Extended Reality Head-Mounted Displays Are Likely to Pose a Significant Risk in Medical Settings While Current Classification Remains as Non-Critical
Abstract
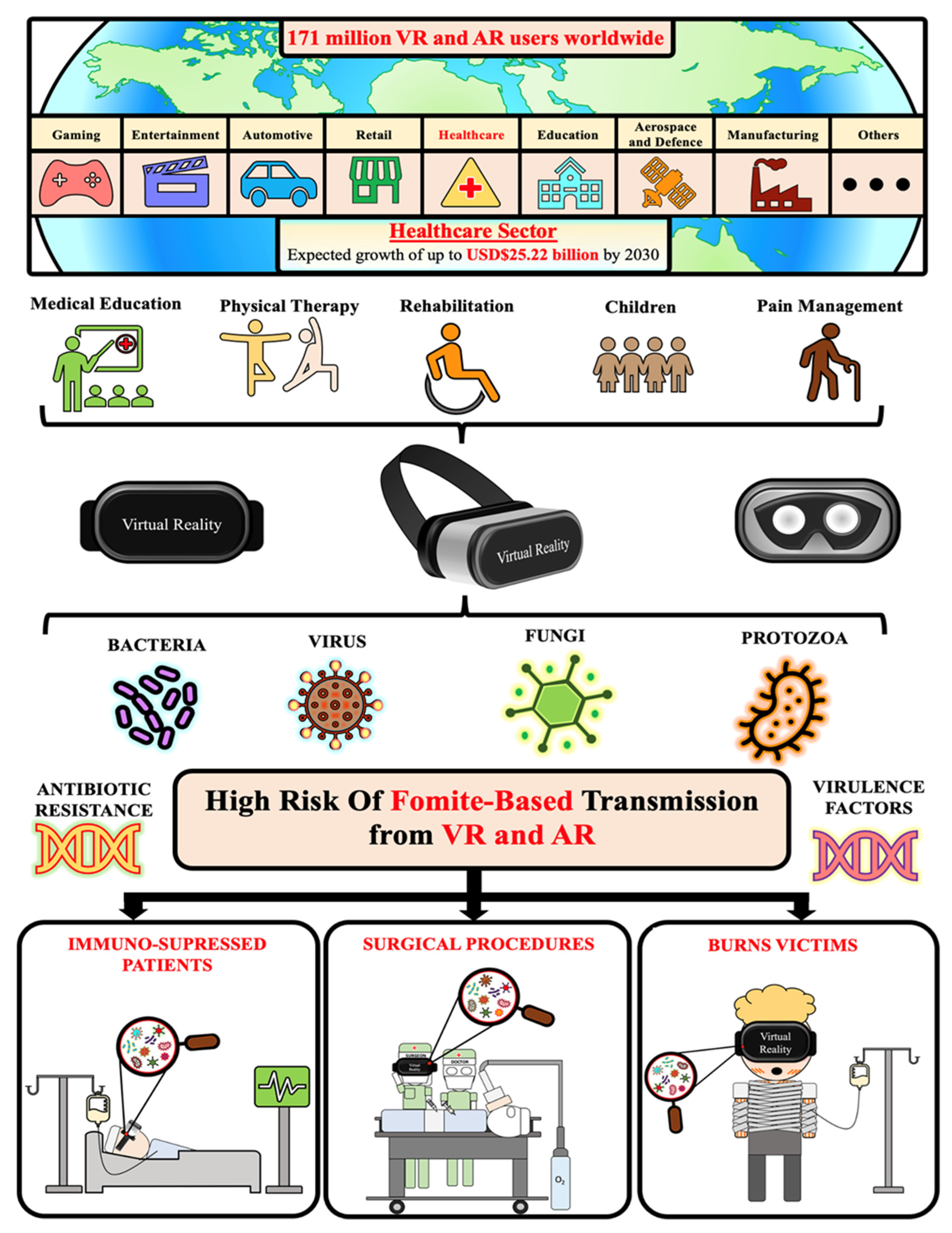
:1. Introduction
Overview
2. Methods
2.1. Search Strategy
2.2. Information Sources and Study Selection
2.3. Data Extraction and Quality Assessment of Sources
3. Results
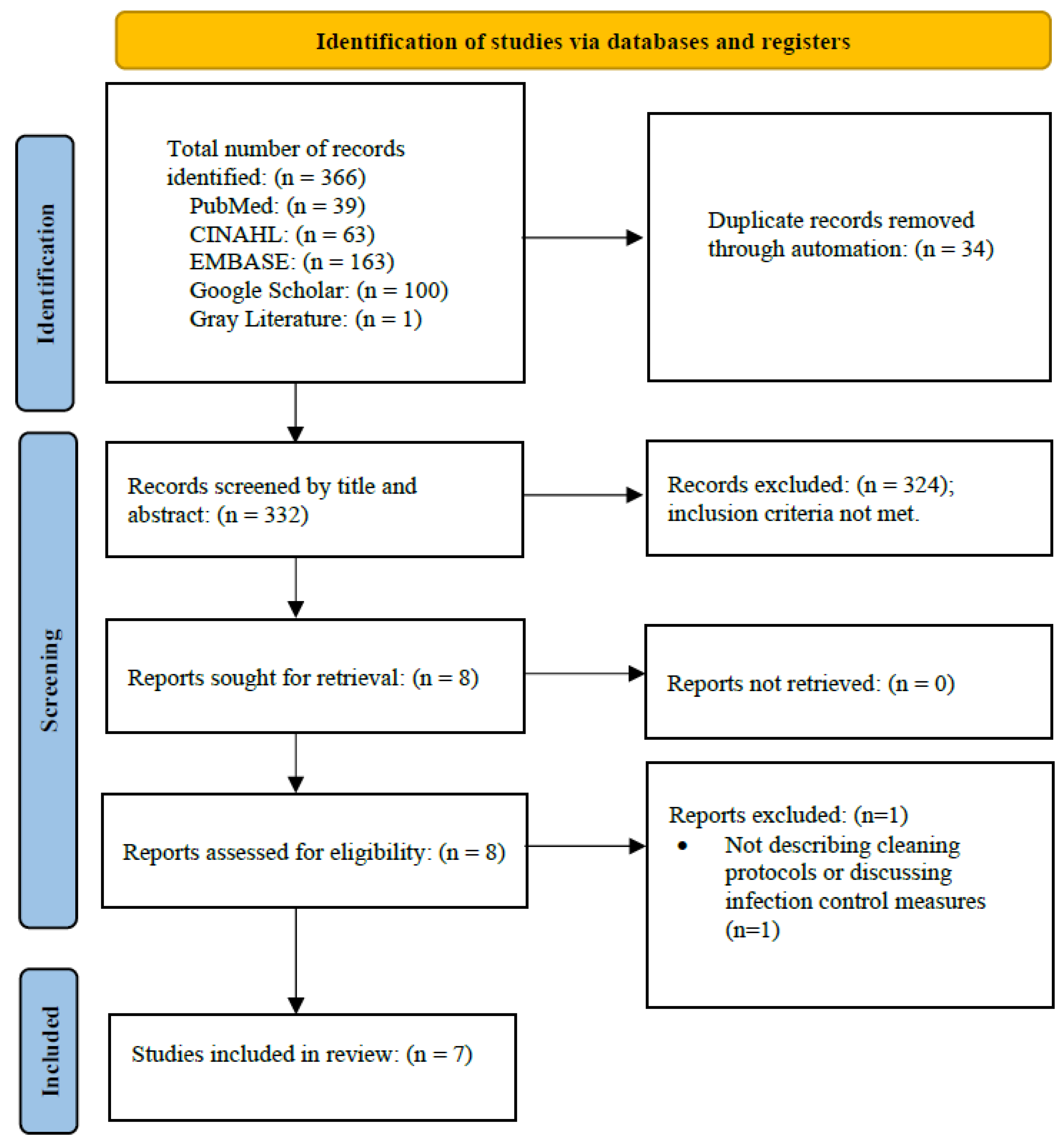
Selection of Sources of Evidence
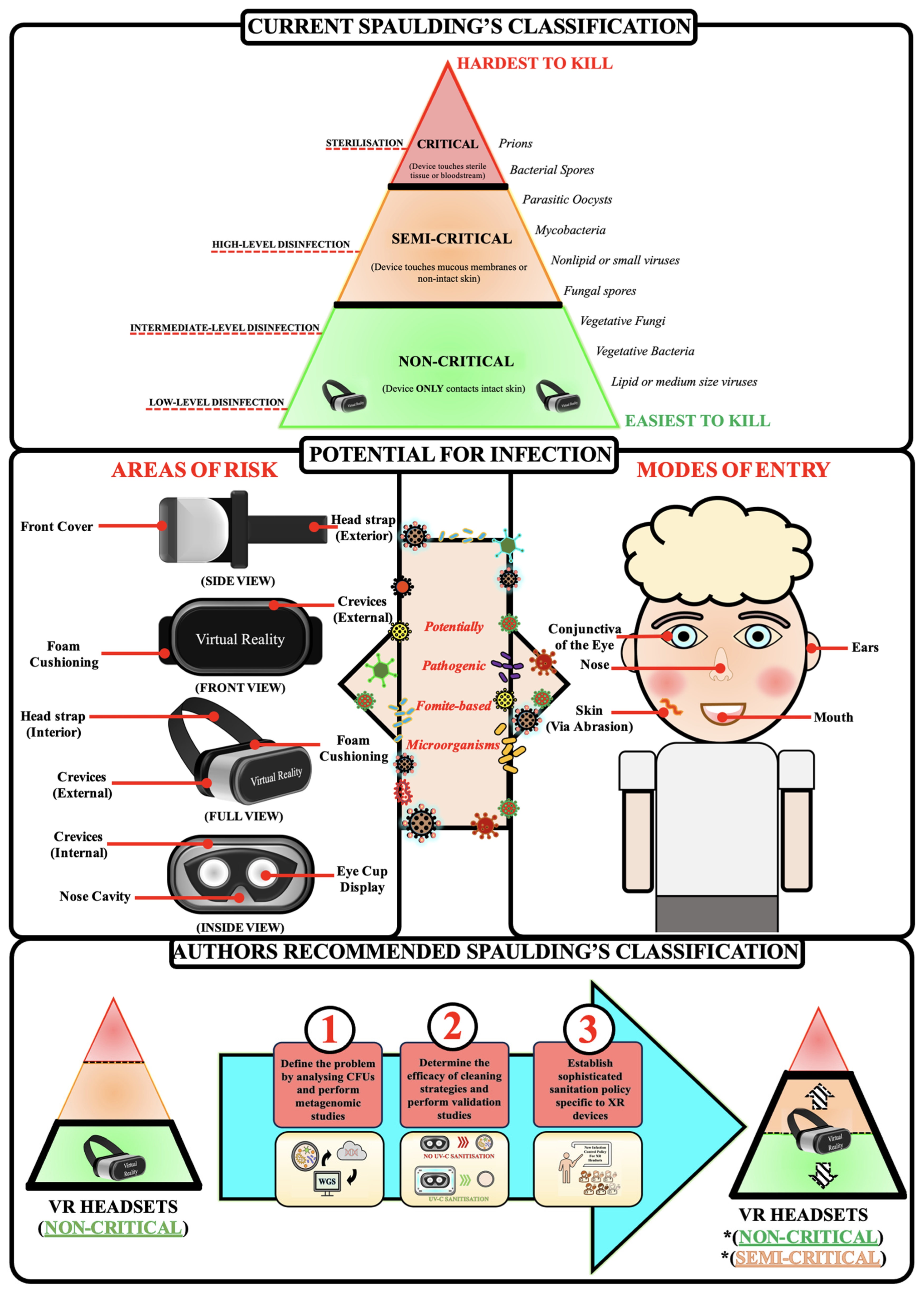
4. Discussion
Overview
5. Study Limitations
6. Author’s Recommendations
7. Conclusions
Funding
Data Availability Statement
Conflicts of Interest
References
- Fortune Business Insights. Virtual Reality (VR in Healthcare Market Size, Share & COVID-19 Impact Analysis, by Component (Hardware, Software, and Content), by Application (Pain Management, Education & Training, Surgery, Paitient Care Management, Rehabilitation & Therapy Procedures, and Post-Traumatic Stress Disorder (PTSD), and Regional Forecast, 2023–2020; Fortune Business Insights: Pune, India, 2022. [Google Scholar]
