Higher Accuracy of Arthroscopy Compared to MRI in the Diagnosis of Chondral Lesions in Acute Ankle Fractures: A Prospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Patients
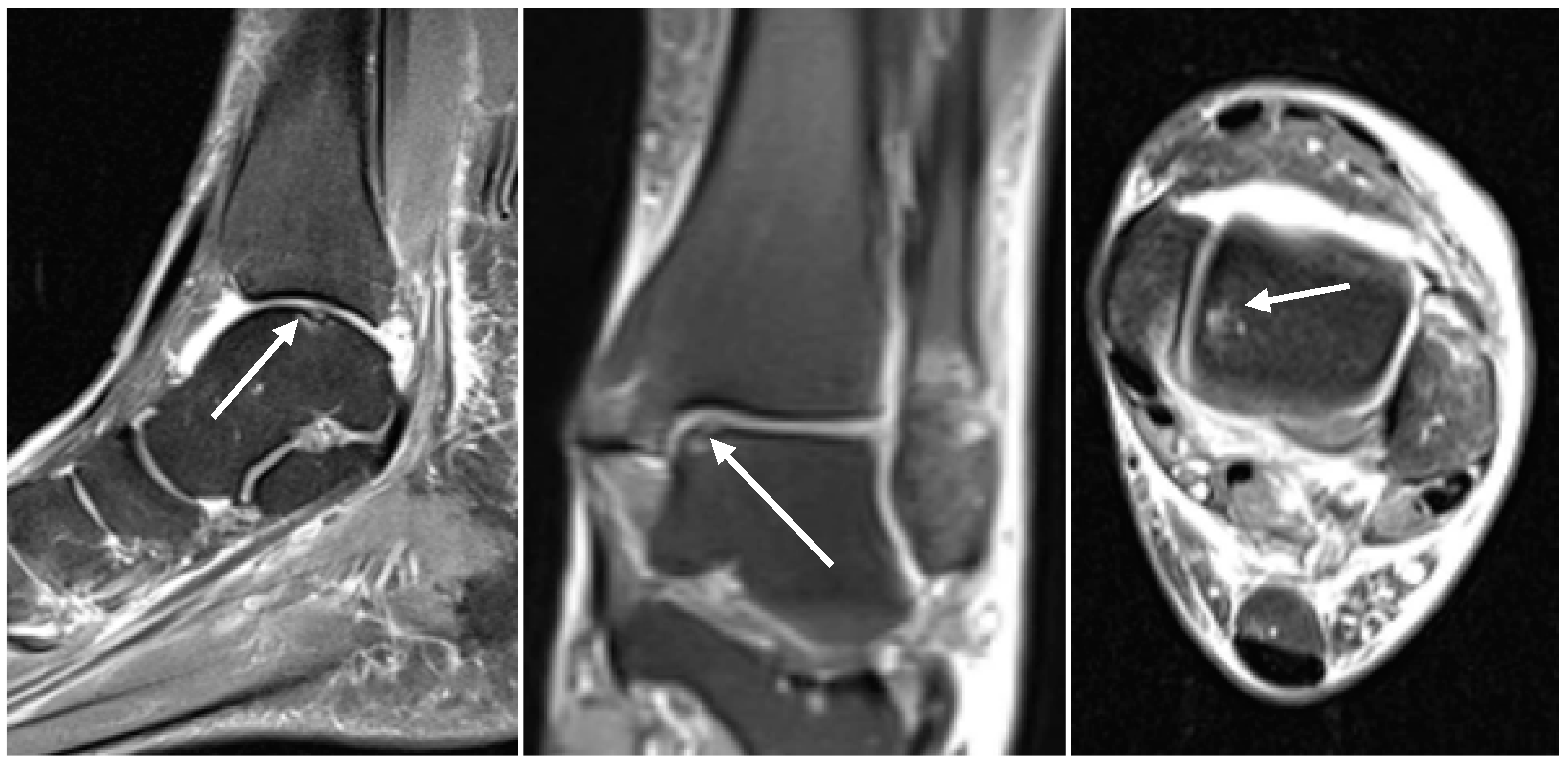
2.2. Radiological Assessment
2.3. Arthroscopic Evaluation
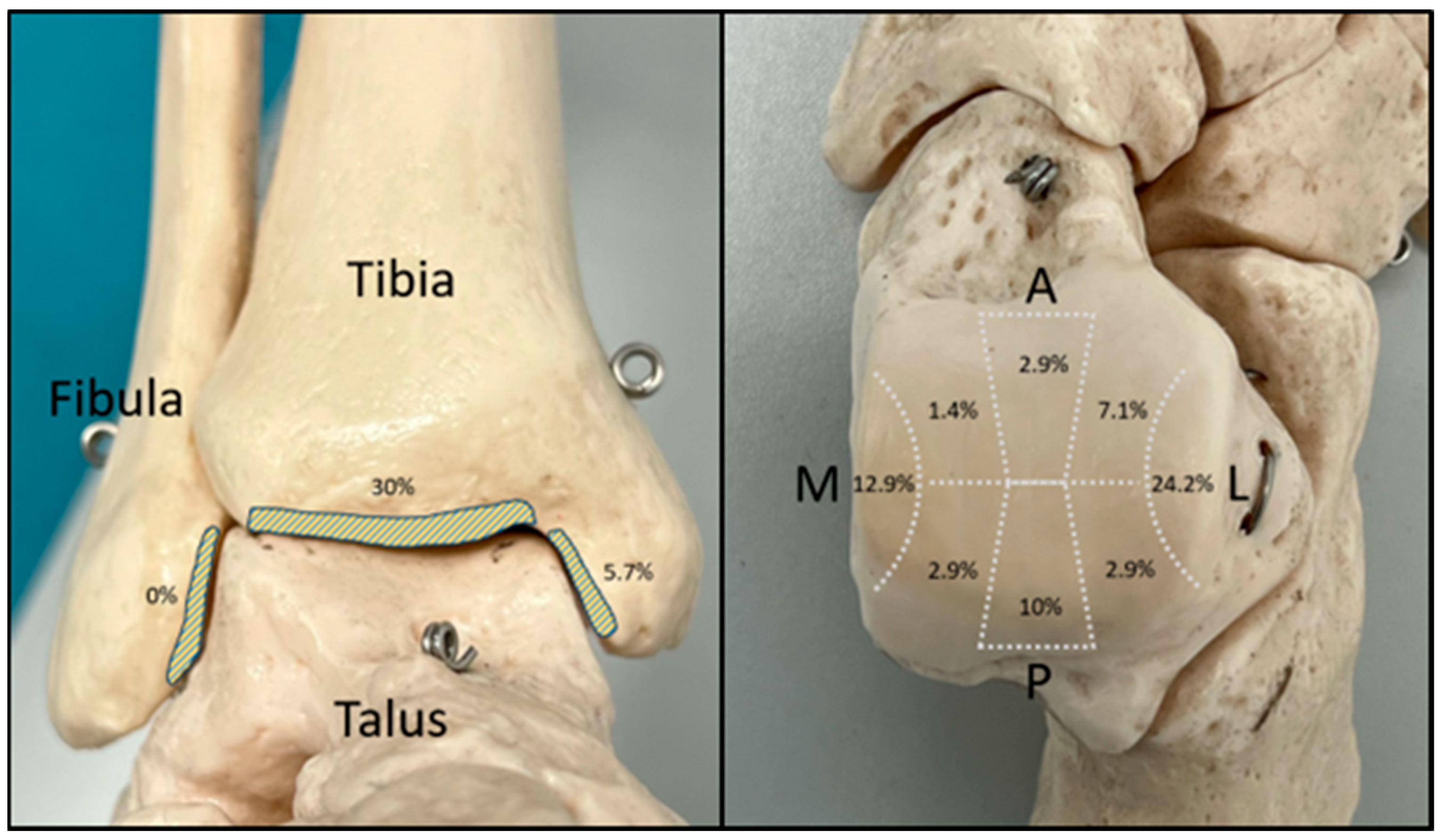
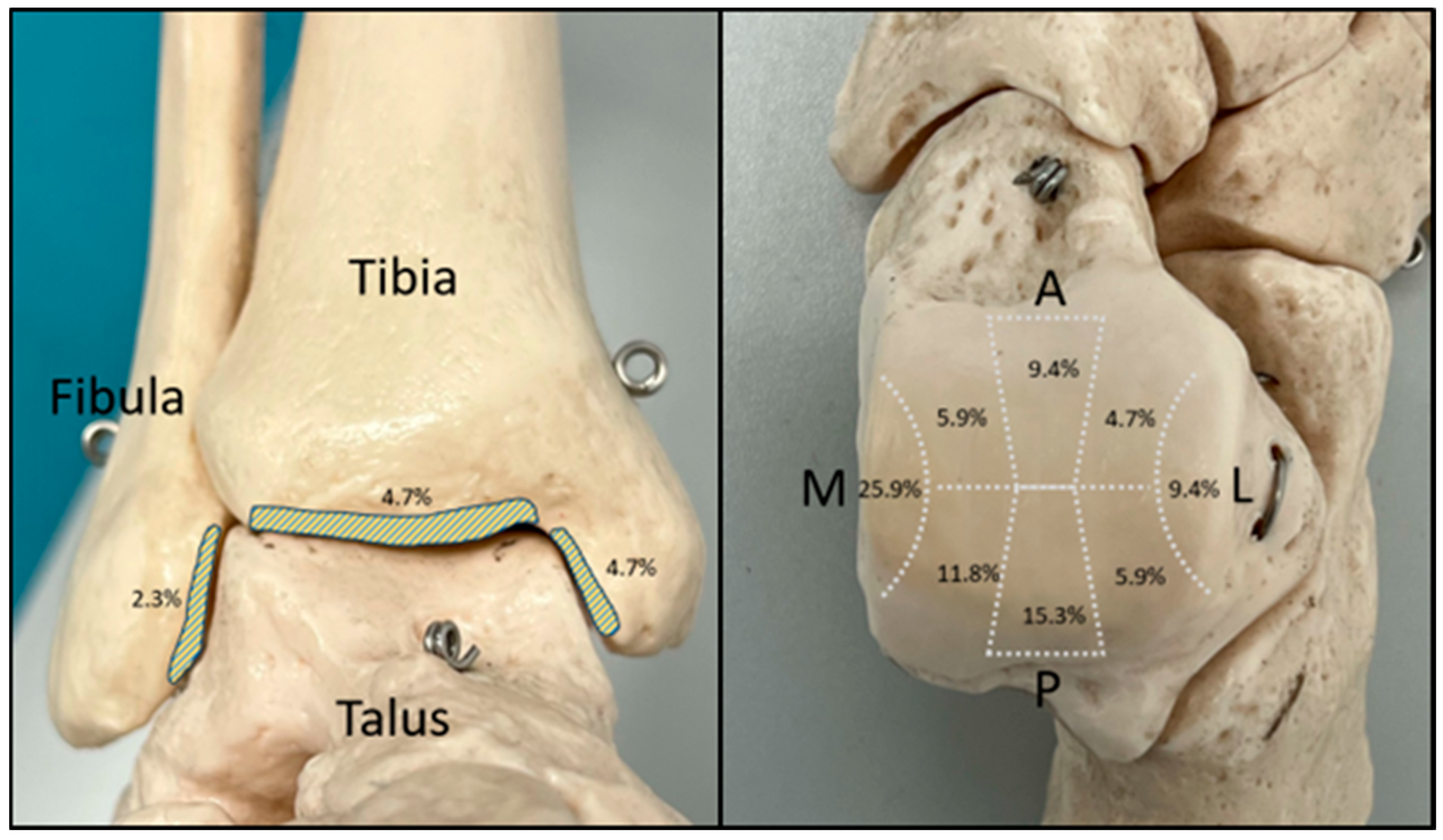
2.4. Assessment of Chondral Lesions
- -
- Grade 0: Normal.
- -
- Grade 1: Superficial lesions. Soft indentation (A) and/or superficial fissures and cracks (B).
- -
- Grade 2: Lesions extending down to <50% of cartilage depth.
- -
- Grade 3: Cartilage defects extending down to >50% of cartilage depth (A) as well as down to the calcified layer (B) and down to but not through the subchondral bone (C). Blisters are included in this grade (D).
- -
- Grade 4: Severely abnormal. Complete cartilage lesion with perforation of the subchondral plate.
2.5. Statistical Analysis
2.6. Ethics Approval
3. Results
3.1. Assessment of the Preoperative MRI Scans
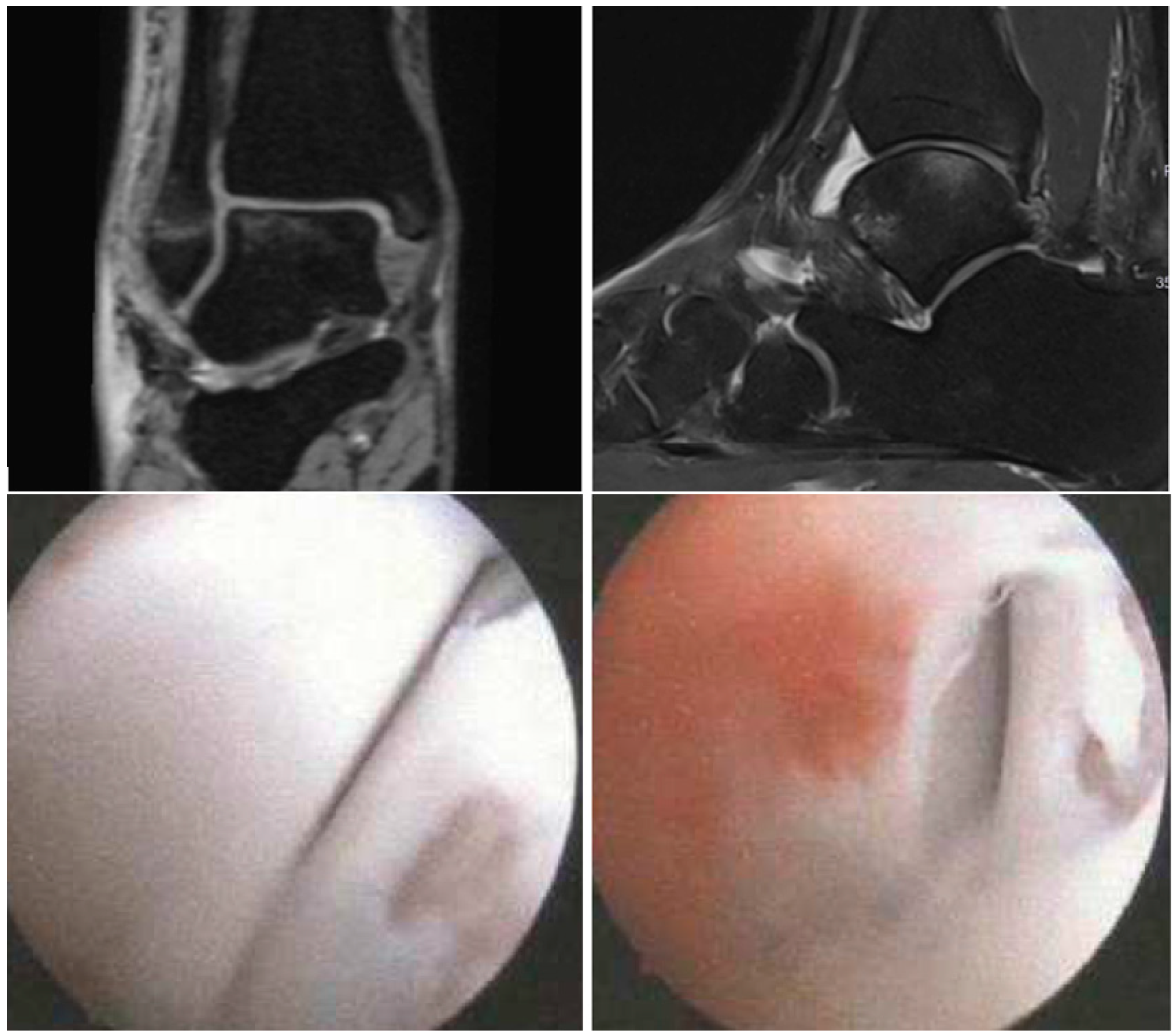
3.2. Evaluation of the Intraoperative Arthroscopic Findings
3.3. Validation
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Aktas, S.; Kocaoglu, B.; Gereli, A.; Nalbantodlu, U.; Guven, O. Incidence of chondral lesions of talar dome in ankle fracture types. Foot Ankle Int. 2008, 29, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Barro, D.; Escalante-Montes, P.K.; Contreras-Del Carmen, N.; Cortes-Aguirre, C.S.; Peralta-Ildefonso, D.; Hernández-Amaro, H.; Rojano-Mejía, D. Factors associated with functionality in patients with closed ankle fracture. Rev. Med. Inst. Mex. Seguro Soc. 2023, 61, 283–288. [Google Scholar] [PubMed]
- Gonzalez, T.A.; Macaulay, A.A.; Ehrlichman, L.K.; Drummond, R.; Mittal, V.; DiGiovanni, C.W. Arthroscopically Assisted Versus Standard Open Reduction and Internal Fixation Techniques for the Acute Ankle Fracture. Foot Ankle Int. 2016, 37, 554–562. [Google Scholar] [CrossRef]
