Figure 1.
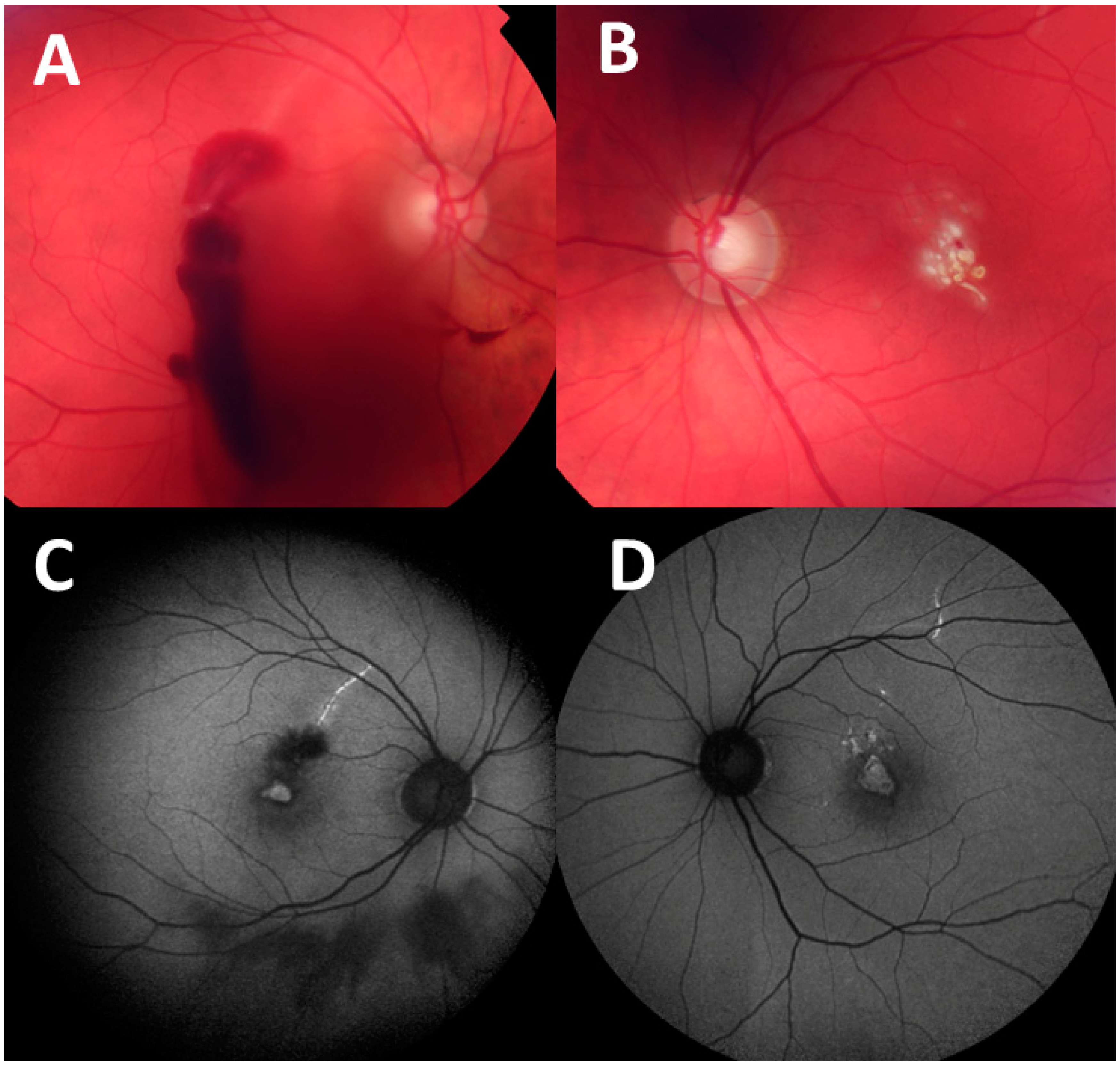
A 40-year-old patient presented after a self-inflicted injury by a handheld class 3 blue laser (450 nm) he purchased on the internet. The patient reported shining the laser through a window, which reflected the beam back into his eyes. The patient’s initial vision was 20/400 in both eyes. Fundus photographs taken at presentation show: (
A) vitreous and preretinal hemorrhages in the right eye and (
B) multiple yellow-white fresh laser burns in the central macula of the left eye. One month later, the patient was only able to count fingers with each eye. Fundus autofluorescence images taken at 1-month visit demonstrate hyperfluorescent curvilinear streaks in superior maculae in the right eye (
C) and left eye (
D). as well as hyperfluorescence in the fovea of both eyes. Retinal streaks point to self-inflicted laser injury, while peer-inflicted laser injuries have been described to result in focal foveal lesions [
1]. Retinal damage from laser pointers may vary in morphology and include subretinal or intraretinal hemorrhage, retinal edema, retinal pigment epithelium scarring, foveal granularity, vitreous or chorioretinal hemorrhage, perifoveal drusenoid-like deposits/pigment clumps, ring-shaped hypopigmented lesions in fovea, macular holes, and rarely, choroidal neovascularization [
2]. The Food and Drug Administration (FDA) have identified 4 major classes of lasers (1–4), of which laser pointers belong to class 3R [
3]. Exposures to direct and even reflected beam should be avoided without eye protection with class 3 or 4 lasers. Injuries to the eye can occur within moments with exposure to class 3 lasers emitting powers greater than 5 mW, and protective mechanisms of blinking or looking away are ineffective with such high powers. Labeling of the devices may not be accurate. The laser institute of America also cautions against pointing a laser at a mirror-like surface as the reflected beam may act like a direct beam on the eye [
3,
4].
