Healing Architecture in Mental Health Facilities in the New European Bauhaus Context
Abstract
1. Introduction
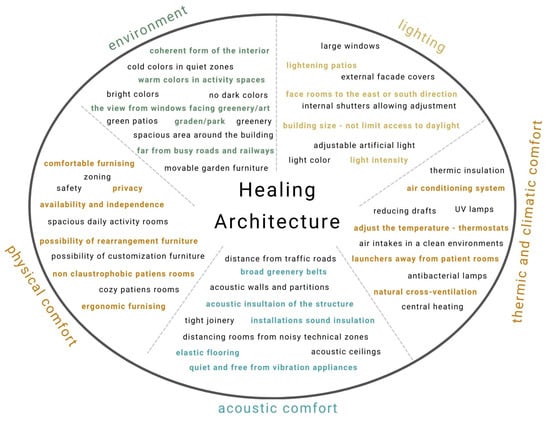
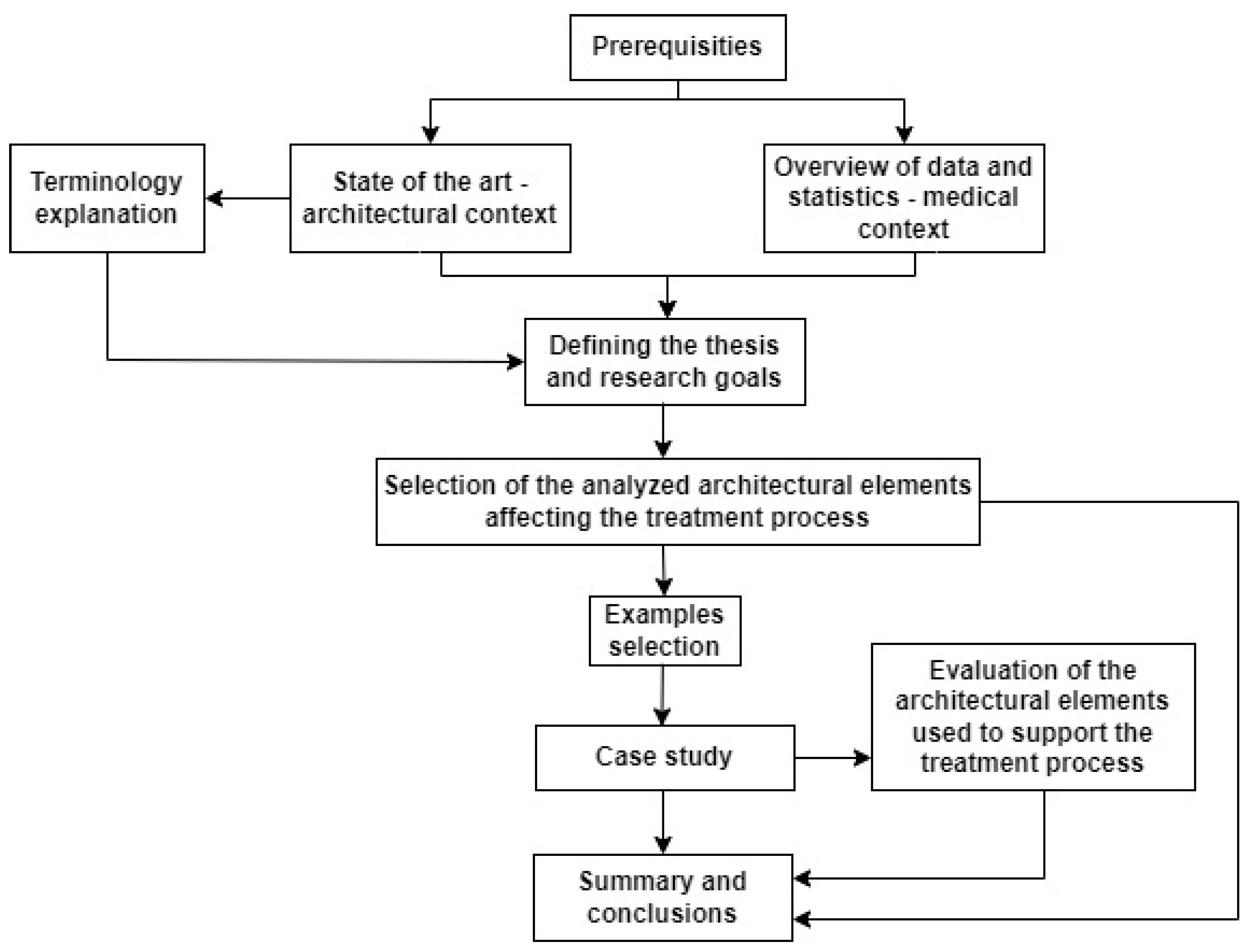
2. Materials and Methods
2.1. Research Structure
- Examining what issues related to architectural design influence the creation of healing architecture;
- Formulating criteria for designing model buildings that take into account the idea of healing architecture;
- Assessment of the quality of healing architecture of selected model examples of psychiatric care buildings.