- Kelemework, A.D.; Haile, A.W.; Bayable, S.D. Assessing the functional outcomes of ankle fracture and its predictive factors following surgical treatment at Addis Ababa burn, emergency, and trauma (AaBET) hospital, Addis Ababa, Ethiopia, 2021: A 5-year retrospective cross-sectional study. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 661–667. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, C.N.; Reilingh, M.L.; Zengerink, M.; van Bergen, C.J.A. Osteochondral defects in the ankle: Why painful? Knee Surg. Sports Traumatol. Arthrosc. Off. J. ESSKA 2010, 18, 570–580. [Google Scholar] [CrossRef] [PubMed]
- Cammas, C.; Ancion, A.; Detrembleur, C.; Tribak, K.; Putineanu, D.; Cornu, O. Frequency and risk factors of complications after surgical treatment of ankle fractures: A retrospective study of 433 patients. Acta Orthop. Belg. 2020, 86, 563–574. [Google Scholar] [PubMed]
- Williamson, E.R.C.; Shimozono, Y.; Toale, J.; Dankert, J.; Hurley, E.T.; Egol, K.A.; Kennedy, J.G. Incidence of Chondral and Osteochondral Lesions in Ankle Fracture Patients Identified With Ankle Arthroscopy Following Rotational Ankle Fracture: A Systematic Review. J. Foot Ankle Surg. 2022, 61, 668–673. [Google Scholar] [CrossRef] [PubMed]
- Leontaritis, N.; Hinojosa, L.; Panchbhavi, V.K. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J. Bone Jt. Surg. Am. 2009, 91, 333–339. [Google Scholar] [CrossRef] [PubMed]
- Stufkens, S.A.; Knupp, M.; Horisberger, M.; Lampert, C.; Hintermann, B. Cartilage lesions and the development of osteoarthritis after internal fixation of ankle fractures: A prospective study. J. Bone Jt. Surg. Am. 2010, 92, 279–286. [Google Scholar] [CrossRef] [PubMed]
- Herrera-Pérez, M.; Valderrabano, V.; Godoy-Santos, A.L.; de César Netto, C.; González-Martín, D.; Tejero, S. Ankle osteoarthritis: Comprehensive review and treatment algorithm proposal. EFORT Open Rev. 2022, 7, 448–459. [Google Scholar] [CrossRef] [PubMed]
- Martijn, H.A.; Lambers, K.T.A.; Dahmen, J.; Stufkens, S.A.S.; Kerkhoffs, G.M.M.J. High incidence of (osteo)chondral lesions in ankle fractures. Knee Surg. Sports Traumatol. Arthrosc. 2021, 29, 1523–1534. [Google Scholar] [CrossRef]
