Abstract
The depletion of health professionals’ morale and motivation in the aftermath of the COVID-19 pandemic sparked an interest in understanding what drives workers to choose and remain motivated in the health sector. This study contributes to a better understanding of this phenomenon by specifically analyzing the sociodemographic underpinnings of health professionals’ public service motivation (PSM) in Portugal. The rationale is to analyze whether PSM varies among health professionals according to gender, age, education, and managerial position in an unexplored area (health) and context (Portugal). A shorter version of the PSM scale was applied to health professionals (doctors and nurses) (n = 413). The results suggest that there are differences regarding gender and age, specifically with female and older participants presenting higher levels of PSM. The same is true for those who hold a managerial position. Our results align with patterns found in studies conducted within other cultural contexts. Most importantly, however, by exploring higher and lower PSM levels according to different sociodemographics, we provide relevant clues for future qualitative studies and formulate practical measures to tackle these issues, thereby strengthening evidence-based policy formulation.
1. Introduction
Understanding what motivates and drives professionals to work in the public sector, a topic extensively explored in research on public service motivation (PSM) (Belrhiti et al. 2019; Perry and Wise 1990; Brewer and Selden 1998; Rainey and Steinbauer 1999), is increasingly pertinent for policymakers, researchers, and practitioners (WHO 2017; Dieleman et al. 2009). PSM encompasses a set of individual beliefs, motivations, and attitudes toward the nature and mission of public institutions (Perry and Wise 1990).
Translating this framework to the healthcare domain is complex due to the centrality of human resources and their motivations in the delivery of care. The quality of the health services is largely determined by the behavior of health workers because of their efforts; thus, human resources have an important power for increase de efficient and effectiveness, more than other services in public administration (Kitsios and Kamariotou 2021). Although research on PSM dates to the 1990s (Perry and Wise 1990; Herzberg et al. 1959; McCarthy et al. 2021), its application to healthcare professionals is relatively recent (Fernandes et al. 2022).
Within this context, healthcare workers are acknowledged by the World Health Organization (WHO) as the cornerstone of healthcare provision. As such, favorable employment conditions, both financial and non-financial incentives, career advancement opportunities, and ongoing investment in education to uphold the quality and equity of their services are relevant matters to consider (Campbell et al. 2014). Motivated employees are better equipped to navigate through various challenges, such as those posed by the recent COVID-19 pandemic (AlAbri and Siron 2020; Wang et al. 2020a; Windarwati et al. 2021).
In the aftermath of the pandemic, healthcare professionals were one of the most affected groups, grappling with high levels of stress and burnout (Bridgeman et al. 2018). The juxtaposition of this strain with the intrinsic motivations of healthcare workers underscores the need to explore the motivations of human resources in the healthcare sector (Nunes and Ferreira 2023).
In the Portuguese context, this crisis impacted the retention of doctors and nurses within the National Health Service (NHS). To properly understand the current situation of healthcare professionals in Portugal, including their motivations, we need a longitudinal perspective, also considering the weight of major events from the past decade, such as the financial crisis (2011–2014), which translated into salary reductions, increased work hours, and decreased investment in equipment, and more recently the COVID-19 pandemic crisis, which worsened pressure on the NHS and its professionals, dictating multifaceted solutions to attract and retain healthcare workers within the NHS (Nova SBE 2022).
While there are common factors affecting the motivation and commitment of healthcare workers, there may be variations across geographical contexts and organizational cultures. Factors such as remuneration (Bansal and Malhotra 2016; Humphrey and Russell 2004; Ferrinho et al. 1998), available resources and working conditions (Mazahir and Khalid 2017; Mbindyo et al. 2009), absenteeism, and the frequency of patient interactions (Aninanya et al. 2016; Franco et al. 2002) are universally recognized. However, these factors often adopt a predominantly individualistic perspective on healthcare workers, overlooking the organizational context, career development opportunities, and management/leadership approaches within institutions (Fernandes et al. 2022).
To evaluate PSM determinants and how they affect professional motivation, it is necessary to account for both sociodemographics and institutional processes (Bright 2005; Perry 1997; Vandenabeele 2007). However, most analyses of sociodemographic antecedents and their impact on PSM have focused on the US context (Kitsios and Kamariotou 2021; Kim et al. 2013), and little is known about PSM sociodemographic antecedents in European countries (Wang et al. 2020b). Additionally, studies have often examined socio-historical antecedents such as gender and age, but findings have been inconsistent. To the best of our knowledge, no research addresses sociodemographic antecedents in PSM specifically for health professionals in the Portuguese context.
This study focuses on the motivation for public service in Portugal and its expression among health professionals, specifically by examining how PSM varies according to different sociodemographic features. To evaluate the motivation of health professionals in Portugal, particularly to work in the public sector, a PSM assessment instrument was used, aiming to align closely with the one developed by Perry (1996). Hence, a concise PSM assessment scale, developed by Kim et al. (2013), was employed. This decision was based on its ease of implementation and its prior testing across various geographic contexts, rendering its application more universally appropriate. Furthermore, its limited application in the Portuguese context, particularly within the healthcare sector, adds an innovative dimension to this study.
Drawing upon the available literature, we propose the following exploratory hypotheses:
H1.
Older health professionals exhibit higher levels of public service motivation.
H2.
Female health professionals have higher levels of public service motivation.
H3.
Health professionals with higher levels of education display higher levels of public service motivation.
H4.
Health professionals with management positions exhibit higher levels of public service motivation compared to non-managers.
The remaining sections outline the brief theoretical concepts, description of the methods used, followed by the results and a discussion of the obtained findings, ending with some concluding remarks and suggestions/limitations for future research.
2. Theoretical Framework
Employees’ motivation within organizations is influenced by a complex set of social, professional, and economic factors whose interactions have been addressed by different fields of knowledge (Lee and Raschke 2016). Concerning public institutions, the administrative reforms carried out in the 1980s, aligned with the “New Public Management” principles, stressed the importance of key concepts such as performance, efficiency, transparency, and efficacy in the delivery of public services (Gruening 2001; Klijn 2012), changing management practices and human resources. However, employees’ motivation to choose and remain in the public sector was overlooked for a long time (Waterhouse 2008; O’Riordan 2013), creating a gap in strategies to attract and retain professionals aligned with public values.
In this context, the term public service motivation (PSM) was introduced by Perry and Wise (1990) in their seminal work on the motivational bases of public service, referring to the sensitivity that individuals have towards the public mission and its respective objectives (Zhang et al. 2022). PSM theory was developed to challenge rational choice perspectives on bureaucratic behavior, which assume a focus on self-interest and maximizing personal gains, such as reputation, power, and monetary rewards. However, goals are often less specified in public organizations, and performance is more difficult to measure and link to external rewards. Therefore, PSM emphasizes the significant role of self-determined motivation, such as moral obligation, intrinsic motivation, and affect in explaining work behavior and job performance in public organizations (Zhang et al. 2022; Wang et al. 2020b).
With this psychological profile, the factors leading individuals to choose public institutions can be categorized as follows (Perry and Vandenabeele 2008; Kim and Vandenabeele 2010; Belrhiti et al. 2019): (i) Rational motives, in which professionals engage in decision-making processes out of a sense of social duty or to enhance their self-esteem; (ii) Affective motives, which encompasses an identification with public service and a compassionate connection with service users, driven by a spirit of self-sacrifice; (iii) Normative motives, meaning an aspiration to altruistically serve the public interest, guided by principles of equity.