- method of logical argumentation,
- case study,
- post-occupancy evaluation (POE), including three types: indicative—general; investigative—EBD Evidence-Based Design; and diagnostic (for conclusion formulation) [14].
- environment,
- lighting,
- thermal comfort and indoor climate,
- acoustic comfort,
- physical comfort.
2.2. The Initial Literature Overview
3. The Detailed Literature Overview in Terms of Architectural Features
3.1. Environment
- space to spend time outside,
- positive distractions,
- interiors as a peaceful environment.
3.2. Lighting
- effective use of natural light,
- limiting the unwanted influence of daylight,
- providing proper quality artificial light.
3.3. Thermic Comfort and Indoor Climate
- thermal comfort,
- air parameters,
- microbiological safety.
3.4. Acoustic Comfort
- external noise sources,
- internal noise sources,
- building compartment isolation properties,
- in-room noise limitation,
3.5. Physical Comfort
- building layout
- rooms size
- furnishings
3.6. Summary
4. Discussion
- Elsinore Psychiatric Hospital,
- Young Women’s Care Home for Mental Health Problems,
- Kronstad Psychiatric Hospital.
4.1. Elsinore Psychiatric Hospital, BIG (Bjarke Ingels Group), 2005
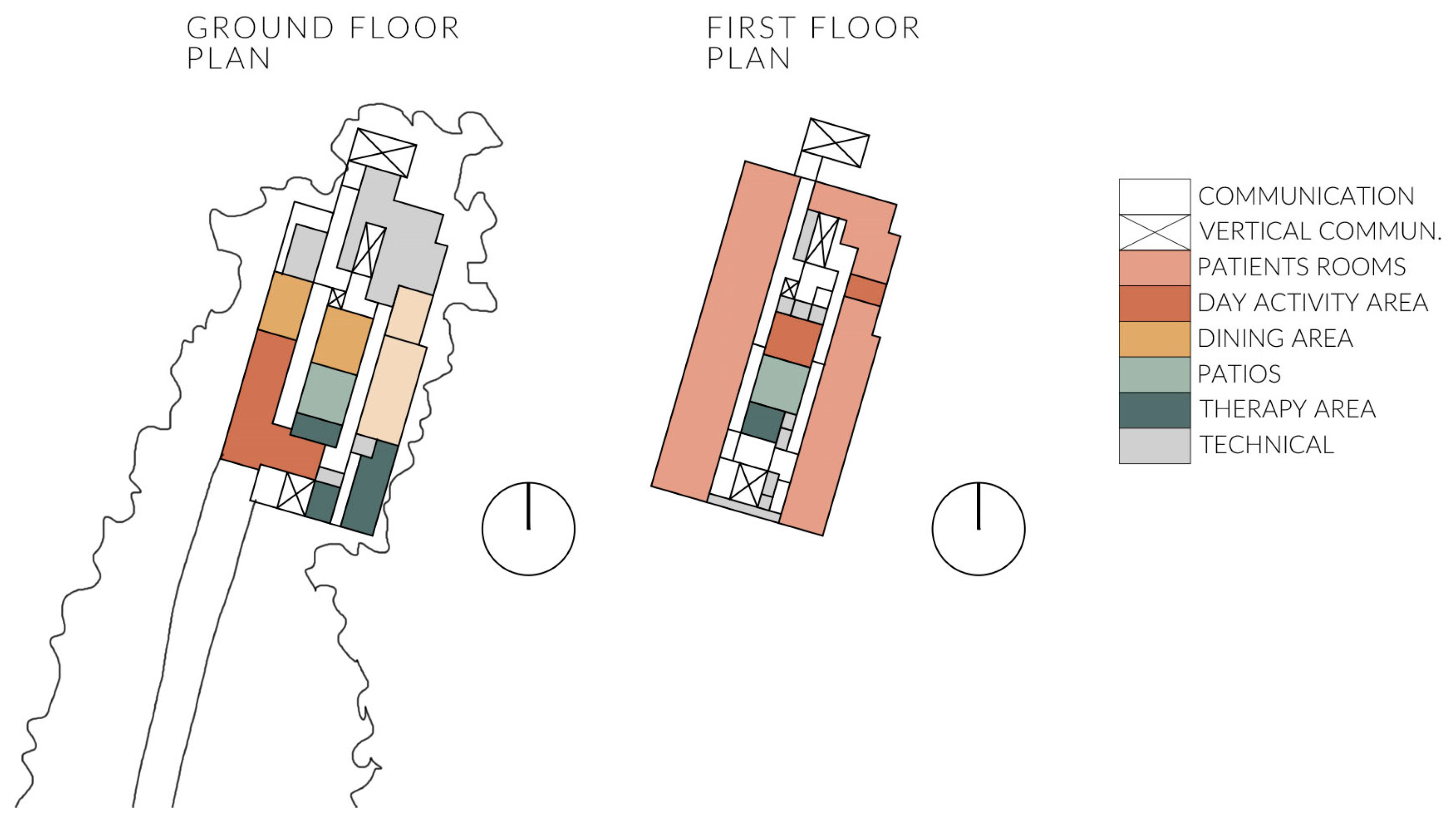
4.2. Young Women’s Care Home for Mental Health Problems, LDA.iMdA Architetti Associati, 2016
4.3. Kronstad Psychiatric Hospital, Origo Architekt Gruppe, 2013
5. Results and Conclusions
- Outdoor space:
- ○
- Positive distractions (i.e., urban elements, minor architectural solutions)
- ○
- Visually appealing and calming surroundings (also views from inside)
- Lighting:
- ○
- Effective use of natural light
- ○
- Limiting the unwanted influence of daylight
- ○
- Providing artificial light
- Thermic and thermal comfort
- Inner and outer air parameters
- Microbiological safety
- Acoustic comfort:
- ○
- Limitation of external noise sources
- ○
- Limitation of internal noise sources
- ○
- Building compartment isolation properties
- ○
- In-room and reverberation noise limitation (also a pleasant soundscape)
- Physical comfort
- Building layout and room sizes (in line with functions)
- Furnishing (in shared areas and adjustable to users’ needs)
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Willis, J.; Goad, P.; Logan, C. Architecture and the Modern Hospital. Nosokomeion to Hygeia; Taylor & Francis: Abingdon, UK, 2019. [Google Scholar]
- Kagan, A.R.; Levi, L. Health and environment—Psychosocial stimuli: A review. Soc. Sci. Med. 1974, 8, 225–241. [Google Scholar] [CrossRef] [PubMed]
- Antonovsky, A. Health, stress, and coping. New Perspect. Ment. Phys. Well-Being 1979, 2, 12–37. [Google Scholar]
- Ulrich, R.S. View Through a Window May Influence Recovery from Surgery. Science 1984, 224, 420–421. [Google Scholar] [CrossRef] [PubMed]
- Cooper, M.C.; Barnes, M. Healing Gardens: Therapeutic Benefits and Design Recommendations; John Wiley & Sons: New York, NY, USA, 1999. [Google Scholar]
