Site-Specific Differences in Bone Mineral Density of Proximal Femur Correlate with the Type of Hip Fracture
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. QCT Scans
2.3. CTXA Measurements
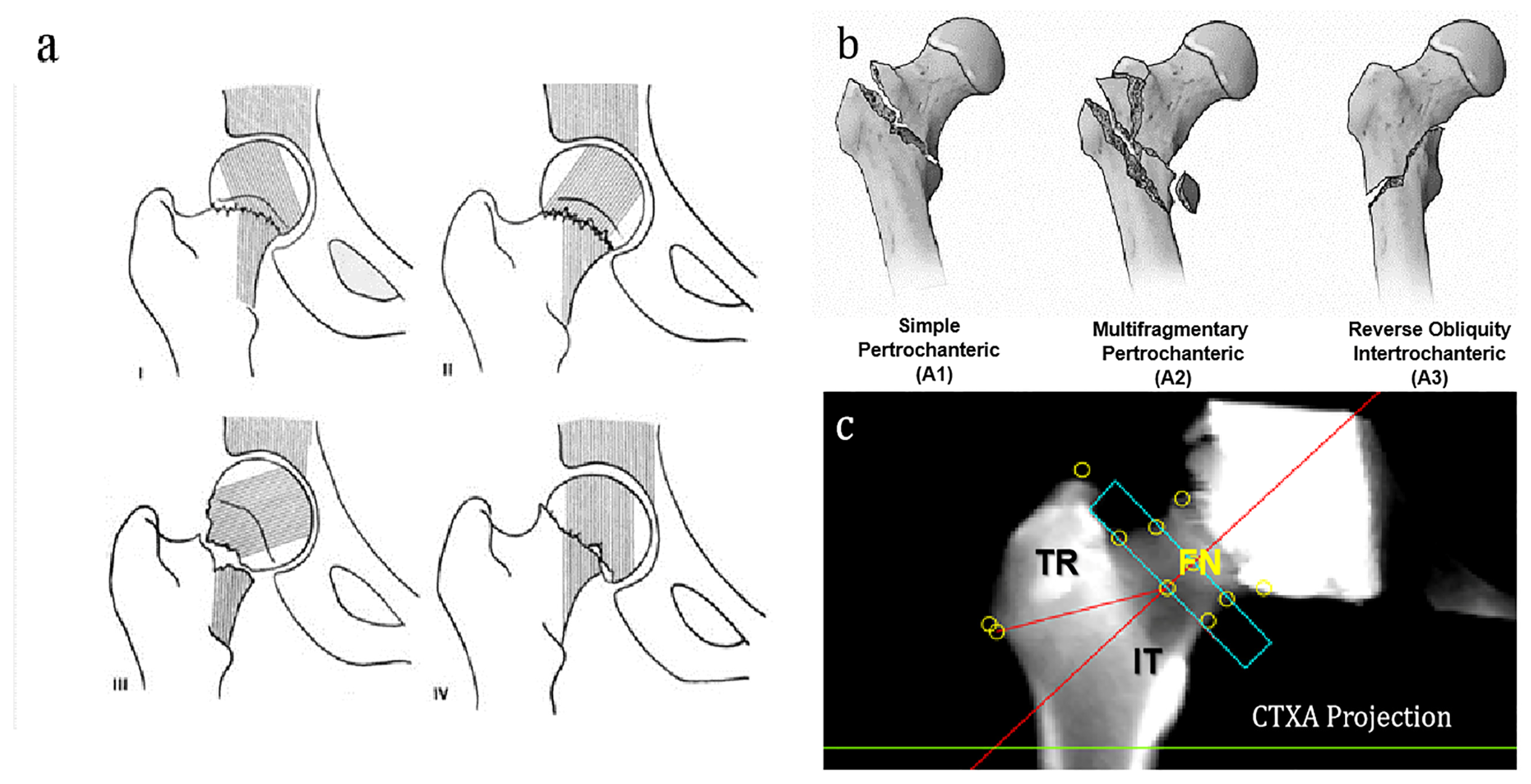
2.4. Subtypes of Neck and Trochanter Fractures
2.5. Statistics
3. Results
3.1. Characteristics of the Study Groups
3.2. CTXA Analysis by QCT
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cooper, C.; Campion, G. Melton, L.J., 3rd. Hip fractures in the elderly: A world-wide projection. Osteoporos. Int. 1992, 2, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.; Cole, Z.A.; Holroyd, C.R.; Earl, S.C.; Harvey, N.C.; Dennison, E.M.; Melton, L.J.; Cummings, S.R.; Kanis, J.A.; IOF CSA Working Group on Fracture Epidemiology. Secular trends in the incidence of hip and other osteoporotic fractures. Osteoporos. Int. 2011, 22, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Guerado, E.; Cruz, E.; Cano, J.R.; Crespo, P.V.; Alaminos, M.; Sánchez-Quevedo, M.C.; Campos, A. Bone mineral density aspects in the femoral neck of hip fracture patients. Injury 2016, 47 (Suppl. S1), S21–S24. [Google Scholar] [CrossRef] [PubMed]
- Garden, R.S. Reduction and fixation of subcapital fractures of the femur. Orthop. Clin. North Am. 1974, 5, 683–712. [Google Scholar] [CrossRef]
- Meinberg, E.G.; Agel, J.; Roberts, C.S.; Karam, M.D.; Kellam, J.F. Fracture and Dislocation Classification Compendium-2018. J. Orthop. Trauma 2018, 32 (Suppl. S1), S1–S170. [Google Scholar] [CrossRef]
- Gjertsen, J.E.; Dybvik, E.; Furnes, O.; Fevang, J.M.; Havelin, L.I.; Matre, K.; Engesæter, L.B. Improved outcome after hip fracture surgery in Norway. Acta Orthop. 2017, 88, 505–511. [Google Scholar] [CrossRef]
- Cauley, J.A.; Lui, L.Y.; Genant, H.K.; Salamone, L.; Browner, W.; Fink, H.A.; Cohen, P.; Hillier, T.; Bauer, D.C.; Cummings, S.R. Study of Osteoporotic Fractures Research Group. Risk factors for severity and type of the hip fracture. J. Bone Miner. Res. 2009, 24, 943–955. [Google Scholar] [CrossRef]
- Zhao, J.; Cai, Q.; Jiang, D.; Wang, L.; Chen, S.; Jia, W. The Associations of Serum Vitamin D and Bone Turnover Markers with the Type and Severity of Hip Fractures in Older Women. Clin. Interv. Aging 2020, 15, 1971–1978. [Google Scholar] [CrossRef]
