A Comprehensive Review on Alcohol Abuse Disorder Fatality, from Alcohol Binges to Alcoholic Cardiomyopathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
3. Results
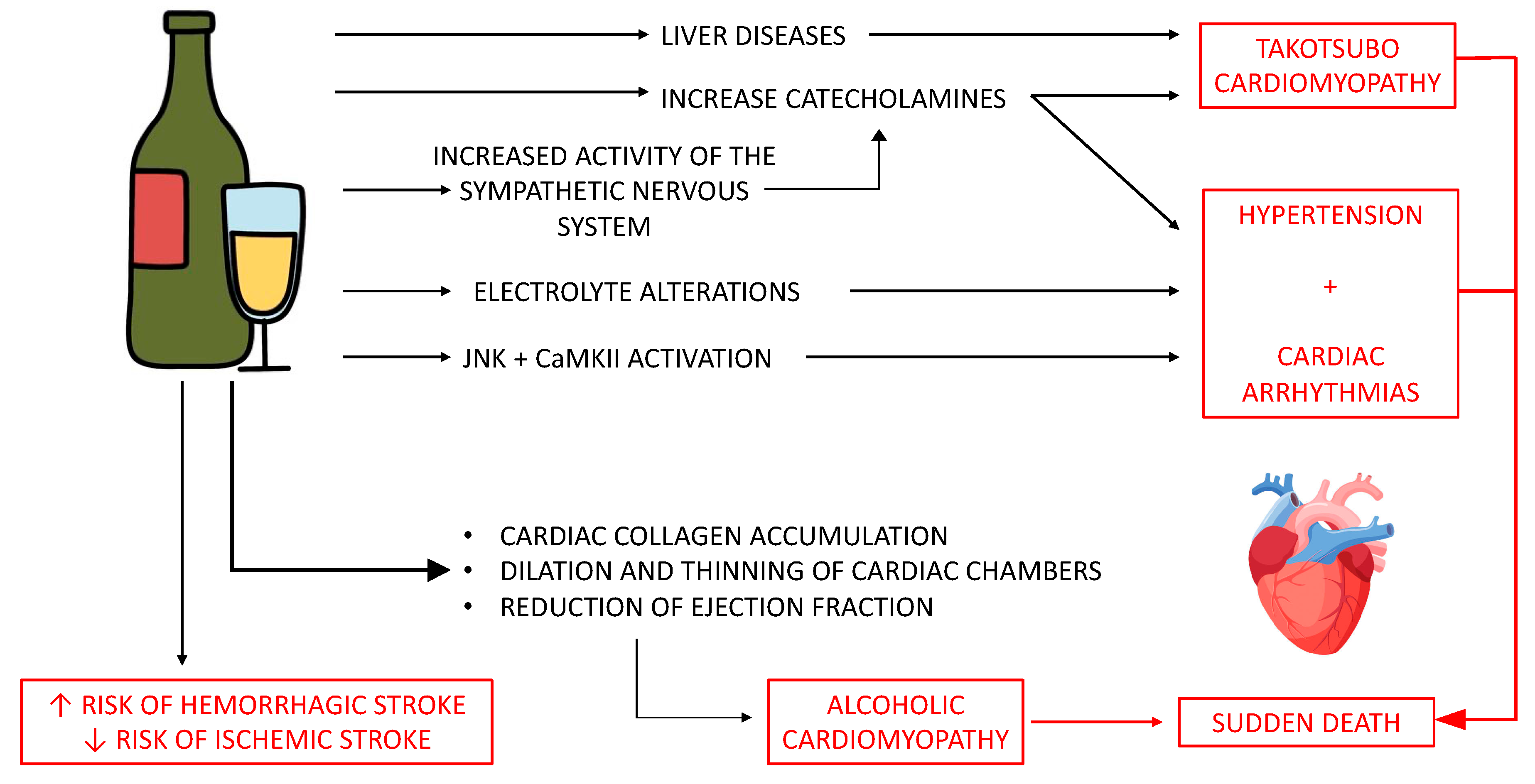
4. Discussion
4.1. Alcohol Consumption and Blood Pressure
4.2. Alcohol Consumption and Cardiac Arrhythmias
4.3. Alcohol Consumption and Sudden Death
4.4. Alcohol Consumption and Stroke
4.5. Alcohol Consumption and Takotsubo Cardiomyopathy
- Transient left ventricular systolic dysfunction (akinesia, dyskinesia or hypokinesia);
- Absence of coronary artery disease or rupture of atherosclerotic plaque. If coronary artery disease is identified, the wall anomalies observed must not be tributary areas of the coronary artery involved;
- New onset ECG abnormalities (ST elevation, T wave inversion, new shoulder blocks) or modest increase in cardiac troponin;
- Absence of pheochromocytoma (which would explain the high level of circulating catecholamines) or myocarditis.
4.6. Demographic Matters in Alcoholic Cardiomiopathy
5. Conclusions
6. Future Directions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Status Report on Alcohol and Health 2018. 2018. Available online: www.who.int/substance_abuse/publications/global_alcohol_report/en/ (accessed on 21 October 2023).