- Darwich, A.; Adam, J.; Dally, F.J.; Hetjens, S.; Jawhar, A. Incidence of concomitant chondral/osteochondral lesions in acute ankle fractures and their effect on clinical outcome: A systematic review and meta-analysis. Arch. Orthop. Trauma Surg. 2020, 141, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Boraiah, S.; Paul, O.; Parker, R.J.; Miller, A.N.; Hentel, K.D.; Lorich, D.G. Osteochondral lesions of talus associated with ankle fractures. Foot Ankle Int. 2009, 30, 481–485. [Google Scholar] [CrossRef] [PubMed]
- Elsner, K.S.; Milbich, J.; Giebel, G.; Hebestreit, H.P. Magnetic resonance tomography study of ankle joint fractures. A prospective pathologic-anatomic study. Unfallchirurg 1996, 99, 581–586. [Google Scholar]
- Smith, K.S.; Drexelius, K.; Challa, S.; Moon, D.K.; Metzl, J.A.; Hunt, K.J. Outcomes Following Ankle Fracture Fixation With or Without Ankle Arthroscopy. Foot Ankle Orthop. 2020, 5, 2473011420904046. [Google Scholar] [CrossRef] [PubMed]
- Baumbach, S.F.; Urresti-Gundlach, M.; Braunstein, M.; Borgmann, L.; Böcker, W.; Vosseller, J.T.; Polzer, H. Propensity Score–Matched Analysis of Arthroscopically Assisted Ankle Facture Treatment Versus Conventional Treatment. Foot Ankle Int. 2021, 42, 400–408. [Google Scholar] [CrossRef]
- Liu, C.; You, J.-X.; Yang, J.; Zhu, H.-F.; Yu, H.-J.; Fan, S.-W.; Li, H.-Y. Arthroscopy-Assisted Reduction in the Management of Isolated Medial Malleolar Fracture. Arthroscopy 2020, 36, 1714–1721. [Google Scholar] [CrossRef]
- Kortekangas, T.; Flinkkilä, T.; Niinimäki, J.; Lepojärvi, S.; Ohtonen, P.; Savola, O.; Pakarinen, H. Effect of Syndesmosis Injury in SER IV (Weber B)–Type Ankle Fractures on Function and Incidence of Osteoarthritis. Foot Ankle Int. 2015, 36, 180–187. [Google Scholar] [CrossRef]
- Mintz, D.N.; Tashjian, G.S.; Connell, D.A.; Deland, J.T.; O’Malley, M.; Potter, H.G. Osteochondral lesions of the talus: A new magnetic resonance grading system with arthroscopic correlation. Arthroscopy 2003, 19, 353–359. [Google Scholar] [CrossRef]
- Lee, K.B.; Bai, L.B.; Park, J.G.; Yoon, T.R. A comparison of arthroscopic and MRI findings in staging of osteochondral lesions of the talus. Knee Surg. Sports Traumatol. Arthrosc. 2008, 16, 1047–1051. [Google Scholar] [CrossRef]
