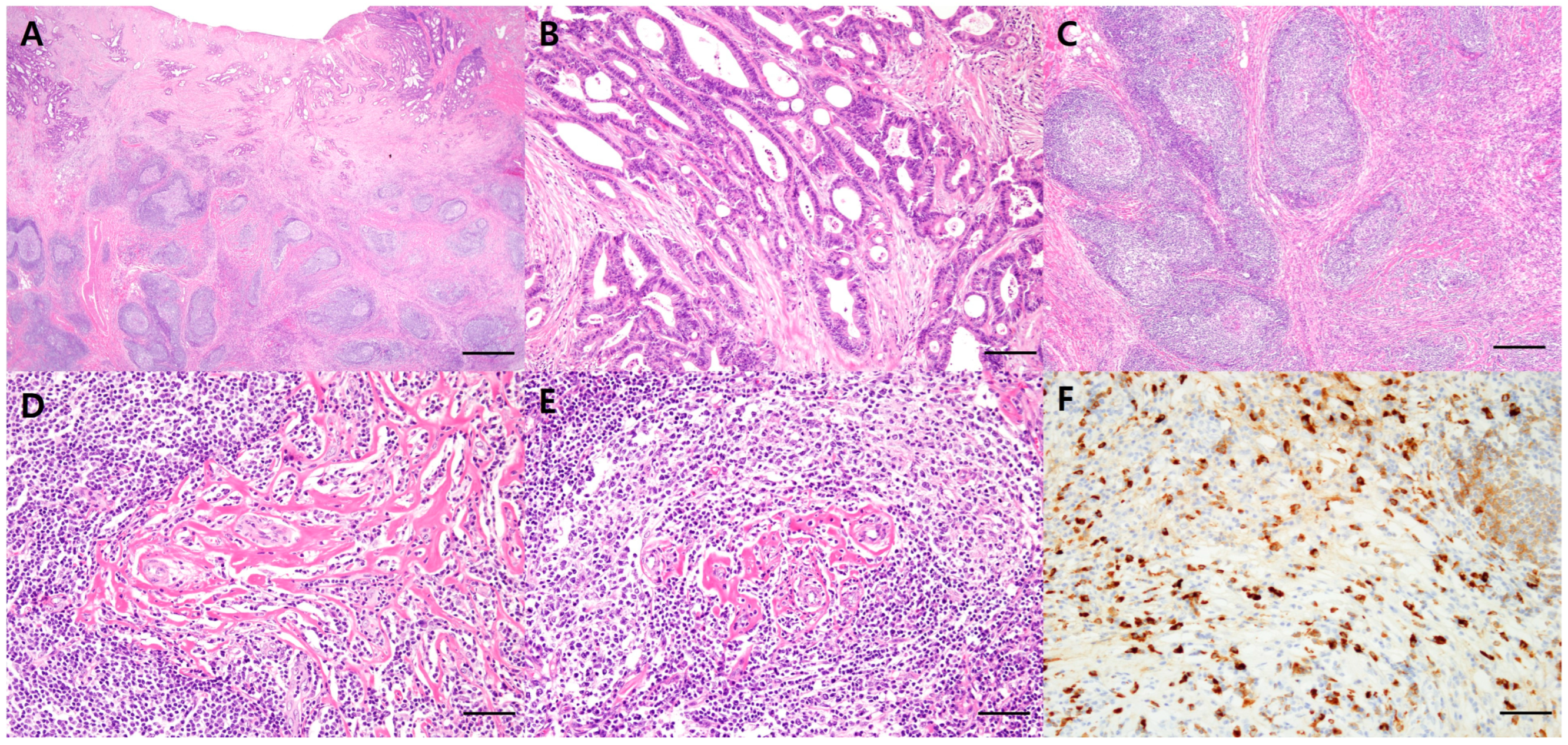
Coexistence of Colorectal Cancer and Immunoglobulin G4-Related Disease in the Same Lesion: A Rare Case with Molecular Classification
Abstract
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Deshpande, V.; Zen, Y.; Chan, J.K. Consensus statement on the pathology of IgG4-related disease. Mod. Pathol. 2012, 25, 1181–1192. [Google Scholar] [CrossRef] [PubMed]
- Umehara, H.; Okazaki, K.; Masaki, Y. Comprehensive diagnostic criteria for IgG4-related disease (IgG4-RD). Mod. Rheumatol. 2012, 22, 21–30. [Google Scholar] [CrossRef]
- Pieringer, H.; Parzer, I.; Wöhrer, A.; Reis, P.; Oppl, B.; Zwerina, J. IgG4-related disease: An orphan disease with many faces. Orphanet J. Rare Dis. 2014, 16, 110. [Google Scholar] [CrossRef] [PubMed]
- Kamisawa, T.; Zen, Y.; Pillai, S.; Stone, J.H. IgG4-related disease. Lancet 2015, 11, 1460–1471. [Google Scholar] [CrossRef] [PubMed]
- Hirano, K.; Tada, M.; Sasahira, N. Incidence of malignancies in patients with IgG4-related disease. Intern. Med. 2014, 53, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Shiokawa, M.; Kodama, Y.; Yoshimura, K. Risk of cancer in patients with autoimmune pancreatitis. Am. J. Gastroenterol. 2013, 108, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Asano, J.; Watanabe, T.; Oguchi, T. Association between immunoglobulin G4-related disease and malignancy within 12 years after diagnosis: An analysis after longterm follow-up. J. Rheumatol. 2015, 42, 2135–2142. [Google Scholar] [CrossRef] [PubMed]
- Schneider, A.; Hirth, M.; Münch, M. Risk of cancer in patients with autoimmune pancreatitis: A single-center experience from Germany. Digestion 2017, 95, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Hamano, H.; Kawa, S.; Horiuchi, A. High serum IgG4 concentrations in patients with sclerosing pancreatitis. N. Engl. J. Med. 2001, 8, 732–738. [Google Scholar] [CrossRef] [PubMed]