- Perkins Coie LLP. Augmented and Virtual Reality Survey Report; Perkins Coie LLP: Washington, DC, USA, 2020. [Google Scholar]
- Barcali, E.; Iadanza, E.; Manetti, L.; Francia, P.; Nardi, C.; Bocchi, L. Augmented reality in surgery: A scoping review. Appl. Sci. 2022, 12, 6890. [Google Scholar] [CrossRef]
- Eves, J.; Sudarsanam, A.; Shalhoub, J.; Amiras, D. Augmented reality in vascular and endovascular surgery: Scoping review. JMIR Serious Games 2022, 10, e34501. [Google Scholar] [CrossRef]
- Zhang, J.; Lu, V.; Khanduja, V. The impact of extended reality on surgery: A scoping review. Int. Orthop. 2023, 47, 611–621. [Google Scholar] [CrossRef]
- Goldsworthy, A.; Chawla, J.; Baumann, O.; Birt, J.; Gough, S. Extended Reality Use in Paediatric Intensive Care: A Scoping Review. J. Intensive Care Med. 2023, 38, 856–877. [Google Scholar] [CrossRef]
- Hill, J.E.; Twamley, J.; Breed, H.; Kenyon, R.; Casey, R.; Zhang, J.; Clegg, A. Scoping review of the use of virtual reality in intensive care units. Nurs. Crit. Care 2022, 27, 756–771. [Google Scholar] [CrossRef]
