Investigation of Delafloxacin Resistance in Multidrug-Resistant Escherichia coli Strains and the Detection of E. coli ST43 International High-Risk Clone
Abstract
1. Introduction
2. Materials and Methods
2.1. Strains
2.2. Determination of the Minimum Inhibitory Concentration (MIC)
2.3. Whole-Genome Sequencing (WGS)
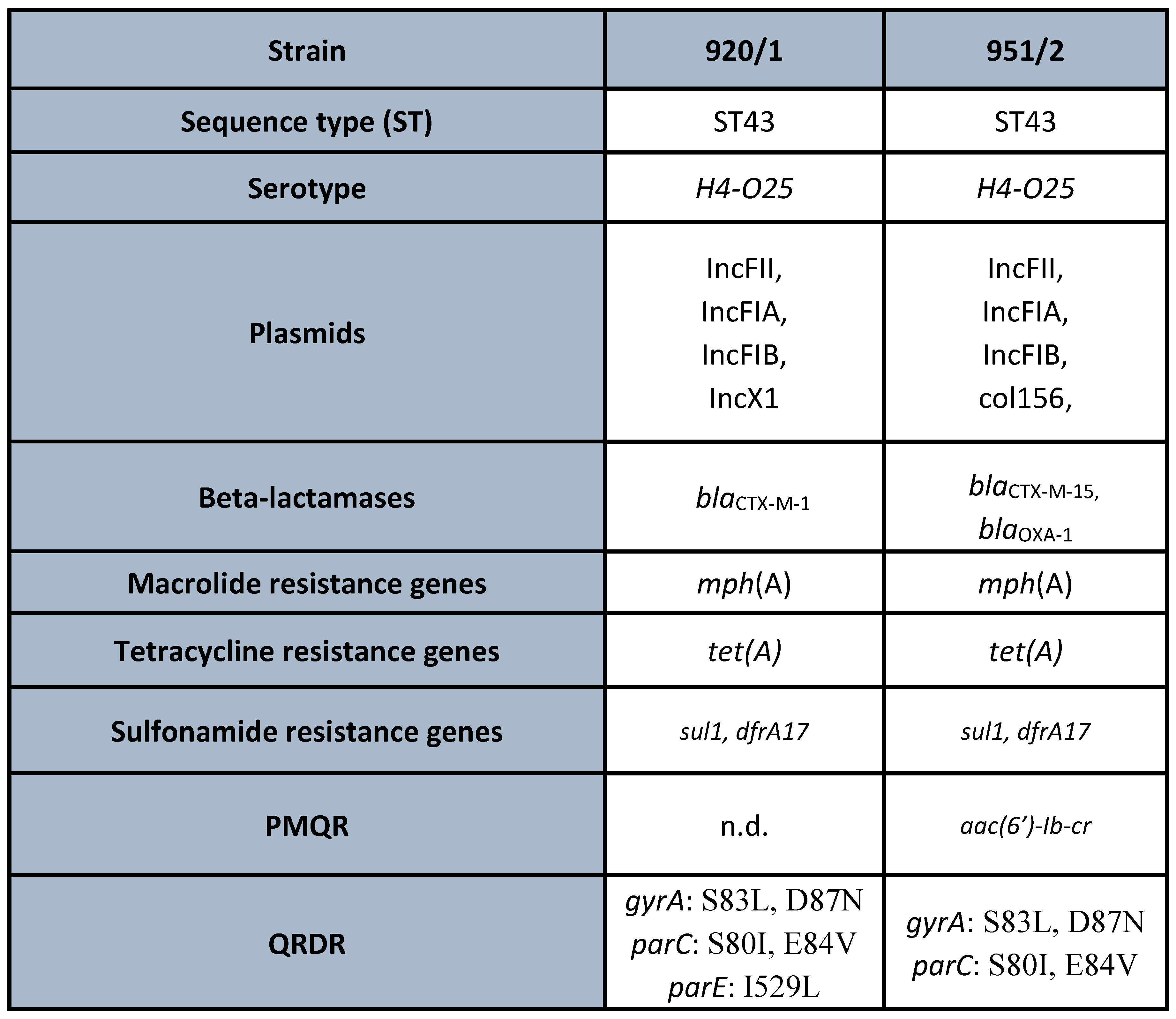
3. Results
4. Discussion
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethics Approval
References
- Mendelson, M.; Sharland, M.; Mpundu, M. Antibiotic resistance: Calling time on the ‘silent pandemic’. JAC Antimicrob. Resist. 2022, 4, dlac016. [Google Scholar] [CrossRef] [PubMed]
- Rehman, S. A parallel and silent emerging pandemic: Antimicrobial resistance (AMR) amid COVID-19 pandemic. J. Infect. Public. Health 2023, 16, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Livermore, D.M. Antibiotic resistance during and beyond COVID-19. JAC Antimicrob. Resist. 2021, 3 (Suppl. S1), i5–i16. [Google Scholar] [CrossRef] [PubMed]
- Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: A systematic analysis. Lancet 2022, 399, 629–655. [Google Scholar] [CrossRef]
- Thompson, T. The staggering death toll of drug-resistant bacteria. Nature, 2022; epub ahead of print. [Google Scholar] [CrossRef]
- O’Neill, J. Review on Antimicrobial Resistance. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations; Wellcome Trust: London, UK, 2014; p. 20. Available online: https://amr-review.org/Publications.html (accessed on 10 February 2020).