To measure PSM and carry out further studies on this concept, experts focused on developing and refining assessment instruments capable of measuring this construct. The PSM measurement scale was first developed by Perry (1996), assuming a multidimensional construct with four types of motives: Compassion, Attraction to Public Service, Commitment to Public Values, and Self-Sacrifice. Compassion is an individual’s affective commitment to the concern and well-being of others or society in general. Attraction to Public Service refers to internal satisfaction or the pleasure of serving the public. Commitment to Public Values reflects a norms-based motive to fulfill social obligations and pursue public values. Self-Sacrifice is a prosocial tendency to make personal sacrifices to contribute to the well-being of others or society in general. Based on these four dimensions, the higher the level of PSM, the more likely an individual is to act beyond monetary or reputational benefits and be aligned with serving the public cause (Perry 1996; Zhang et al. 2022; Wang et al. 2020b).
This scale, consisting of 24 items, was later revised into a PSM measurement instrument validated in 12 countries to address existing weaknesses in the literature and to universalize it to different contexts (Kim 2021). Based on 16 items and the 4 dimensions developed by Perry, this scale aims to provide a better theoretical and empirical basis for measuring PSM, acknowledging that the results obtained and their exact meaning will likely differ between cultures and languages. This variability makes it challenging to develop a single universal PSM scale or make direct comparisons of PSM between countries. In the words of Perry and Vandenabeele (2015), “the scale is shorter, the compassion subscale is more reliable, and the scale’s overall statistical properties are robust”.
Perry (1997), one of the foremost advocates of this construct, emphasized the significance of considering PSM from the perspective of religious, cultural, or family-related factors (Gruening 2001). Thus, the discourse surrounding PSM highlights the need to examine a multitude of factors and understand their interrelationships, including age, gender, education, profession, sector of employment, and managerial positions (Perry and Wise 1990; Bright 2005). In this regard, Pandey and Stazyk (2008) contextualize PSM within: (i) sociodemographic factors (e.g., gender, age, education); (ii) social institutions (e.g., family, religion); and (iii) organizational factors (e.g., years of employment, bureaucratic processes). Nevertheless, there are limited empirical examples in public administration research that provide insights into the antecedents of public service motivation (PSM), especially within the healthcare sector and among its professionals.
The research published so far suggests gender differences, with women often exhibiting higher levels of PSM, particularly in the dimension of compassion (Waterhouse 2008; Belrhiti et al. 2019). However, a study by Forte et al. (2022) and Kim (2016) found that men scored higher than women in that dimension. Positive correlations are noted between age and various dimensions of PSM, with older workers displaying a stronger commitment to the public sector (Forte et al. 2022; Parola et al. 2019; Camilleri 2007; Vandenabeele 2011; Temesgen et al. 2016). Naff and Crum’s (1999) study indicated that an individual’s propensity to serve in the public interest typically increases with age, while the need for compassion, self-sacrifice, and policymaking tends to diminish, albeit marginally, with age.
Regarding education levels, Camilleri’s (2007) study showed a significant yet slight negative correlation between education and PSM dimensions. Other studies (Bright 2005; Vandenabeele 2011; Naff and Crum 1999) revealed that individuals with lower education levels tend to exhibit lower levels of motivation for public service compared to their more educated counterparts. Notably, differences among education levels are particularly evident in the dimension of self-sacrifice.
Concerning the sector of employment, Naff and Crum’s study (1999) suggested that PSM exerts a modest yet statistically significant influence on employees’ considerations of leaving the public sector. This relationship is negative, implying that individuals with higher PSM are less likely to seek employment in the private sector. Regarding managerial positions, some studies suggested that managerial level serves as a robust predictor of PSM (Perry 1996; Kim 2021). Conversely, Desmarais and Gamassou (2014) argued that managers tend to exhibit lower overall PSM, primarily due to reduced sensitivity to the emotional dimensions of PSM, such as compassion and self-sacrifice.
Overall, the literature suggests that both socio-historical contexts and individual characteristics yield a mixture of results that are not always consistent. However, the motivational context related to antecedents and sociodemographic factors tends to correlate with PSM, as described by Camilleri (2007).
The current state of the art justifies the need to develop more robust studies and methodologies to explore the mechanisms supporting the maintenance and commitment of healthcare professionals to the public sector (Belrhiti et al. 2019; Fernandes et al. 2022; Stefurak et al. 2020). To the best of our knowledge, no recent studies have specifically explored PSM in healthcare professionals in Portugal, making it a compelling case study, particularly given the current context outlined above.
3. Materials and Methods
3.1. Setting the Scene
The Portuguese health system has been primarily based on a National Health Service (NHS) since 1979. Operating under the supervision of the Ministry of Health, the NHS comprises various decentralized institutions distributed throughout the territory. Nonetheless, the Ministry of Health holds responsibility for defining and implementing health policies (Santinha et al. 2023).
Financed predominantly through general taxation with universal coverage as its cornerstone, the organization of healthcare services falls under the purview of the Directorate-General for Health at the national level and the Regional Health Administrations at the regional level (Santinha 2016; Simões 2009; Julião and Nunes 2019).1
The NHS offers general, specialist, acute healthcare, and hospital care. Primary care is delivered through family health units and personalized health units, grouped into clusters of basic health units. Secondary and tertiary care is provided by hospital units, which may be geographically clustered into hospital centers (Tavares et al. 2023).
At a public policy level, the existence of a National Health Service implies that the planning of human resources in health focuses, first and foremost, on those dedicated to the public component of the system. Notwithstanding, it is desirable to evaluate and plan for public and private sectors especially if they function in an interconnected and interdependent manner (PlanAPP 2023).
The average annual rate of change in NHS RHS over the period 2010–2023 was approximately 1.7% per year. However, this growth was not uniform: 2019 witnessed significant increases across all categories, indicating a pronounced reinforcement of RHS. Subsequently, in 2020, another substantial increase was observed across all categories, likely reflecting the response to the COVID-19 pandemic (PlanAPP 2023, 2024).
Nurses exhibited the most substantial growth over the past thirteen years, with an average annual increase of approximately 880 professionals. Despite this decade-long increase, the number of nurses (7.4 per 1000 inhabitants in 2023) remains below the EU average (9.2 per 1000 inhabitants) (PlanAPP 2023; OECD 2023).
In percentage terms, the most significant growth occurred among Internal Doctors, with an average annual increase of around 4.4%, rising from approximately 6000 professionals in 2010 to 10,463 in 2023, representing an increase of about 74%. Specialist Doctors experienced an average growth of 27.1% over the period, equivalent to 1.9% per year, translating to an average of 361 additional specialist professionals annually (PlanAPP 2024).
The number of doctors in Portugal has steadily increased since 2000, reaching 5.6 doctors per 1000 inhabitants in 2023 (+1.9 compared to the OECD average). However, this figure refers to all qualified doctors, which presents an inflated estimate when compared to data from other countries, which typically refer solely to practicing doctors (PlanAPP 2023; OECD 2023).
3.2. Instrument
One of the most widely used instruments for measuring PSM is the one developed by Perry (1996), comprising 4 dimensions and 24 items. However, several studies have identified weaknesses in certain dimensions (Coursey and Pandey 2007; Kim 2009; Ritz 2011; Taylor 2007; Wright 2008). In response to these limitations and to create a universal measurement tool adaptable to the demographic realities of various countries, Kim et al. (2013) proposed a more versatile measure. This instrument comprises 16 questions rated on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree), subdivided into four dimensions: “attraction to policy participation (APP)”, “commitment to public values (CPV)”, “compassion (COM)”, and “self-sacrifice (SS)” (Appendix A—Table A1). It is precisely because of its universality and application in different geographic contexts that we used the scale developed by Kim et al. (2013), including, in addition to this, a set of sociodemographic questions such as gender, age group, profession, managerial position, sector of activity, level of education and hospital of current activity (Kim et al. 2013).