- Rehm, J.; Mathers, C.; Povova, S.; Thavorncharoensap, M.; Teerawattananon, Y.; Patra, J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009, 373, 2223–2233. [Google Scholar] [PubMed]
- Fernández-Solà, J. The Effects of Ethanol on the Heart: Alcoholic Cardiomyopathy. Nutrients 2020, 12, 572. [Google Scholar] [CrossRef] [PubMed]
- Szabo, G.; Lippai, D. Converging actions of alcohol on liver and brain immune signaling. Int. Rev. Neurobiol. 2014, 118, 359–380. [Google Scholar] [PubMed]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). Health risks and benefits of alcohol consumption. Alcohol Res. Health 2000, 24, 5–11. [Google Scholar]
- Day, E.; Rudd, J.H.F. Alcohol use disorders and the heart. Addiction 2019, 114, 1670–1678. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- O’Keefe, E.L.; DiNicolantonio, J.J.; O’Keefe, J.H.; Lavie, C.J. Alcohol and CV health: Jekyll and Hyde J-curves. Prog. Cardiovasc. Dis. 2018, 61, 68–75. [Google Scholar]
- Fernández-Solà, J. Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nat. Rev. Cardiol. 2015, 12, 576–587. [Google Scholar]
- Costanzo, S.; Di Castelnuovo, A.; Donati, M.B.; Iacoviello, L.; de Gaetano, G. Alcohol consumption and mortality in patients with cardiovascular disease: A meta-analysis. J. Am. Coll. Cardiol. 2010, 55, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- O’Keefe, J.H.; Bhatti, S.K.; Bajwa, A.; DiNicolantonio, J.J.; Lavie, C.J. Alcohol and cardiovascular health: The dose makes the poison…or the remedy. Mayo Clin. Proc. 2014, 89, 382–393. [Google Scholar] [CrossRef] [PubMed]
- Stătescu, C.; Clement, A.; Șerban, I.L.; Sascău, R. Consensus and Controversy in the Debate over the Biphasic Impact of Alcohol Consumption on the Cardiovascular System. Nutrients 2021, 13, 1076. [Google Scholar] [CrossRef] [PubMed]
- Knochel, J.P. Cardiovascular effects of alcohol. Ann. Intern. Med. 1983, 98 Pt 2, 849–854. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.K.; Regan, T.J. Alcoholic cardiomyopathy: Is it dose-dependent? Congest. Heart Fail. 2002, 8, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Piano, M.R.; Thur, L.A.; Hwang, C.L.; Phillips, S.A. Effects of Alcohol on the Cardiovascular System in Women. Alcohol Res. 2020, 40, 12. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Tobe, S.W.; Kaczorowski, J.; Bacon, S.L.; Vafaei, A.; Hasan, O.S.M.; Krishnan, R.J.; Raifu, A.O.; Rehm, J. Sex-Specific Associations Between Alcohol Consumption and Incidence of Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. J. Am. Heart Assoc. 2018, 7, e008202. [Google Scholar] [CrossRef] [PubMed]
- Davidson, D.M. Cardiovascular effects of alcohol. West. J. Med. 1989, 151, 430–439. [Google Scholar] [PubMed] [PubMed Central]
- Klatsky, A.L. Alcohol and cardiovascular diseases: Where do we stand today? J. Intern. Med. 2015, 278, 238–250. [Google Scholar] [CrossRef] [PubMed]
- Clark, L.T. Alcohol use and hypertension. Clinical considerations and implications. Postgrad. Med. 1984, 75, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Maisch, B. Alcoholic cardiomyopathy: The result of dosage and individual predisposition. Herz 2016, 41, 484–493. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Roerecke, M.; Kaczorowski, J.; Tobe, S.W.; Gmel, G.; Hasan, O.S.M.; Rehm, J. The effect of a reduction in alcohol consumption on blood pressure: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e108–e120. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Jung, M.-H.; Shin, E.-S.; Ihm, S.-H.; Jung, J.-G.; Lee, H.-Y.; Kim, C.-H. The effect of alcohol dose on the development of hypertension in Asian and Western men: Systematic review and meta-analysis. Korean J. Intern. Med. 2020, 35, 906. [Google Scholar] [CrossRef] [PubMed]
- Bulpitt, C.J. How many alcoholic drinks might benefit an older person with hypertension? Hypertension 2005, 23, 1947–1951. [Google Scholar] [CrossRef] [PubMed]
- Kloner, R.A.; Rezkalla, S.H. To drink or not to drink? That is the question. Circulation 2007, 116, 1306–1317. [Google Scholar] [CrossRef] [PubMed]
- Manolis, T.A.; Apostolopoulos, E.J.; Manolis, A.A.; Melita, H.; Manolis, A.S. The proarrhythmic conundrum of alcohol intake. Trends Cardiovasc. Med. 2022, 32, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, P.O.; Lyons, M.; Oldewurtel, H.A.; Regan, T.J. Cardiac conduction abnormalities produced by chronic alcoholism. Am. Heart J. 1976, 91, 66–78. [Google Scholar] [CrossRef] [PubMed]
- Giannopoulos, G.; Anagnostopoulos, I.; Kousta, M.; Vergopoulos, S.; Deftereos, S.; Vassilikos, V. Alcohol Consumption and the Risk of Incident Atrial Fibrillation: A Meta-Analysis. Diagnostics 2022, 12, 479. [Google Scholar] [CrossRef] [PubMed]
