The Noise: A Silent Threat to the Recovery of Patients in Neonatal Intensive Care Units
Abstract
1. Introduction
1.1. Effects of Noise on Premature Neonates
1.2. Noise Levels in Neonatal Intensive Care Units
1.3. Noise Levels in Incubators
1.4. Noise Reduction in NICUs
2. Methodology
2.1. Material and Methods
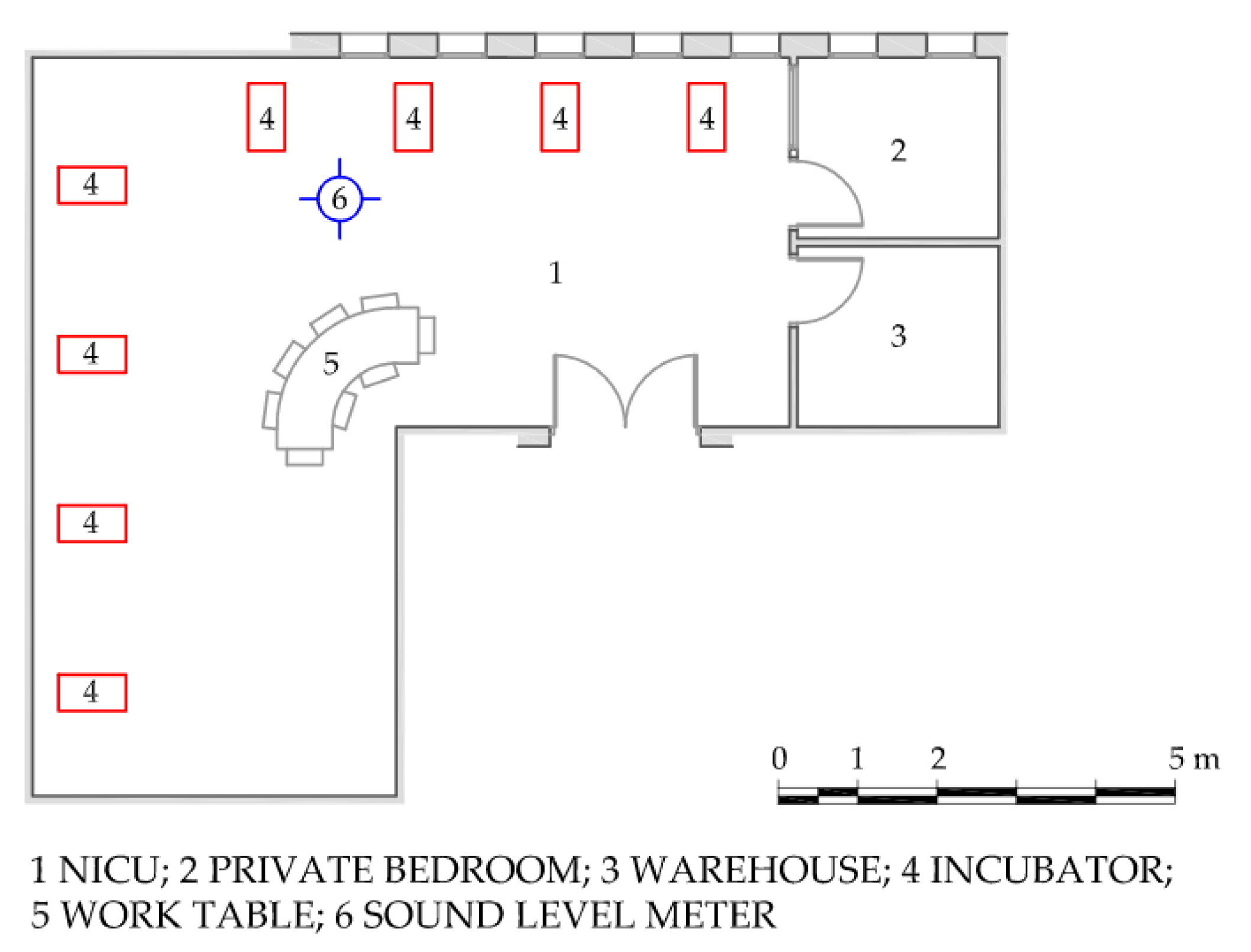
2.2. Features of NICUs
2.2.1. Puerta del Mar University Hospital (HUPM)
2.2.2. Juan Ramón Jiménez University Hospital (HJRJ)
2.3. Data Analysis
- H1. There are no differences between the sound pressure levels measured during the day period (8:00 a.m.–10:00 p.m., excluding feeding periods and shift changes) in the NICU of the HJRJ and the HUPM;
- H2. There are no differences between the sound pressure levels measured during the night period (10:00 p.m.–8:00 a.m.), excluding feeding periods and shift changes) in the NICUs of the HJRJ and the HUPM;
- H3. There are no differences between the sound pressure levels of the daytime feeding periods (10:00 p.m.–8:00 a.m.) in the NICUs of the HJRJ and the HUPM;
- H4. There are no differences between the sound pressure levels of the nocturnal feeding periods (8:00 a.m. to 10:00 p.m.) in the NICUs of the HJRJ and the HUPM;
- H5. There are no differences between the sound pressure levels of the shift changes of healthcare personnel (8:00 a.m. to 10:00 p.m.) in the NICUs of the HJRJ and the HUPM.