3.3. Data Analysis
The sample was analyzed collectively and by professional subgroups (doctors and nurses). For each motivational factor used in the instrument developed by Kim et al. (2013), summed scores were calculated on a scale ranging from 1 to 5, with higher scores indicating greater motivation to perform well in that specific factor. Parametric tests, namely the t-test and ANOVA, were conducted to compare groups based on gender, education, age group, managerial positions, and sector of employment. Multivariate analyses were conducted, with each motivational factor serving as the dependent variable and sociodemographic variables acting as independent variables. Internal consistency reliability was assessed using Cronbach’s alpha coefficient and compared with the respective values observed during the instrument’s development (Kim et al. 2013). All analyses were conducted using SPSS version 29.0.1 (SPSS Inc., Chicago, IL, USA).
3.4. Sample
This study used a non-probabilistic purposeful sample obtained by contacting all hospitals in Portugal (n = 240) across both the public and private sectors. An online questionnaire was administered via the LimeSurvey platform from October 2022 to May 2023. A total of 413 health professionals participated in the study, representing various hospitals in Portugal (Table 1). The COVID-19 pandemic caused significant and unforeseeable delays in data collection, primarily due to the increased workload on hospital staff. To address this, we extended the initial survey period. Although the overburdened hospital staff made it challenging to obtain additional responses, the number of respondents exceeded the sample size needed for a 95% confidence interval with a 5% margin of error for a total of 142,000 healthcare professionals (doctors and nurses) working in Portugal in secondary care. Compared to similar studies (e.g., Schott and Pronk 2014; Jensen et al. 2019), our sample size not only meets but exceeds the necessary threshold, suggesting a robust dataset for analysis. Among the respondents, 82.1% identified as women, while 17.9% identified as men. Concerning the age distribution of participants, 10.7% were aged 30 years or younger, 30.8% were aged between 31 and 40 years, 27.1% were between 41 and 50 years, 22.0% were between 51 and 60 years, and 9.4% were over 60 years old. Regarding the participants’ areas of work, the majority were nurses (73.4%), followed by doctors (26.6%). In terms of educational attainment, 34.9% had a master’s degree, 21.3% had a postgraduate degree, and only 2.2% held a doctorate. Regarding managerial positions, 21.3% of participants held management positions associated with their work. It is worth noting that 79.9% worked exclusively in the public sector, with 17.2% working across both the public and private sectors.

Table 1.
Descriptive statistics of the sample.
4. Results
The reliability analysis for the 16 survey items yielded a Cronbach’s alpha of 0.854. Upon further analysis by dimension, the Cronbach’s alpha values were as follows: “Attraction to policy participation” = 0.534, “Commitment to public values” = 0.676, “Compassion” = 0.807, “Self-sacrifice” = 0.868.
The overall Cronbach’s alpha value aligns with that of the study by Desmarais and Gamassou (2014), which reported a Cronbach’s alpha of 0.850, and exceeds that of (Kim 2016), with a Cronbach’s alpha of 0.774. On average, the four dimensions also align with these studies, with the only dimension below expectations being the “Attraction to policy participation” dimension. The remaining dimensions scored higher, indicating that the instrument is suitable for the Portuguese context.
Table 2 illustrates differences between male and female health professionals. Significant disparities are observed in the dimension of “Commitment to public values” (p < 0.001), indicating significant differences between male and female professionals, t (411) = 2.45, p = 0.015. Further analysis reveals that significant differences (p < 0.001) arise specifically in questions PSM 5 “I believe that equal opportunities for all citizens are very important” and PSM 8 “Acting ethically is essential for good public service”.

Table 2.
T-Test results for the gender of health professionals.
Upon examining the averages across the four dimensions of the PSM instrument, it is evident that the average scores for female health professionals are higher in the dimensions of “Attraction to policy participation” (M = 4.43; SD = 0.46), “Commitment to public values” (M = 4.83; SD = 0.29), and “Compassion” (M = 4.69; SD = 0.43), in contrast to male health professionals. Conversely, in the dimension of “Self-sacrifice”, the average score is higher among male professionals (M = 3.48; SD = 0.82).
There are significant differences in terms of age groups regarding the dimensions of the PSM instrument, particularly in the “Self-sacrifice” dimension, F (4, 408) = 6.49, p < 0.001 (Table 3).

Table 3.
ANOVA results for the age category of health professionals.
The application of the post-hoc Bonferroni test reveals significant differences only between groups in the “Self-sacrifice” dimension, specifically in the age groups <30 years and 51–60 years (p = 0.006), >60 years (p = 0.007); between individuals aged 31–40 years and individuals 51–60 years (p = 0.005), >60 years (p = 0.010); between individuals aged 41–50 years and individuals 51–60 years (p = 0.025), >60 years (p = 0.032).
Upon analyzing the age distribution of health professionals, it is notable that the average is higher in the age group between 51–60 years for the dimensions of “Attraction to policy participation” (M = 4.51; SD = 0.46), “Commitment to public values” (M = 4.87; SD = 0.29), and “Compassion” (M = 4.71; SD = 0.43). Conversely, in the “Self-sacrifice” dimension, the average is higher in the age group over 60 years old (M = 3.76; SD = 0.96).
There are no statistically significant differences between the categories of doctors and nurses (Table 4), as none of the dimensions analyzed yielded p-values < 0.05. When examining the professional categories of health professionals, it is evident that the average scores for nurses are higher than those for doctors in the dimensions of “Attraction to policy participation” (M = 4.43; SD = 0.47) and “Commitment to public values” (M = 4.82; SD = 0.32). Conversely, doctors exhibit a higher average in the “Self-sacrifice” dimension (M = 3.40; SD = 0.82). The average score for the “Compassion” dimension is the same for both professionals (M = 4.66).

Table 4.
t-Test results for the profession category of health professionals.
Upon reviewing the results related to the level of education (Table 5), differences are observed in the dimension of “Commitment to public values” (p = 0.03). Although the Bonferroni Test does not yield statistically significant results, further analysis reveals differences in questions PSM 5 “We consider equal opportunities for all citizens to be very important” (p = 0.001) and PSM6 “I think it is important that citizens can count on the continuous provision of public services” (p = 0.023).

Table 5.
ANOVA results for the education level of health professionals.
Furthermore, professionals with postgraduate degrees demonstrate a higher average in the dimensions of “Attraction to policy participation” (M = 4.42; SD = 0.47) and “Commitment to public values” (M = 4.86; SD = 0.22). In the “Compassion” dimension, the average is higher among doctorate professionals (M = 4.72; SD = 0.66), while in the “Self-sacrifice” dimension, the average is higher among licensed professionals (M = 3.45; SD = 0.87).
While there are no statistically significant differences between sectors (Table 6), the average scores of professionals exclusively working in the public sector are higher in the dimensions of “Attraction to policy participation” (M = 4.43; SD = 0.46), “Commitment to public values” (M = 4.82; SD = 0.30), and “Compassion” (M = 4.67; SD = 0.43). Conversely, in the “Self-sacrifice” dimension, professionals operating in both sectors exhibit a higher average (M = 3.43; SD = 0.75).

Table 6.
ANOVA results for the sector work of health professionals.