- Greenspon, A.J.; Schaal, S.F. The “holiday heart”: Electrophysiologic studies of alcohol effects in alcoholics. Ann. Intern. Med. 1983, 98, 135–139. [Google Scholar] [CrossRef] [PubMed]
- Fauchier, L. Alcoholic cardiomyopathy and ventricular arrhythmias. Chest 2003, 123, 1320. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Solà, J.; Planavila Porta, A. New Treatment Strategies for Alcohol-Induced Heart Damage. Int. J. Mol. Sci. 2016, 29, 1651. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, S.; Yousef, N.; Benjamin, M.M.; Sundararajan, S.; Wingert, R.; Wingert, M.; Mohammed, A.; Jahangir, A. Burden of arrhythmia and electrophysiologic procedures in alcoholic cardiomyopathy hospitalizations. Int. J. Cardiol. 2020, 304, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Bashour, T.T.; Fahdul, H.; Cheng, T.O. Electrocardiographic abnormalities in alcoholic cardiomyopathy. A study of 65 patients. Chest 1975, 68, 24–27. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.G.; Han, K.D.; Choi, J.I.; Boo, K.Y.; Kim, D.Y.; Lee, K.N.; Shim, J.; Kim, J.S.; Kim, Y.H. Frequent drinking is a more important risk factor for new-onset atrial fibrillation than binge drinking: A nationwide population-based study. EP Europace 2020, 22, 216–224. [Google Scholar] [CrossRef] [PubMed]
- Guzzo-Merello, G.; Dominguez, F.; González-López, E.; Cobo-Marcos, M.; Gomez-Bueno, M.; Fernandez-Lozano, I.; Millan, I.; Segovia, J.; Alonso-Pulpon, L.; Garcia-Pavia, P. Malignant ventricular arrhythmias in alcoholic cardiomyopathy. Int. J. Cardiol. 2015, 199, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Johansson, C.; Lind, M.M.; Eriksson, M.; Wennberg, M.; Andersson, J.; Johansson, L. Alcohol consumption and risk of incident atrial fibrillation: A population-based cohort study. Eur. J. Intern. Med. 2020, 76, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Hietanen, S.; Herajärvi, J.; Junttila, J.; Pakanen, L.; Huikuri, H.V.; Liisanantti, J. Characteristics of subjects with alcoholic cardiomyopathy and sudden cardiac death. Heart 2020, 106, 686–690. [Google Scholar] [CrossRef] [PubMed]
- Haukilahti, M.A.E.; Holmström, L.; Vähätalo, J.; Kenttä, T.; Tikkanen, J.; Pakanen, L.; Kortelainen, M.L.; Perkiömäki, J.; Huikuri, H.; Myerburg, R.J.; et al. Sudden Cardiac Death in Women. Circulation 2019, 139, 1012–1021. [Google Scholar] [CrossRef] [PubMed]
- Vikhert, A.M.; Tsiplenkova, V.G.; Cherpachenko, N.M. Alcoholic cardiomyopathy and sudden cardiac death. J. Am. Coll. Cardiol. 1986, 8 (Suppl. A), 3A–11A. [Google Scholar] [CrossRef] [PubMed]
- Guzzo-Merello, G.; Segovia, J.; Dominguez, F.; Cobo-Marcos, M.; Gomez-Bueno, M.; Avellana, P.; Millan, I.; Alonso-Pulpon, L.; Garcia-Pavia, P. Natural history and prognostic factors in alcoholic cardiomyopathy. JACC Heart Fail. 2015, 3, 78–86. [Google Scholar] [CrossRef] [PubMed]
- Laurent, D.; Edwards, J.G. Alcoholic Cardiomyopathy: Multigenic Changes Underlie Cardiovascular Dysfunction. J. Cardiol. Clin. Res. 2014, 2, 1022. [Google Scholar] [PubMed] [PubMed Central]
- Hookana, E.; Junttila, M.J.; Puurunen, V.P.; Tikkanen, J.T.; Kaikkonen, K.S.; Kortelainen, M.L.; Myerburg, R.J.; Huikuri, H.V. Causes of nonischemic sudden cardiac death in the current era. Heart Rhythm. 2011, 8, 1570–1575. [Google Scholar] [CrossRef] [PubMed]
- Mostofsky, E.; Chahal, H.S.; Mukamal, K.J.; Rimm, E.B.; Mittleman, M.A. Alcohol and Immediate Risk of Cardiovascular Events: A Systematic Review and Dose-Response Meta-Analysis. Circulation 2016, 133, 979–987. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Milić, S.; Lulić, D.; Štimac, D.; Ružić, A.; Zaputović, L. Cardiac manifestations in alcoholic liver disease. Postgrad. Med. J. 2016, 92, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Klatsky, A.L. Alcohol and cardiovascular health. Physiol. Behav. 2010, 100, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Angelini, P.; Uribe, C.; Tobis, J.M. Pathophysiology of Takotsubo Cardiomyopathy: Reopened Debate. Tex. Heart Inst. J. 2021, 48, e207490. [Google Scholar] [CrossRef] [PubMed]
- Luu, L.A.; Rawashdeh, B.; Goldaracena, N.; Agarwal, A.; McCracken, E.K.; Sahli, Z.T.; Oberholzer, J.; Pelletier, S.J. Hepatic Artery Thrombosis and Takotsubo Syndrome After Liver Transplantation—Which Came First? Am. J. Case Rep. 2020, 21, e920263. [Google Scholar] [CrossRef] [PubMed]