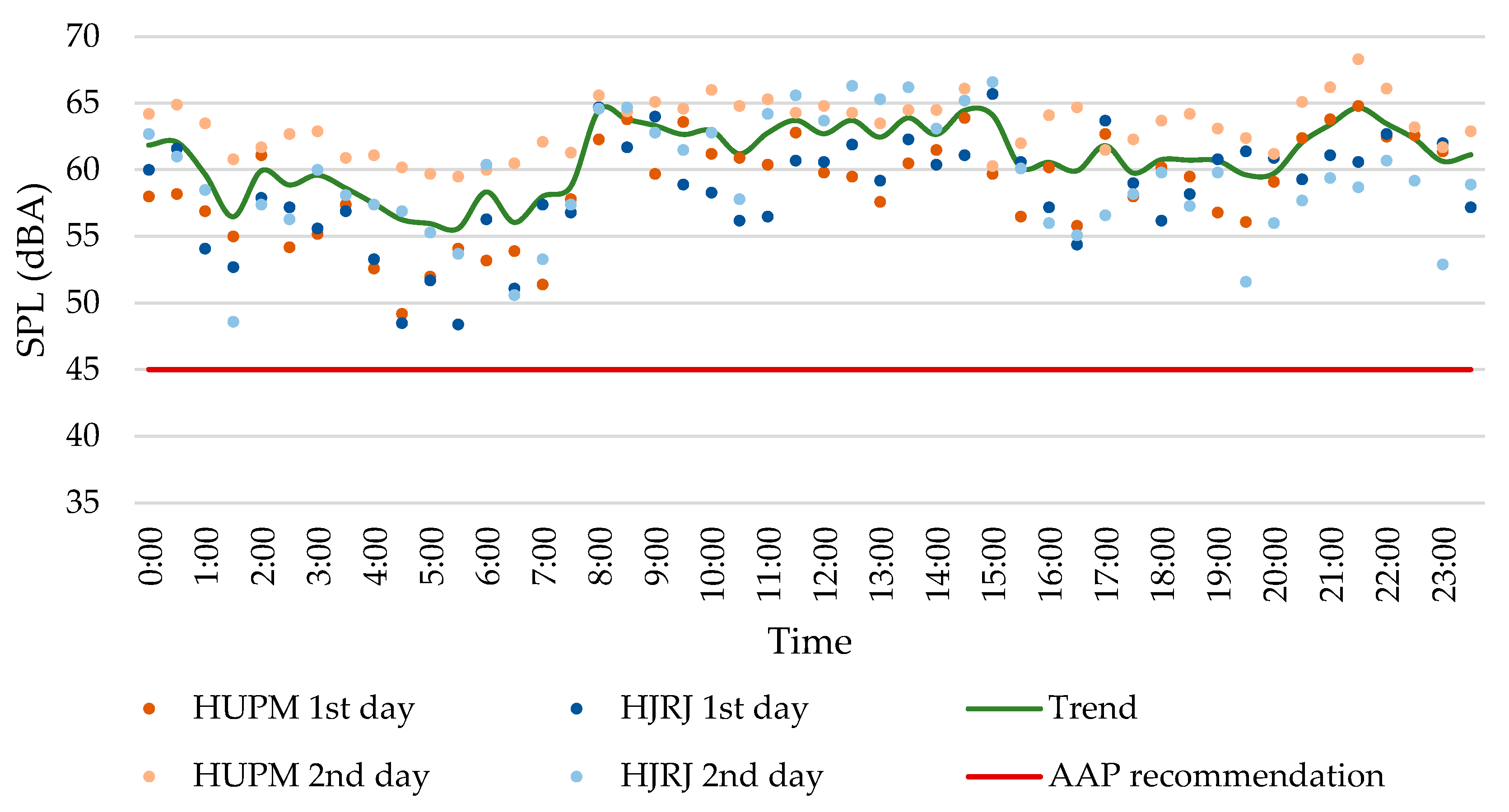
3. Results
3.1. Descriptive Analysis Result
3.2. Statistical Analysis Result
4. Discussion
- V represents the volume of the analysed room in m3.
- A denotes the equivalent acoustic absorption area in m2.
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
- LAeq: A-weighted equivalent continuous sound level;
- LCeq: C-weighted equivalent continuous sound level, LCeq;
- LAIeq; A-weighted Impulsive equivalent continuous sound level;
- LZeq: linear equivalent continuous sound level;
- LAFmin: minimum A-weighted equivalent continuous sound level, measured in an integration period of 0.125 ms (fast);
- LAFmin: maximum A-weighted equivalent continuous sound level, measured in an integration period of 0.125 ms (fast);
- LA10: A-weighted sound pressure level exceeded for 10% of the time;
- LA50: A-weighted sound pressure level exceeded for 50% of the time;
- LA90: A-weighted sound pressure level exceeded for 90% of the time.
References
- Graven, S.N.; Browne, J.V. Auditory Development in the Fetus and Infant. Newborn Infant. Nurs. Rev. 2008, 8, 187–193. [Google Scholar] [CrossRef]
- Duffy, N.; Hickey, L.; Treyvaud, K.; Delany, C. The lived experiences of critically ill infants hospitalised in neonatal intensive care: A scoping review. Early Hum. Dev. 2020, 151, 105244. [Google Scholar] [CrossRef]
- Philpott-Robinson, K.; Lane, S.J.; Korostenski, L.; Lane, A.E. The impact of the Neonatal Intensive Care Unit on sensory and developmental outcomes in infants born preterm: A scoping review. Br. J. Occup. Ther. 2017, 80, 459–469. [Google Scholar] [CrossRef]
- Sehgal, A.; Stack, J. Developmentally Supportive Care and NIDCAP. Indian J. Pediatr. 2006, 73, 1007–1010. [Google Scholar] [CrossRef] [PubMed]
- Als, H.; Lester, B.M.; Tronick, E.Z.; Brazelton, T.B. Toward a research instrument for the assessment of preterm infants’ behavior (APIB). In Theory and Research in Behavioral Pediatrics; Fitzgerald, H.E., Lester, B.M., Yogman, M.W., Eds.; Springer: Boston, MA, USA, 1982; pp. 35–63. [Google Scholar] [CrossRef]
- VanderBerg, K. Individualized developmental care for high risk newborns in the NICU: A practice guideline. Early Hum. Dev. 2007, 83, 433–442. [Google Scholar] [CrossRef]
- Cannizzaro, C.M.; Paladino, M.A. Fisiología y fisiopatología de la adaptación neonatal. Anest. Analg. Reanim. 2011, 24, 59–74. [Google Scholar]
- Bhutta, A.T.; Anand, J.S. Vulnerability of the developing brain. Neuronal mechanisms. Clin. Perinatol. 2002, 29, 357–372. [Google Scholar] [CrossRef]
- Orsi, K.C.; Avena, M.J.; Lurdes de Cacia Pradella-Hallinan, M.; da Luz Gonçalves Pedreira, M.; Tsunemi, M.H.; Machado Avelar, A.F.; Pinheiro, E.M. Effects of Handling and Environment on Preterm Newborns Sleeping in Incubators. J. Obs. Gynecol. Neonatal Nurs. 2017, 46, 238–247. [Google Scholar] [CrossRef]
- Smith, S.W.; Ortmann, A.J.; Clark, W.W. Noise in the neontal intensive care unit: A new approach to examining acoustic events. Noise Health 2018, 20, 121–130. [Google Scholar] [CrossRef]
- Cardoso, S.M.S.; Kozlowski, L.C.; de Lacerda, A.B.M.; Marques, J.M.; Ribas, A. Newborn physiological responses to noise in the neonatal unit. Braz. J. Otorhinolaryngol. 2015, 81, 583–588. [Google Scholar] [CrossRef] [PubMed]
- Haslbeck, F.B. Music therapy for premature infants and their parents: An integrative review. Nord. J. Music Ther. 2012, 21, 203–226. [Google Scholar] [CrossRef]
- Peng, N.; Bachman, J.; Jenkins, R.; Chen, C.; Chang, Y. Relationships between environmental stressors and stress biobehavioral responses of preterm infants in NICU. Adv. Neonatal Care 2013, 13, S2–S10. [Google Scholar] [CrossRef]
- Graven, S.N. Early neurosensory visual development of the fetus and newborn. Clin. Perinatol. 2004, 31, 199–216. [Google Scholar] [CrossRef] [PubMed]
- Hooks, B.M.; Chen, C. Critical periods in the visual system: Changing views for a model of experience-dependent plasticity. Neuron 2007, 56, 312–326. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, J.S.; Stryker, M.P. Development and plasticity of the primary visual cortex. Neuron 2012, 75, 230–249. [Google Scholar] [CrossRef] [PubMed]