- Becker, F.; Douglass, S. The ecology of the patient visit: Physical attractiveness, waiting times, and perceived quality of care. J. Ambul. Care Manag. 2008, 31, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Salonen, H.; Lahtinen, M.; Lappalainen, S.; Nevala, N.; Knibbs, L.D.; Morawska, L.; Reijula, K. Design approaches for promoting beneficial indoor environments in healthcare facilities: A review. Intell. Build. Int. 2013, 5, 26–50. [Google Scholar] [CrossRef]
- Singha, S. Future Healthcare Design; RIBA Publishing: London, UK, 2019. [Google Scholar]
- Singh, V.K.; Lillrank, P. Planning and Designing Healthcare Facilities; Taylor & Francis Group: Abingdon, UK, 2018. [Google Scholar]
- Ulrich, R.S. A theory of supportive design for healthcare facilities. J. Healthc. Desing 1997, 9, 97–109. [Google Scholar]
- Fricke, O.P.; Halswick, D.; Längler, A.; Martin, D.D. Healing Architecture for SickKids Concepts of Environmental and Architectural Factors in Child and Adolescents Psychiatry. Z. Für Kinder-Und Jugendpsychiatrie Und Psychother. 2023, 47, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Sadowski, K. Implementation of the New European Bauhaus Principles as a Context for Teaching Sustainable Architecture. Sustainability 2021, 13, 10715. [Google Scholar] [CrossRef]
- Torchia, D.; Fresta, J.; Corazza, L.; Certomà, C. New European Bauhaus for a Circular Economy and Waste Management: The Lived Experience of a Community Container Garden at the University of Turin. Sustainability 2021, 15, 914. [Google Scholar] [CrossRef]
- Niezabitowska, E. Research Methods and Techniques in Architecture; Wydawnictwo Politechniki Śląskiej: Gliwice, Poland, 2014. [Google Scholar]
- Groat, L.; Wang, D. Architectural Research Methods; John Wiley & Sons: New York, NY, USA, 2002. [Google Scholar]
- Ulrich, R.S. Effects of interior design on wellness: Theory and recent scientific research. J. Health Care Inter. Des. Proc. 1991, 3, 97–109. [Google Scholar]
- Garg, A.; Dewan, A. Manual of Hospital planning and Designing for Medical Administrators. In Architects and Planners; Springer: New York, NY, USA, 2022. [Google Scholar]
- Bellini, E.; Macchi, A.; Setola, N.; Lindahl, D. Sensory Design in the Birth Environment: Learning from Existing Case Studies. Buildings 2023, 13, 604. [Google Scholar] [CrossRef]
- Gross, R.; Sasson, Y.; Zohar, J. Healing environment in psychiatric hospital design. Gen. Hosp. Psychiatry 1998, 20, 108–114. [Google Scholar] [CrossRef] [PubMed]
- Lundin, S. Healing Architecture: Evidence, Intuition, Dialogue; Chalmers Tekniska Hogskola: Gothenburg, Sweden, 2015. [Google Scholar]
- Simonsen, T.P.; Duff, C. Healing architecture and psychiatric practice:(re) ordering work and space in an in-patient ward in Denmark. Sociol. Health Illn. 2020, 42, 379–392. [Google Scholar] [CrossRef] [PubMed]
