Predicting the Invasiveness of Pulmonary Adenocarcinomas in Pure Ground-Glass Nodules Using the Nodule Diameter: A Systematic Review, Meta-Analysis, and Validation in an Independent Cohort
Abstract
1. Introduction
2. Materials and Methods
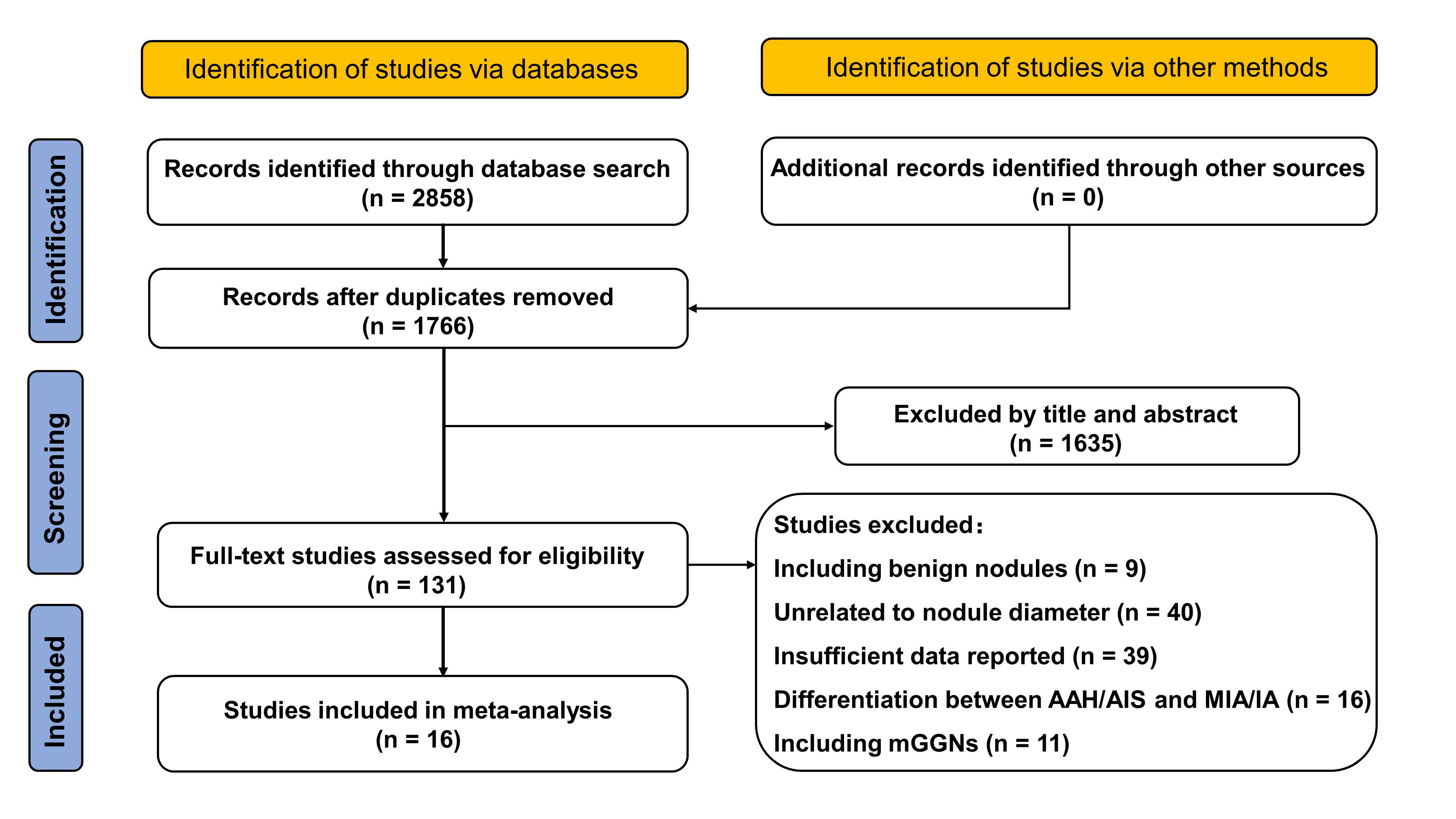
2.1. Search Strategy and Selection Criteria
2.2. Data Extraction
2.3. Quality Assessment
2.4. Meta-Analysis
2.5. Validation Using an Independent Sample
3. Results
3.1. Characteristics of the Included Studies
3.2. Quality Assessment
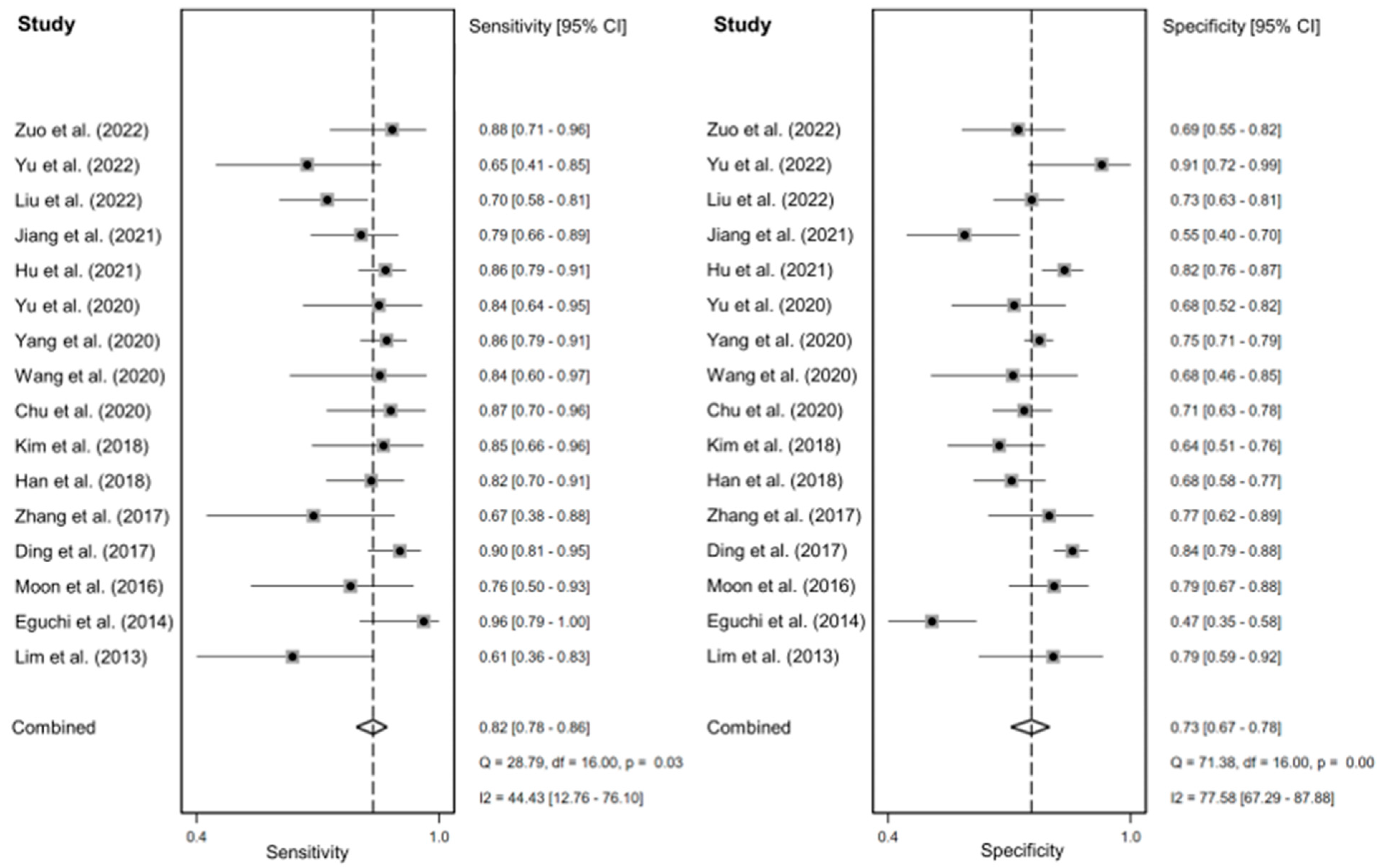
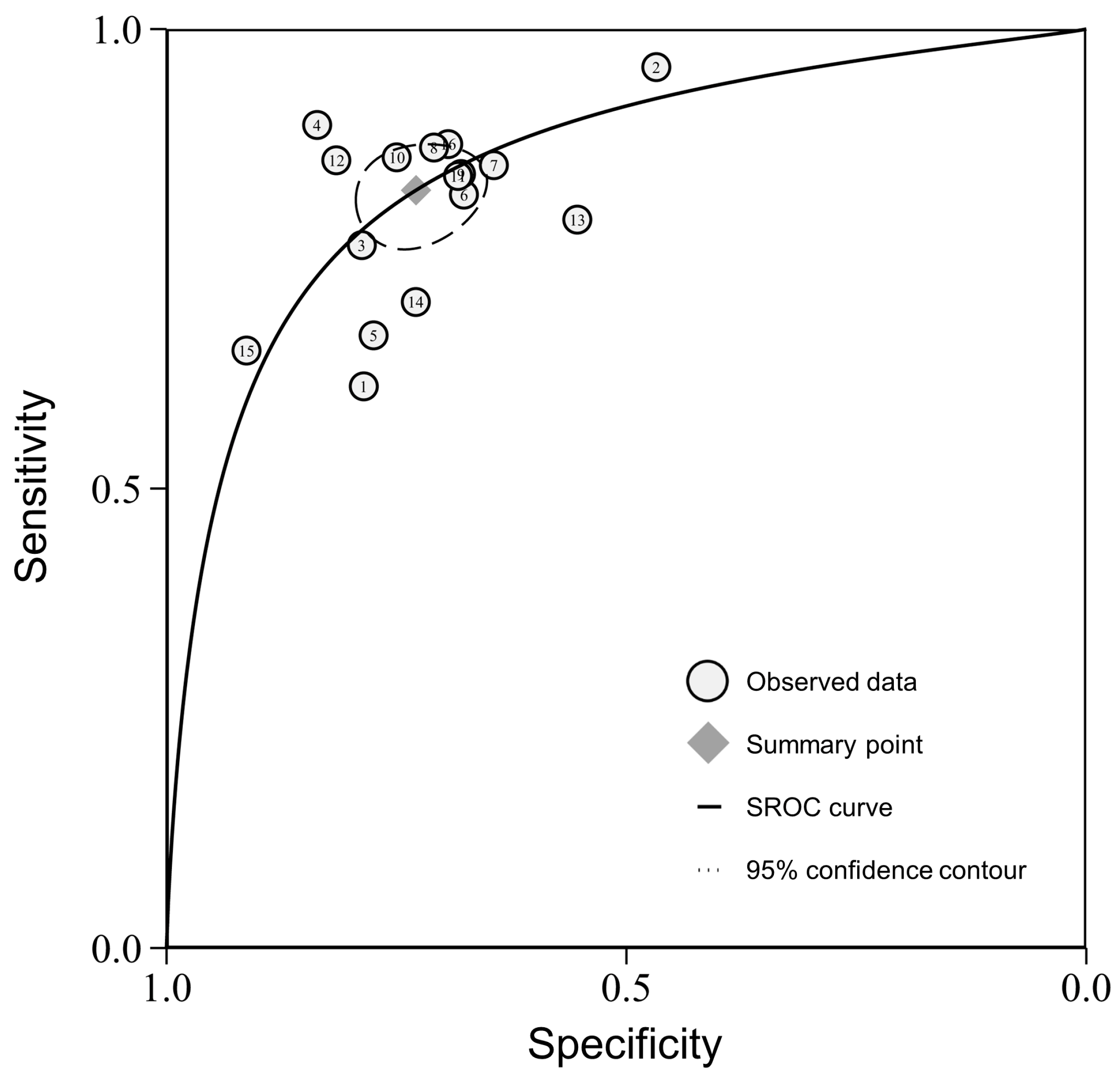
3.3. Meta-Analysis of Diagnostic Performance
3.4. Validation Using an Independent Sample
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA A Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA A Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef] [PubMed]
- Aberle, D.R.; Adams, A.M.; Berg, C.D.; Black, W.C.; Clapp, J.D.; Fagerstrom, R.M.; Gareen, I.F.; Gatsonis, C.; Marcus, P.M.; Sicks, J.D. Reduced lung-cancer mortality with low-dose computed tomographic screening. N. Engl. J. Med. 2011, 365, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Aberle, D.R.; DeMello, S.; Berg, C.D.; Black, W.C.; Brewer, B.; Church, T.R.; Clingan, K.L.; Duan, F.; Fagerstrom, R.M.; Gareen, I.F.; et al. Results of the two incidence screenings in the National Lung Screening Trial. N. Engl. J. Med. 2013, 369, 920–931. [Google Scholar] [CrossRef]
- Lee, C.T. What do we know about ground-glass opacity nodules in the lung? Transl. Lung Cancer Res. 2015, 4, 656–659. [Google Scholar] [CrossRef] [PubMed]
- Pedersen, J.H.; Saghir, Z.; Wille, M.M.; Thomsen, L.H.; Skov, B.G.; Ashraf, H. Ground-Glass Opacity Lung Nodules in the Era of Lung Cancer CT Screening: Radiology, Pathology, and Clinical Management. Oncology 2016, 30, 266–274. [Google Scholar] [PubMed]
- Zhang, Y.; Jheon, S.; Li, H.; Zhang, H.; Xie, Y.; Qian, B.; Lin, K.; Wang, S.; Fu, C.; Hu, H.; et al. Results of low-dose computed tomography as a regular health examination among Chinese hospital employees. J. Thorac. Cardiovasc. Surg. 2020, 160, 824–831.e824. [Google Scholar] [CrossRef]
- Kobayashi, Y.; Mitsudomi, T.; Sakao, Y.; Yatabe, Y. Genetic features of pulmonary adenocarcinoma presenting with ground-glass nodules: The differences between nodules with and without growth. Ann. Oncol. 2015, 26, 156–161. [Google Scholar] [CrossRef]
- Cheng, T.Y.; Cramb, S.M.; Baade, P.D.; Youlden, D.R.; Nwogu, C.; Reid, M.E. The International Epidemiology of Lung Cancer: Latest Trends, Disparities, and Tumor Characteristics. J. Thorac. Oncol. 2016, 11, 1653–1671. [Google Scholar] [CrossRef]