- Bruno, R.R.; Bruining, N.; Jung, C.; VR-ICU Study group Kelm Malte Wolff Georg Wernly Bernhard. Virtual reality in intensive care. Intensive Care Med. 2022, 48, 1227–1229. [Google Scholar] [CrossRef]
- Mo, J.; Vickerstaff, V.; Minton, O.; Tavabie, S.; Taubert, M.; Stone, P.; White, N. How effective is virtual reality technology in palliative care? A systematic review and meta-analysis. Palliat. Med. 2022, 36, 1047–1058. [Google Scholar] [CrossRef]
- Chirico, A.; Lucidi, F.; De Laurentiis, M.; Milanese, C.; Napoli, A.; Giordano, A. Virtual reality in health system: Beyond entertainment. A mini-review on the efficacy of VR during cancer treatment. J. Cell. Physiol. 2016, 231, 275–287. [Google Scholar] [CrossRef]
- Yap, K.Y.-L.; Koh, D.W.H.; Lee, V.S.J.; Wong, L.L. Use of virtual reality in the supportive care management of paediatric patients with cancer. Lancet Child Adolesc. Health 2020, 4, 899–908. [Google Scholar] [CrossRef]
- Zeng, Y.; Zhang, J.-E.; Cheng, A.S.; Cheng, H.; Wefel, J.S. Meta-analysis of the efficacy of virtual reality-based interventions in cancer-related symptom management. Integr. Cancer Ther. 2019, 18, 1534735419871108. [Google Scholar] [CrossRef]
- Pittara, M.; Matsangidou, M.; Stylianides, K.; Petkov, N.; Pattichis, C.S. Virtual reality for pain management in cancer: A comprehensive review. IEEE Access 2020, 8, 225475–225489. [Google Scholar] [CrossRef]
- Sutton, B. 2011 01/04/2018. Available online: https://www.fda.gov/training-and-continuing-education/cdrh-learn/overview-regulatory-requirements-medical-devices-transcript#:~:text=It%20can%20be%20found%20in,%2C%20diagnose%20disease%20in%20man%E2%80%9D (accessed on 27 August 2023).
- Medical Devices Overview 2023. 13 April 2023. Available online: https://www.tga.gov.au/products/medical-devices/medical-devices-overview (accessed on 27 August 2023).
- Is My Product a Medical Device? Available online: https://www.tga.gov.au/resources/my-product-medical-device (accessed on 27 August 2023).