- Beira Jiménez, J.L. Afección Acústica de Pacientes en Incubadoras. Caso de Estudio: Neonatos Prematuros en el Hospital Universitario Puerta del Mar de Cadiz. Ph.D. Thesis, Universidad de Cádiz, Cadiz, Spain, 2021. [Google Scholar]
- Gabor, J.; Cooper, A.; Hanly, P. Sleep disruption in the intensive care unit. Curr. Opin. Crit. Care 2001, 7, 21–27. [Google Scholar] [CrossRef] [PubMed]
- Reinke, L.; Haveman, M.; Horsten, S.; Falck, T.; Heide, E.M.; Pastoor, S.; Hoeven, J.H.; Absalom, A.R.; Tulleken, J.E. The importance of the intensive care unit environment in sleep—A study with healthy participants. J. Sleep Res. 2020, 29, e12959. [Google Scholar] [CrossRef]
- Aaron, J.N.; Carlisle, C.C.; Carskadon, M.A.; Meyer, J.; Hill, N.S.; Millman, R.P. Environmental noise as a cause of sleep disruption in an intermediate respiratory care unit. Sleep 1996, 19, 707–710. [Google Scholar] [CrossRef]
- Almadhoob, A.; Ohlsson, A. Sound reduction management in the neonatal intensive care unit for preterm or very low birth weight infants. Cochrane Database Syst. Rev. 2020, 1, CD010333. [Google Scholar] [CrossRef]
- Morris, B.H.; Philbin, M.K.; Bose, C. Physiological effects of sound on the newborn. J. Perinatol. 2000, 20, S55–S60. [Google Scholar] [CrossRef]
- Wachman, E.M.; Lahav, A. The effects of noise on preterm infants in the NICU. Arch. Dis. Child. Fetal Neonatal Ed. 2011, 96, F305–F309. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Montaño, V. Análisis del Acondicionamiento Acústico del Habitáculo de una Incubadora Neonatal: Propuestas de Mejora. Master’s Thesis, Universidad de Cádiz, Cadiz, Spain, 2018. [Google Scholar]
- Muñoz Illescas, M.L.; Sevilla Salgado, S.; Pérez Lafuente, E. Tecnología y mínima manipulación en prematuros. Enfermería Integral Rev. Científica Col. Of. Enfermería Valencia 2017, 116, 41–45. [Google Scholar]
- Guerra Rodríguez, A.E. Alteraciones del Sueño en los Pacientes Pediátricos Hospitalizado. Ph.D. Thesis, Universidad Autónoma de Nuevo León, San Nicolás de los Garza, Mexico, 2023. [Google Scholar]
- Sibrecht, G.; Wróblewska-Seniuk, K.; Bruschettini, M. Noise or sound management in the neonatal intensive care unit for preterm or very low birth weight infants. Cochrane Database Syst. Rev. 2024, 5, CD010333. [Google Scholar] [CrossRef] [PubMed]
- Wroblewska-Seniuk, K.; Greczka, G.; Dabrowski, P.; Szyfter-Harris, J.; Mazela, J. Hearing impairment in premature newborns—Analysis based on the national hearing screening database in Poland. PLoS ONE 2017, 12, e0184359. [Google Scholar] [CrossRef]
- Hille, E.T.; van Straaten, H.I.; Verkerk, P.H.; Dutch NICU Neonatal Hearing Screening Working Group. Prevalence and independent risk factors for hearing loss in NICU infants. Acta Paediatr. 2007, 96, 1155–1158. [Google Scholar] [CrossRef]
- Nair, V.; Janakiraman, S.; Whittaker, S.; Quail, J.; Foster, T.; Loganathan, P.K. Permanent childhood hearing impairment in infants admitted to the neonatal intensive care unit: Nested case-control study. Eur. J. Pediatr. 2021, 180, 2083–2089. [Google Scholar] [CrossRef]
- Joint Committee on Infant Hearing. Year 2019 position statement: Principles and guidelines for early hearing detection and intervention programs. J. Early Hear. Detect. Interv. 2019, 4, 1–44. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Noise: A hazard for the fetus and newborn. Pediatrics 1997, 100, 724–727. [Google Scholar] [CrossRef]
- White, R.D. Recommended standards for newborn ICU design. J. Perinatol. 2007, 27, S4–S19. [Google Scholar] [CrossRef]
- Sánchez Gómez, S. Effects of acoustic pollution on health. Rev. Salud Ambient. 2007, 7, 175–180. [Google Scholar]
- Altimier, L.; Barton, S.A.; Bender, J.; Browne, J.; Harris, D.; Jaeger, C.B.; Johnson, B.H.; Kenner, C.; Kolberg, K.J.S.; Loder, A.; et al. Recommended standards for newborn ICU design. J. Perinatol. 2023, 43 (Suppl. 1), 2–16. [Google Scholar] [CrossRef] [PubMed]
- Puyana-Romero, V.; Núñez-Solano, D.; Hernández-Molina, R.; Jara-Muñoz, E. Influence of the NICU on the Acoustic Isolation of a Neonatal Incubator. Front. Pediatr. 2020, 8, 588. [Google Scholar] [CrossRef]