When examining whether professionals hold management positions (Table 7), it is observed that there are no statistically significant differences in this regard. However, the average scores of professionals with management positions are higher than those without any management role: “Attraction to policy participation” (M = 4.43; SD = 0.49), “Commitment to public values” (M = 4.83; SD = 0.34), “Compassion” (M = 4.74; SD = 0.41), and “Self-sacrifice” (M = 3.63; SD = 0.88).

Table 7.
T-Test results for the managerial positions of health professionals.
5. Discussion
The primary objective of our study was to explore PSM variations among health professionals in Portugal according to different sociodemographic variables. The results offer significant insights for future studies that employ a qualitative approach for a more comprehensive analysis of each variable. Additionally, these findings can inform the design of practical measures to strengthen evidence-based policy formulation.
We validated H1: “Older health professionals have higher levels of public service motivation”, aligning with existing research (Camilleri 2007; Vandenabeele 2011), confirming age as associated to of higher PSM levels, with younger health professionals showing lower averages across all dimensions compared to their older counterparts. These findings echo previous studies indicating that older workers prioritize commitment to public values (CPV) as they age, while the need for compassion and self-sacrifice tends to decrease with age (Camilleri 2007; Naff and Crum 1999).
In the study by (Ciezar-Andersen and King-Shier 2021), with a sample of nurses, “self-sacrifice” is portrayed as a hallmark of an “ideal nurse” who prioritizes patient care. Younger nurses, however, appeared less inclined to justify self-sacrifice based on external expectations, prioritizing personal well-being over workplace commitment, contrasting with older professionals. Similarly, the study by Forte et al. (2022) with local government workers in Portugal revealed significant differences in CPV and self-sacrifice (SS) dimensions, particularly among workers over 55 years old, in line with our findings. The challenges faced by younger professionals in terms of CPV may reflect serious job market challenges and limited employment opportunities, particularly for young people, exacerbated by the slow post-crisis recovery, especially in the labor market (Sum et al. 2014).
H2: “Female health professionals have higher levels of public service motivation”, was also confirmed, with female healthcare professionals scoring higher in PSM levels than males, except for the SS dimension. DeHart-Davis et al. (2006), found that women score higher than men on measures of compassion and attraction to public policymaking, although the researchers did not find any significant differences between genders on dimensions of commitment to public service. However, in our study, significant differences were observed in the CPV dimension, consistent with previous studies. Further analysis of the CPV dimension underscores disparities in the perception of equal opportunities between genders, highlighting the need for additional research to explore the gender neutrality of CPV. The higher scores among women in attraction to policy participation (APP) are both surprising and intriguing, contradicting the notion of policy making as a defining characteristic of masculinity (DiStefano 2023).
H3: “Health professionals with higher levels of education have higher levels of public service motivation” remains inconclusive due to data limitations. While our study presents disparate averages across different education levels, significant differences were observed in the CPV dimension, aligning with prior research (Bright 2005; Forte et al. 2022; Vandenabeele 2011; Naff and Crum 1999). Similarly, (Perry 1997) and (Moynihan and Pandey 2005) found positive relationships between education and CPV, corroborating our findings. It is important to bear in mind that health professionals are usually highly qualified, and their training requires them to complete a series of educational levels (in the case of doctors, all graduates have a master’s degree), making comparisons less conclusive in this case. However, it is worth underlining that graduate students (likely nurses, for the reasons stated before) score higher in the self-sacrifice dimension, possibly due to the current crisis that the Portuguese NHS is experiencing.
Regarding H4: “Health professionals with management positions have higher levels of public service motivation when compared to non-managers”, although statistically insignificant, professionals in management positions demonstrated higher averages. While inconclusive, our results resonate with existing research indicating a positive relationship between professional management and PSM (Bright 2005). Further studies are also inconclusive, but still with results showing that managers score higher in compassion (COM) and SS (Desmarais and Gamassou 2014).
Our results partially align with existing literature regarding the impact of occupying higher hierarchical positions, which offer greater influence over decision making and contribute to the provision of more effective and efficient public services, thereby increasing PSM levels (Ballart and Ripoll 2023).
Analyses were conducted on the type of sector where health professionals work, but the small sample size in the private sector limits our ability to draw conclusions. While it was expected that professionals in the public sector would exhibit higher PSM levels compared to those in the private sector (Kim and Vandenabeele 2010; Naff and Crum 1999; Stivers 1995), our study’s findings are consistent with this notion, although some studies suggest that these differences may not be straightforward, with a greater emphasis on the CPV dimension (McCarthy et al. 2021).
(Andersen et al. 2011) investigated the influence of PSM on professionals and their performance in a sample of 24 public and private healthcare professionals in Denmark. PSM was at the same high level for public and private healthcare professionals, hence not affecting performance, which varied according to professional standards and economic incentives. However, comparing public professionals with those in private organizations using PSM measurements can be challenging due to the inclusion of items that may be irrelevant to professionals in private settings (Perry 1996; Jacobsen 2021). Although PSM includes more altruistic motives, such as self-sacrifice, civic duty or compassion (clearly intrinsic factors/intrinsic motivation), which, as a rule, health professionals show regardless of their sector of activity health professionals from the private sector value more extrinsic factors (e.g., salary, working conditions) (Fernandes et al. 2022; Perry et al. 2010).
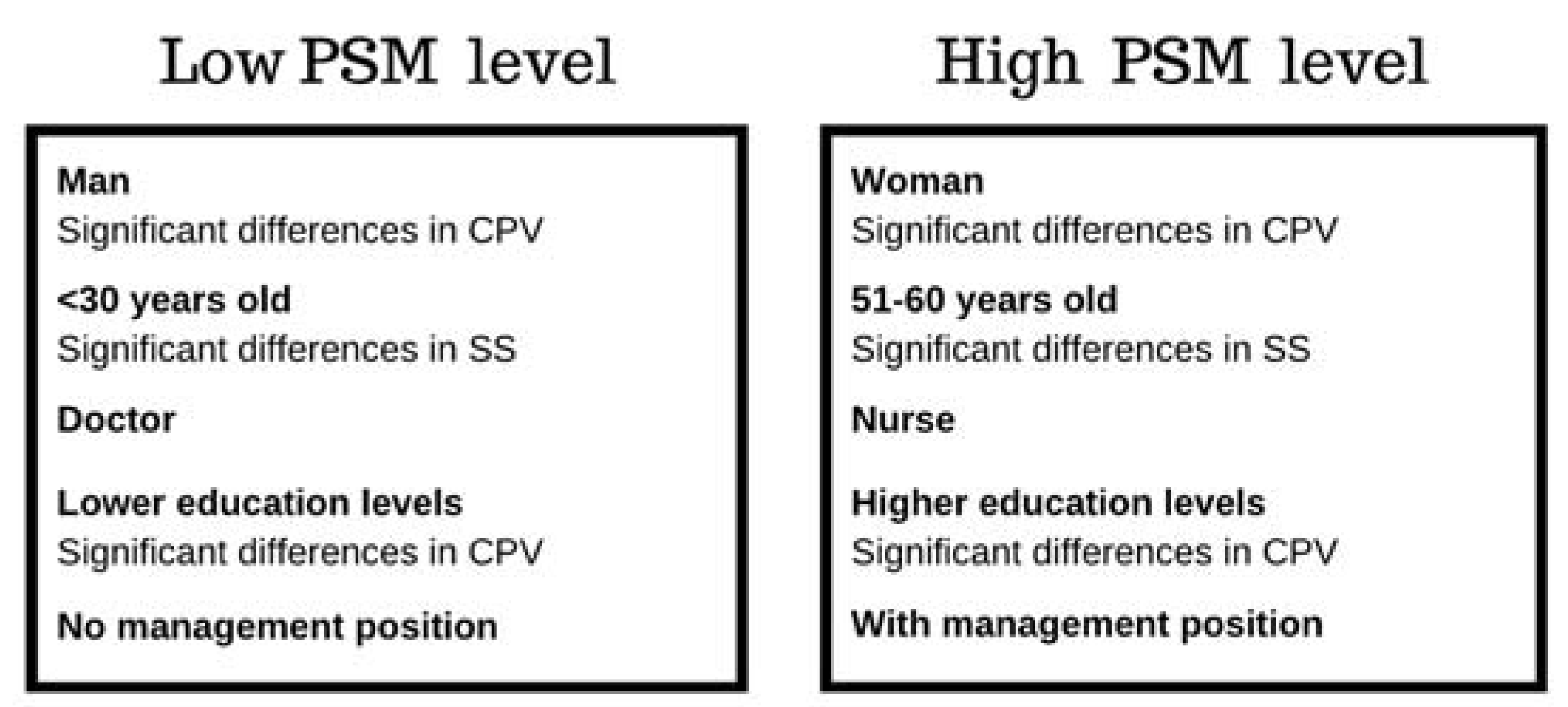
This study sheds light on the profile of the Portuguese health professionals, particularly doctors and nurses, regarding levels of public service motivation (PSM). In the analyzed sample (nurses—female n = 257, male n = 46; and doctors—female n = 82; male n = 28), it is evident that women, nurses, healthcare professionals aged between 51 and 60 years, postgraduates or individuals with higher levels of education, and those in management positions exhibit higher levels of PSM. Conversely, men, doctors, healthcare professionals under 30 years of age, with lower levels of education, and lacking management positions demonstrate lower PSM levels. Figure 1 summarizes these profiles.