- Ghazaly, M.; Badokhon, D.; Alyamani, N.; Alnumani, S. Healing architecture. Civ. Eng. Archit. 2020, 10, 108–117. [Google Scholar] [CrossRef]
- Thorben, P.H.S.; Brown, S.D.; Reavey, P. Vitality and nature in psychiatric spaces: Challenges and prospects for ‘healing architecture’ in the design of inpatient mental health environments. Health Place 2024, 85, 103–169. [Google Scholar]
- Ulrich, R.S.; Cordoza, M.; Hazen, T.; Perkins, S. ICU patient family stress recovery during breaks in a hospital garden and indoor environments. HERD Health Environ. Res. Des. J. 2020, 13, 83–102. [Google Scholar] [CrossRef] [PubMed]
- Nanda, U.; Eisen, S.; Zadeh, R.S.; Owen, D. Effect of visual art on patient anxiety and agitation in a mental health facility and implications for the business case. J. Psychiatr. Ment. Health Nurs. 2011, 18, 386–393. [Google Scholar] [CrossRef]
- Naglaa, E.S. The Impact of Architectural Psychology on the Interior Design of Psychiatric Hospitals. J. Des. Sci. Appl. Arts 2021, 2, 41–59. [Google Scholar]
- Dalke, H.; Little, J.; Niemann, E.; Camgoz, N.; Steadman, G.; Hill, S.; Stott, L. Colour and lighting in hospital design. Opt. Laser Technol. 2006, 38, 343–365. [Google Scholar] [CrossRef]
- Sorensen, W. Designing for Mental Health Facilities: Two Major Factors That Promote Occupant Wellbeing; Utah State University: Logan, UT, USA, 2018. [Google Scholar]
- Karlin, B.E.; Zeiss, R.A. Best Practices: Environmental and Therapeutic Issues in Psychiatric Hospital Design: Toward Best Practices. Psychiatr. Serv. 2006, 57, 1376–1378. [Google Scholar] [CrossRef]
- Connellan, K.; Gaardboe, M.; Riggs, D.; Due, C.; Reinschmidt, A.; Mustillo, L. Stressed Spaces: Mental Health and Architecture. HERD Health Environ. Res. Des. J. 2013, 6, 127–168. [Google Scholar] [CrossRef] [PubMed]
- Bedrosian, T.A.; Nelson, R.J. Timing of light exposure affects mood and brain circuits. Transl. Psychiatry 2017, 7, e1017. [Google Scholar] [CrossRef] [PubMed]
- Humble, M.B. Vitamin D, light and mental health. J. Photochem. Photobiol. B Biol. 2010, 101, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Randle, H.W. Suntanning: Differences in Perceptions Throughout History. Mayo Clin. Proc. 1997, 5, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Aries, M.B.; Aarts, M.P.; van Hoof, J. Daylight and health: A review of the evidence and consequences for the built environment. Light. Res. Technol. 2015, 47, 6–27. [Google Scholar] [CrossRef]
- Winkel, G.H.; Hlahan, C.J. The environmental psychology of the hospital: Is the cure worse than the illness? J. Prev. Interv. Community 1985, 1–2, 11–33. [Google Scholar] [CrossRef]
- Ferrante, T.; Villani, T. Pre-Occupancy Evaluation in Hospital Rooms for Efficient Use of Natural Light—Improved Proposals. Buildings 2022, 12, 2145. [Google Scholar] [CrossRef]
- How Color Affects Architecture. Available online: https://www.archdaily.com/930266/how-color-affects-architecture (accessed on 16 November 2023).