- Yeh, J.; Carroll, J. Takotsubo cardiomyopathy complicating acute pancreatitis: A case report. BMC Gastroenterol. 2021, 21, 134. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al Juboori, A.; Gautam, S.; Kaur, S. Diagnostic Dilemma of Takotsubo Cardiomyopathy in the Setting of Decompensated Cirrhosis. J. Clin. Gastroenterol. 2016, 50, 896. [Google Scholar] [CrossRef] [PubMed]
- Tomson, J.; Lip, G.Y. Alcohol and hypertension: An old relationship revisited. Alcohol Alcohol. 2006, 41, 3–4. [Google Scholar] [PubMed]
- Schoppet, M.; Maisch, B. Alcohol and the heart. Herz 2001, 26, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Brautbar, N.; Altura, B.M. Hypophosphatemia and hypomagnesemia result in cardiovascular dysfunction: Theoretical basis for alcohol-induced cellular injury. Alcohol Clin. Exp. Res. 1987, 11, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Koide, T.; Ozeki, K. The incidence of myocardial abnormalities in man related to the level of ethanol consumption. A proposal of a diagnostic criterion of alcoholic cardiomyopathy. Jpn. Heart J. 1974, 15, 337–348. [Google Scholar] [CrossRef] [PubMed]
- Husain, K.; Ansari, R.A.; Ferder, L. Alcohol-induced hypertension: Mechanism and prevention. World J. Cardiol. 2014, 6, 245–252. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mukamal, K.J.; Chiuve, S.E.; Rimm, E.B. Alcohol consumption and risk for coronary heart disease in men with healthy lifestyles. Arch. Intern. Med. 2006, 166, 2145–2150. [Google Scholar] [CrossRef] [PubMed]
- Regan, T.J.; Morvai, V. Experimental models for studying the effects of ethanol on the myocardium. Acta Medica Scand. Suppl. 1987, 717, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Vasdev, S.C.; Chakravarti, R.N.; Subrahmanyam, D.; Jain, A.C.; Wahi, P.L. Myocardial lesions induced by prolonged alcohol feeding in rhesus monkeys. Cardiovasc Res. 1975, 9, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Engel, T.R.; Luck, J.C. Effect of whiskey on atrial vulnerability and “holiday heart”. J. Am. Coll. Cardiol. 1983, 1, 816–818. [Google Scholar] [CrossRef] [PubMed]
- Triolo, V.; Spanò, M.; Buscemi, R.; Gioè, S.; Malta, G.; Čaplinskiene, M.; Vaiano, F.; Bertol, E.; Zerbo, S.; Albano, G.D.; et al. EtG Quantification in Hair and Different Reference Cut-Offs in Relation to Various Pathologies: A Scoping Review. Toxics 2022, 10, 682. [Google Scholar] [CrossRef] [PubMed]
- Shanoff, H.M. Alcoholic cardiomyopathy: An introductory review. Can. Med. Assoc. J. 1972, 106, 55–62. [Google Scholar] [PubMed] [PubMed Central]
- Cannizzaro, E.; Lavanco, G.; Castelli, V.; Cirrincione, L.; Di Majo, D.; Martines, F.; Argo, A.; Plescia, F. Alcohol and Nicotine Use among Adolescents: An Observational Study in a Sicilian Cohort of High School Students. Int. J. Environ. Res. Public Health 2022, 19, 6152. [Google Scholar] [CrossRef]
- Piano, M.R. Alcoholic Cardiomyopathy: Incidence, Clinical Characteristics, and Pathophysiology. Chest 2002, 121, 1638–1650. [Google Scholar] [CrossRef]
- Klatsky, A.L. Alcohol, cardiovascular diseases and diabetes mellitus. Pharmacol. Res. 2007, 55, 237–247. [Google Scholar] [CrossRef] [PubMed]
- Rubin, E. Cardiovascular effects of alcohol. Pharmacol. Biochem. Behav. 1980, 13 (Suppl. 1), 37–40. [Google Scholar] [CrossRef] [PubMed]
- McCall, D. Alcohol and the cardiovascular system. Curr. Probl. Cardiol. 1987, 12, 355–414. [Google Scholar] [CrossRef] [PubMed]
- Friedman, H.S. Cardiovascular effects of alcohol with particular reference to the heart. Alcohol 1984, 1, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Luca, C. Electrophysiological properties of right heart and atrioventricular conducting system in patients with alcoholic cardiomyopathy. Br. Heart J. 1979, 42, 274–281. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Spies, C.D.; Sander, M.; Stangl, K.; Fernandez-Sola, J.; Preedy, V.R.; Rubin, E.; Andreasson, S.; Hanna, E.Z.; Kox, W.J. Effects of alcohol on the heart. Curr. Opin. Crit. Care 2001, 7, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Douds, A.C.; Maxwell, J.D. Alcohol and the heart: Good and bad news. Addiction 1994, 89, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Van Noord, C.; Straus, S.M.; Sturkenboom, M.C.; Hofman, A.; Aarnoudse, A.J.; Bagnardi, V.; Kors, J.A.; Newton-Cheh, C.; Witteman, J.C.; Stricker, B.H. Psychotropic drugs associated with corrected QT interval prolongation. J. Clin. Psychopharmacol. 2009, 29, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Gambaro, V.; Argo, A.; Cippitelli, M.; Dell’Acqua, L.; Fare, F.; Froldi, R.; Guerrini, K.; Roda, G.; Rusconi, C.; Procaccianti, P. Unexpected variation of the codeine/morphine ratio following fatal heroin overdose. J. Anal. Toxicol. 2014, 38, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Gémes, K.; Malmo, V.; Laugsand, L.E.; Loennechen, J.P.; Ellekjaer, H.; László, K.D.; Ahnve, S.; Vatten, L.J.; Mukamal, K.J.; Janszky, I. Does Moderate Drinking Increase the Risk of Atrial Fibrillation? The Norwegian HUNT (Nord-Trøndelag Health) Study. J. Am. Heart Assoc. 2017, 6, e007094. [Google Scholar] [CrossRef] [PubMed]