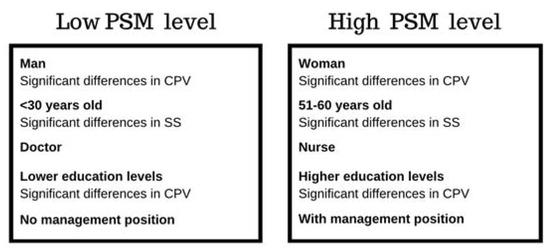
Figure 1.
PSM level in doctors and nurses in Portugal (persona type)—own elaboration based on this study.
Overall, despite the limitations in generalizing to all health professionals in this context, the results of our study indicate that healthcare professionals (doctors and nurses) in Portugal still exhibit high levels of PSM. This is noteworthy considering structural ongoing challenges such as low wages, excessive working hours, an aging workforce, difficulties in recruiting and retaining new professionals, and pandemic-related fatigue. However, the SS dimension received the lowest scores among various sociodemographic antecedents, suggesting that current circumstances may indeed have impacted professionals’ disposition of self-sacrifice. While healthcare professionals strive to deliver optimal patient care with available resources, the pandemic period has posed significant challenges. Additionally, several factors, particularly those related to the design of public health policies, may contribute to some of the observed results, such as low salaries, resource shortages, and absenteeism (Fernandes et al. 2022). On the other hand, recognition and appreciation of their work by supervisors and patients are universally recognized as significant, particularly in environments with fewer resources.
Given that the quality, effectiveness, and efficiency of healthcare services heavily rely on the motivation of health professionals, it is crucial to consider this aspect in health policymaking (Temesgen et al. 2016). The findings of this study hold relevance in the Portuguese context, which grapples with numerous challenges in managing human resources in healthcare, especially in retaining professionals in the public health sector (Nova SBE 2022). Therefore, understanding the factors that motivate health professionals is paramount. Identifying strategies to retain health professionals working in the public health sector is vital, especially in a demographic context that places strain on healthcare systems, many of which lack adequate human and physical resources.
6. Conclusions
In this study, we explored variances in public service motivation (PSM) in the Portuguese context, within public healthcare services. Understanding PSM is crucial as it can significantly impact the attraction to and retention of healthcare professionals in public healthcare services and their commitment to existing conditions.
In the context of the Portuguese NHS, improving the effectiveness of human resources management in health is essential to overcome some of the complex challenges it faces today, such as the scarcity of resources and the growing demand for clinical services, related in part to the marked aging of our population and problems with access to healthcare.
PSM was assessed using a universal scale developed by Kim et al. (2013), adapted from (Perry 1996) version, marking the first application of this scale within the Portuguese healthcare context, specifically among doctors and nurses. Our analysis revealed that PSM tends to be higher among more experienced healthcare professionals and females. While the presence of a management position did not yield statistically significant results, it hinted at higher PSM levels among professionals in such roles. However, contrary to existing literature, educational levels did not seem to be directly linked to PSM levels.
Our findings suggest that the workers with the lowest levels of motivation for public service are doctors under 30 years old. This result is coherent with the aging of this class within the NHS, where half of the specialist doctors are over 61 years old, and the recent mediatic attention to the choice made by recently graduated doctors for the private sector or emigrating to other countries.
The main results presented in this article may inform a more attuned public administration theory of public service motivation (PSM), particularly regarding the role of specific antecedents in relation to PSM. Motivation for public service can vary across different career stages, but it is crucial to recognize that values like self-sacrifice and altruism, which are already declining among younger professionals, cannot be sustained in isolation and require improved working conditions. As the literature indicates, extrinsic factors also play a significant role, prompting a timely reevaluation of policies aimed at enhancing the value and representation of public service to attract and retain professionals.
The findings from this study have several practical implications for policymakers and administrators within the Portuguese NHS. First, understanding the determinants of PSM can support the design of targeted interventions to enhance the motivation and retention of healthcare professionals, particularly younger medical doctors who exhibit lower levels of PSM. By addressing the specific needs and motivations of different demographic groups, the NHS can implement more effective human resource strategies, potentially reducing the emigration of newly graduated doctors and increasing the appeal of public healthcare careers. Additionally, the insights gained from this research can inform the development of policies that emphasize the importance of intrinsic rewards and improved working conditions, thereby fostering a more committed and motivated workforce. Practical steps such as mentorship programs, career development opportunities, and recognition of public service contributions could be instrumental in sustaining high levels of PSM.
While this study sheds light on several antecedents influencing PSM levels, it also highlights the need to further explore the retention and commitment of healthcare professionals in the Portuguese public healthcare sector. However, it is important to acknowledge the study’s limitations, including the omission of certain potential antecedents, such as religion, country of origin, or political spectrum. Additionally, the study lacks comprehensive comparisons between public and private services, an area that warrants attention in future research. In this regard, it would be interesting to have a higher number of respondents, which would allow to conduct further analyses.
Future studies should departure from these results and explore in depth their meaning to design more timely policies to retain health professionals in the public health sector, making it particularly attractive for young and future professionals.
Author Contributions
Conceptualization, A.F., G.S. and T.F.; methodology A.F., G.S. and T.F.; formal analysis, A.F., G.S. and T.F.; investigation, A.F., G.S. and T.F.; writing—original draft preparation, A.F., G.S. and T.F.; writing—review and editing, A.F., G.S. and T.F. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Fundação para a Ciência e Tecnologia, grant number 020.05144.BD, and partially funded by the Programa Operacional Centro 2020, through Fundo Social Europeu.