- Rathbun, A.M.; Shardell, M.; Orwig, D.; Hebel, J.R.; Hicks, G.E.; Beck, T.; Hochberg, M.C.; Magaziner, J. Differences in the trajectory of bone mineral density change measured at the total hip and femoral neck between men and women following hip fracture. Arch. Osteoporos. 2016, 11, 9. [Google Scholar] [CrossRef]
- Bouxsein, M.L.; Eastell, R.; Lui, L.Y.; Wu, L.A.; de Papp, A.E.; Grauer, A.; Marin, F.; Cauley, J.A.; Bauer, D.C.; Black, D.M.; et al. Change in Bone Density and Reduction in Fracture Risk: A Meta-Regression of Published Trials. J. Bone Miner. Res. 2019, 34, 632–642. [Google Scholar] [CrossRef]
- Lang, T.F.; Keyak, J.H.; Heitz, M.W.; Augat, P.; Lu, Y.; Mathur, A.; Genant, H.K. Volumetric quantitative computed tomography of the proximal femur: Precision and relation to bone strength. Bone 1997, 21, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Lv, H.C.; Liu, J.H.; Cui, X.; Sun, G.F.; Hu, J.W.; Zhang, L.C.; Tang, P.F. Differences in Bone Mineral Density and Hip Geometry in Trochanteric and Cervical Hip Fractures in Elderly Chinese Patients. Orthop. Surg. 2019, 11, 263–269. [Google Scholar] [CrossRef] [PubMed]
- Gnudi, S.; Malavolta, N.; Testi, D.; Viceconti, M. Differences in proximal femur geometry distinguish vertebral from femoral neck fractures in osteoporotic women. Br. J. Radiol. 2004, 77, 219–223. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Museyko, O.; Su, Y.; Brown, K.; Yang, R.; Zhang, Y.; Duanmu, Y.; Guo, Z.; Zhang, W.; Yan, D.; et al. QCT of the femur: Comparison between QCTPro CTXA and MIAF Femur. Bone 2019, 120, 262–270. [Google Scholar] [CrossRef]
- Wang, L.; Cheng, X.G.; Su, Y.B.; Brown, K.; Xu, L.; Li, K.; Zhang, C.X.; Zhang, Y.; Duanmu, Y.Y.; Wu, X.B.; et al. Sex-related variations in cortical and trabecular bone of the femoral neck in an elderly Chinese population. Osteoporos. Int. 2017, 28, 2391–2399. [Google Scholar] [CrossRef]
- Khoo, B.C.C.; Cheng, X.G.; Brown, K.; Lewis, J.R.; Su, Y.B.; Guo, Z.; Li, K.; Prince, R.L. Differences in femoral neck structure between elderly Caucasian and Chinese populations: A cross-sectional study of Perth-Beijing cohorts. Arch. Osteoporos. 2017, 12, 72. [Google Scholar] [CrossRef]
- Cheng, X.; Wang, L.; Wang, Q.; Ma, Y.; Su, Y.; Li, K. Validation of quantitative computed tomography-derived areal bone mineral density with dual energy X-ray absorptiometry in an elderly Chinese population. Chin. Med. J. Engl. 2014, 127, 1445–1449. [Google Scholar]