- Bae, S.; Lee, H.K.; Lee, K.; Lim, S.; Rim, N.J.; Kim, J.S.; Cho, J. Comparison of arthroscopic and magnetic resonance imaging findings in osteochondral lesions of the talus. Foot Ankle Int. 2012, 33, 1058–1062. [Google Scholar] [CrossRef] [PubMed]
- Yasui, Y.; Wollstein, A.; Murawski, C.D.; Kennedy, J.G. Operative Treatment for Osteochondral Lesions of the Talus: Biologics and Scaffold-Based Therapy. Cartilage 2017, 8, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Choi, W.J.; Choi, G.W.; Kim, J.S.; Lee, J.W. Prognostic significance of the containment and location of osteochondral lesions of the talus: Independent adverse outcomes associated with uncontained lesions of the talar shoulder. Am. J. Sports Med. 2013, 41, 126–133. [Google Scholar] [CrossRef]
- Mak, K.H.; Chan, K.M.; Leung, P.C. Ankle fracture treated with the AO principle--an experience with 116 cases. Injury 1985, 16, 265–272. [Google Scholar] [CrossRef]
- Ferkel, R.D.; Zanotti, R.M.; Komenda, G.A.; Sgaglione, N.A.; Cheng, M.S.; Applegate, G.R.; Dopirak, R.M. Arthroscopic treatment of chronic osteochondral lesions of the talus: Long-term results. Am. J. Sports Med. 2008, 36, 1750–1762. [Google Scholar] [CrossRef]
- Brittberg, M.; Winalski, C.S. Evaluation of cartilage injuries and repair. J. Bone Jt. Surg. Am. 2003, 85 (Suppl. 2), 58–69. [Google Scholar] [CrossRef]
- Smith, G.D.; Taylor, J.; Almqvist, K.F.; Erggelet, C.; Knutsen, G.; Garcia Portabella, M.; Smith, T.; Richardson, J.B. Arthroscopic assessment of cartilage repair: A validation study of 2 scoring systems. Arthroscopy 2005, 21, 1462–1467. [Google Scholar] [CrossRef]
- Brittberg, M.; Peterson, L. Introduction of an articular cartilage classification. ICRS Newsl. 1998, 1, 5–8. [Google Scholar]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Darwich, A.; Nörenberg, D.; Adam, J.; Hetjens, S.; Schilder, A.; Obertacke, U.; Gravius, S.; Jawhar, A. A Multi-Disciplinary MRI Assessment May Optimize the Evaluation of Chondral Lesions in Acute Ankle Fractures: A Prospective Study. Diagnostics 2023, 13, 3220. [Google Scholar] [CrossRef]
