Abstract
We describe the case of a 43-year-old female with hereditary hemochromatosis, previously without cardiac issues, who presented with a severe fever (>40 to 41 °C) to our hospital. Initial assessments, including transthoracic echocardiography, showed no typical signs of infective endocarditis. A contrast-enhanced CT scan revealed a hypodense area in the right subscapular muscle, alongside pleural thicknesses. Due to the critical condition, a central venous catheter (CVC) was implanted for immediate intravenous treatment. Subsequent blood cultures, positive for Staphylococcus aureus, and transesophageal echocardiography led to a diagnosis of multivalvular infective endocarditis (MIE). Subsequently, the patient underwent positron emission tomography/computed tomography (PET/CT) with [18F]Fluorodeoxyglucose ([18F]FDG), which detected increased tracer incorporation in the muscle lesion, CVC, and pleural thicknesses. The final diagnosis was CVC infection and septic embolism to the subscapular muscle in a patient with pleuritis. This case showcases the critical role of [18F]FDG PET/CT as whole-body imaging modality in diagnosing and managing complex infective cases.
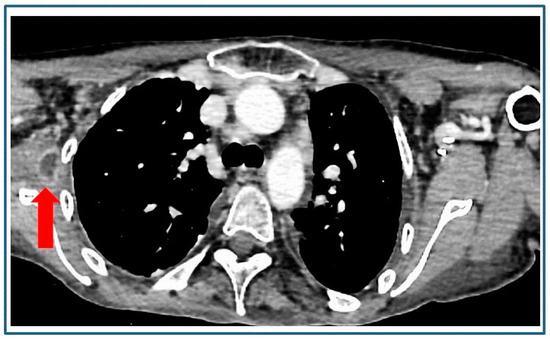
Figure 1.
A 43-year-old female patient with hereditary hemochromatosis, submitted to regular check-up visits and without previous cardiac history, presented with a high fever level (>40 to 41 °C) and was in severely debilitating conditions. At admission, blood was drawn for standard hematologic tests, blood chemistries, and blood culture. Transthoracic echocardiography was also performed, revealing no evidence of typical patterns for infective endocarditis. Subsequently, a contrast-enhanced multislice computed tomography (ce-CT) scan detected a focal hypodense area with “rim enhancement” in the right subscapular muscle (red arrow), the clinical attribution of which remained uncertain, coupled with some pleural thicknesses. Due to the life-threatening nature of the situation and concerns about achieving adequate antibiotic concentrations, a central venous catheter (CVC) was implanted to promptly initiate immediate treatment with intravenous fluids and broad-spectrum antibiotics. After 72 h, patient’s overall conditions improved, with a fever decrease, and this allowed for the execution of further clinical investigations. Blood culture came back positive for Staphylococcus aureus (S. aureus), and transesophageal echocardiography findings led to a diagnosis of multivalvular infective endocarditis (MIE) due to mitral-aortic involvement.
Figure 1.
A 43-year-old female patient with hereditary hemochromatosis, submitted to regular check-up visits and without previous cardiac history, presented with a high fever level (>40 to 41 °C) and was in severely debilitating conditions. At admission, blood was drawn for standard hematologic tests, blood chemistries, and blood culture. Transthoracic echocardiography was also performed, revealing no evidence of typical patterns for infective endocarditis. Subsequently, a contrast-enhanced multislice computed tomography (ce-CT) scan detected a focal hypodense area with “rim enhancement” in the right subscapular muscle (red arrow), the clinical attribution of which remained uncertain, coupled with some pleural thicknesses. Due to the life-threatening nature of the situation and concerns about achieving adequate antibiotic concentrations, a central venous catheter (CVC) was implanted to promptly initiate immediate treatment with intravenous fluids and broad-spectrum antibiotics. After 72 h, patient’s overall conditions improved, with a fever decrease, and this allowed for the execution of further clinical investigations. Blood culture came back positive for Staphylococcus aureus (S. aureus), and transesophageal echocardiography findings led to a diagnosis of multivalvular infective endocarditis (MIE) due to mitral-aortic involvement.