- Von Kroge, S.; Stürznickel, J.; Bechler, U.; Stockhausen, K.E.; Eissele, J.; Hubert, J.; Amling, M.; Beil, F.T.; Busse, B.; Rolvien, T. Impaired bone quality in the superolateral femoral neck occurs independent of hip geometry and bone mineral density. Acta Biomater. 2022, 141, 233–243. [Google Scholar] [CrossRef]
- Su, Y.B.; Wang, L.; Wu, X.B.; Yi, C.; Yang, M.H.; Yan, D.; Cheng, K.B.; Cheng, X.G. The spatial differences in bone mineral density and hip structure between low-energy femoral neck and trochanteric fractures in elderly Chinese using quantitative computed tomography. Bone 2019, 124, 62–68. [Google Scholar] [CrossRef]
- Yu, A.; Carballido-Gamio, J.; Wang, L.; Lang, T.F.; Su, Y.; Wu, X.; Wang, M.; Wei, J.; Yi, C.; Cheng, X. Spatial Differences in the Distribution of Bone Between Femoral Neck and Trochanteric Fractures. J. Bone Miner. Res. 2017, 32, 1672–1680. [Google Scholar] [CrossRef]
- Taylor, M.; Perilli, E.; Martelli, S. Development of a surrogate model based on patient weight, bone mass and geometry to predict femoral neck strains and fracture loads. J. Biomech. 2017, 55, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Aldieri, A.; Bhattacharya, P.; Paggiosi, M.; Eastell, R.; Audenino, A.L.; Bignardi, C.; Morbiducci, U.; Terzini, M. Improving the Hip Fracture Risk Prediction with a Statistical Shape-and-Intensity Model of the Proximal Femur. Ann. Biomed. Eng. 2022, 50, 211–221. [Google Scholar] [CrossRef] [PubMed]
- Johannesdottir, F.; Poole, K.E.; Reeve, J.; Siggeirsdottir, K.; Aspelund, T.; Mogensen, B.; Jonsson, B.Y.; Sigurdsson, S.; Harris, T.B.; Gudnason, V.G.; et al. Distribution of cortical bone in the femoral neck and hip fracture: A prospective case-control analysis of 143 incident hip fractures; the AGES-REYKJAVIK Study. Bone 2011, 48, 1268–1276. [Google Scholar] [CrossRef] [PubMed]
- Duboeuf, F.; Hans, D.; Schott, A.M.; Kotzki, P.O.; Favier, F.; Marcelli, C.; Meunier, P.J.; Delmas, P.D. Different morphometric and densitometric parameters predict cervical and trochanteric hip fracture: The EPIDOS Study. J. Bone Miner. Res. 1997, 12, 1895–1902. [Google Scholar] [CrossRef] [PubMed]