- McKinney, M.E.; Gatchel, R.J.; Brantley, D.; Harrington, R. The impact of biofeedback-manipulated physiological change on emotional state. Basic Appl. Soc. Psychol. 1980, 1, 15–21. [Google Scholar] [CrossRef]
- Pieczara, J. Naturalne Przewietrzanie i Komfort Termiczny w Budynkach Użyteczności Publicznej; Teka Komisji Architektury Urbanistyki i Studiów Krajobrazowych: Warsaw, Poland, 2016. [Google Scholar]
- Butera, F.M. Principles of thermal comfort. Renew. Sustain. Energy Rev. 1998, 2, 39–66. [Google Scholar] [CrossRef]
- Wang, Z.; de Dear, R.; Luo, M.; Lin, B.; He, Y.; Ghahramani, A.; Zhu, Y. Individual difference in thermal comfort: A literature review. Build. Environ. 2018, 138, 181–193. [Google Scholar] [CrossRef]
- Alotaibi, B.S.; Lo, S. Thermal environment perceptions from a longitudinal study of indoor temperature profiles in inpatient wards. Buildings 2020, 10, 136. [Google Scholar] [CrossRef]
- Djongyang, N.; Tchinda, R.; Njomo, D. Thermal comfort: A review paper. Renew. Sustain. Energy Rev. 2010, 14, 2626–2640. [Google Scholar] [CrossRef]
- Brown, D.; Martiskainen, M. How sociotechnical norms shape transition pathways: The co-evolution of three European heating, ventilation, and cooling (HVAC) regimes. Energy Res. Soc. Sci. 2024, 107, 103–346. [Google Scholar] [CrossRef]
- Verheye, J. Thermal comfort of patients: Objective and subjective measurements in patient rooms of a Belgian healthcare facility. Build. Environ. 2011, 46, 1195–1204. [Google Scholar] [CrossRef]
- Brelih, N. Thermal and acoustic comfort requirements in European standards and national regulations. Fed. Eur. Heat. Vent. Air Cond. Assoc. (REHVA) J. 2013, 4, 16–19. [Google Scholar]
- Rey, F.J.; Velasco, E. Experimental study of indoor air quality, energy saving and analysis of ventilation norms in climatised areas. Energy Build. 2020, 33, 57–67. [Google Scholar] [CrossRef]
- Ülar, P.; Kurnitski, J.; Voll, H. Design criteria for outdoor air intakes and exhaust air outlets located on an external wall Jarek Kurnitski. E3S Web Conf. EDP Sci. 2020, 172, 09008. [Google Scholar]
- Kuborn, X.; Pecceu, S. A Study of the Influence of the Position of a Chimney Terminal on the Vertical Walls of a Building on the Air Quality of the Ventilation Air Supply. In Proceedings of the 40th AIVC—8th TightVent—6th venticool Conference, Ghent, Belgium, 15–16 October 2019. [Google Scholar]
- Chohan, A.H.; Awad, J. Wind Catchers: An Element of Passive Ventilation in Hot, Arid and Humid Regions, a Comparative Analysis of Their Design and Function. Sustainability 2022, 14, 11088. [Google Scholar] [CrossRef]
