | HK | Chr.Infl. | None | Phakic | Yes | 12 |
| 15 | F | 66 | BK | ST | CE, Trab-M | PC-IOL | No | 24 |
| 16 | F | 75 | BCU | PAS, CI | CE | PC-IOL | Yes | 12 |
| 17 | M | 70 | BK | PreG, ST | CE | PC-IOL | Yes | 15 |
| 18 | F | 29 | BK | ST, Aphakia | CE | Aphakic | No | 15 |
| 19 | M | 44 | HK | Chr.Infl., PAS | None | Phakic | Yes | 12 |
| 20 | F | 77 | BK | ST | CE | PC-IOL | Yes | 12 |
| 21 | M | 71 | BK | PreG, ST, PAS | PV, CE, SO, AV | PC-IOL | Yes | 15 |
| 22 | M | 69 | PTL | PAS | WC, CE, PI | PC-IOL | Yes | 18 |
| 23 | M | 63 | BK | PAS, RI | PV, CE | PC-IOL | No | 15 |
| 24 | M | 54 | PTL | PAS, ST | WC, Trab-M | Phakic | Yes | 12 |
| 25 | F | 70 | BK | PreG, ST | CE | PC-IOL | Yes | 12 |
| 26 | M | 62 | BK | PAS, RI | PV, SO, CE | PC-IOL | No | 12 |
| Parameter/Time | IOP (Median (IQR)) | Medication (Median (IQR)) | Acetazolamide Usage (Nr., %) |
|---|---|---|---|
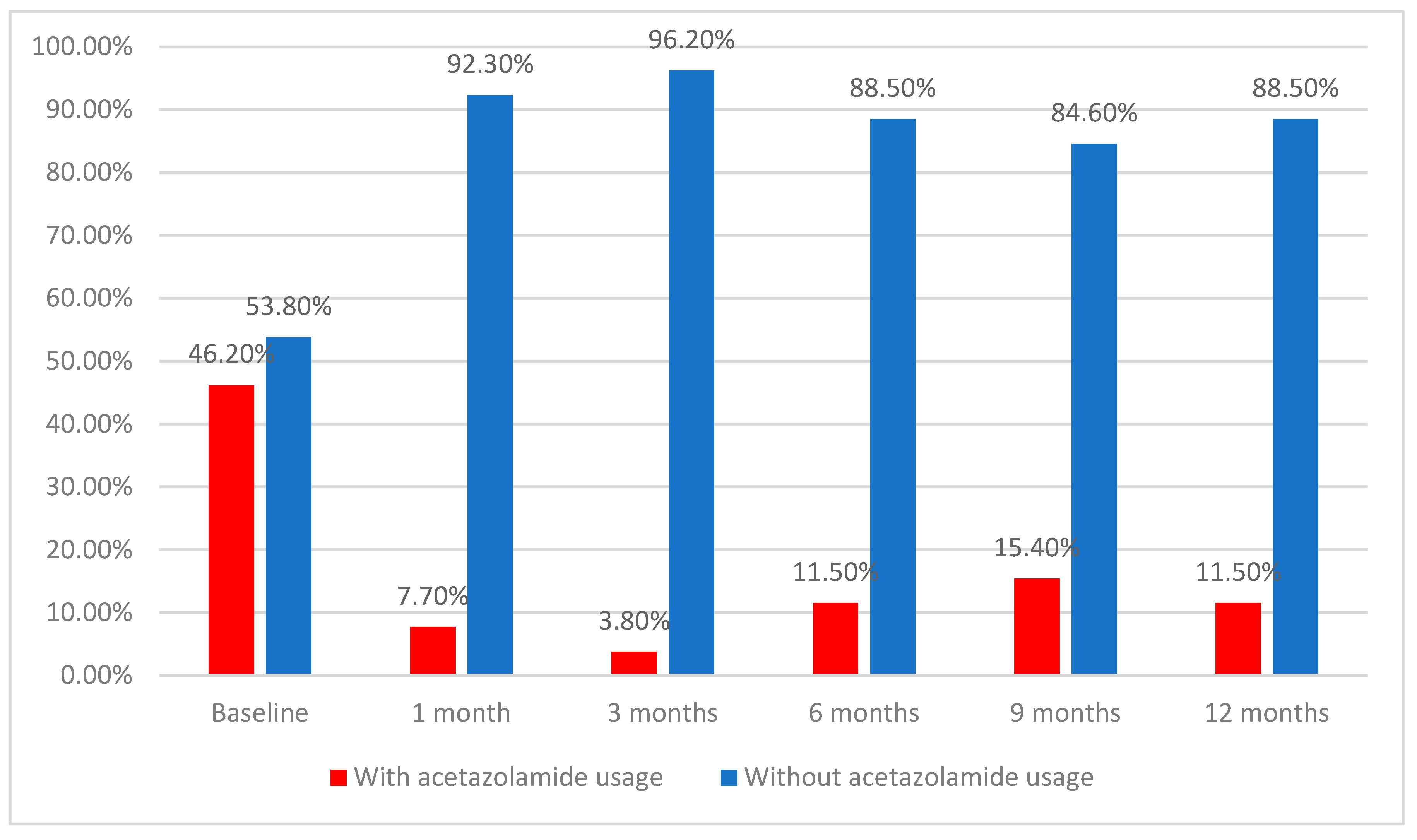
| Baseline | 29 (26–32) | 3 (2–3) | 12 (46.2%) |
| 1 month | 19 (16–21.25) | 2 (0.75–3) | 2 (7.7%) |
| 3 months | 17 (15.75–19.25) | 1.5 (0–2) | 1 (3.8%) |
| 6 months | 16.5 (13.5–20.5) | 1.5 (0–3) | 3 (11.5%) |
| 9 months | 16 (13.75–18.25) | 2 (0–3) | 4 (15.4%) |
| 12 months | 18 (16–20.25) | 1 (0.75–3) | 3 (11.5%) |
| p | <0.001 * | <0.001 * | <0.001 ** |
| Patient | Preoperative BCVA | BCVA after 12 Months | Clear Graft after Baseline | Clear Graft after 12 Months |
|---|---|---|---|---|
| 1 | HM | HM | No | No |
| 2 | 6/60 | 6/10 | Yes | Yes |
| 3 | CF | HM | No | No |
| 4 | 6/20 | 6/20 | Yes | Yes |
| 5 | 6/60 | 6/10 | Yes | Yes |
| 6 | CF | HM | Yes | No |
| 7 | 6/30 | 6/30 | Yes | Yes |
| 8 | CF | 6/120 | No | Yes |
| 9 | 6/30 | 6/30 | Yes | Yes |