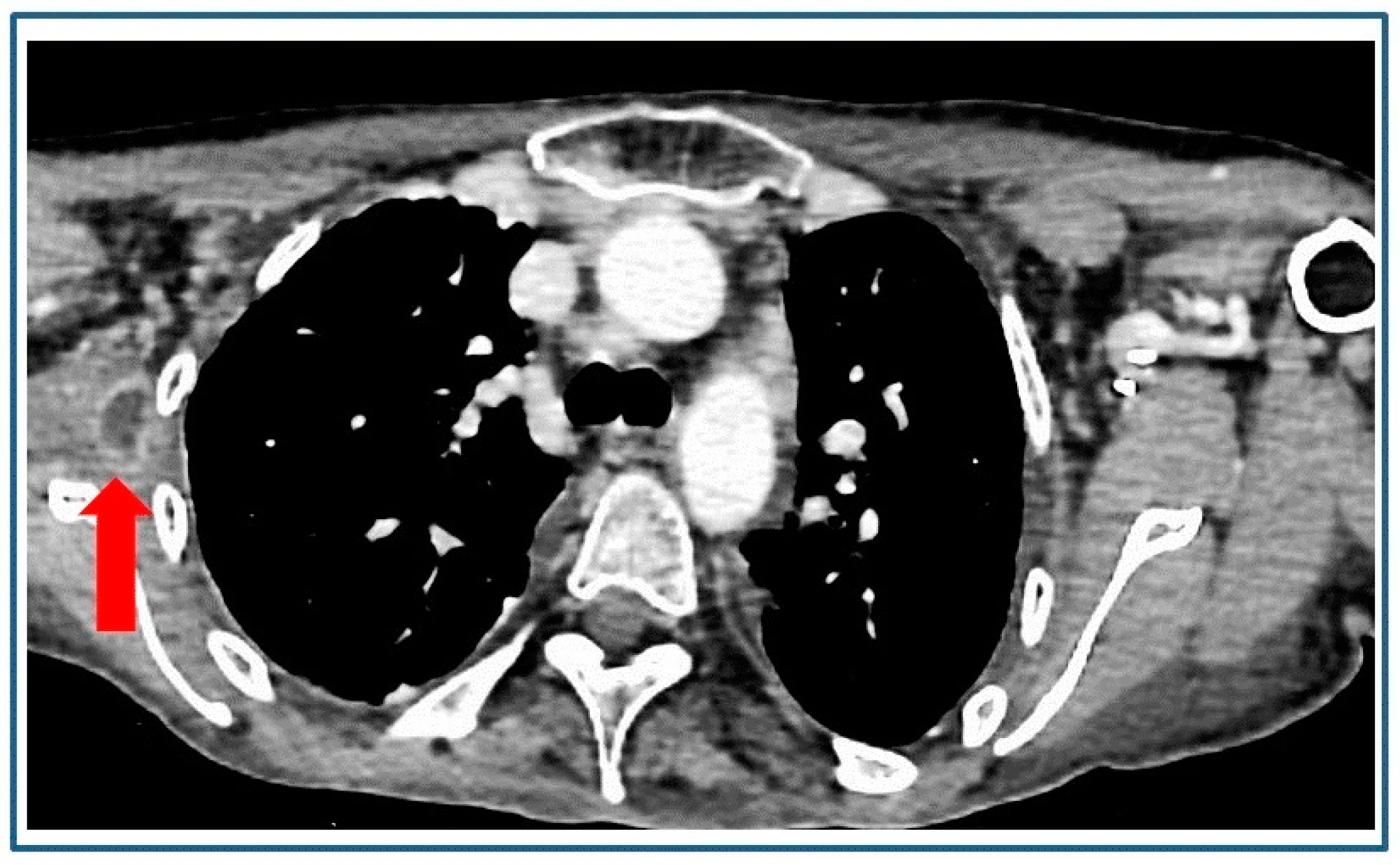
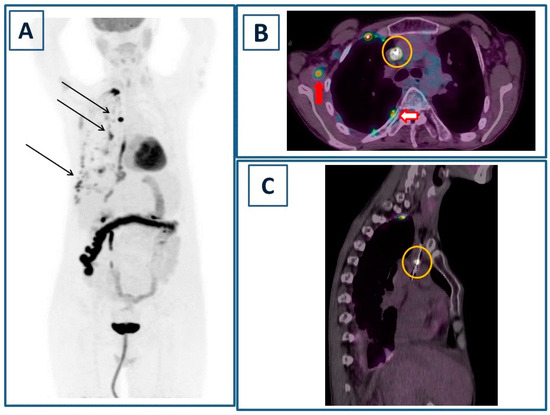