- Aldawoud, A. Windows design for maximum cross-ventilation in buildings. Adv. Build. Energy Res. 2017, 11, 67–86. [Google Scholar] [CrossRef]
- Pibiri, M.C. Indoor air purification and ventilation systems sanitation with essential oils. Int. J. Aromather. 2006, 16, 149–153. [Google Scholar] [CrossRef]
- Lualdi, M.; Cavalleri, A.; Bianco, A.; Biasin, M.; Cavatorta, C.; Clerici, M.; Galli, P.; Pareschi, G.; Pignoli, E. Ultraviolet C lamps for disinfection of surfaces potentially contaminated with SARS-CoV-2 in critical hospital settings: Examples of their use and some practical advice. BMC Infect. Dis. 2021, 21, 594. [Google Scholar] [CrossRef] [PubMed]
- Leone, M.J.; Dasht, H.S.; Coughlin, B.; Tesh, R.A.; Quadri, S.A.; Bucklin, A.A.; Aoor, A.; Krishnamurthy, P.V.; Ye, E.M.; Hemmige, A.; et al. Sound and light levels in intensive care units in a large urban hospital in the United States. Chronobiol. Int. 2023, 40, 759–768. [Google Scholar] [CrossRef] [PubMed]
- Lindborg, P.; Lenzi, S.; Han, N.; Spagnol, S.; Kamphuis, D.J.; Özcan, E.; Quek, A. Disturbed Sleep: Estimating Night-time Sound Annoyance at a Hospital Ward. In Proceedings of the Forum Acousticum, 10th Convention of the European Acoustics Association, Torino, Italy, 1 January 2023. [Google Scholar]
- Juraszyński, J.; Nitsch, A.; Porębowicz, S.; Radwański, Z. Projektowanie Obiektów Służby Zdrowia; Arkady: Warsaw, Poland, 1973. [Google Scholar]
- Freire, S.; Gomes, N. Advancing Environmental Noise Pollution Analysis in Urban Areas By Considering the Variation of Population Exposure in Space and Time. Int. Arch. Photogramm. Remote Sens. Spat. Inf. Sci. 2013, 40, 155–160. [Google Scholar] [CrossRef]
- Cai, M.; Lan, Z.; Zhang, Z.; Wang, H. Evaluation of road traffic noise exposure based on high-resolution population distribution and grid-level noise data. Build Environ. 2019, 147, 211–220. [Google Scholar] [CrossRef]
- Peris, E. Noise Pollution is a Major Problem, Both for Human Health and the Environment, Interview with Peris. E.; European Environmental Agency (EEA): Copenhagen, Denmark, 2020; 01. [Google Scholar]
- Directive 2002/49/EC of the European Parliament and of the Council of 25 June 2002 Relating to the Assessment and Management of Environmental Noice, 18/07/2002 ed. Official Journal L 189. pp. 0012–0026. Available online: https://eur-lex.europa.eu/eli/dir/2002/49/oj (accessed on 4 September 2019).