| 10 | CF | CF | Yes | Yes |
| 11 | CF | HM | No | No |
| 12 | 6/15 | 6/15 | Yes | Yes |
| 13 | 6/20 | 6/20 | Yes | Yes |
| 14 | 6/120 | CF | Yes | No |
| 15 | CF | CF | No | No |
| 16 | 6/30 | 6/30 | Yes | Yes |
| 17 | 6/60 | 6/60 | Yes | Yes |
| 18 | HM | HM | No | No |
| 19 | 6/20 | 6/20 | Yes | Yes |
| 20 | CF | HM | Yes | No |
| 21 | 6/120 | CF | Yes | No |
| 22 | 6/20 | 6/20 | Yes | Yes |
| 23 | HM | LP | No | No |
| 24 | 6/30 | 6/30 | Yes | Yes |
| 25 | 6/60 | 6/60 | Yes | Yes |
| 26 | HM | LP | No | No |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zemba, M.; Dumitrescu, O.-M.; Stamate, A.-C.; Barac, I.R.; Tataru, C.P.; Branisteanu, D.C. Micropulse Transscleral Cyclophotocoagulation for Glaucoma after Penetrating Keratoplasty. Diagnostics 2022, 12, 1143. https://doi.org/10.3390/diagnostics12051143
Zemba M, Dumitrescu O-M, Stamate A-C, Barac IR, Tataru CP, Branisteanu DC. Micropulse Transscleral Cyclophotocoagulation for Glaucoma after Penetrating Keratoplasty. Diagnostics. 2022; 12(5):1143. https://doi.org/10.3390/diagnostics12051143
Chicago/Turabian StyleZemba, Mihail, Otilia-Maria Dumitrescu, Alina-Cristina Stamate, Ileana Ramona Barac, Calin Petru Tataru, and Daniel Constantin Branisteanu. 2022. "Micropulse Transscleral Cyclophotocoagulation for Glaucoma after Penetrating Keratoplasty" Diagnostics 12, no. 5: 1143. https://doi.org/10.3390/diagnostics12051143
APA StyleZemba, M., Dumitrescu, O. -M., Stamate, A. -C., Barac, I. R., Tataru, C. P., & Branisteanu, D. C. (2022). Micropulse Transscleral Cyclophotocoagulation for Glaucoma after Penetrating Keratoplasty. Diagnostics, 12(5), 1143. https://doi.org/10.3390/diagnostics12051143