Institutional Review Board Statement
Procedures of this research comply with international standards of human research, in accordance with the Declaration of Helsinki, and were approved by the Ethics Committee of Clinical Academic Centre Egas Moniz Health Alliance (06-CE-ICVS/CAC-EMHA/20.04.2023) and all reference ethics committees from the different hospitals recruiting participants. All participants signed the informed consent and accepted their participation in the study.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Acknowledgments
Gonçalo Santinha would like to acknowledge the contribution of the research unit on Governance, Competitiveness, and Public Policies (UIDB/04058/2020) + (UIDP/04058/2020), funded by national funds through FCT—Portuguese Foundation for Science and Technology.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Translation of the original English version of PSM Kim Scale to Portuguese.
Table A1.
Translation of the original English version of PSM Kim Scale to Portuguese.
| Attraction to Public Participation | Atração pela Participação Pública |
|---|---|
| PSM1: I admire people who initiate or are involved in activities to aid my community | PSM1: Admiro pessoas que começam ou estão envolvidas em atividades de apoio à minha comunidade |
| PSM2: It is important to contribute to activities that tackle social problems | PSM2: Considero importante contribuir para atividades focadas em problemas sociais |
| PSM3: Meaningful public service is very important to me | PSM3: O serviço público é importante para mim |
| PSM4: It is important for me to contribute to the common good | PSM4: Contribuo para a minha comunidade sem esperar nada em retorno |
| Commitment to public values | Compromisso com os valores públicos |
| PSM5: I think equal opportunities for citizens are very important | PSM5: Considero que a igualdade de oportunidades para todos os cidadãos é muito importante |
| PSM5: It is important that citizens can rely on the continuous provision of public services | PSM 6: Acho importante que os cidadãos possam contar com a prestação contínua de serviços públicos |
| PSM7: It is fundamental that the interests of future generations are taken into account when developing public policies | PSM7: Considero fundamental que os interesses das gerações futuras sejam levados em consideração no desenvolvimento de políticas públicas |
| PSM8: To act ethically is essential for public servants | PSM8: Agir com ética é essencial para um bom serviço público |
| Compassion | Compaixão |
| PSM9: I feel sympathetic to the plight of the underprivileged | PSM9: Sinto-me solidário/a com a situação de pessoas em condições de vulnerabilidade |
| PSM10: I empathize with other people who face difficulties | PSM10: Sinto empatia por outras pessoas que enfrentam dificuldades |
| PSM11: I get very upset when I see other people being treated unfairly | PSM11: Perturba-me muito ver pessoas a ser alvo de injustiças |
| PSM12: Considering the welfare of others is very important | PSM12: Considero o bem-estar dos outros muito importante |
| Self-Sacrifice | Autossacrifício |
| PSM13: I am prepared to make sacrifices for the good of society | PSM13: Estou pronto/a para fazer sacríficos em prol da sociedade |
| PSM14: I believe in putting civic duty before self | PSM14: Acredito que o dever está acima das necessidades/vontades individuais |
| PSM15: I am willing to risk personal loss to help society | PSM15: Aceitaria perdas pessoais para ajudar a sociedade |
| PSM16: I would agree to a good plan to make a better life for the poor, even if it costs me money | PSM16: Concordaria com um bom plano que realmente ajudasse as pessoas em situações de vulnerabilidade, mesmo com custos pessoais |
Note
| 1 | The NHS has undergone several reforms, particularly since 2023. Regional Health Administrations (RHAs) will be abolished, giving way to Local Health Units, an organizational model that, within a geographic area, integrates primary and secondary healthcare in the same management structure. However, due to the very recent legislative elections leading to a new Government, it is uncertain whether there may be setbacks in these measures. |
References
- AlAbri, Ismail, and Rusinah Siron. 2020. Health Care Professional Attitude and Motivation During COVID-19: A Case of Health Sector of Oman. Systematic Reviews in Pharmacy 11: 1035–40. [Google Scholar] [CrossRef]
- Andersen, Bogh Lotte, Thomas Pallesen, and Lene Holm Pedersen. 2011. Does Ownership Matter? Public Service Motivation Among Physiotherapists in the Private and Public Sectors in Denmark. Review of Public Personnel Administration 31: 10–27. [Google Scholar] [CrossRef]
- Aninanya, Apiung, Natasha Howard, John Williams, Benjamin Apam, Helen Prytherch, Svetla Loukanova, Karanja Kamara, and Easmon Otupiri. 2016. Can Performance-Based Incentives Improve Motivation of Nurses and Midwives in Primary Facilities in Northern Ghana? A Quasi-Experimental Study. Global Health Action 9: 32404. [Google Scholar] [CrossRef] [PubMed]
- Ballart, Xavier, and Guillem Ripoll. 2023. Transformational Leadership, Basic Needs Satisfaction and Public Service Motivation: Evidence from Social Workers in Catalonia. International Journal of Public Administration 47: 820–30. [Google Scholar] [CrossRef]
- Bansal, Ravinder, and Meenakshi Malhotra. 2016. A Case Study of Motivational Levels among Personnel Working in a Government Teaching Hospital of Punjab. Biomedicine and Pharmacology Journal 9: 585–91. [Google Scholar] [CrossRef]
- Belrhiti, Zakaria, Wim Van Damme, Abdelmounim Belalia, and Bruno Marchal. 2019. Does Public Service Motivation Matter in Moroccan Public Hospitals? A Multiple Embedded Case Study. International Journal for Equity in Health 18: 160. [Google Scholar] [CrossRef] [PubMed]
- Brewer, Gene, and Sally Selden. 1998. Whistle Blowers in the Federal Civil Service: New Evidence of the Public Service Ethic. Journal of Public Administration Research and Theory 8: 413–39. [Google Scholar] [CrossRef]
- Bridgeman, Patrick, Mary Bridgeman, and Joseph Barone. 2018. Burnout Syndrome among Healthcare Professionals. American Journal of Health-System Pharmacy 75: 147–52. [Google Scholar] [CrossRef]
- Bright, Leonard. 2005. Public Employees with High Levels of Public Service Motivation: Who Are They, Where Are They, and What Do They Want? Review of Public Personnel Administration 25: 138–54. [Google Scholar] [CrossRef]
- Camilleri, Emanuel. 2007. Antecedents Affecting Public Service Motivation. Personnel Review 36: 356–77. [Google Scholar] [CrossRef]
- Campbell, Jim, Gilles Dussault, and James Buchan. 2014. A Universal Truth: No Health without a Workforce. Forum Report, Third Global Forum on Human Resources for Health. Geneva: Global Health Workforce Alliance and World Health Organization. [Google Scholar]