- ArAc-Multibook—Multimedia textbook for architectural acoustics, International Partnership ArAc-Multibook. 2015. Available online: https://arac-multibook.com/ (accessed on 27 January 2024).
- Everest, F.A.; Pohlmann, K.C. Master Handbook of Acoustics 2014; Mc Graw Hill: New York, NY, USA, 2014. [Google Scholar]
- Beldam, M.B. Short reverberation time in critical care is not enough. In Acoustic Bulletin, Ecophon; Acoustic Bulletin: Helsingborg, Sweden, 2018; Available online: https://www.acousticbulletin.com/short-reverberation-time-critical-care-not-enough/ (accessed on 9 November 2023).
- PN-B-02151-2:2018-01; Polish Norm Building Acoustics—Requirements Regarding Accept-Able Sound Level in Rooms Determines the Maximum Noise Level A of Noise in Rooms Intended for Human Stay—In Residential Buildings and Public Buildings. Polish Normalization Committee (PKN): Warsaw, Poland, 2018.
- PN-B-02151-4; Building Acoustics. Protection from noise in buildings. Part 4: Requirements for reverberation conditions and speech intelligibility in rooms with guidelines for conducting research. Polish Normalization Committee (PKN): Warsaw, Poland, 2015.
- Carthey, J.F. Australasian Health Facility Guidelines: Results of a user survey. Facilities 2013, 31, 574–590. [Google Scholar] [CrossRef]
- Chohan, A.H.; Awad, J. Shaping the Architects of Tomorrow, Interplay of Teaching Philosophies and Practice Requirements: An Empirical Taxonomy of Professional Architectural Practice in the UAE. Buildings 2023, 13, 1231. [Google Scholar] [CrossRef]
- Big—Bjarke Ingels Group, Jds. Julien De Smedt Architects. Available online: https://divisare.com/projects/218546-big-bjarke-ingels-group-jds-julien-de-smedt-architects-ellsinore-psychiatric-clinic (accessed on 5 February 2024).
- Google Maps. Available online: https://www.google.com/maps/ (accessed on 27 January 2024).
- Helsingør Psychiatric Hospital. Available online: https://www.archiweb.cz/en/b/psychiatricka-klinika (accessed on 27 January 2024).
- Psychiatric Hospital, Helsingør. Available online: https://arquitecturaviva.com/works/hospital-psiquiatrico-4#lg=1&slide=2 (accessed on 27 January 2024).
- Elsinor. Available online: https://arquitecturaviva.com/tag/elsinor (accessed on 5 February 2024).
- Psychiatric Hospital Helsingor. Available online: https://architizer.com/projects/psychiatric-hospital-helsingor/ (accessed on 5 February 2024).
- Casa Verde. Available online: https://divisare.com/projects/375231-lda-imda-architetti-associati-simone-bossi-casa-verde-young-women-s-care-home-for-mental-health-problems (accessed on 6 February 2024).
- Casa Verde Young Women’s Care Home for Mental Health. Available online: https://www.archdaily.com/886409/casa-verde-young-womens-care-home-for-mental-health-ldmda-architetti-associati (accessed on 27 January 2024).