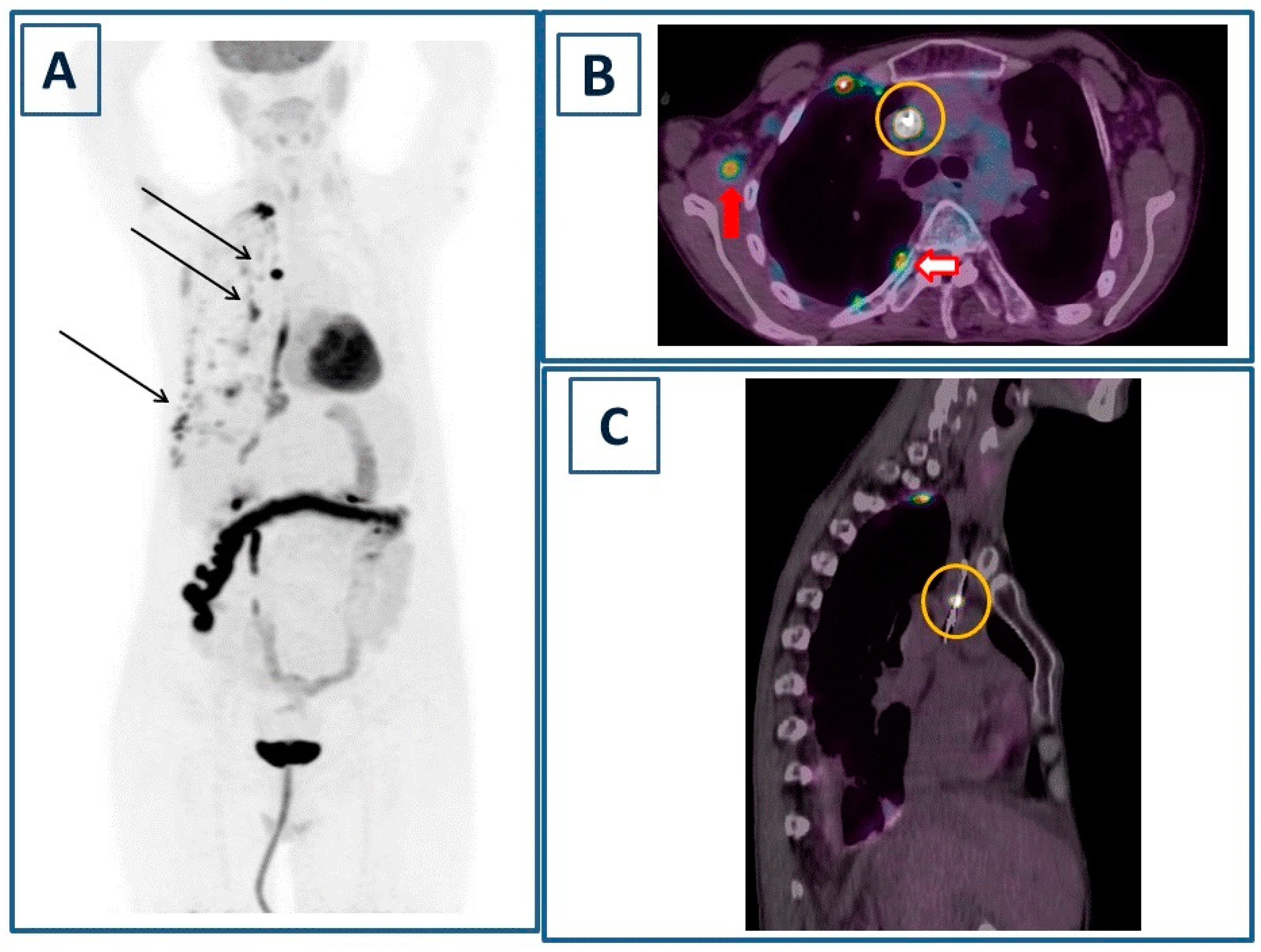
Figure 2.