- Ciezar-Andersen, Sylwia, and Kathryn King-Shier. 2021. Detriments of a Self-Sacrificing Nursing Culture on Recruitment and Retention: A Qualitative Descriptive Study. Canadian Journal of Nursing Research 53: 233–41. [Google Scholar] [CrossRef] [PubMed]
- Coursey, David, and Sanjay Pandey. 2007. Public Service Motivation Measurement: Testing an Abridged Version of Perry’s Proposed Scale. Administration & Society 39: 547–68. [Google Scholar] [CrossRef]
- DeHart-Davis, Leisha, Justin Marlowe, and Sanjay Pandey. 2006. Gender Dimensions of Public Service Motivation. Public Administration Review 66: 873–87. [Google Scholar] [CrossRef]
- Desmarais, Céline, and Claire Gamassou. 2014. All Motivated by Public Service? The Links Between Hierarchical Position and Public Service Motivation. International Review of Administrative Sciences 80: 131–50. [Google Scholar] [CrossRef]
- Dieleman, Marjolein, Barend Gerretsen, and Gert Wilt. 2009. Human Resource Management Interventions to Improve Health Workers’ Performance in Low- and Middle-Income Countries: A Realist Review. Health Research Policy and Systems 7: 7. [Google Scholar] [CrossRef]
- DiStefano, Michelle. 2023. Bureau Men, Settlement Women: Constructing Public Administration in the Progressive Era. In Administrative Theory & Praxis. Oxfordshire: Tylor & Francis. [Google Scholar] [CrossRef]
- Fernandes, Alexandre, Gonçalo Santinha, and Teresa Forte. 2022. Public Service Motivation and Determining Factors to Attract and Retain Health Professionals in the Public Sector: A Systematic Review. Behavioral Sciences 12: 95. [Google Scholar] [CrossRef]
- Ferrinho, Paulo, Wim Van Lerberghe, Manuel Julien, Evelize Fresta, Aurélio Gomes, Francisco Dias, Aldina Gonçalves, and Bárbara Bäckström. 1998. How and Why Public Sector Doctors Engage in Private Practice in Portuguese-speaking African Countries. Health Policy and Planning 13: 332–38. [Google Scholar] [CrossRef]
- Forte, Teresa, Gonçalo Santinha, Mariana Oliveira, and Marta Patrão. 2022. The High Note of Meaning: A Case Study of Public Service Motivation of Local Government Officials. Social Sciences 11: 411. [Google Scholar] [CrossRef]
- Franco, Lynne, Sara Bennett, and Ruth Kanfer. 2002. Health Sector Reform and Public Sector Health Worker Motivation: A Conceptual Framework. Social Science & Medicine 54: 1255–66. [Google Scholar] [CrossRef]
- Gruening, Gernod. 2001. Origin and Theoretical Basis of New Public Management. International Public Management Journal 4: 1–25. [Google Scholar] [CrossRef]
- Herzberg, Frederick, Bernard Mausner, and Barbara Snyderman. 1959. The Motivation to Work, 2nd ed. Hoboken: Wiley. [Google Scholar]
- Humphrey, Charlotte, and Jill Russell. 2004. Motivation and Values of Hospital Consultants in South-East England Who Work in the National Health Service and Do Private Practice. Social Science & Medicine 59: 1241–50. [Google Scholar] [CrossRef]
- Jacobsen, Ingvar. 2021. Motivational Differences? Comparing Private, Public and Hybrid Organizations. Public Organization Review 21: 561–75. [Google Scholar] [CrossRef]
- Jensen, Ulrich, Lotte Andersen, and Christian Jacobsen. 2019. Only When We Agree! How Value Congruence Moderates the Impact of Goal-Oriented Leadership on Public Service Motivation. Public Administration Review 79: 12–24. [Google Scholar] [CrossRef]
- Julião, Rui, and Alexandre Nunes. 2019. Descentralização de Competências para as Autarquias Locais: O Caso do Setor da Saúde. Revista Portuguesa de Gestão e Saúde 27: 8. [Google Scholar]
- Kim, Sangmook. 2009. Testing the Structure of Public Service Motivation in Korea: A Research Note. Journal of Public Administration Research and Theory 19: 839–51. [Google Scholar] [CrossRef]
- Kim, Sangmook. 2016. Job Characteristics, Public Service Motivation, and Work Performance in Korea. Gestion et Management Public 5: 7–24. [Google Scholar] [CrossRef]
- Kim, Sangmook. 2021. Partial Metric Invariance of the International Measure of Public Service Motivation among Twelve Countries: A Research Note. International Journal of Public Administration 45: 1103–9. [Google Scholar] [CrossRef]
- Kim, Sangmook, and Wouter Vandenabeele. 2010. A Strategy for Building Public Service Motivation Research Internationally. Public Administration Review 70: 701–9. [Google Scholar] [CrossRef]
- Kim, Sangmook, Wouter Vandenabeele, Bradley Wright, Lotte Andersen, Francesco Cerase, Robert Christensen, Céline Desmarais, Maria Koumenta, Peter Leisink, Bangcheng Liu, and et al. 2013. Investigating the Structure and Meaning of Public Service Motivation across Populations: Developing an International Instrument and Addressing Issues of Measurement Invariance. Journal of Public Administration Research and Theory 23: 79–102. [Google Scholar] [CrossRef]
- Kitsios, Fotis, and Maria Kamariotou. 2021. Job Satisfaction Behind Motivation: An Empirical Study in Public Health Workers. Heliyon 7: e06857. [Google Scholar] [CrossRef]
- Klijn, Erik-Hans. 2012. Public Management and Governance: A Comparison of Two Paradigms to Deal with Modern Complex Problems. In The Handbook of Governance. Edited by David Levi Faur. Oxford: Oxford University, pp. 201–14. [Google Scholar]
- Lee, Michael, and Robyn Raschke. 2016. Understanding Employee Motivation and Organizational Performance: Arguments for a Set-Theoretic Approach. Journal of Innovation & Knowledge 1: 162169. [Google Scholar] [CrossRef]
- Mazahir, Shama, and Shazia Khalid. 2017. Work Environment and Situational Motivation of Doctors in Public Sector Hospitals. Annals of King Edward Medical University 23: 1509. [Google Scholar] [CrossRef]
- Mbindyo, Patrick, Lucy Gilson, Duane Blaauw, and Mike English. 2009. Contextual Influences on Health Worker Motivation in District Hospitals in Kenya. Implementation Science 4: 43. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, Dermot, Ping Wei, Fabian Homberg, and Vurain Tabvuma. 2021. Public Service Motivation in the Chinese Public and Private Sectors. Evidence-Based HRM 9: 1–17. [Google Scholar] [CrossRef]
- Moynihan, Donald, and Sanjay Pandey. 2005. The Role of Organizations in Fostering Public Service Motivation. College Station: The Bush School of Government & Public Service, Texas A&M University. [Google Scholar]
- Naff, Katherine, and John Crum. 1999. Working for America: Does Public Service Motivation Make a Difference? Review of Public Personnel Administration 19: 5–16. [Google Scholar] [CrossRef]
- Nova SBE. 2022. Recursos Humanos em Saúde: Relatório 2022. Edited by Pedro Barros and Eduardo Costa. Available online: https://www.novasbe.unl.pt/Portals/0/Files/Social%20Equity%20Initiative/Nova%20SBE_KC%20Health_Recursos%20Humanos_2022.pdf (accessed on 15 May 2024).