- Sinagra, G.; Fabris, E.; Romani, S.; Negri, F.; Stolfo, D.; Brun, F.; Merlo, M. Dilated Cardiomyopathy at the Crossroad: Multidisciplinary Approach. In Dilated Cardiomyopathy: From Genetics to Clinical Management; Sinagra, G., Merlo, M., Pinamonti, B., Eds.; Springer: Cham, Switzerland, 2019; Chapter 15. [Google Scholar] [PubMed]
- Corović, N.; Duraković, Z.; Misigoj-Duraković, M. Dispersion of the corrected QT and JT interval in the electrocardiogram of alcoholic patients. Alcohol Clin. Exp. Res. 2006, 30, 150–154. [Google Scholar] [CrossRef] [PubMed]
- Roshchevskaya, I.M.; Smirnova, S.L.; Tsorin, I.B.; Stolyaruk, V.N.; Nadorova, A.V.; Vititnova, M.B.; Kolik, L.G.; Kryzhanovskii, S.A. Specific Features of Depolarization of the Left and Right Atria in Rats with Alcoholic Cardiomyopathy. Bull. Exp. Biol. Med. 2018, 165, 617–620. [Google Scholar] [CrossRef] [PubMed]
- Kryzhanovskii, S.A.; Kolik, L.G.; Tsorin, I.B.; Stolyaruk, V.N.; Vititnova, M.B.; Ionova, E.O.; Sorokina, A.V.; Durnev, A.D. Alcoholic Cardiomyopathy: Translation Model. Bull. Exp. Biol. Med. 2017, 163, 627–631. [Google Scholar] [CrossRef] [PubMed]
- Dundung, A.; Kumar, A.; Guria, R.T.; Preetam, M.; Tara, R.K.; Kumar, B.; Saba, M.K. Clinical profile and prognostic factors of alcoholic cardiomyopathy in tribal and non-tribal population. Open Heart 2020, 7, e001335, Erratum in Open Heart 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Guerrini, K.; Argo, A.; Borroni, C.; Catalano, D.; Dell’Acqua, L.; Farè, F.; Procaccianti, P.; Roda, G.; Gambaro, V. Development and validation of a reliable method for studying the distribution pattern for opiates metabolites in brain. J. Pharm. Biomed. Anal. 2013, 73, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Okojie, O.M.; Javed, F.; Chiwome, L.; Hamid, P. Hypertension and Alcohol: A Mechanistic Approach. Cureus 2020, 12, e10086. [Google Scholar] [CrossRef]
- Kajander, O.A.; Kupari, M.; Laippala, P.; Savolainen, V.; Pajarinen, J.; Penttilä, A.; Karhunen, P.J. Dose dependent but non-linear effects of alcohol on the left and right ventricle. Heart 2001, 86, 417–423. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ahmed, A.N.; Elton, R.A.; Busuttil, A. Assessment of myocardial vasculature in chronic alcoholics without established cardiomyopathy. Int. J. Leg. Med. 1996, 109, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Cannizzaro, C.; Malta, G.; Antonina, A.; Brancato, A.; Roda, G.; Casagni, E.; Fumagalli, L.; Valoti, E.; Froldi, R.; Procaccianti, P.; et al. Behavioural and pharmacological characterization of a novel cannabinomimetic adamantane-derived indole, APICA, and considerations on the possible misuse as a psychotropic spice abuse, in C57bl/6J mice. Forensic Sci. Int. 2016, 265, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Roda, G.; Liberti, V.; Arnoldi, S.; Argo, A.; Rusconi, C.; Suardi, S.; Gambaro, V. Capillary electrophoretic and extraction conditions for the analysis of Catha edulis FORKS active principles. Forensic Sci. Int. 2013, 228, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Boyd, B.; Solh, T. Takotsubo cardiomyopathy: Review of broken heart syndrome. JAAPA 2020, 33, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Amin, H.Z.; Amin, L.Z.; Pradipta, A. Takotsubo Cardiomyopathy: A Brief Review. J. Med. Life 2020, 13, 3–7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, J.; Rao, Z.; Hong, F.; Agopian, V.; Nguyen-Lee, J.; Steadman, R.H.; Wray, C.; Xia, V.W. Takotsubo syndrome after liver transplantation: An association with intraoperatively administered epinephrine and fentanyl. Clin. Transplant. 2021, 35, e14463. [Google Scholar] [CrossRef] [PubMed]
- Shamaa, O.; Jafri, S.M.; Shamaa, M.T.; Brown, K.; Venkat, D. Takotsubo Cardiomyopathy Following Liver Transplantation: A Report of 2 Cases. Transplant. Proc. 2021, 53, 239–243. [Google Scholar] [CrossRef] [PubMed]
- Maestas, C.; Lazkani, M.; Sultan, M.; Kolli, G.; Sheikh, M.; Cherukuri, M. Severe takotsubo cardiomyopathy following orthotopic liver transplantation: A case series. Clin. Res. Hepatol. Gastroenterol. 2019, 43, e48–e53. [Google Scholar] [CrossRef] [PubMed]
- Van de Walle, S.O.; Gevaert, S.A.; Gheeraert, P.J.; De Pauw, M.; Gillebert, T.C. Transient stress-induced cardiomyopathy with an "inverted takotsubo" contractile pattern. Mayo Clin. Proc. 2006, 81, 1499–1502. [Google Scholar] [CrossRef] [PubMed]