- Yang, W.; Sun, Y.; Fang, W.; Qian, F.; Ye, J.; Chen, Q.; Jiang, Y.; Yu, K.; Han, B. High-resolution Computed Tomography Features Distinguishing Benign and Malignant Lesions Manifesting as Persistent Solitary Subsolid Nodules. Clin. Lung Cancer 2018, 19, e75–e83. [Google Scholar] [CrossRef]
- Travis, W.D.; Brambilla, E.; Nicholson, A.G.; Yatabe, Y.; Austin, J.H.M.; Beasley, M.B.; Chirieac, L.R.; Dacic, S.; Duhig, E.; Flieder, D.B.; et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J. Thorac. Oncol. 2015, 10, 1243–1260. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Asamura, H.; Bankier, A.A.; Beasley, M.B.; Detterbeck, F.; Flieder, D.B.; Goo, J.M.; MacMahon, H.; Naidich, D.; Nicholson, A.G.; et al. The IASLC Lung Cancer Staging Project: Proposals for Coding T Categories for Subsolid Nodules and Assessment of Tumor Size in Part-Solid Tumors in the Forthcoming Eighth Edition of the TNM Classification of Lung Cancer. J. Thorac. Oncol. 2016, 11, 1204–1223. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, A.G.; Tsao, M.S.; Beasley, M.B.; Borczuk, A.C.; Brambilla, E.; Cooper, W.A.; Dacic, S.; Jain, D.; Kerr, K.M.; Lantuejoul, S.; et al. The 2021 WHO Classification of Lung Tumors: Impact of Advances Since 2015. J. Thorac. Oncol. 2022, 17, 362–387. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Wang, R.; Zhang, Y.; Li, Y.; Cheng, C.; Pan, Y.; Xiang, J.; Zhang, Y.; Chen, H.; Sun, Y. Precise Diagnosis of Intraoperative Frozen Section Is an Effective Method to Guide Resection Strategy for Peripheral Small-Sized Lung Adenocarcinoma. J. Clin. Oncol. 2016, 34, 307–313. [Google Scholar] [CrossRef]
- Yotsukura, M.; Asamura, H.; Motoi, N.; Kashima, J.; Yoshida, Y.; Nakagawa, K.; Shiraishi, K.; Kohno, T.; Yatabe, Y.; Watanabe, S.I. Long-Term Prognosis of Patients With Resected Adenocarcinoma In Situ and Minimally Invasive Adenocarcinoma of the Lung. J. Thorac. Oncol. 2021, 16, 1312–1320. [Google Scholar] [CrossRef]
- Deng, C.; Zheng, Q.; Zhang, Y.; Jin, Y.; Shen, X.; Nie, X.; Fu, F.; Ma, X.; Ma, Z.; Wen, Z.; et al. Validation of the Novel International Association for the Study of Lung Cancer Grading System for Invasive Pulmonary Adenocarcinoma and Association With Common Driver Mutations. J. Thorac. Oncol. 2021, 16, 1684–1693. [Google Scholar] [CrossRef]
- Hou, L.; Wang, T.; Chen, D.; She, Y.; Deng, J.; Yang, M.; Zhang, Y.; Zhao, M.; Zhong, Y.; Ma, M.; et al. Prognostic and predictive value of the newly proposed grading system of invasive pulmonary adenocarcinoma in Chinese patients: A retrospective multicohort study. Mod. Pathol. 2022, 35, 749–756. [Google Scholar] [CrossRef]