- Hey, H.W.; Sng, W.J.; Lim, J.L.; Tan, C.S.; Gan, A.T.; Ng, J.H.; Kagda, F.H. Interpretation of hip fracture patterns using areal bone mineral density in the proximal femur. Arch Orthop. Trauma Surg. 2015, 135, 164716–164753. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.C.; Wang, C.J.; Shyu, Y.I. Variations in bone mineral density of proximal femora of elderly people with hip fractures: A case-control analysis. J. Trauma 2011, 71, 1720–1725. [Google Scholar] [CrossRef]
- Cho, Y.; Lee, I.; Ha, S.H.; Park, J.H.; Park, J.H. Comparison of hip subregion bone mineral density to the type of proximal femur fracture. Arch. Osteoporos. 2020, 15, 122. [Google Scholar] [CrossRef]
- Fox, K.M.; Cummings, S.R.; Williams, E.; Stone, K.; Study of Osteoporotic Fractures. Femoral neck and intertrochanteric fractures have different risk factors: A prospective study. Osteoporos. Int. 2000, 11, 1018–1023. [Google Scholar] [CrossRef]
- Feldman, F.; Robinovitch, S.N. Reducing hip fracture risk during sideways falls: Evidence in young adults of the protective effects of impact to the hands and stepping. J. Biomech. 2007, 40, 2612–2618. [Google Scholar] [CrossRef]
- Rudman, K.E.; Aspden, R.M.; Meakin, J.R. Compression or tension? The stress distribution in the proximal femur. Biomed. Eng. Online 2006, 5, 12. [Google Scholar] [CrossRef]
- Szulc, P.; Duboeuf, F.; Schott, A.M.; Dargent-Molina, P.; Meunier, P.J.; Delmas, P.D. Structural determinants of hip fracture in elderly women: Re-analysis of the data from the EPIDOS study. Osteoporos. Int. 2006, 17, 231–236. [Google Scholar] [CrossRef] [PubMed]

| Characteristics (Mean ± SD) | Total (n = 593) | Nondisplaced FN Fracture (n = 87) | Displaced FN Fracture (n = 317) | Total FN Fracture (n = 404) | p-Value 1 | IT Fracture A1 (n = 76) | IT Fracture A2 (n = 90) | IT Fracture A3 (n = 23) | Total IT Fracture (n = 189) | p-Value 2 | p-Value 3 | p-Value 4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male, % (n) | 27.99 (166) | 24.14 (21) | 27.76 (88) | 26.98 (109) | 0.50 | 22.37 (17) | 27.78 (25) | 65.22 (15) | 30.16 (57) | <0.01 | <0.01 | 0.42 |
| Age (years) | 79.59 ± 7.62 | 77.67 ± 7.53 | 78.68 ± 7.70 | 78.46 ± 7.66 | 0.25 | 81.57 ± 6.84 | 82.55 ± 7.12 | 81.18 ± 6.80 | 81.99 ± 6.95 | 0.53 | <0.01 | <0.01 |
| Height (cm) | 161.50 ± 8.22 | 161.66 ± 7.86 | 161.89 ± 7.44 | 161.84 ± 7.52 | 0.71 | 160.08 ± 7.25 | 161.16 ± 6.93 | 161.57 ± 19.68 | 160.78 ± 9.54 | 0.06 | 0.15 | 0.34 |