- Hedjoudje, A.; Cervoni, J.P.; Patry, C.; Chatot, M.; Faivre, M.; Thévenot, T. Takotsubo cardiomyopathy triggered by delirium tremens in a cirrhotic patient with acute-on-chronic liver failure: A case report. Clin. Res. Hepatol. Gastroenterol. 2020, 44, e54–e58. [Google Scholar] [CrossRef] [PubMed]
- Doyen, D.; Dellamonica, J.; Moceri, P.; Moschietto, S.; Hyvernat, H.; Ferrari, E.; Bernardin, G. Tako-Tsubo cardiomyopathy presenting with cardiogenic shock successfully treated with milrinone: A case report. Heart Lung 2014, 43, 331–333. [Google Scholar] [CrossRef] [PubMed]
- Shaaban, A.; Gangwani, M.K.; Pendela, V.S.; Vindhyal, M.R. Alcoholic Cardiomyopathy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef]
- WHO, Global Health Observatory. Prevalence of Hypertension among Adults Aged 30–79 Years; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/data/gho/data/indicators/indicator-details/gho/prevalence-of-hypertension-among-adults-aged-30-79-years (accessed on 19 October 2023).
- Zhong, L.; Chen, W.; Wang, T.; Zeng, Q.; Lai, L.; Lai, J.; Lin, J.; Tang, S. Alcohol and Health Outcomes: An Umbrella Review of Meta-Analyses Base on Prospective Cohort Studies. Front. Public Health 2022, 10, 859947. [Google Scholar] [CrossRef] [PubMed]
- Daka, B.; Bennet, L.; Råstam, L.; Hellgren, M.I.; Li, Y.; Magnusson, M.; Lindblad, U. Association between self-reported alcohol consumption and diastolic dysfunction: A cross-sectional study. BMJ Open 2023, 13, e069937. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Ding, X.; Zhang, F.; Chen, L.; Luo, Q.; Xiao, M.; Liu, X.; Wu, Y.; Tang, W.; Qiu, J.; et al. Association between alcohol consumption and risk of stroke among adults: Results from a prospective cohort study in Chongqing, China. BMC Public Health 2023, 23, 1593. [Google Scholar] [CrossRef]
- Labaca, G.; Segura-García, L.; Álvarez, F.J.; Bosque-Prous, M. Differential health effects of alcoholic beverages: An umbrella review of observational studies. Rev. Esp. Salud Pública 2020, 94, e20201114. [Google Scholar]
- Tang, L.; Xu, T.; Li, H.; Zhang, M.; Wang, A.; Tong, W.; Xu, T.; Sun, Y.; Zhang, Y. Hypertension, alcohol drinking and stroke incidence: A population-based prospective cohort study among inner Mongolians in China. J. Hypertens. 2014, 32, 1091–1096; discussion 1096. [Google Scholar] [CrossRef] [PubMed]
- Batubo, N.P.; Moore, J.B.; Zulyniak, M.A. Dietary factors and hypertension risk in West Africa: A systematic review and meta-analysis of observational studies. J. Hypertens. 2023, 41, 1376–1388. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Vacca, A.; Bulfone, L.; Cicco, S.; Brosolo, G.; Da Porto, A.; Soardo, G.; Catena, C.; Sechi, L.A. Alcohol Intake and Arterial Hypertension: Retelling of a Multifaceted Story. Nutrients 2023, 15, 958. [Google Scholar] [CrossRef]
- Minzer, S.; Losno, R.A.; Casas, R. The Effect of Alcohol on Cardiovascular Risk Factors: Is There New Information? Nutrients 2020, 12, 912. [Google Scholar] [CrossRef]
- Attard, R.; Dingli, P.; Doggen, C.J.; Cassar, K.; Farrugia, R.; Bezzina Wettinger, S. The impact of frequency, pattern, intensity, and type of alcohol consumption, and its combined effect with smoking on inflammation, lipid profile, and the risk of myocardial infarction. J. Public Health 2021, 29, 611–624. [Google Scholar] [CrossRef]

| Mesh Terms | Authors | Study Design | N° Subjects | Outcomes |
|---|---|---|---|---|
| Alcohol consumption and blood pressure | O’Keefe, 2014 [11] | Review | /// | Drinking more than two drinks in a day raises the risk of hypertension. |
| Stătescu, 2021 [12] | Review | /// | Any daily amount of alcohol consumed, even minimal amounts, had no protective effects on blood pressure. | |
| Knochel, 1983 [13] | Review | /// | In chronic alcoholics without clinical evidence of heart disease, a blood ethanol level of 150 mg/dL elevated left ventricular end diastolic pressure and decreased stroke volume. | |
| Lee, 2002 [14] | Review | /// | Consumption of more than 40 g of ethanol per day increases blood pressure. Excessive alcohol consumption is responsible for 7% of all hypertension cases. | |
| Piano, 2020 [15] | Review | /// | In women the consumption of 1–2 drinks a day does not affect blood pressure levels. | |
| Roerecke, 2018 [16] | Systematic review and meta-analysis | 326,254 | Any alcohol consumed in men increases the risk of hypertension. In women, there was no risk of hypertension for consumption of 1 to 2 drinks/day. | |