- Schmid, M.R.; Pfirrmann, C.W.; Hodler, J.; Vienne, P.; Zanetti, M. Cartilage lesions in the ankle joint: Comparison of MR arthrography and CT arthrography. Skelet. Radiol. 2003, 32, 259–265. [Google Scholar] [CrossRef]
- Verhagen, R.A.; Maas, M.; Dijkgraaf, M.G.; Tol, J.L.; Krips, R.; van Dijk, C.N. Prospective study on diagnostic strategies in osteochondral lesions of the talus. Is MRI superior to helical CT? J. Bone Jt. Surg. Br. 2005, 87, 41–46. [Google Scholar] [CrossRef]
- Dipaola, J.D.; Nelson, D.W.; Colville, M.R. Characterizing osteochondral lesions by magnetic resonance imaging. Arthrosc. J. Arthrosc. Relat. Surg. 1991, 7, 101–104. [Google Scholar] [CrossRef]
- Elias, I.; Jung, J.W.; Raikin, S.M.; Schweitzer, M.W.; Carrino, J.A.; Morrison, W.B. Osteochondral lesions of the talus: Change in MRI findings over time in talar lesions without operative intervention and implications for staging systems. Foot Ankle Int. 2006, 27, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Yasui, Y.; Hannon, C.P.; Fraser, E.J.; Ackermann, J.; Boakye, L.; Ross, K.A.; Duke, G.L.; Shimozono, Y.; Kennedy, J.G. Lesion Size Measured on MRI Does Not Accurately Reflect Arthroscopic Measurement in Talar Osteochondral Lesions. Orthop. J. Sports Med. 2019, 7, 2325967118825261. [Google Scholar] [CrossRef]
- Campbell, A.B.; Knopp, M.V.; Kolovich, G.P.; Wei, W.; Jia, G.; Siston, R.A.; Flanigan, D.C. Preoperative MRI underestimates articular cartilage defect size compared with findings at arthroscopic knee surgery. Am. J. Sports Med. 2013, 41, 590–595. [Google Scholar] [CrossRef]
- Gomoll, A.H.; Yoshioka, H.; Watanabe, A.; Dunn, J.C.; Minas, T. Preoperative Measurement of Cartilage Defects by MRI Underestimates Lesion Size. Cartilage 2011, 2, 389–393. [Google Scholar] [CrossRef]
- Vallotton, J.A.; Meuli, R.A.; Leyvraz, P.F.; Landry, M. Comparison between magnetic resonance imaging and arthroscopy in the diagnosis of patellar cartilage lesions: A prospective study. Knee Surg. Sports Traumatol. Arthrosc. 1995, 3, 157–162. [Google Scholar] [CrossRef]
- Choi, W.J.; Park, K.K.; Kim, B.S.; Lee, J.W. Osteochondral lesion of the talus: Is there a critical defect size for poor outcome? Am. J. Sports Med. 2009, 37, 1974–1980. [Google Scholar] [CrossRef]