| Weight (kg) | 60.68 ± 11.36 | 60.61 ± 11.93 | 60.86 ± 10.73 | 60.81 ± 10.99 | 0.71 | 57.58 ± 10.87 | 60.94 ± 12.85 | 67.26 ± 10.55 | 60.39 ± 12.14 | <0.01 | 0.02 | 0.73 |
| BMI (kg/m2) | 23.33 ± 5.44 | 23.18 ± 4.27 | 23.19 ± 3.58 | 23.19 ± 3.73 | 0.57 | 22.42 ± 3.67 | 23.38 ± 4.41 | 28.52 ± 19.26 | 23.65 ± 7.95 | 0.05 | 0.17 | 0.93 |
| Days from injury to emergency | 1.12 ± 1.49 | 1.25 ± 1.36 | 1.21 ± 1.59 | 1.22 ± 1.54 | 0.09 | 1.05 ± 1.55 | 0.67 ± 0.90 | 1.35 ± 2.05 | 0.91 ± 1.37 | 0.51 | 0.06 | 0.03 |
| Femoral neck–shaft angle | 45.86 ± 6.02 | 46.20 ± 5.57 | 46.69 ± 5.49 | 46.58 ± 5.51 | 0.69 | 44.57 ± 7.07 | 44.28 ± 6.71 | 43.74 ± 6.08 | 44.33 ± 6.75 | 0.74 | <0.01 | <0.01 |
| TH aBMD | 0.63 ± 0.16 | 0.64 ± 0.14 | 0.66 ± 0.16 | 0.66 ± 0.16 | 0.62 | 0.54 ± 0.13 | 0.59 ± 0.13 | 0.67 ± 0.17 | 0.58 ± 0.14 | <0.01 | <0.01 | <0.01 |
| TH vBMD | 223.56 ± 60.92 | 228.02 ± 58.09 | 232.52 ± 62.08 | 231.56 ± 61.20 | 0.66 | 194.25 ± 53.29 | 210.44 ± 54.23 | 231.18 ± 69.05 | 206.45 ± 56.80 | 0.05 | <0.01 | <0.01 |
| TH bone mass | 22.03 ± 9.26 | 22.17 ± 8.72 | 22.92 ± 9.94 | 22.76 ± 9.68 | 0.75 | 18.48 ± 7.72 | 20.57 ± 7.24 | 26.61 ± 9.64 | 20.46 ± 8.10 | <0.01 | <0.01 | 0.01 |
| FN aBMD | 0.54 ± 0.14 | 0.57 ± 0.14 | 0.55 ± 0.14 | 0.55 ± 0.14 | 0.35 | 0.48 ± 0.13 | 0.50 ± 0.13 | 0.54 ± 0.16 | 0.50 ± 0.14 | 0.02 | <0.01 | <0.01 |
| FN vBMD | 202.03 ± 48.01 | 204.68 ± 42.81 | 206.87 ± 46.46 | 206.40 ± 45.66 | 0.91 | 185.51 ± 44.57 | 197.2 ± 52.34 | 198.82 ± 67.71 | 192.70 ± 51.59 | 0.32 | 0.01 | <0.01 |
| FN bone mass | 1.86 ± 0.54 | 1.97 ± 0.60 | 1.89 ± 0.53 | 1.91 ± 0.55 | 0.33 | 1.65 ± 0.52 | 1.76 ± 0.51 | 2.01 ± 0.54 | 1.74 ± 0.53 | <0.01 | <0.01 | <0.01 |
| TR aBMD | 0.43 ± 0.12 | 0.44 ± 0.11 | 0.45 ± 0.12 | 0.45 ± 0.12 | 0.54 | 0.36 ± 0.10 | 0.38 ± 0.10 | 0.44 ± 0.14 | 0.38 ± 0.11 | 0.02 | <0.01 | <0.01 |
| TR vBMD | 140.88 ± 37.15 | 145.96 ± 33.85 | 148.05 ± 37.35 | 147.60 ± 36.59 | 0.76 | 121.15 ± 32.95 | 127.67 ± 32.14 | 139.62 ± 43.01 | 126.50 ± 34.23 | 0.11 | <0.01 | <0.01 |
| TR bone mass | 4.56 ± 1.77 | 4.85 ± 1.80 | 4.76 ± 1.73 | 4.78 ± 1.74 | 0.77 | 3.77 ± 1.80 | 4.10 ± 1.52 | 5.26 ± 1.90 | 4.11 ± 1.74 | <0.01 | <0.01 | <0.01 |
| IT aBMD | 0.76 ± 0.19 | 0.77 ± 0.16 | 0.79 ± 0.19 | 0.79 ± 0.18 | 0.54 | 0.65 ± 0.18 | 0.72 ± 0.16 | 0.82 ± 0.20 | 0.70 ± 0.18 | <0.01 | <0.01 | <0.01 |