| Davidson, 1989 [17] | Observational study | 83,947 | Male subjects who consumed <2 drinks per day had no increase in blood pressure levels compared with controls, while women who consumed <2 drinks per day had lower blood pressure values than controls. | |
| Klatsky, 2015 [18] | Review | /// | The hypertensive effect caused by alcohol disappears four days after the last intake. | |
| Clark, 1984 [19] | Review | /// | Women who drink alcohol in moderation have mean blood pressures that are lower than those of teetotalers. | |
| Husain, 2014 [20] | Review | /// | After a month of alcohol abstinence, a 7.2 mmHg drop in mean arterial pressure occurred in heavy drinkers. | |
| Roerecke, 2017 [21] | Systematic review and meta-analysis | 2865 | In individuals who consumed more than two drinks daily, reducing alcohol consumption was linked to a higher reduction in blood pressure. | |
| Jung, 2020 [22] | Systematic review and meta-analysis | 86,188 | Any alcohol consumption, even in quantities less than 20 g per day, is associated with an increased risk of hypertension. | |
| Bulpit, 2005 [23] | Review | /// | Systolic pressure decreased by 3.3 mmHg and diastolic pressure decreased by 2.0 mmHg with a 76% reduction in alcohol consumption. | |
| Kloner, 2007 [24] | Review | /// | There was a higher incidence of hypertension in individuals who drank three or more drinks per day. | |
| Alcohol consumption and cardiac arrhythmias | Manolis, 2022 [25] | Retrospective observational study | 47,002 | HR for AF of 1.38 when comparing participants consuming >7 drinks per week with abstainers. |
| Ettinger, 1976 [26] | Animals experimental study | /// | In guinea pigs, prolongation of the H–Q interval and the QRS complex reflects the duration of alcohol exposure and the quantity consumed. | |
| Giannopoulos, 2022 [27] | Meta-analysis | /// | Atrial fibrillation is the most frequent cardiac arrhythmia both in chronic alcohol consumers and in alcoholic binges. | |
| Greenspon, 1983 [28] | Human experimental study | 14 | In 71% of cases, consumption of 90 mL of 80-proof whiskey resulted in sustained or nonsustained atrial or ventricular tachyarrhythmias. | |
| Fauchier, 2003 [29] | Observational study | 75 | In patients with alcoholic cardiomyopathy, alcohol abstinence significantly reduces cardiac arrhythmic events. | |
| Fernàndez-Solà, 2016 [30] | Review | /// | The consumption of more than five drinks induces an acute decrease in myocyte contractility and arrhythmia and may cause sudden death. | |
| Sulaiman, 2020 [31] | Observational study | 75,430 | In patients with alcoholic cardiomyopathy, cardiac arrhythmias occur in 48% of cases, and 10% of cases are the cause of hospitalization. | |
| Bashour, 1975 [32] | Observational study | 65 | Premature ventricular contractions and first-degree atrioventricular blocks are the main ECG alterations in patients with alcoholic cardiomyopathy, occurring in 37% and 34% of cases, respectively. | |
| Kim, 2020 [33] | Observational study | 9,776,956 | The amount of alcohol taken during each drinking session was not an independent risk factor for new-onset atrial fibrillation. Still, frequent drinking and weekly alcohol intake were significant risk factors. | |
| Guzzo-Merello, 2015 [34] | Retrospective observational study | 94 | Ventricular arrhythmias did not occur in patients with alcoholic cardiomyopathy and ejection fraction > 40% or NYHA class 1. | |
| Johansson, 2020 [35] | Observational study | 109,230 | The consumption of increasing quantities of alcohol was associated with an increased risk of developing this cardiac arrhythmia. | |
| Alcohol consumption and sudden death | Hietanen, 2019 [36] | Retrospective observational study | 5869 | Of patients who died from alcoholic cardiomyopathy, 77.9% had never received a diagnosis of cardiac pathology. |
| Haukilahti, 2019 [37] | Retrospective observational study | 5869 | Alcoholic cardiomyopathy is responsible for 5.3% and 4% of sudden cardiac deaths in men and women, respectively. | |
| Vikhert, 1986 [38] | Observational study | 752 | Among subjects who died from sudden cardiac death, 17% had alcohol abuse, and the majority were under 50 years of age. | |
| Guzzo-Merello, 2015 [39] | Observational study | 282 | In this 59-month observational study, 8.5% of patients with alcoholic cardiomyopathy died due to sudden cardiac death. | |
| Laurent, 2022 [40] | Review | /// | Alcoholic cardiomyopathy is responsible for 16–19% of sudden cardiac deaths and is the leading cause of non-ischemic cardiac death in subjects aged 40–59 years. | |