Figure 1.
A 40-year-old patient presented after a self-inflicted injury by a handheld class 3 blue laser (450 nm) he purchased on the internet. The patient reported shining the laser through a window, which reflected the beam back into his eyes. The patient’s initial vision was 20/400 in both eyes. Fundus photographs taken at presentation show: (
A) vitreous and preretinal hemorrhages in the right eye and (
B) multiple yellow-white fresh laser burns in the central macula of the left eye. One month later, the patient was only able to count fingers with each eye. Fundus autofluorescence images taken at 1-month visit demonstrate hyperfluorescent curvilinear streaks in superior maculae in the right eye (
C) and left eye (
D). as well as hyperfluorescence in the fovea of both eyes. Retinal streaks point to self-inflicted laser injury, while peer-inflicted laser injuries have been described to result in focal foveal lesions [
1]. Retinal damage from laser pointers may vary in morphology and include subretinal or intraretinal hemorrhage, retinal edema, retinal pigment epithelium scarring, foveal granularity, vitreous or chorioretinal hemorrhage, perifoveal drusenoid-like deposits/pigment clumps, ring-shaped hypopigmented lesions in fovea, macular holes, and rarely, choroidal neovascularization [
2]. The Food and Drug Administration (FDA) have identified 4 major classes of lasers (1–4), of which laser pointers belong to class 3R [
3]. Exposures to direct and even reflected beam should be avoided without eye protection with class 3 or 4 lasers. Injuries to the eye can occur within moments with exposure to class 3 lasers emitting powers greater than 5 mW, and protective mechanisms of blinking or looking away are ineffective with such high powers. Labeling of the devices may not be accurate. The laser institute of America also cautions against pointing a laser at a mirror-like surface as the reflected beam may act like a direct beam on the eye [
3,
4].
![Diagnostics 14 00361 g001]()
Figure 2.
Optical coherence tomography (OCT) images taken at presentation show preretinal hemorrhage in the right eye (
A) and retinal disruption with preretinal hyper-reflective lesion in the left eye (
B). One month later, the OCT images demonstrate the development of full-thickness macular holes in the right (
C) and left eye (
D), and retinal pigment epithelium clumping and outer retinal atrophy in curvilinear streak areas in the right eye (
E). While laser-induced macular holes may spontaneously close, surgical intervention may be necessary for persistent cases and may result in increased visual acuity [
4]. Spectral domain OCT is reportedly a sensitive tool for evaluating retinal damage and the subsequent evolution of retinal changes [
5].
Figure 2.
Optical coherence tomography (OCT) images taken at presentation show preretinal hemorrhage in the right eye (
A) and retinal disruption with preretinal hyper-reflective lesion in the left eye (
B). One month later, the OCT images demonstrate the development of full-thickness macular holes in the right (
C) and left eye (
D), and retinal pigment epithelium clumping and outer retinal atrophy in curvilinear streak areas in the right eye (
E). While laser-induced macular holes may spontaneously close, surgical intervention may be necessary for persistent cases and may result in increased visual acuity [
4]. Spectral domain OCT is reportedly a sensitive tool for evaluating retinal damage and the subsequent evolution of retinal changes [
5].