| IT vBMD | 272.39 ± 78.07 | 278.41 ± 74.72 | 282.76 ± 79.12 | 281.82 ± 78.12 | 0.75 | 235.33 ± 72.76 | 258.25 ± 69.48 | 284.52 ± 85.28 | 252.23 ± 74.22 | 0.03 | <0.01 | <0.01 |
| IT bone mass | 15.35 ± 8.44 | 15.00 ± 8.23 | 16.10 ± 8.92 | 15.86 ± 8.78 | 0.36 | 12.62 ± 7.31 | 14.32 ± 6.99 | 19.30 ± 8.64 | 14.24 ± 7.57 | <0.01 | <0.01 | 0.06 |
| Muscle Parameters | Unadjusted Models | Adjusted Models 1 | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| IT fracture A1 vs. displaced FN fracture | ||||
| Femoral neck–shaft angle | 0.68 (0.52, 0.89) | <0.01 | 0.73 (0.55, 0.96) | 0.03 |
| TH aBMD | 0.43 (0.32, 0.58) | <0.01 | 0.42 (0.29, 0.59) | <0.01 |
| TH vBMD | 0.49 (0.36, 0.66) | <0.01 | 0.50 (0.36, 0.70) | <0.01 |
| TH bone mass | 0.53 (0.38, 0.75) | <0.01 | 0.57 (0.40, 0.81) | <0.01 |
| FN aBMD | 0.53 (0.39, 0.72) | <0.01 | 0.47 (0.32, 0.69) | <0.01 |
| FN vBMD | 0.60 (0.46, 0.79) | <0.01 | 0.65 (0.48, 0.87) | <0.01 |
| FN bone mass | 0.62 (0.48, 0.82) | <0.01 | 0.50 (0.34, 0.73) | <0.01 |
| TR aBMD | 0.41 (0.30, 0.56) | <0.01 | 0.40 (0.28, 0.57) | <0.01 |
| TR vBMD | 0.44 (0.32, 0.59) | <0.01 | 0.43 (0.31, 0.61) | <0.01 |
| TR bone mass | 0.51 (0.38, 0.69) | <0.01 | 0.46 (0.32, 0.66) | <0.01 |
| IT aBMD | 0.46 (0.34, 0.60) | <0.01 | 0.44 (0.32, 0.61) | <0.01 |
| IT vBMD | 0.51 (0.38, 0.68) | <0.01 | 0.52 (0.38, 0.72) | <0.01 |
| IT bone mass | 0.60 (0.43, 0.83) | <0.01 | 0.65 (0.47, 0.90) | 0.01 |
| IT fracture A1 vs. nondisplaced FN fracture | ||||
| Femoral neck–shaft angle | 0.78 (0.57, 1.05) | 0.10 | 0.83 (0.60, 1.15) | 0.26 |
| TH aBMD | 0.43 (0.29, 0.63) | <0.01 | 0.48 (0.32, 0.72) | <0.01 |
| TH vBMD | 0.51 (0.36, 0.74) | <0.01 | 0.57 (0.39, 0.83) | <0.01 |
| TH bone mass | 0.60 (0.42, 0.86) | 0.01 | 0.64 (0.44, 0.94) | 0.02 |
| FN aBMD | 0.51 (0.35, 0.72) | <0.01 | 0.52 (0.34, 0.78) | <0.01 |
| FN vBMD | 0.61 (0.43, 0.87) | 0.01 | 0.72 (0.49, 1.05) | 0.09 |
| FN bone mass | 0.59 (0.44, 0.81) | <0.01 | 0.53 (0.35, 0.80) | <0.01 |
| TR aBMD | 0.43 (0.30, 0.63) | <0.01 | 0.48 (0.32, 0.72) | <0.01 |
| TR vBMD | 0.45 (0.31, 0.65) | <0.01 | 0.49 (0.33, 0.73) | <0.01 |
| TR bone mass | 0.53 (0.37, 0.75) | <0.01 | 0.50 (0.34, 0.74) | <0.01 |
| IT aBMD | 0.44 (0.30, 0.64) | <0.01 | 0.47 (0.32, 0.71) | <0.01 |
| IT vBMD | 0.53 (0.37, 0.76) | <0.01 | 0.57 (0.39, 0.83) | <0.01 |