- MacMahon, H.; Naidich, D.P.; Goo, J.M.; Lee, K.S.; Leung, A.N.C.; Mayo, J.R.; Mehta, A.C.; Ohno, Y.; Powell, C.A.; Prokop, M.; et al. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017. Radiology 2017, 284, 228–243. [Google Scholar] [CrossRef]
- Lee, S.M.; Park, C.M.; Goo, J.M.; Lee, H.J.; Wi, J.Y.; Kang, C.H. Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: Differentiation by using CT features. Radiology 2013, 268, 265–273. [Google Scholar] [CrossRef]
- Lim, H.J.; Ahn, S.; Lee, K.S.; Han, J.; Shim, Y.M.; Woo, S.; Kim, J.H.; Yie, M.; Lee, H.Y.; Yi, C.A. Persistent pure ground-glass opacity lung nodules ≥ 10 mm in diameter at CT scan: Histopathologic comparisons and prognostic implications. Chest 2013, 144, 1291–1299. [Google Scholar] [CrossRef]
- Liang, J.; Xu, X.Q.; Xu, H.; Yuan, M.; Zhang, W.; Shi, Z.F.; Yu, T.F. Using the CT features to differentiate invasive pulmonary adenocarcinoma from pre-invasive lesion appearing as pure or mixed ground-glass nodules. Br. J. Radiol. 2015, 88, 20140811. [Google Scholar] [CrossRef]
- Chu, Z.G.; Li, W.J.; Fu, B.J.; Lv, F.J. CT Characteristics for Predicting Invasiveness in Pulmonary Pure Ground-Glass Nodules. AJR. Am. J. Roentgenol. 2020, 215, 351–358. [Google Scholar] [CrossRef]
- Jiang, Y.; Che, S.; Ma, S.; Liu, X.; Guo, Y.; Liu, A.; Li, G.; Li, Z. Radiomic signature based on CT imaging to distinguish invasive adenocarcinoma from minimally invasive adenocarcinoma in pure ground-glass nodules with pleural contact. Cancer Imaging 2021, 21, 1. [Google Scholar] [CrossRef]
- Bai, C.; Choi, C.M.; Chu, C.M.; Anantham, D.; Chung-Man Ho, J.; Khan, A.Z.; Lee, J.M.; Li, S.Y.; Saenghirunvattana, S.; Yim, A. Evaluation of Pulmonary Nodules: Clinical Practice Consensus Guidelines for Asia. Chest 2016, 150, 877–893. [Google Scholar] [CrossRef]
- Christensen, J.; Prosper, A.E.; Wu, C.C.; Chung, J.; Lee, E.; Elicker, B.; Hunsaker, A.R.; Petranovic, M.; Sandler, K.L.; Stiles, B.; et al. ACR Lung-RADS v2022: Assessment Categories and Management Recommendations. J. Am. Coll. Radiol. 2023, 9, S1546-1440(23)00761-5. [Google Scholar] [CrossRef]
- Mazzone, P.J.; Silvestri, G.A.; Souter, L.H.; Caverly, T.J.; Kanne, J.P.; Katki, H.A.; Wiener, R.S.; Detterbeck, F.C. Screening for Lung Cancer: CHEST Guideline and Expert Panel Report. Chest 2021, 160, e427–e494. [Google Scholar] [CrossRef]