- Powers, R.T.; Dowd, T.C.; Giza, E. Surgical Treatment for Osteochondral Lesions of the Talus. Arthroscopy 2021, 37, 3393–3396. [Google Scholar] [CrossRef]
- Yasui, Y.; Shimozono, Y.; Hung, C.W.; Marangon, A.; Wollstein, A.; Gianakos, A.L.; Murawski, C.D.; Kennedy, J.G. Postoperative Reoperations and Complications in 32,307 Ankle Fractures With and Without Concurrent Ankle Arthroscopic Procedures in a 5-Year Period Based on a Large U.S. Healthcare Database. J. Foot Ankle Surg. 2019, 58, 6–9. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.J.; Patel, D. Imaging update on cartilage. J. Clin. Orthop. Trauma 2021, 22, 101610. [Google Scholar] [CrossRef] [PubMed]
- Krakowski, P.; Karpiński, R.; Jojczuk, M.; Nogalska, A.; Jonak, J. Knee MRI Underestimates the Grade of Cartilage Lesions. Appl. Sci. 2021, 11, 1552. [Google Scholar] [CrossRef]
- LaPrade, R.F.; Cram, T.R.; Mitchell, J.J.; Geeslin, A.G.; Lockard, C.A.; Fitzcharles, E.K.; Dornan, G.J. Axial-Oblique Versus Standard Axial 3-T Magnetic Resonance Imaging for the Detection of Trochlear Cartilage Lesions: A Prospective Study. Orthop. J. Sports Med. 2018, 6, 2325967118801009. [Google Scholar] [CrossRef] [PubMed]
- Danieli, M.V.; Guerreiro, J.P.; Queiroz, A.; Pereira, H.; Tagima, S.; Marini, M.G.; Cataneo, D.C. Diagnosis and classification of chondral knee injuries: Comparison between magnetic resonance imaging and arthroscopy. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 1627–1633. [Google Scholar] [CrossRef] [PubMed]
- Chopra, A.; Grainger, A.J.; Dube, B.; Evans, R.; Hodgson, R.; Conroy, J.; Macdonald, D.; Robinson, P. Comparative reliability and diagnostic performance of conventional 3T magnetic resonance imaging and 1.5T magnetic resonance arthrography for the evaluation of internal derangement of the hip. Eur. Radiol. 2018, 28, 963–971. [Google Scholar] [CrossRef]
- Cheng, Q.; Zhao, F.-C. Comparison of 1.5- and 3.0-T magnetic resonance imaging for evaluating lesions of the knee: A systematic review and meta-analysis (PRISMA-compliant article). Medicine 2018, 97, e12401. [Google Scholar] [CrossRef]