- Bright, K.R.; Boone, S.A.; Gerba, C.P. Occurrence of bacteria and viruses on elementary classroom surfaces and the potential role of classroom hygiene in the spread of infectious diseases. J. Sch. Nurs. 2010, 26, 33–41. [Google Scholar] [CrossRef]
- Vasickova, P.; Pavlik, I.; Verani, M.; Carducci, A. Issues concerning survival of viruses on surfaces. Food Environ. Virol. 2010, 2, 24–34. [Google Scholar] [CrossRef]
- Kramer, A.; Assadian, O. Survival of microorganisms on inanimate surfaces. Use Biocidal Surf. Reduct. Healthc. Acquir. Infect. 2014, 7–26. [Google Scholar] [CrossRef]
- Wang, Z.; He, R.; Chen, K. Thermal comfort and virtual reality headsets. Appl. Ergon. 2020, 85, 103066. [Google Scholar] [CrossRef]
- Xu, X.; Kilroy, D.; Mangina, E.; Campbell, A.G. Work-in-progress—Adapting a virtual reality anatomy teaching tool for mobility: Pilot study. In Proceedings of the 2020 6th International Conference of the Immersive Learning Research Network (iLRN), San Luis Obispo, CA, USA, 21–25 June 2020; pp. 328–331. [Google Scholar]
- Tajouri, L.; Campos, M.; Olsen, M.; Lohning, A.; Jones, P.; Moloney, S.; Grimwood, K.; Ugail, H.; Mahboub, B.; Alawar, H. The role of mobile phones as a possible pathway for pathogen movement, a cross-sectional microbial analysis. Travel Med. Infect. Dis. 2021, 43, 102095. [Google Scholar] [CrossRef]
- Doron, S.; Gorbach, S.L. Bacterial infections: Overview. Int. Encycl. Public Health 2008, 273–282. [Google Scholar] [CrossRef]
- Stone, P.W. Economic burden of healthcare-associated infections: An American perspective. Expert Rev. Pharmacoecon. Outcomes Res. 2009, 9, 417–422. [Google Scholar] [CrossRef]
- Marchetti, A.; Rossiter, R. Economic burden of healthcare-associated infection in US acute care hospitals: Societal perspective. J. Med. Econ. 2013, 16, 1399–1404. [Google Scholar] [CrossRef]
- Chow, E.J.; Mermel, L.A. Hospital-acquired respiratory viral infections: Incidence, morbidity, and mortality in pediatric and adult patients. In Open Forum Infectious Diseases; Oxford University Press: Cary, NC, USA, 2017; p. ofx006. [Google Scholar]
- Zingg, W.; Hopkins, S.; Gayet-Ageron, A.; Holmes, A.; Sharland, M.; Suetens, C.; Almeida, M.; Asembergiene, J.; Borg, M.A.; Budimir, A. Health-care-associated infections in neonates, children, and adolescents: An analysis of paediatric data from the European Centre for Disease Prevention and Control point-prevalence survey. Lancet Infect. Dis. 2017, 17, 381–389. [Google Scholar] [CrossRef]
- Peters, M.D.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar] [CrossRef]
- Creel, B. Bacterial Load in Virtual Reality Headsets. In Proceedings of the 26th ACM Symposium on Virtual Reality Software and Technology, Virtual, 1–4 November 2020. [Google Scholar]
- Roberts, S.C.; Havill, N.L.; Flores, R.M.; Hendrix II, C.A.; Williams, M.J.; Feinn, R.S.; Choi, S.J.; Martinello, R.A.; Marks, A.M.; Murray, T.S. Disinfection of Virtual Reality Devices in Health Care Settings: In Vitro Assessment and Survey Study. J. Med. Internet Res. 2022, 24, e42332. [Google Scholar] [CrossRef]
- Daniel, V.; Jones, R.; Dhillon, R.; Duckers, J.; Rattenbury, S. EPS9. 09 Pilot study to evaluate the use of dry chlorine dioxide gas for sterilisation of virtual reality headsets. J. Cyst. Fibros. 2023, 22, S63. [Google Scholar] [CrossRef]
- Høeg, E.R.; Lange, B. A Survey of Virtual Reality Hygiene Practices. In Proceedings of the International Conference on Disability, Virtual Reality & Associated Technologies, Ponta Delgada, Portugal, 6–8 September 2022. [Google Scholar]
- Moore, N.; Dempsey, K.; Hockey, P.; Jain, S.; Poronnik, P.; Shaban, R.Z.; Ahmadpour, N. Innovation during a pandemic: Developing a guideline for infection prevention and control to support education through virtual reality. Front. Digit. Health 2021, 3, 628452. [Google Scholar] [CrossRef]
- International Standards Organisation. Augmented and Virtual Reality Safety–Guidance on Safe Immersion, Set Up and Usage; International Standards Organisation: Geneva, Switzerland, 2024; pp. 1–27. [Google Scholar]
- Goldsworthy, A.; Chawla, J.; Birt, J.; Baumann, O.; Gough, S. Use of extended reality in sleep health, medicine, and research: A scoping review. Sleep 2023, 46, zsad201. [Google Scholar] [CrossRef]
- McDonnell, G.; Burke, P. Disinfection: Is it time to reconsider Spaulding? J. Hosp. Infect. 2011, 78, 163–170. [Google Scholar] [CrossRef]
- Rutala, W.A.; Weber, D.J. Disinfection and sterilization in health care facilities: An overview and current issues. Infect. Dis. Clin. 2016, 30, 609–637. [Google Scholar] [CrossRef]
- Burt, M. Theme Parks Employ Virtual Reality as Part of the Entertainment Mix—But What Do Audiences Think? 2023. Available online: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4475874 (accessed on 10 April 2024).