- Zhen, X.; Lundborg, C.S.; Sun, X.; Hu, X.; Dong, H. Economic burden of antibiotic resistance in ESKAPE organisms: A systematic review. Antimicrob. Resist. Infect. Control 2019, 8, 137. [Google Scholar] [CrossRef]
- Orosz, L.; Lengyel, G.; Ánosi, N.; Lakatos, L.; Burián, K. Changes in resistance pattern of ESKAPE pathogens between 2010 and 2020 in the clinical center of University of Szeged, Hungary. Acta Microbiol. Immunol. Hung. 2022, 69, 27–34. [Google Scholar] [CrossRef]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; Harbarth, S.; Mendelson, M.; Monnet, D.L.; Pulcini, C.; Kahlmeter, G.; Kluytmans, J.; Carmeli, Y.; et al. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef]
- Butler, M.S.; Paterson, D.L. Antibiotics in the clinical pipeline in October 2019. J. Antibiot. 2020, 73, 329–364. [Google Scholar] [CrossRef]
- Syed, Y.Y. Cefiderocol: A Review in Serious Gram-Negative Bacterial Infections. Drugs 2021, 81, 1559–1571. [Google Scholar] [CrossRef]
- Saravolatz, L.D.; Stein, G.E. Plazomicin: A new aminoglycoside. Clin. Infect. Dis. 2020, 70, 704–709. [Google Scholar] [CrossRef]
- Bush, K.; Bradford, P.A. Interplay between beta-lactamases and new beta-lactamase inhibitors. Nat. Rev. Microbiol. 2019, 17, 295–306. [Google Scholar] [CrossRef]
- Kocsis, B.; Gulyás, D.; Szabó, D. Delafloxacin, Finafloxacin, and Zabofloxacin: Novel Fluoroquinolones in the Antibiotic Pipeline. Antibiotics 2021, 10, 1506. [Google Scholar] [CrossRef]
- Dong Wha Pharm’s Quinolone Antibacterial Agent, “Zabolante”, Wins at the 19th KNDA (Press Release 28 February 2018). Available online: https://www.dong-wha.co.kr/english/customer/dnews/content.asp?t_idx=1139 (accessed on 20 August 2021).
- U.S. Food and Drug Administration. BAXDELA (Delafloxacin) Prescribing Information and Medication Guide. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/208610s000,208611s000lbl.pdf (accessed on 8 December 2018).
- U.S. Food and Drug Administration. XTORO Prescribing Information and Medication Guide 2014. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2014/206307s000lbl.pdf (accessed on 20 August 2021).
- Kocsis, B.; Domokos, J.; Szabo, D. Chemical structure and pharmacokinetics of novel quinolone agents represented by avarofloxacin, delafloxacin, finafloxacin, zabofloxacin and nemonoxacin. Ann. Clin. Microbiol. Antimicrob. 2016, 15, 34. [Google Scholar] [CrossRef]
- Rusu, A.; Lungu, I.A.; Moldovan, O.L.; Tanase, C.; Hancu, G. Structural Characterization of the Millennial Antibacterial (Fluoro)Quinolones-Shaping the Fifth Generation. Pharmaceutics 2021, 13, 1289. [Google Scholar] [CrossRef]
- Lungu, I.A.; Moldovan, O.L.; Biriș, V.; Rusu, A. Fluoroquinolones Hybrid Molecules as Promising Antibacterial Agents in the Fight against Antibacterial Resistance. Pharmaceutics 2022, 14, 1749. [Google Scholar] [CrossRef]
- Rusu, A.; Munteanu, A.C.; Arbănași, E.M.; Uivarosi, V. Overview of Side-Effects of Antibacterial Fluoroquinolones: New Drugs versus Old Drugs, a Step Forward in the Safety Profile? Pharmaceutics 2023, 15, 804. [Google Scholar] [CrossRef]
- European Medicines Agency (EMA). Quinolone- and Fluoroquinolone-Containing Medicinal Products: Disabling and Potentially Permanent Side Effects Lead to Suspension or Restrictions of Quinolone and Fluoroquinolone Antibiotics. Available online: https://www.ema.europa.eu/en/medicines/human/referrals/quinolone-fluoroquinolone-containing-medicinal-products (accessed on 8 December 2018).