- Nunes, Alexandre, and Diogo Ferreira. 2023. Evaluating Portuguese Public Hospitals Performance: Any Difference Before and During COVID-19? Sustainability 15: 294. [Google Scholar] [CrossRef]
- OECD. 2023. Health at a Glance 2023: OECD Indicators. Paris: OECD Publishing. [Google Scholar] [CrossRef]
- O’Riordan, Joanna. 2013. Public Service Motivation: State of Public Service Series. Dublin: Institute of Public Administration, pp. 1–36. [Google Scholar]
- Pandey, Sanjay, and Edmund Stazyk. 2008. Antecedents and Correlates of Public Service Motivation. In Motivation in Public Management: The Call of Public Service. Edited by James Perry and Annie Hondeghem. Oxford: Oxford University Press, pp. 101–17. [Google Scholar]
- Parola, Heather, Harari Michael, Herst David, and Prysmakova Palina. 2019. Demographic Determinants of Public Service Motivation: A Meta-Analysis of PSM-Age and -Gender Relationships. Public Management Review 21: 1397–419. [Google Scholar] [CrossRef]
- Perry, James. 1996. Measuring Public Service Motivation: An Assessment of Construct Reliability and Validity. Journal of Public Administration Research and Theory 6: 5–22. [Google Scholar] [CrossRef]
- Perry, James. 1997. Antecedents of Public Service Motivation. Journal of Public Administration Research and Theory 7: 181–97. [Google Scholar] [CrossRef]
- Perry, James, and Lois Wise. 1990. The Motivational Bases of Public Service. Public Administration Review 50: 367–73. [Google Scholar] [CrossRef]
- Perry, James, and Wouter Vandenabeele. 2008. Behavioral Dynamics: Institutions, Identities, and Self-Regulation. In Motivation in Public Management: The Call of Public Service. Edited by James Perry and Annie Hondeghem. Oxford: Oxford Academic. [Google Scholar] [CrossRef]
- Perry, James, and Wouter Vandenabeele. 2015. Public Service Motivation Research: Achievements, Challenges, and Future Directions. Public Administration Review 75: 692–99. [Google Scholar] [CrossRef]
- Perry, James, Hondeghem Annie, and Lois Wise. 2010. Revisiting the Motivational Bases of Public Service: Twenty Years of Research and an Agenda for the Future. Public Administration Review 70: 681–90. [Google Scholar] [CrossRef]
- PlanAPP. 2023. Planeamento de Recursos Humanos em Saúde—Radiografia dos Instrumentos de Planeamento; Lisbon: Coleção Profissionais de Saúde, p. 2. Available online: https://www.planapp.gov.pt/wp-content/uploads/2024/03/PlanAPP_PlaneamentoRHS.pdf (accessed on 15 May 2024).
- PlanAPP. 2024. Os Profissionais do SNS: Retrato e Evolução; Lisbon: Coleção Profissionais de Saúde, p. 1. Available online: https://www.planapp.gov.pt/wp-content/uploads/2024/03/PlanAPP_ProfissionaisSNS-2.pdf (accessed on 15 May 2024).
- Rainey, Hal, and Paula Steinbauer. 1999. Galloping Elephants: Developing Elements of a Theory of Effective Government Organizations. Journal of Public Administration Research and Theory 9: 1–32. [Google Scholar] [CrossRef]
- Ritz, Adrian. 2011. Attraction to Public Policy Making: A Qualitative Inquiry into Improvements in PSM Measurement. Public Administration 89: 1128–47. [Google Scholar] [CrossRef]
- Santinha, Gonçalo. 2016. Governance for Health: Is the Cultural ‘Lone Ranger’ Behaviour Still Prevailing? Perspectives from Policy-Makers in Portugal. Public Policy and Administration 31: 147–68. [Google Scholar] [CrossRef]
- Santinha, Gonçalo, Alexandre Fernandes, Rafaela Oliveira, and Nelson Pacheco Rocha. 2023. Designing a Health Strategy at Local Level: A Conceptual Framework for Local Governments. International Journal of Environmental Research and Public Health 13: 6250. [Google Scholar] [CrossRef] [PubMed]
- Schott, Carina, and Jan Pronk. 2014. Investigating and Explaining Organizational Antecedents of PSM. Evidence-Based HRM: A Global Forum for Empirical Scholarship 2: 28–56. [Google Scholar] [CrossRef]
- Simões, Jorge. 2009. Tendências Internacionais nas Políticas Públicas de Saúde. Janus 22: 1–7. Available online: https://www.janusonline.pt/arquivo/2009/2009_2_2.html (accessed on 17 July 2024).
- Stefurak, Tres, Ron Morgan, and Burke Johnson. 2020. The Relationship of Public Service Motivation to Job Satisfaction and Job Performance of Emergency Medical Services Professionals. Public Personnel Management 49: 590–616. [Google Scholar] [CrossRef]
- Stivers, Camilla. 1995. Settlement Women and Bureau Men: Constructing a Usable Past for Public Administration. Public Administration Review 55: 522–29. [Google Scholar] [CrossRef]
- Sum, Andrew, Ishwar Khatiwada, Mykhaylo Trubskyy, and Sheila Palma. 2014. The Plummeting Labor Market Fortunes of Teens and Young Adults. Washington: The Brookings Institution. [Google Scholar]
- Tavares, Jéssica, Gonçalo Santinha, and Nelson Rocha. 2023. Implementation of the World Health Organization Age-Friendly Principles: A Case Study from Portugal. International Journal of Environmental Research and Public Health 20: 6532. [Google Scholar] [CrossRef] [PubMed]
- Taylor, Jeannette. 2007. The Impact of Public Service Motives on Work Outcomes in Australia: A Comparative Multi-Dimensional Analysis. Public Administration 85: 931–59. [Google Scholar] [CrossRef]
- Temesgen, Wayuma, Yohannes Ejigu, Fitsum Weldegebreal, and Mirkuzie Woldie. 2016. Motivation of Health Workers and Associated Factors in Public Hospitals of West Amhara, Northwest Ethiopia. Patient Preference and Adherence 10: 159–69. [Google Scholar] [CrossRef]
- Vandenabeele, Wouter. 2007. Toward a Public Administration Theory of Public Service Motivation. Public Management Review 9: 545–56. [Google Scholar] [CrossRef]
- Vandenabeele, Wouter. 2011. Who Wants to Deliver Public Service? Do Institutional Antecedents of Public Service Motivation Provide an Answer? Review of Public Personnel Administration 31: 87–107. [Google Scholar] [CrossRef]
- Wang, Hui, Yu Liu, Kaili Hu, Meng Zhang, Meichen Du, Haishan Huang, and Xiao Yue. 2020a. Healthcare Workers’ Stress When Caring for COVID-19 Patients: An Altruistic Perspective. Nursing Ethics 27: 1490–500. [Google Scholar] [CrossRef]
- Wang, Tse-Min, Arjen van Witteloostuijn, and Florian Heine. 2020b. A Moral Theory of Public Service Motivation. Frontiers in Psychology 11: 517763. [Google Scholar] [CrossRef]
- Waterhouse, Jennifer. 2008. Motivation in Public Management: The Call of Public Service edited by James L. Perry and Annie Hondeghem. Australian Journal of Public Administration 67: 505–7. [Google Scholar] [CrossRef]
- Windarwati, Dwi, Niken Ati, Deka Paraswati, Khaqul Ilmy, Ahmad Supianto, Fahrul Rizzal, Dwi Sulaksono, Retno Lestari, and Lilik Supriati. 2021. Stressor, Coping Mechanism, and Motivation among Health Care Workers in Dealing with Stress Due to the COVID-19 Pandemic in Indonesia. Asian Journal of Psychiatry 56: 102470. [Google Scholar] [CrossRef]
- World Health Organization. 2017. A Health Policy and Systems Research Reader on Human Resources for Health. Edited by Asha George, Kerry Scott and Veloshnee Govender. Geneva: World Health Organisation. [Google Scholar]
- Wright, Bradley E. 2008. Methodological Challenges Associated with Public Service Motivation Research. In Motivation in Public Management. Edited by James L. Perry and Annie Hondeghem. Oxford: Oxford University Press, pp. 80–98. [Google Scholar]
- Zhang, Hongming, Qingya Zhang, Guoliang Huang, Jin Ke, Ni Zhao, Wanting Huang, and Jun Zhang. 2022. Analysis of Evaluation Dimensions of Public Service Motivation of Chinese College Students-Qualitative Study Based on Grounded Theory. International Journal of Environmental Research and Public Health 19: 15084. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).