| Sequence | Fat-Saturated Proton-Density-Weighted Turbo Spin Echo (PD TSE) | T1-Weighted Turbo Spin Echo (T1 TSE) | T2-Weighted Turbo Spin Echo (T2 TSE) |
|---|---|---|---|
| Slice thickness (in mm) | 2 (coronal, sagittal) 3 (transversal) | 2 (coronal) | 3 (transversal) |
| TR (in ms) | 3470–4000 | 556 | 5000 |
| TE (in ms) | 40–47 | 12 | 73 |
| Field of view (FOV) (in cm) | 14 | 14 | 14 |
| Matrix | 512 × 384 | 512 × 384 | 512 × 384 |
| Number of CLs Detected | 1 | 2 | 3 | Total |
|---|---|---|---|---|
| Number of patients | 27 | 11 | 7 | 45 patients |
| Total | 70 CLs | |||
| Zone | Mean Size (mm2) | ICRS Classification | Subchondral Edema | Total | ||||
|---|---|---|---|---|---|---|---|---|
| 1a | 1b | 2 | 3a | 4 | ||||
| 1 | 23.78 | - | 1 | 4 | 2 | 2 | 2 | 9 |
| 2 | 40 | - | - | - | 1 | 1 | 1 | 2 |
| 3 | 14.86 | - | - | 3 | 4 | - | 3 | 7 |
| 4 | 17.5 | - | - | 1 | 1 | - | 0 | 2 |
| 5 | 13.71 | - | 2 | 6 | 9 | - | 7 | 17 |
| 6 | 11.4 | - | 1 | 2 | 2 | - | 3 | 5 |
| 7 | 9 | - | - | 1 | 1 | - | 0 | 2 |
| 8 | 35 | - | - | - | - | 1 | 0 | 1 |
| F1 | - | - | - | - | - | - | 0 | 0 |
| T1 | 26.75 | - | - | 1 | 2 | 1 | 1 | 4 |
| T2 | 36.81 | - | - | 3 | 5 | 13 | 19 | 21 |
| Total | 20.8 | 0 | 4 | 21 | 27 | 18 | 36 | 70 |
| Number of CLs Detected | 1 | 2 | 3 | 5 | 6 | 7 | 8 | Total |
|---|---|---|---|---|---|---|---|---|
| Number of patients | 30 | 9 | 2 | 2 | 1 | 1 | 1 | 46 patients |
| Total | 85 CLs | |||||||
| Zone | Mean Size (mm2) | ICRS Classification | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1a | 1b | 2 | 3a | 3b | 3c | 4 | |||
| 1 | 42.09 | - | - | 13 | 4 | - | 2 | 3 | 22 |
| 2 | 76.7 | 2 | - | 1 | 3 | - | 2 | 2 | 10 |
| 3 | 47.15 | - | 2 | 6 | 3 | - | - | 2 | 13 |
| 4 | 19.8 | - | 1 | - | 2 | - | - | 2 | 5 |
| 5 | 13.38 | 1 | 2 | 1 | 3 | 1 | - | - | 8 |
| 6 | 116.25 | - | - | - | 2 | - | - | 2 | 4 |
| 7 | 22.63 | 3 | 1 | 2 | 1 | - | - | 1 | 8 |
| 8 | 40.8 | - | - | - | 3 | 1 | - | 1 | 5 |
| F1 | 29.5 | 1 | - | - | - | - | - | 1 | 2 |
| T1 | 25.75 | 1 | - | - | - | - | - | 3 | 4 |
| T2 | 43.75 | - | 1 | 1 | - | 1 | - | 1 | 4 |