- Casa Verde Young Women’s Care Home for Mental Health Problems. Available online: https://architizer.com/projects/casa-verde-young-womens-care-home-for-mental-health-problems/ (accessed on 6 February 2024).
- Two Layers of Microperforated Aluminum for the Façade of LDA.iMDA’s Casa Verde. Available online: https://www.floornature.com/architectural-solutions/two-layers-microperforated-aluminium-facade-ldaimdaas-casa-v-16458/ (accessed on 6 February 2024).
- Kronstad Psychiatric Hospital. Available online: https://www.archdaily.com/451158/kronstad-origo-arkitektgruppe (accessed on 6 February 2024).
- Kronstad Psychiatric Centre, Bergen. Available online: https://www.architecturenorway.no/projects/working/kronstad-2013/ (accessed on 7 February 2024).



| Environment | Criterium |
| Outdoor space |
|
| Positive distractions |
|
| Visually appealing and calming surroundings |
|
| Lighting | Criterium |
| Effective use of natural light |
|
| Limiting the unwanted influence of daylight |
|
| Providing artificial light |
|
| Thermic Comfort | Criterium |
| Thermal comfort |
|
| Air parameters |
|
| Microbiological safety |
|
| Acoustic Comfort | Criterium |
| Limitation of external noise sources |
|
| Limitation of internal noise sources |
|
| Building compartment isolation properties |
|
| In-room noise limitation |
|
| Reverberation noise limitation |
|
| Physical Comfort | Criterium |
| Building layout |
|
| Room size |
|
| Furnishing |
|
| Environment Criterium | Case Study 1 | Case Study 2 | Case Study 3 |
| + | + | − |
| + | + | − |
| + | + | + |
| + | + | + |
| + | No data | + |
| + | + | + |
| + | + | − |
| + | + | + |
| − | + | + |
| + | + | + |
| + | + | + |
| + | + | + |
| − | + | + |
| Lighting Criterium | Case Study 1 | Case Study 2 | Case Study 3 |
| + | + | +/− |
| + | − | + |
| + | + | + |
| + | + | + |
| + | + | + |
| − | + | − |
| − | + | − |
| Thermic Comfort Criterium | Case Study 1 | Case Study 2 | Case Study 3 |
| + | No data | + |
| − | + | + |
| + | + | + |
| + | + | + |
| No data | + | No data |
| No data | + | No data |
| + | + | + |
| − | − | − |
| + | + | + |
| Acoustic Comfort Criterium | Case Study 1 | Case Study 2 | Case Study 3 |
| + | + | − |
| + | + | − |
| + | + | + |
| + | + | + |
| + | + | + |
| + | + | + |
| + | + | + |
| + | + | + |
| + | + | + |
| + | − | + |
| + | + | + |
| Physical Comfort Criterium | Case Study 1 | Case Study 2 | Case Study 3 |
| + | + | + |
| + | + | + |
| − | + | − |
| + | + | + |
| + | + | + |
| + | + | + |
| + | No data | No data |
| + | No data | − |
| + | + | + |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jablonska, J.; Furmanczyk, J. Healing Architecture in Mental Health Facilities in the New European Bauhaus Context. Buildings 2024, 14, 1056. https://doi.org/10.3390/buildings14041056
Jablonska J, Furmanczyk J. Healing Architecture in Mental Health Facilities in the New European Bauhaus Context. Buildings. 2024; 14(4):1056. https://doi.org/10.3390/buildings14041056
Chicago/Turabian StyleJablonska, Joanna, and Jozefina Furmanczyk. 2024. "Healing Architecture in Mental Health Facilities in the New European Bauhaus Context" Buildings 14, no. 4: 1056. https://doi.org/10.3390/buildings14041056
APA StyleJablonska, J., & Furmanczyk, J. (2024). Healing Architecture in Mental Health Facilities in the New European Bauhaus Context. Buildings, 14(4), 1056. https://doi.org/10.3390/buildings14041056