- Hutchinson, G.; Du, L.; Ahmad, K. Incubator-based Sound Attenuation: Active Noise Control In A Simulated Clinical Environment. PLoS ONE 2020, 15, e0235287. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Salazar, A.D.; Gallegos-Martínez, J.; Reyes-Hernández, J. Level and Noise Sources in the Neonatal Intensive Care Unit of a Reference Hospital. Investig. Educ. Enferm. 2020, 38, e13. [Google Scholar] [CrossRef]
- Hernández-Molina, R.; Beira-Jiménez, J.L.; Rodríguez-Montaño, V.; Fernández Zacarías, F.; Bienvenido-Huertas, D.; Lubián López, S.; Cueto-Ancela, J.L. Characterizing the acoustic environment in a Neonatal Intensive Care Unit. Appl. Acoust. 2020, 165, 107301. [Google Scholar] [CrossRef]
- Williams, A.L.; van Drongelen, W.; Lasky, R.E. Noise in contemporary neonatal intensive care. J. Acoust. Soc. Am. 2007, 121, 2681–2690. [Google Scholar] [CrossRef] [PubMed]
- Lasky, R.E.; Williams, A.L. Noise and light exposures for extremely low birth weight newborns during their stay in the neonatal intensive care unit. Pediatrics 2009, 123, 540–546. [Google Scholar] [CrossRef]
- Casey, L.; Fucile, S.; Flavin, M.; Dow, K. A two-pronged approach to reduce noise levels in the neonatal intensive care unit. Early Hum. Dev. 2020, 146, 105073. [Google Scholar] [CrossRef]
- Pineda, R.; Durant, P.; Mathur, A.; Inder, T.; Wallendorf, M.; Schlaggar, B.L. Auditory Exposure in the Neonatal Intensive Care Unit: Room Type and Other Predictors. J. Pediatr. 2017, 183, 56–66.e3. [Google Scholar] [CrossRef]
- Liu, W. Comparing sound measurements in the single-family room with open unit design neonatal intensive care unit: The impact of equipment noise. J. Perinatol. 2012, 32, 368–373. [Google Scholar] [CrossRef]
- Pineda, R.; Neil, J.; Dierker, D.; Smyser, C.D.; Wallendorf, M.; Kidokoro, H.; Reynolds, L.C.; Walker, S.; Rogers, C.; Mathur, A.M.; et al. Alterations in brain structure and neurodevelopmental outcome in preterm infants hospitalized in different neonatal intensive care unit environments. J. Pediatr. 2014, 164, 52–60.e2. [Google Scholar] [CrossRef] [PubMed]
- Pineda, R.; Stransky, K.; Rogers, C.; Duncan, M.H.; Smith, G.C.; Neil, J.; Inder, T. The single-patient room in the NICU: Maternal and family effects. J. Perinatol. 2012, 32, 545–551. [Google Scholar] [CrossRef]
- Domanico, R.; Davis, D.K.; Coleman, F.; Davis, B.O. Documenting the NICU design dilemma: Comparative patient progress in open-ward and single family room units. J. Perinatol. 2011, 31, 281–288. [Google Scholar] [CrossRef] [PubMed]
- Lester, B.M.; Hawes, K.; Abar, B.; Sullivan, M.; Miller, R.; Bigsby, R.; Laptook, A.; Salisbury, A.; Taub, M.; Lagasse, L.L.; et al. Single-Family Room Care and Neurobehavioral and Medical Outcomes in Preterm Infants. Pediatrics 2014, 134, 754–760. [Google Scholar] [CrossRef] [PubMed]
- Monson, B.; Rock, J.; Cull, M.; Soloveychilk, V. Neonatal intensive care unit incubators reduce language and noise levels more than the womb. J. Perinatol. 2020, 40, 600–606. [Google Scholar] [CrossRef]
- Hernández-Molina, R.; Fernádez Zacarías, F.; Puyana-Romero, V.; Rodríguez-Montaño, V.M.; Beira-Jiménez, J.L.; Cueto-Ancela, J.L.; Lubián López, S. Análisis del ambiente sonoro en una unidad de cuidados intensivos de neonatología. In Proceedings of the FIA 2018 XI Congreso Iberoamericano de Acústica-Tecniacústica: 49º Congreso Español de Acústica y X Congreso Ibérico de Acústica, Cadiz, Spain, 24–26 October 2018. [Google Scholar]
- Konkani, A.; Oakley, B. Noise in hospital intensive care units—A critical review of a critical topic. J. Crit. Care 2012, 27, 522.e1–522.e9. [Google Scholar] [CrossRef]
- Fortes-Garrido, J.C.; Velez-Pereira, A.M.; Gázquez, M.; Hidalgo-Hidalgo, M.; Bolívar, J.P. The characterization of noise levels in a neonatal intensive care unit and the implications for noise management. J. Environ. Health Sci. Eng. 2014, 12, 104. [Google Scholar] [CrossRef]
- Neille, J.; George, K.; Khoza-Shangase, K. A study investigating sound sources and noise levels in neonatal intensive care units. S. Afr. J. Child. Health 2014, 8, 6–10. [Google Scholar] [CrossRef]
- Parra, J.; de Suremain, A.; Berne Audeoud, F.; Ego, A.; Debillon, T. Sound levels in a neonatal intensive care unit significantly exceeded recommendations, especially inside incubators. Acta Paediatr. 2017, 106, 1909–1914. [Google Scholar] [CrossRef]