- Azari, A.A.; Arabi, A. Conjunctivitis: A systematic review. J. Ophthalmic Vis. Res. 2020, 15, 372. [Google Scholar] [CrossRef]
- Gallandat, K.; Kolus, R.C.; Julian, T.R.; Lantagne, D.S. A systematic review of chlorine-based surface disinfection efficacy to inform recommendations for low-resource outbreak settings. Am. J. Infect. Control 2021, 49, 90–103. [Google Scholar] [CrossRef]
| Study ID | Article Type | Aim(s) | Comments |
|---|---|---|---|
| Moore et al., 2021 [33] | Cleaning Guideline | Aim 1: Document the process of developing an operational guide for cleaning and disinfection of HMDs in New South Wales, Australia. Aim 2: Describe the emergence of VR as a supporting modality for clinical education, the principles of infection prevention and control and how these principles underpin the development of a guideline for VR cleaning and disinfection to ensure the safety of users. Aim 3: We then identify future directions for research and innovation. | Take home messages:
|
| International Standards Organisation [34] | Guidance Document | Aim 1: Provide guidance on the safe set up and usage of VR and AR in consumer and enterprise domains. | Take home messages:
|
| Høeg and Lange, 2022 [32] | Survey | Aim 1: Survey a range of stakeholders who use VR HMDs to understand the range of hygiene practices currently utilised and identify areas for future research. | Most popular VR headsets in use:
|
| Goldsworthy et al., 2023 [6] | Scoping Review | Aim 1: Determine what cleaning/infection control policies/procedures are utilised for XR in paediatric intensive care units. | VR HMDs Utilised:
|
| Roberts et al., 2022 [30] | Survey and Microbial Count | Aim 1: Determine current disinfection practices in health care settings and how they were established. Aim 2: Report on the effect of commonly used disinfectant wipes on the disinfection of VR headsets experimentally contaminated with common bacterial pathogens. Aim 3: Describe a standard operating procedure to reduce infections with multi-patient VR utilisation. |
VR systems used in healthcare:
|
| Creel et al., 2020 [29] | Microbial Count and rRNA sequencing | Aim 1: Analyse the potential for these headsets to become contaminated. |
Take home messages:
|
| Daniel et al., 2023 [31] | Microbial Count | Aim 1: Evaluate the use of dry chlorine dioxide (dCl02) gas with parametric validation as a standardised decontamination method for VR HMDs. |
Take home messages:
|
| Study ID | Country | Setting | Population | Number of Sampled VR Headsets | Microorganism Group | Colony Growth (Viability) | DNA Extraction Kit | DNA Sequencing | Antibiotic Sensitivity Test |
|---|---|---|---|---|---|---|---|---|---|
| Creel et al., 2020 [29] | United States of America | Public lab space at the University of Mississippi | University Students | 2 | Bacteria | Yes | MoBio Ultra Clean Microbial DNA Isolation Kit | 16S rRNA gene sequencing | Yes |
| Roberts, et al., 2022 [30] | United States of America | Laboratory setting | Inoculation of HMDs | 2 | Bacteria | Yes | No | No | No |
| Daniel et al., 2023 [31] | United Kingdom | Laboratory setting | Inoculation of HMDs | 2 | Bacteria | Yes | No | No | No |
| Cleaning Protocol Details | Roberts et al., 2022 [30] | Moore et al., 2021 [33] | Creel et al., 2020 [29] | Daniel et al., 2023 [31] | International Standards Organisation, 2023 [34] | |
|---|---|---|---|---|---|---|
| Before XR Use | Examine the device for signs of contamination, and if no obvious signs of contamination proceed to use. | ✕ | ✕ | ✕ | ✕ | ✓ |
| User to wash hands before use. | N/A | ✕ | ✕ | ✕ | † | |
| Patient and staff perform hand hygiene. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Fit nonporous cover over facial interface. | ✓ | ✕ | ✓ | ✕ | † | |
| Cover hair with surgical cap. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Fit user with face mask. | ✕ | ✕ | ✓ | ✕ | ✕ | |