In order to better define the muscle lesion detected on ce-CT, positron emission tomography/computed tomography (PET/CT) was performed 60 min after the injection of 3.7 MBq/kg of [18F]Fluorodeoxyglucose ([18F]FDG). Maximum Intensity Projection (A) showed multiple areas of focal-increased tracer incorporation in the right hemithorax (black arrows), as well as non-specific uptake in the transverse colon and diffusely decreased liver uptake (mean standardized uptake value/SUVmean 1.69). The corresponding fused PET/CT axial image (B) showed focal tracer incorporation within the muscle lesion (red arrow, maximum standardized uptake value/SUVmax 3.6) and in correspondence to the CVC (yellow circle, SUVmax 32.6). Additionally, increased [18F]FDG consumption was observed due to multiple focal pleural thicknesses (red bordered arrows, SUVmax 8.4). Oblique sagittal projection (C) localized the tracer uptake in the intracaval portion of the CVC well (yellow circle). Of note, there were no identified foci of abnormal uptake at the level of the heart valves, probably related to the small size of the vegetations and the suboptimal preparation of the patient, resulting in an increased baseline cardiac activity. PET/CT findings were consistent with CVC infection and septic embolism to the right subscapular muscle in a patient with pleuritis. A PET/CT-guided biopsy of the muscle lesion, carried out to confirm the diagnosis, revealed necroinflammatory tissue with neutrophils. CVC was promptly removed and subjected to a culture test, which yielded a positive result for S. aureus. Multivalvular infective endocarditis (MIE) is a rare clinical condition with a prognosis that, despite advances in diagnosis and therapy, remains grim [1]. Septic embolisms are infrequent but are linked to elevated mortality and morbidity [2,3]. In these situations, imaging plays a crucial role in promptly detecting septic foci and monitoring the response to therapy. Nuclear medicine offers a diverse array of imaging techniques for the diagnosis and surveillance of infective endocarditis [4]. Scintigraphy using radiolabeled leukocytes for white blood cell (WBC) imaging has found extensive application in clinical practice. However, despite its high specificity, WBC scintigraphy is associated with certain limitations. These include the complex labeling procedure involving patients’ autologous leukocytes and the necessity for a multi-time-point acquisition protocol, encompassing early (1 h), delayed (4 h), and late (24 h) scans to capture the entire cell migration process [5]. Moreover, planar scans exhibit suboptimal spatial resolution, necessitating the use of hybrid single-photon computed tomography/computed tomography (SPECT/CT) to enhance diagnostic accuracy [6,7]. In recent years, [18F]FDG PET/CT has emerged as a prominent imaging modality for diagnosing infective endocarditis, as well as infections related to CVCs and implantable cardiac devices. This is attributed to the tracer’s ability to accumulate in activated leukocytes [8]. In comparison to SPECT/CT, PET/CT offers numerous advantages, including superior spatial resolution, an extended field of view (traditionally spanning from the skull base to proximal thighs), a streamlined one-day protocol, and the ability to achieve accurate quantification. Notably, PET/CT proves particularly valuable in detecting extracardiac infectious sites resulting from septic embolisms. While pulmonary septic embolisms, identified as focal points of increased tracer incorporation, have been extensively reported, the documentation of muscle septic embolisms through PET/CT remains limited [9,10,11]. Another important consideration pertains to the diffusely reduced uptake of [18F]FDG observed in the liver of our patient. In this context, a previously published retrospective study conducted on a substantial cohort (n = 1487) of cancer patients demonstrated that diminished liver uptake could be linked to poor nutritional status, anemia, impaired liver function, and systemic inflammation. Although the case we are describing is non-oncological, all the aforementioned conditions were present, suggesting a plausible explanation for the observed low hepatic [18F]FDG uptake [12]. In conclusion, our case underscores the significance of [18F]FDG PET/CT in this context and sets the stage for future investigations into the recently introduced Long Axial Field-of-View (LAFOV) scanners. These PET/CT scanners boast superior sensitivity, enabling low-dose and rapid protocols. This advancement holds promise for further enhancing our understanding and diagnostic capabilities in the field [13,14].
Figure 2.