- Li, T.; Matsushima, M.; Timpson, W.; Young, S.; Miedema, D.; Gupta, M.; Heldt, T. Epidemiology of patient monitoring alarms in the neonatal intensive care unit. J. Perinatol. 2018, 38, 1030–1038. [Google Scholar] [CrossRef]
- Santos, J.; Carvalhais, C.; Xavier, A.; Silva, M. Assessment and characterization of sound pressure levels in portuguese Neonatal Intensive Care Units. Arch. Environ. Occup. Health 2017, 73, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Gray, L.; Philbin, M.K. Measuring Sound in Hospital Nurseries. J. Perinatol. 2001, 20, S100–S104. [Google Scholar] [CrossRef]
- Rodríguez-Montaño, V.; Beira-Jiménez, J.L.; Fernández-Zacarías, F.; Cueto-Ancela, J.L.; Puyana-Romero, V.; Hernández-Molina, R. The frequency spectrum of the acoustic environment in a Neonatal Intensive Care Unit. J. King Saud Univ.-Sci. 2023, 35, 102621. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Guidelines for Perinatal Care, 8th ed.; American Academy of Pediatrics: Itasca, IL, USA, 2017. [Google Scholar]
- Quiroga, A.; Chattas, G.; Castañeda, A.G.; Julcarima, M.R.; Bueno, T.M.; Diz, A.I.; Ordaz, J.P.; López, I.; Carrera, B. Guía de Práctica Clínica de Termorregulación en el Recién Nacido; Sociedad Iberoamericana de Neonatologia: Buenos Aires, Argentina, 2010. [Google Scholar]
- Restin, T.; Gaspar, M.; Bassler, D.; Kurtcuoglu, V.; Scholkmann, F.; Haslbeck, F.B. Newborn incubators do not protect from high noise levels in the Neonatal Intensive Care Unit and are relevant noise sources by themselves. Children 2021, 8, 704. [Google Scholar] [CrossRef]
- Fernández Zacarías, F.; Beira Jiménez, J.L.; Bustillo Velázquez-Gaztelu, P.J.; Hernández Molina, R.; Lubián López, S. Noise level in neonatal incubators: A comparative study of three models. Int. J. Pediatr. Otorhinolaryngol. 2018, 107, 150–154. [Google Scholar] [CrossRef]
- Valdés-de la Torre, G.E.; Martina Luna, M.; Braverman Bronstein, A.; Iglesias Leboreiro, J.; Bernárdez Zapata, I. Comparative measurement of noise intensity inside and outside closed incubators. Perinatol. Reprod. Humana 2018, 32, 65–69. [Google Scholar] [CrossRef]
- Rodríguez-Montaño, V.; Beira-Jiménez, J.L.; Puyana-Romero, V.; Cueto-Ancela, J.L.; Hernández-Molina, R.; Fernández-Zacarías, F. Acoustic conditioning of the neonatal incubator compartment: Improvement proposal. Front. Pediatr. 2022, 10, 955553. [Google Scholar] [CrossRef] [PubMed]
- Hernández-Molina, R.; Puyana-Romero, V.; Beira-Jiménez, J.L.; Morgado-Estévez, A.; Bienvenido-Bárcena, R.; Fernández-Zacarías, F. Silent Neonatal Incubators, Prototype NICA+. Acoustics 2024, 6, 638–650. [Google Scholar] [CrossRef]
- Webb, A.R.; Heller, H.T.; Benson, C.B.; Lahav, A. Mother’s voice and heartbeat sounds elicit auditory plasticity in the human brain before full gestation. Proc. Natl. Acad. Sci. USA 2015, 112, 3152–3157. [Google Scholar] [CrossRef]
- Caskey, M.; Stephens, B.; Tucker, R.; Vohr, B. Importance of Parent Talk on the Development of Preterm Infant Vocalizations. Pediatrics 2011, 128, 910–916. [Google Scholar] [CrossRef]
- Balsan, M.J.; Burns, J.; Kimock, F.; Hirsch, E.; Unger, A.; Telesco, R.; Bloch-Salisbury, E. A pilot study to assess the safety, efficacy and ease of use of a novel hearing protection device for hospitalized neonates. Early Hum. Dev. 2021, 156, 105365. [Google Scholar] [CrossRef] [PubMed]
- Abujarir, R.; Salama, H.; Greer, W.; Al Thani, M.; Visda, F. The impact of earmuffs on vital signs in the neonatal intensive care unit. J. Neonatal Perinat. Med. 2012, 5, 249–259. [Google Scholar] [CrossRef]
- Milette, I. Decreasing Noise Level in Our NICU: The Impact of a Noise Awareness Educational Program. Adv. Neonatal Care 2010, 10, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Liu, W. The impact of a noise reduction quality improvement project upon sound levels in the open-unit-design neonatal intensive care unit. J. Perinatol. 2010, 30, 489–496. [Google Scholar] [CrossRef]
- Chow, V.Y.; Shellhaas, R.A. Acoustic environment profile of the neonatal intensive care unit: High ambient noise and limited language exposure. J. Neonatal Nurs. 2016, 22, 159–162. [Google Scholar] [CrossRef]
- Ley 37/2003, de 17 de noviembre, del Ruido. Boletín Of. del Estado, num. 276, 2003. Available online: https://www.boe.es/eli/es/l/2003/11/17/37/con (accessed on 15 May 2024).