- Fei, Y.; Shi, J.; Lin, W. Intrathoracic involvements of immunoglobulin G4-related sclerosing disease. Medicine 2015, 94, e2150. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, M.; Takahashi, H.; Tabeya, T. Risk of malignancies in IgG4-related disease. Mod. Rheumatol. 2012, 22, 414–418. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Wu, Y.; Liu, J.; Zhuang, Y.; Jin, X.; Wang, L. The risk of malignancy in patients with IgG4-related disease: A systematic review and meta-analysis. Arthritis Res. Ther. 2022, 24, 14. [Google Scholar] [CrossRef] [PubMed]
- Tang, H.; Yang, H.; Zhang, P.; Wu, D.; Zhang, S.; Zhao, J.; Peng, L.; Chen, H.; Fei, Y.; Zhang, X.; et al. Malignancy and IgG4-related disease: The incidence, related factors and prognosis from a prospective cohort study in China. Sci. Rep. 2020, 10, 4910. [Google Scholar] [CrossRef] [PubMed]
- Sodavarapu, S.; Ghotra, G.S.; Obad, N.; Goyal, M.; Gill, A.S. IgG4-Related Diseases–Continues To Be a Cancer Mimicker. Cureus 2019, 12, 1. [Google Scholar] [CrossRef] [PubMed]
- Lemaitre, S.; Esquerda, G.M.; Guardiola, A.C.; Jordi, T.; Sanda, N.; González-Candial, M. Colon cancer and IgG4-related disease with orbital inflammation and bilateral optic perineuritis: A case report. Medicine 2018, 97, e12197. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Na, K.; Kim, S.-W. Coexistence of Colorectal Cancer and Immunoglobulin G4-Related Disease in the Same Lesion: A Rare Case with Molecular Classification. Diagnostics 2024, 14, 138. https://doi.org/10.3390/diagnostics14020138
Na K, Kim S-W. Coexistence of Colorectal Cancer and Immunoglobulin G4-Related Disease in the Same Lesion: A Rare Case with Molecular Classification. Diagnostics. 2024; 14(2):138. https://doi.org/10.3390/diagnostics14020138
Chicago/Turabian StyleNa, Kiyong, and So-Woon Kim. 2024. "Coexistence of Colorectal Cancer and Immunoglobulin G4-Related Disease in the Same Lesion: A Rare Case with Molecular Classification" Diagnostics 14, no. 2: 138. https://doi.org/10.3390/diagnostics14020138
APA StyleNa, K., & Kim, S.-W. (2024). Coexistence of Colorectal Cancer and Immunoglobulin G4-Related Disease in the Same Lesion: A Rare Case with Molecular Classification. Diagnostics, 14(2), 138. https://doi.org/10.3390/diagnostics14020138