| Hookana, 2011 [41] | Observational study | 2661 | A total of 19% of deaths from sudden cardiac death were caused by alcoholic cardiomyopathy, representing the second cause of death after obesity (23.7%). | |
| Alcohol consumption and stroke | O’Keefe, 2014 [11] | Observational study | 47,100 | In women, consuming more than or equal to 300 g of alcohol each week is linked to a two-fold increased risk of stroke. |
| Mostofsky, 2016 [42] | Systematic review and meta-analysis | 29,457 | The consumption of six drinks per week reduces the risk of ischemic stroke by 19%; however, there is a 2.25-fold risk of onset of ischemic stroke with the consumption of 19 drinks per week. | |
| Milic, 2016 [43] | Review | /// | Excessive alcohol consumption is associated with the onset of stroke-like episodes within 24 h, suggesting that excessive alcohol consumption may predispose to the risk of stroke and sudden death. | |
| Klatsky, 2010 [44] | Review | /// | There is a greater risk of hemorrhagic stroke in subjects who consume large quantities of alcohol than in those who drink small or medium quantities, probably caused by an increase in systemic blood pressure. | |
| Alcohol consumption and Takostubo cardiomyopthy | Angelini, 2021 [45] | /// | /// | In the scientific literature, there is no reference to a possible etiological role of alcohol consumption in Takotsubo cardiomyopathy. Liver disease and elevated circulating catecholamine levels were considered two probable etiological factors in Takotsubo cardiomyopathy. |
| Luu, 2020 [46] | ||||
| Yeh, 2021 [47] | ||||
| Al Juboori, 2016 [48] |
| Author | Epidemiology Data | Pathology Findings | Cardiac Sudden Death |
|---|---|---|---|
| Hietanen S, et al. [36] | subset of Fingesture cohort; period: 1998–2017, Northern Finland, autopsy study | Alcoholic cardiomyopathy | 4.9% of patient cohort |
| Hietanen S, et al. [36] | 5869 autopsies performed on subjects who died from sudden cardiac death | 77.9% of patients had never been diagnosed with a heart disease in life. The most present risk factors: hypertension, type 2 diabetes mellitus, and hypercholesterolemia. | |
| Corović N, et al. [73] | Clinical study of changes in the cardiovascular system of alcoholic patients admitted for control of their health status and evaluation of their working ability | Alcohol abuse is related to significantly higher dispersions of the QTc and JTc intervals and thus a significantly higher estimation of relative risk for prolonged QTc interval and higher QTc dispersion than the control group, i.e., higher risk of arrhythmias. | Alcohol-related cardiac arrhythmias are more often the cause of death, due to the prolongation of the QT interval, than are the consequences of coronary atherosclerosis. |
| Hookana E, et.al [41] | 2661 consecutive victims of SCD (Northern Finland) included in the study: autopsies plus available medical records and standardized questionnaires. | CM related to obesity, fibrotic CM, and alcoholic CM are commonly associated with nonischemic SCD. | Alcoholic CM accounted for (19.0%) of all SCD cases; alcoholic CM was the most common cause of death in subjects between 40 and 59 years of age (25.8%) |
| Roshchevskaya IM, et al. [74] | Animal model | Reduction in cardiac inotropic function was accompanied by dilation of the cardiac chambers | Electric instability, malignant heart rhythm disturbances |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Argo, A.; Pitingaro, W.; Puntarello, M.; Buscemi, R.; Malta, G.; D’Anna, T.; Albano, G.D.; Zerbo, S. A Comprehensive Review on Alcohol Abuse Disorder Fatality, from Alcohol Binges to Alcoholic Cardiomyopathy. Diagnostics 2024, 14, 1189. https://doi.org/10.3390/diagnostics14111189
Argo A, Pitingaro W, Puntarello M, Buscemi R, Malta G, D’Anna T, Albano GD, Zerbo S. A Comprehensive Review on Alcohol Abuse Disorder Fatality, from Alcohol Binges to Alcoholic Cardiomyopathy. Diagnostics. 2024; 14(11):1189. https://doi.org/10.3390/diagnostics14111189
Chicago/Turabian StyleArgo, Antonina, Walter Pitingaro, Maria Puntarello, Roberto Buscemi, Ginevra Malta, Tommaso D’Anna, Giuseppe Davide Albano, and Stefania Zerbo. 2024. "A Comprehensive Review on Alcohol Abuse Disorder Fatality, from Alcohol Binges to Alcoholic Cardiomyopathy" Diagnostics 14, no. 11: 1189. https://doi.org/10.3390/diagnostics14111189
APA StyleArgo, A., Pitingaro, W., Puntarello, M., Buscemi, R., Malta, G., D’Anna, T., Albano, G. D., & Zerbo, S. (2024). A Comprehensive Review on Alcohol Abuse Disorder Fatality, from Alcohol Binges to Alcoholic Cardiomyopathy. Diagnostics, 14(11), 1189. https://doi.org/10.3390/diagnostics14111189