- Mogle, B.T.; Steele, J.M.; Thomas, S.J.; Bohan, K.B.H.; Kufel, W.D. Clinical review of delafloxacin: A novel anionic fluoroquinolone. J. Antimicrob. Chemother. 2018, 73, 1439–1451. [Google Scholar] [CrossRef]
- Sharma, R.; Sandrock, C.E.; Meehan, J.; Theriault, N. Community-Acquired Bacterial Pneumonia-Changing Epidemiology, Resistance Patterns, and Newer Antibiotics: Spotlight on Delafloxacin. Clin. Drug Investig. 2020, 40, 947–960. [Google Scholar] [CrossRef]
- European Medicines Agency. Quofenix (Delafloxacin): Summary of Product Characteristics. 2019. Available online: https://www.ema.europa.eu/ (accessed on 16 March 2020).
- Scott, L.J. Delafloxacin: A review in acute bacterial skin and skin structure infections. Drugs 2020, 80, 1247–1258. [Google Scholar] [CrossRef]
- Melinta Therapeutics. Baxdela (Delafloxacin) Tablets, for Oral Use; Baxdela (Delafloxacin) for Injection, for Intravenous Use: U.S. Prescribing Information. 2019. Available online: https://baxdela.com/docs/baxdela-prescribing-information.pdf (accessed on 16 March 2020).
- Hooper, D.C.; Jacoby, G.A. Mechanisms of drug resistance: Quinolone resistance. Ann. N. Y. Acad. Sci. 2015, 1354, 12–31. [Google Scholar] [CrossRef] [PubMed]
- Vila, J.; Ruiz, J.; Marco, F.; Barcelo, A.; Goñi, P.; Giralt, E.; Jimenez de Anta, T. Association between double mutation in gyrA gene of ciprofloxacin-resistant clinical isolates of Escherichia coli and MICs. Antimicrob. Agents Chemother. 1994, 38, 2477–2479. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Martínez, J.M.; Machuca, J.; Cano, M.E.; Calvo, J.; Martínez-Martínez, L.; Pascual, A. Plasmid-mediated quinolone resistance: Two decades on. Drug Resist. Update 2016, 29, 13–29. [Google Scholar] [CrossRef] [PubMed]
- Kocsis, B.; Szmolka, A.; Szabo, O.; Gulyas, D.; Kristóf, K.; Göcző, I.; Szabo, D. Ciprofloxacin Promoted qnrD Expression and Phylogenetic Analysis of qnrD Harboring Plasmids. Microb. Drug Resist. 2019, 25, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Albornoz, E.; Tijet, N.; De Belder, D.; Gomez, S.; Martino, F.; Corso, A.; Melano, R.G.; Petroni, A. qnrE1, a Member of a New Family of Plasmid-Located Quinolone Resistance Genes, Originated from the Chromosome of Enterobacter Species. Antimicrob. Agents Chemother. 2017, 61, e02555-16. [Google Scholar] [CrossRef]
- Wang, C.; Yin, M.; Zhang, X.; Guo, Q.; Wang, M. Identification of qnrE3 and qnrE4, New Transferable Quinolone Resistance qnrE Family Genes Originating from Enterobacter mori and Enterobacter asburiae, Respectively. Antimicrob. Agents Chemother. 2021, 65, e0045621. [Google Scholar] [CrossRef]
- Núñez-Samudio, V.; Pecchio, M.; Pimentel-Peralta, G.; Quintero, Y.; Herrera, M.; Landires, I. Molecular Epidemiology of Escherichia coli Clinical Isolates from Central Panama. Antibiotics 2021, 10, 899. [Google Scholar] [CrossRef]
- Clermont, O.; Gordon, D.; Denamur, E. Guide to the various phylogenetic classification schemes for Escherichia coli and the correspondence among schemes. Microbiology 2015, 161, 980–988. [Google Scholar] [CrossRef]
- Johnson, J.R.; Clermont, O.; Johnston, B.; Clabots, C.; Tchesnokova, V.; Sokurenko, E.; Junka, A.F.; Maczynska, B.; Denamur, E. Rapid and specific detection, molecular epidemiology, and experimental virulence of the O16 subgroup within Escherichia coli sequence type 131. J. Clin. Microbiol. 2014, 52, 1358–1365. [Google Scholar] [CrossRef]