- Wood, D.E.; Kazerooni, E.A.; Aberle, D.; Berman, A.; Brown, L.M.; Eapen, G.A.; Ettinger, D.S.; Ferguson, J.S.; Hou, L.; Kadaria, D.; et al. NCCN Guidelines® Insights: Lung Cancer Screening, Version 1.2022. J. Natl. Compr. Cancer Netw. 2022, 20, 754–764. [Google Scholar] [CrossRef]
- Kodama, K.; Higashiyama, M.; Yokouchi, H.; Takami, K.; Kuriyama, K.; Kusunoki, Y.; Nakayama, T.; Imamura, F. Natural history of pure ground-glass opacity after long-term follow-up of more than 2 years. Ann. Thorac. Surg. 2002, 73, 386–392. [Google Scholar] [CrossRef]
- Eguchi, T.; Kondo, R.; Kawakami, S.; Matsushita, M.; Yoshizawa, A.; Hara, D.; Matsuoka, S.; Takeda, T.; Miura, K.; Agatsuma, H.; et al. Computed tomography attenuation predicts the growth of pure ground-glass nodules. Lung Cancer 2014, 84, 242–247. [Google Scholar] [CrossRef]
- Wang, H.; Weng, Q.; Hui, J.; Fang, S.; Wu, X.; Mao, W.; Chen, M.; Zheng, L.; Wang, Z.; Zhao, Z.; et al. Value of TSCT Features for Differentiating Preinvasive and Minimally Invasive Adenocarcinoma From Invasive Adenocarcinoma Presenting as Subsolid Nodules Smaller Than 3 cm. Acad. Radiol. 2020, 27, 395–403. [Google Scholar] [CrossRef]
- Zhang, Y.; Tang, J.; Xu, J.; Cheng, J.; Wu, H. Analysis of pulmonary pure ground-glass nodule in enhanced dual energy CT imaging for predicting invasive adenocarcinoma: Comparing with conventional thin-section CT imaging. J. Thorac. Dis. 2017, 9, 4967–4978. [Google Scholar] [CrossRef]
- Ding, H.; Shi, J.; Zhou, X.; Xie, D.; Song, X.; Yang, Y.; Liu, Z.; Wang, H. Value of CT Characteristics in Predicting Invasiveness of Adenocarcinoma Presented as Pulmonary Ground-Glass Nodules. Thorac. Cardiovasc. Surg. 2017, 65, 136–141. [Google Scholar] [CrossRef]
- Hu, F.; Huang, H.; Jiang, Y.; Feng, M.; Wang, H.; Tang, M.; Zhou, Y.; Tan, X.; Liu, Y.; Xu, C.; et al. Discriminating invasive adenocarcinoma among lung pure ground-glass nodules: A multi-parameter prediction model. J. Thorac. Dis. 2021, 13, 5383–5394. [Google Scholar] [CrossRef]
- Han, L.; Zhang, P.; Wang, Y.; Gao, Z.; Wang, H.; Li, X.; Ye, Z. CT quantitative parameters to predict the invasiveness of lung pure ground-glass nodules (pGGNs). Clin. Radiol. 2018, 73, 504.e501–504.e507. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Whiting, P.F.; Rutjes, A.W.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.; Sterne, J.A.; Bossuyt, P.M. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 2011, 155, 529–536. [Google Scholar] [CrossRef]