- Real Decreto 1367/2007, de 19 de octubre, por el que se desarrolla la Ley 37/2003, de 17 de noviembre, del Ruido, en lo referente a zonificación acústica, objetivos de calidad y emisiones acústicas. Boletín Of. del Estado, num. 254, 2007. Available online: https://www.boe.es/eli/es/rd/2007/10/19/1367/con (accessed on 15 May 2024).
- Código Técnico de la Edificación (CTE) Documento Básico de Protección frente al Ruido (DB-HR). Ministerio de Transportes, Movilidad y Agenda Urbana, 2019. Available online: https://www.codigotecnico.org/DocumentosCTE/ProteccionRuido.html (accessed on 15 May 2024).
- Ley 14/2007, de 3 de julio, de Investigación biomédica. Boletín Of. del Estado, num. 159, 2007, 28826–28848. Available online: https://www.boe.es/eli/es/l/2007/07/03/14 (accessed on 15 May 2024).
- UNE-ISO 1996-2:2020; Acoustics. Description, Measurement and Assessment of Environmental Noise. Part 2: Determination of Sound Pressure Levels. ISO: Geneva, Switzerland, 2020.
- EN-IEC 61672:2013; Electroacoustics. Sound Level Meters. International Electrotechnical Commission: Geneva, Switzerland, 2013.
- Fumero Rodríguez, M. Estudio de Afección Acústica a Neonatos en la UCI Pediátrica del Hospital General Juan Ramón Jiménez de Huelva. Master’s Thesis, Universidad de Cádiz, Cadiz, Spain, 2010. [Google Scholar]
- Sullivan, G.; Feinn, R. Using Effect Size—Or why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef]
- Coe, R. It’s the effect size, stupid: What effect size is and why it is important. In Proceedings of the Conference of the British Educational Research Association, Exeter, UK, 14 September 2002. [Google Scholar]
- Rosenthal, R. Parametric measures of effect size. In The Handbook of Research Synthesis; Russell Sage Foundation: New York, NY, USA, 1994; pp. 231–244. [Google Scholar]
- Bartz, A.E. Basic Statistical Concepts, 4th ed.; Merrill: Upper Saddle River, NJ, USA, 1999. [Google Scholar]
- Mangini, C.; Zarantonello, L.; Formentin, C.; Giusti, G.; Domenie, E.D.; Ruggerini, D.; Costa, R.; Skene, D.J.; Basso, D.; Battagliarin, L.; et al. Managing circadian disruption due to hospitalization: A pilot randomized controlled trial of the circadian care inpatient management system. J. Biol. Rhythm. 2024, 39, 183–199. [Google Scholar] [CrossRef]
- Bergmans, D.H.T.; Veerbeek, H.W.; Jabben, J.; Schreurs, E. A Method to Calculate Ambient Aircraft Background Noise. In Proceedings of the 8th European Conference on Noise Control 2009: EURONOISE 2009, Edinburgh, UK, 26–28 October 2009. [Google Scholar]
- Moreira Pinheiro, E.; Guinsburg, R.; de Araujo Nabuco, M.A.; Kakehashi, T.Y. Ruido en la Unidad de Terapia Intensiva Neonatal y en el interior de la incubadora. Rev. Lat.-Am. Enferm. 2011, 19, 1214–1221. [Google Scholar]
- Recuero, M. Contaminación Acústica; Universidad Politécnica de Madrid: Madrid, Spain, 2002. [Google Scholar]
- Egan, M.D. Architectural Acoustics; McGraw-Hill: New York, NY, USA, 1998. [Google Scholar]
- Carrión, A. Diseño Acústico de Espacios Arquitectónicos; Edicions UPC: Barcelona, Spain, 1998. [Google Scholar]
- Puyana-Romero, V.; Núñez-Solano, D.; Hernández-Molina, R.; Fernández-Zacarías, F.; Beira-Jiménez, J.L.; Garzón, C.; Jara-Muñoz, E. Reverberation time measurements of a neonatal incubator. Appl. Acoust. 2020, 167, 107374. [Google Scholar] [CrossRef]
- Puyana-Romero, V.; Núñez-Solano, D.; Fernández-Zacarías, F.; Jara-Muñoz, E.; Hernández-Molina, R. The importance of reverberation for the design of neonatal incubators. Front. Pediatr. 2021, 9, 584736. [Google Scholar] [CrossRef]
- Sabine, W.C. Collected Papers on Acoustics; Harvard University Press: Cambridge, UK, 1922. [Google Scholar]
- Negreira, J. Reducción de niveles de ruido en unidades de neonates. Integración 2020, 96, 10–13. Available online: https://integration.ecophon.com/globalassets/media/pdf-and-documents/es/integracion96_acustica_neonatos.pdf/ (accessed on 15 May 2024).