| IT bone mass | 0.72 (0.51, 1.00) | 0.05 | 0.75 (0.53, 1.06) | 0.11 |
| IT fracture A2 vs. displaced FN fracture | ||||
| Femoral neck–shaft angle | 0.64 (0.49, 0.83) | <0.01 | 0.63 (0.48, 0.82) | <0.01 |
| TH aBMD | 0.62 (0.48, 0.80) | <0.01 | 0.60 (0.44, 0.80) | <0.01 |
| TH vBMD | 0.68 (0.53, 0.88) | <0.01 | 0.68 (0.51, 0.90) | 0.01 |
| TH bone mass | 0.74 (0.56, 0.97) | 0.03 | 0.75 (0.56, 1.01) | 0.06 |
| FN aBMD | 0.73 (0.57, 0.93) | 0.01 | 0.68 (0.50, 0.93) | 0.01 |
| FN vBMD | 0.82 (0.65, 1.04) | 0.10 | 0.86 (0.67, 1.11) | 0.24 |
| FN bone mass | 0.82 (0.66, 1.02) | 0.07 | 0.76 (0.56, 1.02) | 0.07 |
| TR aBMD | 0.48 (0.36, 0.64) | <0.01 | 0.46 (0.33, 0.64) | <0.01 |
| TR vBMD | 0.54 (0.41, 0.71) | <0.01 | 0.53 (0.39, 0.72) | <0.01 |
| TR bone mass | 0.62 (0.47, 0.82) | <0.01 | 0.63 (0.46, 0.86) | <0.01 |
| IT aBMD | 0.66 (0.51, 0.85) | <0.01 | 0.65 (0.49, 0.87) | <0.01 |
| IT fracture A2 vs. nondisplaced FN fracture | ||||
| Femoral neck–shaft angle | 0.74 (0.55, 1.00) | 0.05 | 0.71 (0.51, 0.98) | 0.04 |
| TH aBMD | 0.63 (0.45, 0.89) | 0.01 | 0.73 (0.51, 1.05) | 0.09 |
| TH vBMD | 0.72 (0.52, 1.00) | 0.05 | 0.79 (0.56, 1.11) | 0.18 |
| TH bone mass | 0.77 (0.55, 1.07) | 0.12 | 0.83 (0.59, 1.18) | 0.30 |
| FN aBMD | 0.67 (0.50, 0.91) | 0.01 | 0.75 (0.52, 1.07) | 0.11 |
| FN vBMD | 0.87 (0.64, 1.17) | 0.34 | 1.01 (0.73, 1.40) | 0.95 |
| FN bone mass | 0.77 (0.59, 1.00) | 0.05 | 0.78 (0.55, 1.09) | 0.14 |
| TR aBMD | 0.49 (0.34, 0.71) | <0.01 | 0.56 (0.38, 0.84) | 0.01 |
| TR vBMD | 0.55 (0.39, 0.78) | <0.01 | 0.62 (0.43, 0.90) | 0.01 |
| TR bone mass | 0.59 (0.42, 0.83) | <0.01 | 0.64 (0.44, 0.93) | 0.02 |
| IT aBMD | 0.67 (0.48, 0.94) | 0.02 | 0.75 (0.52, 1.08) | 0.12 |
| Muscle Parameters | Unadjusted Models | Adjusted Models 1 | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| IT fracture A2 vs. IT fracture A1 | ||||
| Femoral neck–shaft angle | 0.97 (0.74, 1.27) | 0.82 | 0.92 (0.69, 1.24) | 0.60 |
| TH aBMD | 1.50 (1.05, 2.13) | 0.03 | 1.59 (1.05, 2.40) | 0.03 |
| TH vBMD | 1.42 (1.00, 2.02) | 0.05 | 1.47 (1.00, 2.16) | 0.05 |
| TH bone mass | 1.40 (0.95, 2.05) | 0.09 | 1.39 (0.93, 2.08) | 0.10 |
| FN aBMD | 1.28 (0.93, 1.75) | 0.13 | 1.39 (0.94, 2.07) | 0.10 |
| FN vBMD | 1.29 (0.95, 1.76) | 0.10 | 1.32 (0.94, 1.84) | 0.11 |