- Vamvakas, E.C. Meta-analyses of studies of the diagnostic accuracy of laboratory tests: A review of the concepts and methods. Arch. Pathol. Lab. Med. 1998, 122, 675–686. [Google Scholar]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Liu, J.; Yang, X.; Li, Y.; Xu, H.; He, C.; Qing, H.; Ren, J.; Zhou, P. Development and validation of qualitative and quantitative models to predict invasiveness of lung adenocarcinomas manifesting as pure ground-glass nodules based on low-dose computed tomography during lung cancer screening. Quant. Imaging Med. Surg. 2022, 12, 2917–2931. [Google Scholar] [CrossRef]
- Mu, G.; Chen, Y.; Wu, D.; Zhan, Y.; Zhou, X.; Gao, Y. Relu Cascade of Feature Pyramid Networks for CT Pulmonary Nodule Detection; Springer International Publishing: Cham, Switzerland, 2019; pp. 444–452. [Google Scholar]
- Wang, Q.; Zhou, X.; Wang, C.; Liu, Z.; Huang, J.; Zhou, Y.; Li, C.; Zhuang, H.; Cheng, J.Z.J.I.A. WGAN-Based Synthetic Minority Over-Sampling Technique: Improving Semantic Fine-Grained Classification for Lung Nodules in CT Images. IEEE Access 2019, 7, 18450–18463. [Google Scholar] [CrossRef]
- Hawass, N.E. Comparing the sensitivities and specificities of two diagnostic procedures performed on the same group of patients. Br. J. Radiol. 1997, 70, 360–366. [Google Scholar] [CrossRef]
- Yang, H.H.; Lv, Y.L.; Fan, X.H.; Ai, Z.Y.; Xu, X.C.; Ye, B.; Hu, D.Z. Factors distinguishing invasive from pre-invasive adenocarcinoma presenting as pure ground glass pulmonary nodules. Radiat. Oncol. 2020, 15, 186. [Google Scholar] [CrossRef]
- Zuo, Z.; Wang, P.; Zeng, W.; Qi, W.; Zhang, W. Measuring pure ground-glass nodules on computed tomography: Assessing agreement between a commercially available deep learning algorithm and radiologists’ readings. Acta Radiol. 2023, 64, 1422–1430. [Google Scholar] [CrossRef]
- Kim, H.; Goo, J.M.; Park, C.M. Evaluation of T categories for pure ground-glass nodules with semi-automatic volumetry: Is mass a better predictor of invasive part size than other volumetric parameters? Eur. Radiol. 2018, 28, 4288–4295. [Google Scholar] [CrossRef]
- Moon, Y.; Sung, S.W.; Lee, K.Y.; Sim, S.B.; Park, J.K. Pure ground-glass opacity on chest computed tomography: Predictive factors for invasive adenocarcinoma. J. Thorac. Dis. 2016, 8, 1561–1570. [Google Scholar] [CrossRef]
- Yu, Y.; Cheng, J.J.; Li, J.Y.; Zhang, Y.; Lin, L.Y.; Zhang, F.; Xu, J.R.; Zhao, X.J.; Wu, H.W. Determining the invasiveness of pure ground-glass nodules using dual-energy spectral computed tomography. Transl. Lung Cancer Res. 2020, 9, 484–495. [Google Scholar] [CrossRef]