- Da Silva, L.; Soares, L.; Rocha, R.; Edson, J. Measurement of acoustic noise levels in a neonatal intensive care unit. REME 2015, 19, 27–31. [Google Scholar] [CrossRef]
- Kuhn, P.; Zores, C.; Langlet, C.; Escande, B.; Astruc, D.; Dufour, A. Moderate acoustic chances can disrupt the sleep of very preterm infants in their incubators. Acta Paediatr. 2013, 102, 949–954. [Google Scholar] [CrossRef] [PubMed]
- Joshi, G.; Tada, N. Analysis of noise level in neonatal intensive care unit and post natal ward of a tertiary care hospital in an urban city. Int. J. Contemp. Pediatr. 2016, 3, 1358–1361. [Google Scholar] [CrossRef]

| Day Period (without Feeding and Staff Shift Changes), Huelva and Cadiz | ||||||
|---|---|---|---|---|---|---|
| Metrics | Mean Rank | Z | p-Value | r, Absolute Value | Effect Size | |
| HJRJ | HUPM | |||||
| LAeq [dBA] | 43.16 | 65.24 | −3.69 | 0.00 | 0.36 | Low |
| LAIeq [dBA] | 46.38 | 60.84 | −2.41 | 0.02 | 0.24 | Low |
| LAFmáx [dBA] | 55.80 | 48.00 | −1.30 | 0.19 | 0.13 | |
| LAFmín [dBA] | 30.50 | 82.50 | −8.69 | 0.00 | 0.85 | Very Strong |
| LCeq [dBC] | 72.23 | 23.37 | −8.11 | 0.00 | 0.80 | Very Strong |
| LA10 [dBA] | 44.75 | 63.07 | −3.06 | 0.00 | 0.30 | Low |
| LA50 [dBA] | 37.45 | 73.02 | −5.94 | 0.00 | 0.58 | Moderate |
| LA90 [dBA] | 32.49 | 79.78 | −7.90 | 0.00 | 0.77 | Very Strong |
| LZeq 40 Hz [dB] | 74.50 | 22.50 | −8.69 | 0.00 | 0.85 | Very Strong |
| LZeq 50 Hz [dB] | 74.50 | 22.50 | −8.71 | 0.00 | 0.85 | Very Strong |
| LZeq 63 Hz [dB] | 74.50 | 22.50 | −8.69 | 0.00 | 0.85 | Very Strong |
| LZeq 80 Hz [dB] | 73.88 | 23.35 | −8.44 | 0.00 | 0.83 | Very Strong |
| LZeq 100 Hz [dB] | 72.79 | 24.83 | −8.01 | 0.00 | 0.79 | Very Strong |
| LZeq 125 Hz [dB] | 55.46 | 48.47 | −1.17 | 0.24 | 0.11 | |
| LZeq 160 Hz [dB] | 48.80 | 57.55 | −1.46 | 0.14 | 0.14 | |
| LZeq 200 Hz [dB] | 49.71 | 56.31 | −1.10 | 0.27 | 0.11 | |
| LZeq 250 Hz [dB] | 41.79 | 67.10 | −4.23 | 0.00 | 0.41 | Moderate |
| LZeq 315 Hz [dB] | 40.02 | 69.52 | −4.93 | 0.00 | 0.48 | Moderate |
| LZeq 400 Hz [dB] | 45.29 | 62.33 | −2.85 | 0.00 | 0.28 | Low |
| LZeq 500 Hz [dB] | 46.60 | 60.55 | −2.33 | 0.02 | 0.23 | Low |
| LZeq 630 Hz [dB] | 45.25 | 62.39 | −2.86 | 0.00 | 0.28 | Low |
| LZeq 800 Hz [dB] | 39.48 | 70.25 | −5.14 | 0.00 | 0.50 | Moderate |
| LZeq 1 kHz [dB] | 43.16 | 65.24 | −3.69 | 0.00 | 0.36 | Low |
| LZeq 1.25 kHz [dB] | 39.62 | 70.07 | −5.09 | 0.00 | 0.50 | Moderate |
| LZeq 1.6 kHz [dB] | 41.49 | 67.51 | −4.35 | 0.00 | 0.43 | Moderate |
| LZeq 2 kHz [dB] | 47.16 | 59.78 | −2.11 | 0.03 | 0.21 | Low |
| LZeq 2.5 kHz [dB] | 48.44 | 58.03 | −1.60 | 0.11 | 0.16 | |
| LZeq 3.15 kHz [dB] | 51.93 | 53.27 | −0.22 | 0.82 | 0.02 | |
| LZeq 4 kHz [dB] | 45.59 | 61.92 | −2.73 | 0.01 | 0.27 | Low |
| LZeq 5 kHz [dB] | 51.13 | 54.36 | −0.54 | 0.59 | 0.05 | |
| LZeq 6.3 kHz [dB] | 52.42 | 52.61 | −0.03 | 0.97 | 0.00 | |
| LZeq 8 kHz [dB] | 51.75 | 53.52 | −0.30 | 0.77 | 0.03 | |
| LZeq 10 kHz [dB] | 51.33 | 54.10 | −0.46 | 0.64 | 0.05 | |
| LZeq 12.5 kHz [dB] | 51.14 | 54.35 | −0.54 | 0.59 | 0.05 | |
| LZeq 16 kHz [dB] | 50.21 | 55.63 | −0.90 | 0.37 | 0.09 | |
| LZeq 20 kHz [dB] | 48.19 | 58.38 | −1.70 | 0.09 | 0.17 | |
| Night Period (without Feeding and Staff Shift Changes), Huelva and Cadiz | ||||||
|---|---|---|---|---|---|---|
| Metrics | Mean Rank | Z | p-Value | r, Absolute Value | Effect Size | |
| HJRJ | HUPM | |||||
| LAeq [dBA] | 33.92 | 50.38 | −3.10 | 0.00 | 0.35 | Low |
| LAFmín [dBA] | 24.50 | 64.50 | −7.55 | 0.00 | 0.84 | Very Strong |
| LCeq [dBC] | 56.50 | 16.50 | −7.56 | 0.00 | 0.84 | Very Strong |
| LA50 [dBA] | 32.34 | 52.73 | −3.85 | 0.00 | 0.43 | Moderate |
| LA90 [dBA] | 25.25 | 63.38 | −7.19 | 0.00 | 0.80 | Very Strong |
| LZeq 40 Hz [dB] | 56.50 | 16.50 | −7.56 | 0.00 | 0.84 | Very Strong |
| LZeq 50 Hz [dB] | 56.50 | 16.50 | −7.58 | 0.00 | 0.85 | Very Strong |
| LZeq 63 Hz [dB] | 55.19 | 18.47 | −7.56 | 0.00 | 0.84 | Very Strong |
| LZeq 80 Hz [dB] | 52.36 | 22.70 | −6.93 | 0.00 | 0.77 | Strong |