- Kocsis, B.; Gulyás, D.; Szabó, D. Emergence and Dissemination of Extraintestinal Pathogenic High-Risk International Clones of Escherichia coli. Life 2022, 12, 2077. [Google Scholar] [CrossRef]
- Pitout, J.D.D.; DeVinney, R. Escherichia coli ST131: A multidrug-resistant clone primed for global domination. F1000Res 2017, 6, 1–7. [Google Scholar] [CrossRef]
- Asgharzadeh, S.; Golmoradi Zadeh, R.; Taati Moghadam, M.; Farahani Eraghiye, H.; Sadeghi Kalani, B.; Masjedian Jazi, F.; Mirkalantari, S. Distribution and expression of virulence genes (hlyA, sat) and genotyping of Escherichia coli O25b/ST131 by multi-locus variable number tandem repeat analysis in Tehran, Iran. Acta Microbiol. Immunol. Hung. 2022, 69, 314–322. [Google Scholar] [CrossRef] [PubMed]
- Kocsis, E.; Lo Cascio, G.; Piccoli, M.; Cornaglia, G.; Mazzariol, A. KPC-3 carbapenemase harbored in FIIk plasmid from Klebsiella pneumoniae ST512 and Escherichia coli ST43 in the same patient. Microb. Drug Resist. 2014, 20, 377–382. [Google Scholar] [CrossRef] [PubMed]
- Suwantarat, N.; Rudin, S.D.; Marshall, S.H.; Hujer, A.M.; Perez, F.; Hujer, K.M.; Domitrovic, T.N.; Dumford, D.M., 3rd; Donskey, C.J.; Bonomo, R.A. Infections caused by fluoroquinolone-resistant Escherichia coli following transrectal ultrasound-guided biopsy of the prostate. J. Glob. Antimicrob. Resist. 2014, 2, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Pajand, O.; Rahimi, H.; Darabi, N.; Roudi, S.; Ghassemi, K.; Aarestrup, F.M.; Leekitcharoenphon, P. Arrangements of Mobile Genetic Elements among Virotype E Subpopulation of Escherichia coli Sequence Type 131 Strains with High Antimicrobial Resistance and Virulence Gene Content. mSphere 2021, 6, e0055021. [Google Scholar] [CrossRef]
- Massella, E.; Giacometti, F.; Bonilauri, P.; Reid, C.; Djordjevic, S.; Merialdi, G.; Bacci, C.; Fiorentini, L.; Massi, P.; Bardasi, L.; et al. Antimicrobial Resistance Profile and ExPEC Virulence Potential in Commensal Escherichia coli of Multiple Sources. Antibiotics 2021, 10, 351. [Google Scholar] [CrossRef]
- Tóth, K.; Tóth, Á.; Kamotsay, K.; Németh, V.; Szabó, D. Population snapshot of the extended-spectrum β-lactamase-producing Escherichia coli invasive strains isolated from a Hungarian hospital. Ann. Clin. Microbiol. Antimicrob. 2022, 21, 3. [Google Scholar] [CrossRef]
- Melegh, S.; Schneider, G.; Horváth, M.; Jakab, F.; Emődy, L.; Tigyi, Z. Identification and characterization of CTX-M-15 producing Klebsiella pneumoniae clone ST101 in a Hungarian university teaching hospital. Acta Microbiol. Immunol. Hung. 2015, 62, 233–245. [Google Scholar] [CrossRef]
- Kocsis, B.; Kocsis, E.; Fontana, R.; Cornaglia, G.; Mazzariol, A. Identification of blaLAP-2 and qnrS1 genes in the internationally successful Klebsiella pneumoniae ST147 clone. J. Med. Microbiol. 2013, 62, 269–273. [Google Scholar] [CrossRef]
- Domokos, J.; Damjanova, I.; Kristof, K.; Ligeti, B.; Kocsis, B.; Szabo, D. Multiple Benefits of Plasmid-Mediated Quinolone Resistance Determinants in Klebsiella pneumoniae ST11 High-Risk Clone and Recently Emerging ST307 Clone. Front. Microbiol. 2019, 10, 157. [Google Scholar] [CrossRef]
- Horváth, M.; Kovács, T.; Kun, J.; Gyenesei, A.; Damjanova, I.; Tigyi, Z.; Schneider, G. Virulence Characteristics and Molecular Typing of Carbapenem-Resistant ST15 Klebsiella pneumoniae Clinical Isolates, Possessing the K24 Capsular Type. Antibiotics 2023, 12, 479. [Google Scholar] [CrossRef]