In order to better define the muscle lesion detected on ce-CT, positron emission tomography/computed tomography (PET/CT) was performed 60 min after the injection of 3.7 MBq/kg of [18F]Fluorodeoxyglucose ([18F]FDG). Maximum Intensity Projection (A) showed multiple areas of focal-increased tracer incorporation in the right hemithorax (black arrows), as well as non-specific uptake in the transverse colon and diffusely decreased liver uptake (mean standardized uptake value/SUVmean 1.69). The corresponding fused PET/CT axial image (B) showed focal tracer incorporation within the muscle lesion (red arrow, maximum standardized uptake value/SUVmax 3.6) and in correspondence to the CVC (yellow circle, SUVmax 32.6). Additionally, increased [18F]FDG consumption was observed due to multiple focal pleural thicknesses (red bordered arrows, SUVmax 8.4). Oblique sagittal projection (C) localized the tracer uptake in the intracaval portion of the CVC well (yellow circle). Of note, there were no identified foci of abnormal uptake at the level of the heart valves, probably related to the small size of the vegetations and the suboptimal preparation of the patient, resulting in an increased baseline cardiac activity. PET/CT findings were consistent with CVC infection and septic embolism to the right subscapular muscle in a patient with pleuritis. A PET/CT-guided biopsy of the muscle lesion, carried out to confirm the diagnosis, revealed necroinflammatory tissue with neutrophils. CVC was promptly removed and subjected to a culture test, which yielded a positive result for S. aureus. Multivalvular infective endocarditis (MIE) is a rare clinical condition with a prognosis that, despite advances in diagnosis and therapy, remains grim [1]. Septic embolisms are infrequent but are linked to elevated mortality and morbidity [2,3]. In these situations, imaging plays a crucial role in promptly detecting septic foci and monitoring the response to therapy. Nuclear medicine offers a diverse array of imaging techniques for the diagnosis and surveillance of infective endocarditis [4]. Scintigraphy using radiolabeled leukocytes for white blood cell (WBC) imaging has found extensive application in clinical practice. However, despite its high specificity, WBC scintigraphy is associated with certain limitations. These include the complex labeling procedure involving patients’ autologous leukocytes and the necessity for a multi-time-point acquisition protocol, encompassing early (1 h), delayed (4 h), and late (24 h) scans to capture the entire cell migration process [5]. Moreover, planar scans exhibit suboptimal spatial resolution, necessitating the use of hybrid single-photon computed tomography/computed tomography (SPECT/CT) to enhance diagnostic accuracy [6,7]. In recent years, [18F]FDG PET/CT has emerged as a prominent imaging modality for diagnosing infective endocarditis, as well as infections related to CVCs and implantable cardiac devices. This is attributed to the tracer’s ability to accumulate in activated leukocytes [8]. In comparison to SPECT/CT, PET/CT offers numerous advantages, including superior spatial resolution, an extended field of view (traditionally spanning from the skull base to proximal thighs), a streamlined one-day protocol, and the ability to achieve accurate quantification. Notably, PET/CT proves particularly valuable in detecting extracardiac infectious sites resulting from septic embolisms. While pulmonary septic embolisms, identified as focal points of increased tracer incorporation, have been extensively reported, the documentation of muscle septic embolisms through PET/CT remains limited [9,10,11]. Another important consideration pertains to the diffusely reduced uptake of [18F]FDG observed in the liver of our patient. In this context, a previously published retrospective study conducted on a substantial cohort (n = 1487) of cancer patients demonstrated that diminished liver uptake could be linked to poor nutritional status, anemia, impaired liver function, and systemic inflammation. Although the case we are describing is non-oncological, all the aforementioned conditions were present, suggesting a plausible explanation for the observed low hepatic [18F]FDG uptake [12]. In conclusion, our case underscores the significance of [18F]FDG PET/CT in this context and sets the stage for future investigations into the recently introduced Long Axial Field-of-View (LAFOV) scanners. These PET/CT scanners boast superior sensitivity, enabling low-dose and rapid protocols. This advancement holds promise for further enhancing our understanding and diagnostic capabilities in the field [13,14].
Author Contributions
Conceptualization, L.F.; resources and data curation, A.L.; writing—original draft preparation, L.F.; writing—review and editing, F.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent was obtained from the patient.