- Yu, Y.; Fu, Y.; Chen, X.; Zhang, Y.; Zhang, F.; Li, X.; Zhao, X.; Cheng, J.; Wu, H. Dual-layer spectral detector CT: Predicting the invasiveness of pure ground-glass adenocarcinoma. Clin. Radiol. 2022, 77, e458–e465. [Google Scholar] [CrossRef]
- Hsu, W.C.; Huang, P.C.; Pan, K.T.; Chuang, W.Y.; Wu, C.Y.; Wong, H.F.; Yang, C.T.; Wan, Y.L. Predictors of Invasive Adenocarcinomas among Pure Ground-Glass Nodules Less Than 2 cm in Diameter. Cancers 2021, 13, 3945. [Google Scholar] [CrossRef]
- Dai, J.; Yu, G.; Yu, J. Can CT imaging features of ground-glass opacity predict invasiveness? A meta-analysis. Thorac. Cancer 2018, 9, 452–458. [Google Scholar] [CrossRef]
- He, S.; Chen, C.; Wang, Z.; Yu, X.; Liu, S.; Huang, Z.; Chen, C.; Liang, Z.; Chen, C. The use of the mean computed-tomography value to predict the invasiveness of ground-glass nodules: A meta-analysis. Asian J. Surg. 2023, 46, 677–682. [Google Scholar] [CrossRef]
- Fan, L.; Fang, M.; Li, Z.; Tu, W.; Wang, S.; Chen, W.; Tian, J.; Dong, D.; Liu, S. Radiomics signature: A biomarker for the preoperative discrimination of lung invasive adenocarcinoma manifesting as a ground-glass nodule. Eur. Radiol. 2019, 29, 889–897. [Google Scholar] [CrossRef]
- Wu, G.; Woodruff, H.C.; Shen, J.; Refaee, T.; Sanduleanu, S.; Ibrahim, A.; Leijenaar, R.T.H.; Wang, R.; Xiong, J.; Bian, J.; et al. Diagnosis of Invasive Lung Adenocarcinoma Based on Chest CT Radiomic Features of Part-Solid Pulmonary Nodules: A Multicenter Study. Radiology 2020, 297, 451–458. [Google Scholar] [CrossRef]
- Wu, L.; Gao, C.; Ye, J.; Tao, J.; Wang, N.; Pang, P.; Xiang, P.; Xu, M. The value of various peritumoral radiomic features in differentiating the invasiveness of adenocarcinoma manifesting as ground-glass nodules. Eur. Radiol. 2021, 31, 9030–9037. [Google Scholar] [CrossRef]
- Li, Y.; Liu, J.; Yang, X.; Xu, H.; Qing, H.; Ren, J.; Zhou, P. Prediction of invasive adenocarcinomas manifesting as pure ground-glass nodules based on radiomic signature of low-dose CT in lung cancer screening. Br. J. Radiol. 2022, 95, 20211048. [Google Scholar] [CrossRef]
- Kao, T.N.; Hsieh, M.S.; Chen, L.W.; Yang, C.J.; Chuang, C.C.; Chiang, X.H.; Chen, Y.C.; Lee, Y.H.; Hsu, H.H.; Chen, C.M.; et al. CT-Based Radiomic Analysis for Preoperative Prediction of Tumor Invasiveness in Lung Adenocarcinoma Presenting as Pure Ground-Glass Nodule. Cancers 2022, 14, 5888. [Google Scholar] [CrossRef]
- American College of Radiology. Lung CT Screening Reporting and Data System (Lung-RADS, v2022). Available online: https://www.acr.org/Clinical-Resources/Reporting-and-Data-Systems/Lung-Rads (accessed on 29 December 2023).