- Muraya, A.; Kyany’a, C.; Kiyaga, S.; Smith, H.J.; Kibet, C.; Martin, M.J.; Kimani, J.; Musila, L. Antimicrobial Resistance and Virulence Characteristics of Klebsiella pneumoniae Isolates in Kenya by Whole-Genome Sequencing. Pathogens. 2022, 11, 545. [Google Scholar] [CrossRef]
- Navon-Venezia, S.; Kondratyeva, K.; Carattoli, A. Klebsiella pneumoniae: A major worldwide source and shuttle for antibiotic resistance. FEMS Microbiol. Rev. 2017, 41, 252–275. [Google Scholar] [CrossRef]
- Toth, A.; Kocsis, B.; Damjanova, I.; Kristof, K.; Janvari, L.; Paszti, J.; Csercsik, R.; Topf, J.; Szabo, D.; Hamar, P.; et al. Fitness cost associated with resistance to fluoroquinolones is diverse across clones of Klebsiella pneumoniae and may select for CTX-M-15 type extended-spectrum beta-lactamase. Eur. J. Clin. Microbiol. Infect. Dis. 2014, 33, 837–843. [Google Scholar] [CrossRef]
- Machuca, J.; Briales, A.; Labrador, G.; Díaz-de-Alba, P.; López-Rojas, R.; Docobo-Pérez, F.; Martínez-Martínez, L.; Rodríguez-Baño, J.; Pachón, M.E.; Pascual, A.; et al. Interplay between plasmid-mediated and chromosomal-mediated fluoroquinolone resistance and bacterial fitness in Escherichia coli. J. Antimicrob. Chemother. 2014, 69, 3203–3215. [Google Scholar] [CrossRef]
- Fuzi, M.; Szabo, D.; Csercsik, R. Double-Serine Fluoroquinolone Resistance Mutations Advance Major International Clones and Lineages of Various Multi-Drug Resistant Bacteria. Front. Microbiol. 2017, 8, 2261. [Google Scholar] [CrossRef]
- Soge, O.O.; Salipante, S.J.; No, D.; Duffy, E.; Roberts, M.C. In Vitro Activity of Delafloxacin against Clinical Neisseria gonorrhoeae Isolates and Selection of Gonococcal Delafloxacin Resistance. Antimicrob. Agents Chemother. 2016, 60, 3106–3111. [Google Scholar] [CrossRef]
- De la Rosa, J.M.O.; Fernández, M.A.; Rodríguez-Villodres, Á.; Casimiro-Soriguer, C.S.; Cisneros, J.M.; Lepe, J.A. High-level delafloxacin resistance through the combination of two different mechanisms in Staphylococcus aureus. Int. J. Antimicrob. Agents 2023, 61, 106795. [Google Scholar] [CrossRef]
- Brown Elliott, B.A.; Wallace, R.J., Jr. Comparison of In Vitro Susceptibility of Delafloxacin with Ciprofloxacin, Moxifloxacin, and Other Comparator Antimicrobials against Isolates of Nontuberculous Mycobacteria. Antimicrob. Agents Chemother. 2021, 65, e0007921. [Google Scholar] [CrossRef]




Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gulyás, D.; Kamotsay, K.; Szabó, D.; Kocsis, B. Investigation of Delafloxacin Resistance in Multidrug-Resistant Escherichia coli Strains and the Detection of E. coli ST43 International High-Risk Clone. Microorganisms 2023, 11, 1602. https://doi.org/10.3390/microorganisms11061602
Gulyás D, Kamotsay K, Szabó D, Kocsis B. Investigation of Delafloxacin Resistance in Multidrug-Resistant Escherichia coli Strains and the Detection of E. coli ST43 International High-Risk Clone. Microorganisms. 2023; 11(6):1602. https://doi.org/10.3390/microorganisms11061602
Chicago/Turabian StyleGulyás, Dániel, Katalin Kamotsay, Dóra Szabó, and Béla Kocsis. 2023. "Investigation of Delafloxacin Resistance in Multidrug-Resistant Escherichia coli Strains and the Detection of E. coli ST43 International High-Risk Clone" Microorganisms 11, no. 6: 1602. https://doi.org/10.3390/microorganisms11061602
APA StyleGulyás, D., Kamotsay, K., Szabó, D., & Kocsis, B. (2023). Investigation of Delafloxacin Resistance in Multidrug-Resistant Escherichia coli Strains and the Detection of E. coli ST43 International High-Risk Clone. Microorganisms, 11(6), 1602. https://doi.org/10.3390/microorganisms11061602