Data Availability Statement
The data presented in this article are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Álvarez-Zaballos, S.; González-Ramallo, V.; Quintana, E.; Muñoz, P.; de la Villa-Martínez, S.; Fariñas, M.C.; Arnáiz-de Las Revillas, F.; de Alarcón, A.; Rodríguez-Esteban, M.Á.; Miró, J.M.; et al. Multivalvular Endocarditis: A Rare Condition with Poor Prognosis. J. Clin. Med. 2022, 11, 4736. [Google Scholar] [CrossRef] [PubMed]
- Aalaei-Andabili, S.H.; Martin, T.; Hess, P.; Hoh, B.; Anderson, M.; Klodell, C.T.; Beaver, T.M. Management of Septic Emboli in Patients with Infectious Endocarditis. J. Card. Surg. 2017, 32, 274–280. [Google Scholar] [CrossRef] [PubMed]
- Yano, S.; Usui, N.; Asai, O.; Dobashi, N.; Osawa, H.; Takei, Y.; Takahara, S.; Ogasawara, Y.; Yamaguchi, Y.; Saito, T.; et al. Septic Intramuscular Embolism in a Neutropenic Patient with Myelodysplastic Syndrome Accompanied by Asymptomatic Septic Pulmonary Emboli. Intern. Med. 2005, 44, 1100–1102. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ferro, P.; Boni, R.; Slart, R.H.; Erba, P.A. Imaging of Endocarditis and Cardiac Device-Related Infections: An Update. Semin. Nucl. Med. 2023, 53, 184–198. [Google Scholar] [CrossRef] [PubMed]
- Erba, P.A.; Lancellotti, P.; Vilacosta, I.; Gaemperli, O.; Rouzet, F.; Hacker, M.; Signore, A.; Slart, R.H.J.A.; Habib, G. Recommendations on Nuclear and Multimodality Imaging in IE and CIED Infections. Eur. J. Nucl. Med. Mol. Imaging 2018, 45, 1795–1815. [Google Scholar] [CrossRef] [PubMed]
- Filippi, L.; Schillaci, O. SPECT/CT with a Hybrid Camera: A New Imaging Modality for the Functional Anatomical Mapping of Infections. Expert. Rev. Med. Devices 2006, 3, 699–703. [Google Scholar] [CrossRef] [PubMed]
- Filippi, L.; Biancone, L.; Petruzziello, C.; Schillaci, O. Tc-99m HMPAO-Labeled Leukocyte Scintigraphy with Hybrid SPECT/CT Detects Perianal Fistulas in Crohn Disease. Clin. Nucl. Med. 2006, 31, 541–542. [Google Scholar] [CrossRef] [PubMed]
- Pizzi, M.N.; Roque, A.; Fernández-Hidalgo, N.; Cuéllar-Calabria, H.; Ferreira-González, I.; Gonzàlez-Alujas, M.T.; Oristrell, G.; Gracia-Sánchez, L.; González, J.J.; Rodríguez-Palomares, J.; et al. Improving the Diagnosis of Infective Endocarditis in Prosthetic Valves and Intracardiac Devices With 18F-Fluordeoxyglucose Positron Emission Tomography/Computed Tomography Angiography: Initial Results at an Infective Endocarditis Referral Center. Circulation 2015, 132, 1113–1126. [Google Scholar] [CrossRef] [PubMed]
- Akgun, E.; Akyel, R. Unexpected Septic Pulmonary Embolism Imaging with 18-F FDG PET/CT in an Infective Endocarditis Case: Case Report. Egypt. J. Radiol. Nucl. Med. 2022, 53, 230. [Google Scholar] [CrossRef]
- Mikail, N.; Benali, K.; Mahida, B.; Vigne, J.; Hyafil, F.; Rouzet, F.; Le Guludec, D. 18F-FDG-PET/CT Imaging to Diagnose Septic Emboli and Mycotic Aneurysms in Patients with Endocarditis and Cardiac Device Infections. Curr. Cardiol. Rep. 2018, 20, 14. [Google Scholar] [CrossRef] [PubMed]
- Amraoui, S.; Tlili, G.; Sohal, M.; Berte, B.; Hindié, E.; Ritter, P.; Ploux, S.; Denis, A.; Derval, N.; Rinaldi, C.A.; et al. Contribution of PET Imaging to the Diagnosis of Septic Embolism in Patients with Pacing Lead Endocarditis. JACC Cardiovasc. Imaging 2016, 9, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Nakamoto, R.; Okuyama, C.; Ishizu, K.; Higashi, T.; Takahashi, M.; Kusano, K.; Kagawa, S.; Yamauchi, H. Diffusely Decreased Liver Uptake on FDG PET and Cancer-Associated Cachexia with Reduced Survival. Clin. Nucl. Med. 2019, 44, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Spencer, B.A.; McBride, K.; Hunt, H.; Jones, T.; Cherry, S.R.; Badawi, R.D. Practical Considerations for Total-Body PET Acquisition and Imaging. Methods Mol. Biol. 2024, 2729, 371–389. [Google Scholar] [CrossRef] [PubMed]
- Mingels, C.; Caobelli, F.; Alavi, A.; Sachpekidis, C.; Wang, M.; Nalbant, H.; Pantel, A.R.; Shi, H.; Rominger, A.; Nardo, L. Total-Body PET/CT or LAFOV PET/CT? Axial Field-of-View Clinical Classification. Eur. J. Nucl. Med. Mol. Imaging 2023. ahead of print. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