| FN bone mass | 1.25 (0.94, 1.66) | 0.13 | 1.39 (0.95, 2.05) | 0.09 |
| TR aBMD | 1.26 (0.87, 1.81) | 0.22 | 1.26 (0.83, 1.92) | 0.27 |
| TR vBMD | 1.26 (0.89, 1.79) | 0.19 | 1.32 (0.89, 1.97) | 0.17 |
| TR bone mass | 1.22 (0.90, 1.66) | 0.21 | 1.29 (0.91, 1.81) | 0.15 |
| IT aBMD | 1.53 (1.09, 2.14) | 0.01 | 1.64 (1.11, 2.41) | 0.01 |
| IT vBMD | 1.44 (1.02, 2.03) | 0.04 | 1.49 (1.03, 2.17) | 0.04 |
| IT bone mass | 1.31 (0.91, 1.88) | 0.14 | 1.26 (0.87, 1.83) | 0.23 |
| IT fracture A3 vs. IT fracture A1 | ||||
| Femoral neck–shaft angle | 0.94 (0.62, 1.41) | 0.75 | 0.92 (0.54, 1.58) | 0.77 |
| TH aBMD | 2.39 (1.40, 4.10) | <0.01 | 1.73 (0.96, 3.14) | 0.07 |
| TH vBMD | 2.06 (1.25, 3.40) | <0.01 | 1.65 (0.94, 2.92) | 0.08 |
| TH bone mass | 2.18 (1.30, 3.64) | <0.01 | 1.88 (1.03, 3.42) | 0.04 |
| FN aBMD | 1.80 (1.17, 2.74) | 0.01 | 1.37 (0.82, 2.30) | 0.23 |
| FN vBMD | 1.42 (0.93, 2.18) | 0.11 | 1.17 (0.71, 1.94) | 0.53 |
| FN bone mass | 2.11 (1.39, 3.19) | <0.01 | 1.70 (1.00, 2.89) | 0.05 |
| TR aBMD | 1.82 (1.12, 2.97) | 0.02 | 1.17 (0.66, 2.08) | 0.59 |
| TR vBMD | 1.73 (1.07, 2.80) | 0.02 | 1.21 (0.69, 2.13) | 0.51 |
| TR bone mass | 1.78 (1.15, 2.78) | 0.01 | 1.24 (0.73, 2.11) | 0.42 |
| IT aBMD | 2.44 (1.41, 4.22) | <0.01 | 1.80 (0.98, 3.30) | 0.06 |
| IT vBMD | 2.01 (1.22, 3.31) | 0.01 | 1.68 (0.95, 2.98) | 0.08 |
| IT bone mass | 1.98 (1.21, 3.23) | 0.01 | 1.86 (1.03, 3.36) | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, N.; Yuan, Y.; Yin, L.; Yang, M.; Liu, Y.; Zhang, W.; Ma, K.; Zhou, F.; Cheng, Z.; Wang, L.; et al. Site-Specific Differences in Bone Mineral Density of Proximal Femur Correlate with the Type of Hip Fracture. Diagnostics 2023, 13, 1877. https://doi.org/10.3390/diagnostics13111877
Li N, Yuan Y, Yin L, Yang M, Liu Y, Zhang W, Ma K, Zhou F, Cheng Z, Wang L, et al. Site-Specific Differences in Bone Mineral Density of Proximal Femur Correlate with the Type of Hip Fracture. Diagnostics. 2023; 13(11):1877. https://doi.org/10.3390/diagnostics13111877
Chicago/Turabian StyleLi, Ning, Yi Yuan, Lu Yin, Minghui Yang, Yandong Liu, Wenshuang Zhang, Kangkang Ma, Fengyun Zhou, Zitong Cheng, Ling Wang, and et al. 2023. "Site-Specific Differences in Bone Mineral Density of Proximal Femur Correlate with the Type of Hip Fracture" Diagnostics 13, no. 11: 1877. https://doi.org/10.3390/diagnostics13111877