| Total | 43.4 | 8 | 7 | 24 | 21 | 3 | 4 | 18 | 85 |
| Zone | CL Identification | ICRS Classification | Size Evaluation | ||
|---|---|---|---|---|---|
| Kappa | p Value | Kappa | p Value | p Value | |
| 1 | 0.3825 | 0.0005 | 0.3196 | 0.3955 | <0.0001 |
| 2 | 0.1237 | 0.0114 | 0.1403 | 0.9576 | 0.0313 |
| 3 | 0.1919 | 0.1088 | 0.1768 | 0.8713 | 0.0108 |
| 4 | 0.2544 | 0.1797 | 0.1207 | 0.9473 | 0.2188 |
| 5 | 0.1905 | 0.0290 | 0.1094 | 0.9159 | 0.0991 |
| 6 | −0.0699 | 0.7389 | −0.0479 | 0.9856 | 0.4063 |
| 7 | 0.1605 | 0.0339 | 0.0741 | 0.8775 | 0.0273 |
| 8 | −0.0251 | 0.1025 | −0.0149 | 0.6767 | 0.2188 |
| T1 | 0.2031 | 1.000 | 0.0933 | 0.9311 | 0.9844 |
| T2 | 0.0679 | 0.0002 | 0.0650 | 0.2137 | 0.0004 |
| F1 | 0 | 0.1573 | 0 | 0.1573 | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Darwich, A.; Nörenberg, D.; Adam, J.; Hetjens, S.; Bdeir, M.; Schilder, A.; Thier, S.; Gravius, S.; Jawhar, A. Higher Accuracy of Arthroscopy Compared to MRI in the Diagnosis of Chondral Lesions in Acute Ankle Fractures: A Prospective Study. Diagnostics 2024, 14, 1810. https://doi.org/10.3390/diagnostics14161810
Darwich A, Nörenberg D, Adam J, Hetjens S, Bdeir M, Schilder A, Thier S, Gravius S, Jawhar A. Higher Accuracy of Arthroscopy Compared to MRI in the Diagnosis of Chondral Lesions in Acute Ankle Fractures: A Prospective Study. Diagnostics. 2024; 14(16):1810. https://doi.org/10.3390/diagnostics14161810
Chicago/Turabian StyleDarwich, Ali, Dominik Nörenberg, Julia Adam, Svetlana Hetjens, Mohamad Bdeir, Andreas Schilder, Steffen Thier, Sascha Gravius, and Ahmed Jawhar. 2024. "Higher Accuracy of Arthroscopy Compared to MRI in the Diagnosis of Chondral Lesions in Acute Ankle Fractures: A Prospective Study" Diagnostics 14, no. 16: 1810. https://doi.org/10.3390/diagnostics14161810
APA StyleDarwich, A., Nörenberg, D., Adam, J., Hetjens, S., Bdeir, M., Schilder, A., Thier, S., Gravius, S., & Jawhar, A. (2024). Higher Accuracy of Arthroscopy Compared to MRI in the Diagnosis of Chondral Lesions in Acute Ankle Fractures: A Prospective Study. Diagnostics, 14(16), 1810. https://doi.org/10.3390/diagnostics14161810