| Assess device for disinfectant suitability. | ✓ | ✕ | ✕ | ✕ | ✓ | |
| Use disinfecting wipes to clean all surfaces. | ✕ | ✕ | ✓ | ✕ | ✕ | |
| Use a device-compatible, EPA-registered product List H according to the manufacturer’s instructions for use, ensuring all surfaces are saturated. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| After XR Use | Expose VR HMD to 2000 ppm/h of dClO2 gas. | ✕ | ✕ | ✕ | ✓ | ✕ |
| Proper use of UV-C light. | ✕ | ✕ | ✕ | ✕ | ✓ | |
| Patient to perform hand hygiene. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Staff to perform hand hygiene. | ✓ | ✓ | ✕ | ✕ | ✕ | |
| Staff don appropriate PPE inclusive of nitrile gloves +/− other equipment as required by patient’s transmission-based isolation protocols (if applicable). | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Remove device from patient and place on a clean disposable pad. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Remove facial interface barrier. If disposable, discard. | ✓ | ✓ | ✕ | ✕ | ✕ | |
| Clean reusable face pads with a detergent solution or wipe. | ✕ | ✓ | ✕ | ✕ | ✕ | |
| Clean hands with alcohol-based hand rub or soap and water. | ✕ | ✓ | ✕ | ✕ | ✕ | |
| Clean all visibly soiled areas with disposable wipes or paper towels. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Ensure surfaces are wet for 2–4 min following wiping with chemical disinfectant. | ✕ | ✕ | ✕ | ✕ | ✓ | |
| Clean lenses with microfiber cloth. | ✕ | ✕ | ✕ | ✕ | ✓ | |
| Use a device-compatible, EPA-registered product List H according to the manufacturer’s instructions for use, ensuring all surfaces are saturated. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Use a new wipe to clean each surface. | ✕ | ✓ | ✕ | ✕ | ✕ | |
| Allow HMD and controllers to dry. | ✓ | ✓ | ✕ | ✕ | ✓ | |
| Store device in dry space physically separated from non-disinfected devices. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Leave items to dry and store them in a clean, sealable and disposable bag. | ✕ | ✓ | ✕ | ✕ | ✕ | |
| Patient to perform hand hygiene. | ✓ | ✕ | ✕ | ✕ | ✕ | |
| Staff to perform hand hygiene. | ✓ | ✓ | ✕ | ✕ | ✕ | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Goldsworthy, A.; Olsen, M.; Koh, A.; Demaneuf, T.; Singh, G.; Almheiri, R.; Chapman, B.; Almazrouei, S.; Ghemrawi, R.; Senok, A.; et al. Extended Reality Head-Mounted Displays Are Likely to Pose a Significant Risk in Medical Settings While Current Classification Remains as Non-Critical. Microorganisms 2024, 12, 815. https://doi.org/10.3390/microorganisms12040815
Goldsworthy A, Olsen M, Koh A, Demaneuf T, Singh G, Almheiri R, Chapman B, Almazrouei S, Ghemrawi R, Senok A, et al. Extended Reality Head-Mounted Displays Are Likely to Pose a Significant Risk in Medical Settings While Current Classification Remains as Non-Critical. Microorganisms. 2024; 12(4):815. https://doi.org/10.3390/microorganisms12040815
Chicago/Turabian StyleGoldsworthy, Adrian, Matthew Olsen, Andy Koh, Thibaut Demaneuf, Gobinddeep Singh, Reem Almheiri, Brendan Chapman, Shaima Almazrouei, Rose Ghemrawi, Abiola Senok, and et al. 2024. "Extended Reality Head-Mounted Displays Are Likely to Pose a Significant Risk in Medical Settings While Current Classification Remains as Non-Critical" Microorganisms 12, no. 4: 815. https://doi.org/10.3390/microorganisms12040815
APA StyleGoldsworthy, A., Olsen, M., Koh, A., Demaneuf, T., Singh, G., Almheiri, R., Chapman, B., Almazrouei, S., Ghemrawi, R., Senok, A., McKirdy, S., Alghafri, R., & Tajouri, L. (2024). Extended Reality Head-Mounted Displays Are Likely to Pose a Significant Risk in Medical Settings While Current Classification Remains as Non-Critical. Microorganisms, 12(4), 815. https://doi.org/10.3390/microorganisms12040815