| LZeq 100 Hz [dB] | 46.22 | 31.92 | −5.59 | 0.00 | 0.63 | Very Strong |
| LZeq 125 Hz [dB] | 46.22 | 31.92 | −2.70 | 0.01 | 0.30 | Low |
| LZeq 250 Hz [dB] | 34.81 | 49.03 | −2.68 | 0.01 | 0.30 | Low |
| LZeq 315 Hz [dB] | 35.74 | 47.64 | −2.24 | 0.02 | 0.25 | Low |
| LZeq 800 Hz [dB] | 29.30 | 57.30 | −5.28 | 0.00 | 0.59 | Moderate |
| LZeq 1 kHz [dB] | 36.21 | 46.94 | −2.02 | 0.04 | 0.23 | Low |
| LZeq 1.25 kHz [dB] | 31.74 | 53.64 | −4.13 | 0.00 | 0.46 | Moderate |
| LZeq 1.6 kHz [dB] | 33.20 | 51.45 | −3.44 | 0.00 | 0.38 | Low |
| Feeding, Day Period, Huelva and Cadiz | ||||||
|---|---|---|---|---|---|---|
| Metric | Mean Rank | Z | p-Value | r, Absolute Value | Effect Size | |
| HJRJ | HUPM | |||||
| LAFmín [dBA] | 6.50 | 16.00 | −3.56 | 0.00 | 0.82 | Very Strong |
| LCeq [dBC] | 14.33 | 4.75 | −3.18 | 0.00 | 0.73 | Strong |
| LA90 [dBA] | 7.08 | 15.00 | −2.96 | 0.00 | 0.68 | Very Strong |
| LZeq 40 Hz [dB] | 13.50 | 4.00 | −3.56 | 0.00 | 0.82 | Very Strong |
| LZeq 50 Hz [dB] | 13.50 | 4.00 | −3.57 | 0.00 | 0.82 | Very Strong |
| LZeq 63 Hz [dB] | 13.50 | 4.00 | −3.57 | 0.00 | 0.82 | Very Strong |
| LZeq 80 Hz [dB] | 13.17 | 4.57 | −3.21 | 0.00 | 0.74 | Strong |
| LZeq 100 Hz [dB] | 13.50 | 4.00 | −3.55 | 0.00 | 0.82 | Very Strong |
| LZeq 800 Hz [dB] | 7.96 | 13.50 | −2.07 | 0.04 | 0.48 | Moderate |
| Feeding, Night Period, Huelva and Cadiz | ||||||
|---|---|---|---|---|---|---|
| Metric | Mean Rank | Z | p-Value | r, Absolute Value | Effect Size | |
| HJRJ | HUPM | |||||
| LAFmín [dBA] | 5.00 | 12.50 | −3.18 | 0.00 | 0.82 | Very Strong |
| LCeq [dBC] | 11.00 | 3.50 | −3.18 | 0.00 | 0.82 | Very Strong |
| LA90 [dBA] | 5.89 | 11.17 | −2.25 | 0.02 | 0.58 | Moderate |
| LZeq 40 Hz [dB] | 11.00 | 3.50 | −3.19 | 0.00 | 0.82 | Very Strong |
| LZeq 50 Hz [dB] | 11.00 | 3.50 | −3.21 | 0.00 | 0.83 | Very Strong |
| LZeq 63 Hz [dB] | 11.00 | 3.50 | −3.20 | 0.00 | 0.83 | Very Strong |
| LZeq 80 Hz [dB] | 11.00 | 3.50 | −3.19 | 0.00 | 0.82 | Very Strong |
| LZeq 100 Hz [dB] | 11.00 | 3.50 | −3.19 | 0.00 | 0.82 | Very Strong |
| LZeq 125 Hz [dB] | 10.83 | 3.75 | −3.02 | 0.00 | 0.78 | Strong |
| Staff Shift Changes, Day Period, Huelva and Cadiz | ||||||
|---|---|---|---|---|---|---|
| Metric | Mean Rank | Z | p-Value | r, Absolute Value | Effect Size | |
| HJRJ | HUPM | |||||
| LAFmín [dB] | 5.00 | 12.00 | −3.01 | 0.00 | 0.80 | Very Strong |
| LCeq [dB] | 10.00 | 3.00 | −3.50 | 0.00 | 0.93 | Very Strong |
| LA90 [dB] | 5.67 | 10.80 | −2.20 | 0.03 | 0.59 | Moderate |
| LZeq 40 Hz [dB] | 10.00 | 3.00 | −3.01 | 0.00 | 0.80 | Very Strong |
| LZeq 50 Hz [dB] | 10.00 | 3.00 | −3.01 | 0.00 | 0.80 | Very Strong |
| LZeq 63 Hz [dB] | 10.00 | 3.00 | −3.02 | 0.00 | 0.81 | Very Strong |
| LZeq 80 Hz [dB] | 10.00 | 3.00 | −3.00 | 0.00 | 0.80 | Very Strong |
| LZeq 100 Hz [dB] | 9.56 | 3.80 | −2.47 | 0.01 | 0.66 | Strong |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Montaño, V.M.; Puyana-Romero, V.; Hernández-Molina, R.; Beira-Jiménez, J.L. The Noise: A Silent Threat to the Recovery of Patients in Neonatal Intensive Care Units. Buildings 2024, 14, 2778. https://doi.org/10.3390/buildings14092778
Rodríguez-Montaño VM, Puyana-Romero V, Hernández-Molina R, Beira-Jiménez JL. The Noise: A Silent Threat to the Recovery of Patients in Neonatal Intensive Care Units. Buildings. 2024; 14(9):2778. https://doi.org/10.3390/buildings14092778
Chicago/Turabian StyleRodríguez-Montaño, Víctor M., Virginia Puyana-Romero, Ricardo Hernández-Molina, and Juan L. Beira-Jiménez. 2024. "The Noise: A Silent Threat to the Recovery of Patients in Neonatal Intensive Care Units" Buildings 14, no. 9: 2778. https://doi.org/10.3390/buildings14092778
APA StyleRodríguez-Montaño, V. M., Puyana-Romero, V., Hernández-Molina, R., & Beira-Jiménez, J. L. (2024). The Noise: A Silent Threat to the Recovery of Patients in Neonatal Intensive Care Units. Buildings, 14(9), 2778. https://doi.org/10.3390/buildings14092778