- Goo, J.M.; Tongdee, T.; Tongdee, R.; Yeo, K.; Hildebolt, C.F.; Bae, K.T. Volumetric measurement of synthetic lung nodules with multi-detector row CT: Effect of various image reconstruction parameters and segmentation thresholds on measurement accuracy. Radiology 2005, 235, 850–856. [Google Scholar] [CrossRef]
| Study (Year) | Country | No. of Patients | No. of pGGNs | Age (Years) | No. of Males (%) | No. of Smokers (%) | Measure of Diameter | Slice Thickness (mm) | Matrix | |
|---|---|---|---|---|---|---|---|---|---|---|
| IA | non-IA | |||||||||
| Lim et al. (2013) [20] | Korea | 46 | 18 | 28 | 61.4 | 26 (56.5) | 14 (30.4) | maximal | 0.75–2.5 | NA |
| Eguchi et al. (2014) [29] | Japan | 98 | 24 | 77 | 64.3 | 39 (38.6) | 31 (30.7) | maximal | 1.25 | NA |
| Moon et al. (2016) [47] | Korea | 83 | 17 | 66 | 58.4 | 31 (37.3) | 19 (22.9) | maximal | NA | NA |
| Ding et al. (2017) [32] | China | NA | 86 | 275 | 54.5 | 125 (34.6) | NA | maximal | 1.0 | NA |
| Zhang et al. (2017) # [31] | China | 53 | 15 | 40 | 59.0 * | 13 (24.5) | 0 (0) | maximal | 1.25 | NA |
| Han et al. (2018) # [34] | China | 154 | 61 | 102 | 55.2 | 52 (33.8) | NA | maximal | 1.25 | NA |
| Kim et al. (2018) [46] | Korea | 86 | 27 | 59 | NA | 41 (47.7) | NA | mean | 0.625–1.25 | NA |
| Chu et al. (2020) [22] | China | 161 | 31 | 141 | 53.4 | 48 (27.9) | 29 (16.9) | mean | 0.625 | NA |
| Wang et al. (2020) [30] | China | 44 | 19 | 25 | NA | NA | NA | maximal | 0.9 | 1024 × 1024 |
| Yang et al. (2020) [44] | China | 641 | 136 | 523 | NA | 200 (30.3) | 309 (46.9) | mean | NA | 1024 × 1024 |
| Yu et al. (2020) # [48] | China | 62 | 25 | 41 | 55.4 | 19 (30.6) | 4 (6.5) | maximal | 1.25 | NA |
| Hu et al. (2021) [33] | China | 309 | 133 | 211 | 53.4 | 98 (28.5) | NA | mean | 1.0 | NA |
| Jiang et al. (2021) [23] | China | 100 | 53 | 47 | 60.5 * | 29 (29.0) | 8 (8.0) | maximal | 1.0–1.5 | 512 × 512 |
| Liu et al. (2022) [40] | China | 160 | 64 | 96 | 51.4 | 54(33.8) | NA | mean | 0.625 | 512 × 512 |
| Yu et al. (2022) # [49] | China | 42 | 20 | 23 | 56.4 | 8 (19.1) | NA | maximal | 1.0 | NA |
| Zuo et al. (2023) # [45] | China | 68 | 32 | 49 | 52.6 | 18(26.5) | NA | maximal | 0.625–1.25 | NA |
| Study | TP | FP | FN | TN | Cut-off (mm) |
|---|---|---|---|---|---|
| Lim et al. (2013) [20] | 11 | 6 | 7 | 22 | 16.4 |
| Eguchi et al. (2014) [29] | 23 | 41 | 1 | 36 | 11.0 |
| Moon et al. (2016) [47] | 13 | 14 | 4 | 52 | 15.0 |
| Ding et al. (2017) [32] | 77 | 45 | 9 | 230 | 12.0 |
| Zhang et al. (2017) [31] | 10 | 9 | 5 | 31 | 16.1 |
| Han et al. (2018) [34] | 50 | 33 | 11 | 69 | 17.2 |
| Kim et al. (2018) [46] | 23 | 21 | 4 | 38 | 10.4 |
| Chu et al. (2020) [22] | 27 | 41 | 4 | 100 | 10.5 |
| Wang et al. (2020) [30] | 16 | 8 | 3 | 17 | 8.5 |
| Yang et al. (2020) [44] | 117 | 131 | 19 | 392 | 10.1 |
| Yu et al. (2020) [48] | 21 | 13 | 4 | 28 | 9.4 |
| Hu et al. (2021) [33] | 114 | 39 | 19 | 172 | 9.8 |
| Jiang et al. (2021) [23] | 42 | 21 | 11 | 26 | 13.9 |
| Liu et al. (2022) [40] | 45 | 26 | 19 | 70 | 10.0 |
| Yu et al. (2022) [49] | 13 | 2 | 7 | 21 | 14.0 |
| Zuo et al. (2023) [45] | 28 | 15 | 4 | 34 | NA |
| Study | Risk of Bias | Applicability Concerns | |||||
|---|---|---|---|---|---|---|---|
| Patient Selection | Index Test | Reference Standard | Flow and Timing | Patient Selection | Index Test | Reference Standard | |
| Lim et al. (2013) [20] | - | - | + | ? | - | + | + |
| Eguchi et al. (2014) [29] | + | - | + | ? | + | + | + |
| Moon et al. (2016) [47] | + | - | + | + | + | + | + |
| Ding et al. (2017) [32] | + | - | ? | + | + | + | ? |
| Zhang et al. (2017) [31] | - | - | ? | ? | - | + | ? |
| Han et al. (2018) [34] | + | - | ? | ? | + | + | ? |
| Kim et al. (2018) [46] | + | - | ? | + | + | + | + |
| Chu et al. (2020) [22] | + | - | ? | + | + | + | ? |
| Wang et al. (2020) [30] | + | - | ? | + | + | + | + |
| Yang et al. (2020) [44] | - | - | + | ? | - | + | + |
| Yu et al. (2020) [48] | + | - | ? | ? | + | + | ? |
| Hu et al. (2021) [33] | + | - | + | ? | + | + | + |
| Jiang et al. (2021) [23] | - | - | + | + | - | + | + |
| Liu et al. (2022) [40] | + | - | + | + | + | + | + |
| Yu et al. (2022) [49] | - | - | + | + | - | + | + |
| Zuo et al. (2023) [45] | + | - | + | + | + | + | + |
| Covariates | No. of Reports | Sensitivity (95% CI) | p | Specificity (95% CI) | p | |
|---|---|---|---|---|---|---|
| Percentage of males | 16 | 0.73 (0.06–0.99) | 0.77 | 0.38 (0.02–0.95) | 0.38 | |
| Percentage of smokers | 16 | 0.96 (0.60–1.00) | 0.22 | 0.76 (0.22–0.97) | 0.81 | |
| Measure of diameter | 11 | Maximal diameter | 0.82 (0.76–0.87) | <0.01 | 0.72 (0.66–0.79) | <0.01 |
| 5 | Mean diameter | 0.84 (0.77–0.90) | 0.74 (0.66–0.82) | |||
| Slice thickness | 12 | All < 1.5 mm | 0.84 (0.79–0.88) | 0.58 | 0.73 (0.67–0.79) | 0.58 |
| 2 | Not all < 1.5 mm | 0.73 (0.57–0.88) | 0.67 (0.49–0.85) | |||
| Reconstruction matrix | 2 | 1024 × 1024 | 0.86 (0.80–0.91) | 0.11 | 0.75 (0.71–0.78) | 0.01 |
| 2 | 512 × 512 | 0.74 (0.66–0.82) | 0.67 (0.59–0.75`) | |||
| Patient selection | 11 | Low risk | 0.85 (0.81–0.89) | 0.04 | 0.72 (0.66–0.78) | <0.01 |
| 5 | High risk | 0.76 (0.67–0.85) | 0.76 (0.67–0.85) |
| Characteristics | IA (n = 82) | Non-IA (n = 128) | p |
|---|---|---|---|
| Gender (male/female) | 0.88 | ||
| Female | 53 | 84 | |
| Male | 29 | 44 | |
| Age | 59.6 ± 10.5 | 49.2 ± 11.8 | <0.01 |
| Maximal diameter | 16.7 ± 5.6 | 9.6 ± 3.4 | <0.01 |
| Mean diameter | 14.8 ± 4.7 | 8.6 ± 2.9 | <0.01 |
| Measures | Sensitivity (95% CI) | Specificity (95% CI) | Cut-off |
|---|---|---|---|
| Maximal diameter | 0.72 (0.61–0.81) | 0.86 (0.79–0.91) | > 13.2 mm |
| Mean diameter | 0.85 (0.78–0.91) | 0.83 (0.75–0.89) | > 10.4 mm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, J.; Yang, X.; Li, Y.; Xu, H.; He, C.; Zhou, P.; Qing, H. Predicting the Invasiveness of Pulmonary Adenocarcinomas in Pure Ground-Glass Nodules Using the Nodule Diameter: A Systematic Review, Meta-Analysis, and Validation in an Independent Cohort. Diagnostics 2024, 14, 147. https://doi.org/10.3390/diagnostics14020147
Liu J, Yang X, Li Y, Xu H, He C, Zhou P, Qing H. Predicting the Invasiveness of Pulmonary Adenocarcinomas in Pure Ground-Glass Nodules Using the Nodule Diameter: A Systematic Review, Meta-Analysis, and Validation in an Independent Cohort. Diagnostics. 2024; 14(2):147. https://doi.org/10.3390/diagnostics14020147
Chicago/Turabian StyleLiu, Jieke, Xi Yang, Yong Li, Hao Xu, Changjiu He, Peng Zhou, and Haomiao Qing. 2024. "Predicting the Invasiveness of Pulmonary Adenocarcinomas in Pure Ground-Glass Nodules Using the Nodule Diameter: A Systematic Review, Meta-Analysis, and Validation in an Independent Cohort" Diagnostics 14, no. 2: 147. https://doi.org/10.3390/diagnostics14020147
APA StyleLiu, J., Yang, X., Li, Y., Xu, H., He, C., Zhou, P., & Qing, H. (2024). Predicting the Invasiveness of Pulmonary Adenocarcinomas in Pure Ground-Glass Nodules Using the Nodule Diameter: A Systematic Review, Meta-Analysis, and Validation in an Independent Cohort. Diagnostics, 14(2), 147. https://doi.org/10.3390/diagnostics14020147






