Ultrasound-Guided Percutaneous Neuromodulation in Patients with Unilateral Anterior Knee Pain: A Randomized Clinical Trial
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Clinical Assessment
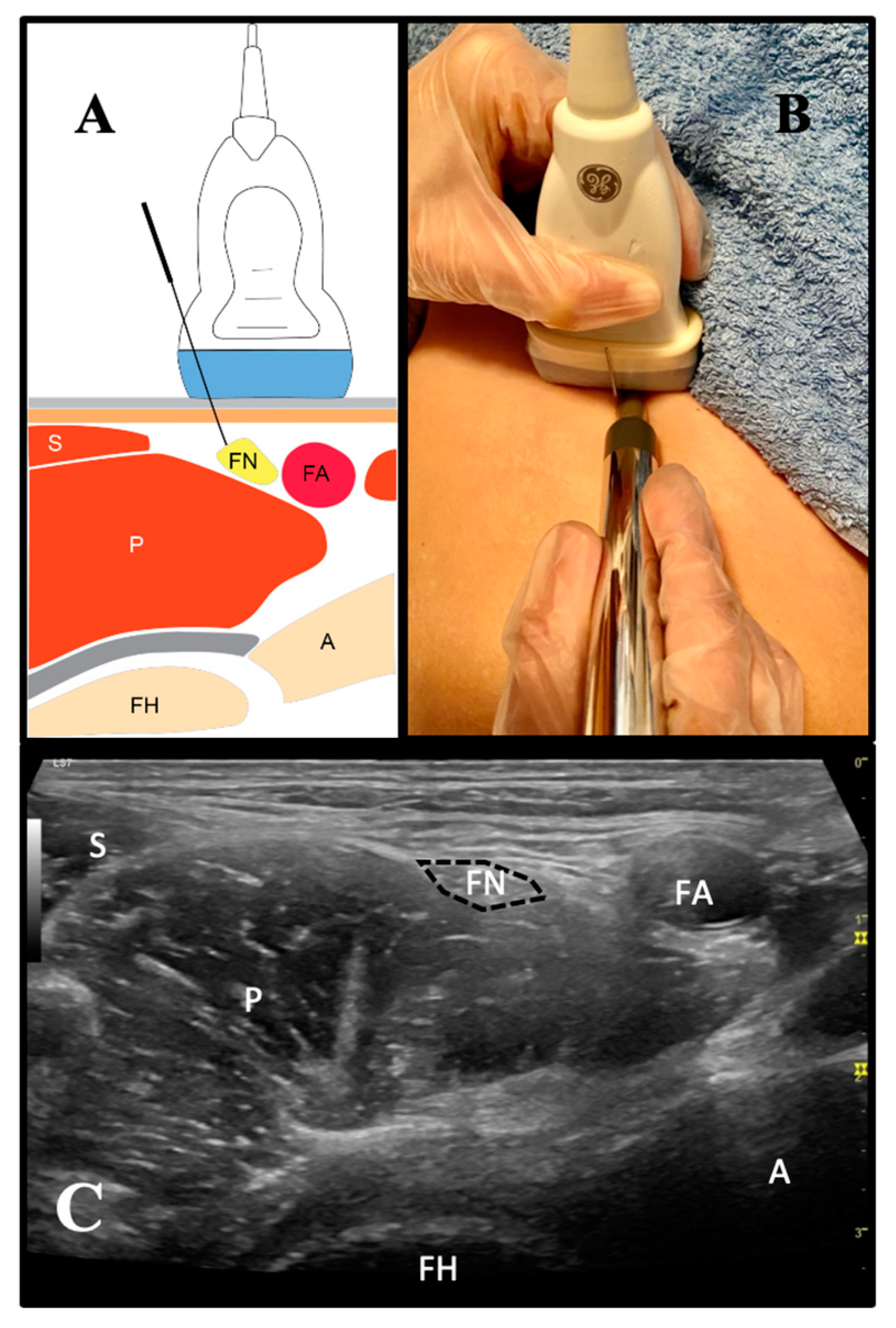
2.3. Ultrasound-Guided Percutaneous Neuromodulation Intervention
2.4. Sample Size Calculation
2.5. Data Analysis
3. Results
4. Discussion
Clinical Relevance
- US-guided PNM may be an effective therapeutic procedure for patients with AKP;
- US-guided PNM causes not only a local effect on the target tissue, but also a distal effect (in this case, a crossover effect);
- One single-shot PNM intervention per week may be enough.
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sanchís-Alfonso, V. Holistic approach to understanding anterior knee pain. Clinical implications. Knee Surg Sports Traumatol. Arthrosc. 2014, 22, 2275–2285. [Google Scholar] [PubMed]
- Fairbank, J.; Pynsent, P.; Van Poortvliet, J.; Phillips, H. Mechanical factors in the incidence of knee pain in adolescents and young adults. J. Bone Jt. Surg. Br. 1984, 66, 685–693. [Google Scholar] [CrossRef] [Green Version]
- Goldberg, B. Chronic anterior knee pain in the adolescent. Pediatr. Ann. 1991, 20, 186–187. [Google Scholar] [CrossRef] [PubMed]
- Gunther, K.P.; Thielemann, F.; Bottesi, M. Anterior knee pain in children and adolescents: Diagnosis and conservative treatment. Orthopade 2003, 32, 110–118. [Google Scholar]
- Sanchis-Alfonso, V.; Dye, S.F. How to deal with anterior knee pain in the active young patient. Sports Health 2017, 9, 346–351. [Google Scholar] [CrossRef]
- Rodríguez-Fernández, A.L.; Rebollo-Roldán, J.; Jiménez-Rejano, J.J.; Güeita-Rodríguez, J. Strength-Duration curves of the common fibular nerve show hypoexcitability in people with functional ankle instability. PM&R 2016, 8, 536–544. [Google Scholar]
- De-la-Cruz-Torres, B. Strength-duration curve of radial nerve in patients with lateral elbow pain. J. Sport Rehabil. 2019, 18, 1–6. [Google Scholar] [CrossRef]
- Sanchis-Alfonso, V.; Roselló-Sastre, E. Anterior knee pain in the young patient-what causes the pain? “Neural model”. Acta Orthop. Scand. 2003, 74, 697–703. [Google Scholar] [CrossRef] [Green Version]
- Lin, P.L.; Shih, Y.F.; Chen, W.Y.; Ma, H.L. Neurodynamic responses to the femoral slump test in patients with anterior knee pain syndrome. J. Orthop. Sports Phys. Ther. 2014, 44, 350–357. [Google Scholar] [CrossRef] [Green Version]
- Wall, P.; Sweet, W. Temporary abolition of pain in man. Science 1967, 155, 108–109. [Google Scholar] [CrossRef]
- Ilfeld, B.M.; Gilmore, C.A.; Grant, S.A.; Bolognesi, M.P.; Del Gaizo, D.J.; Wongsarnpigoon, A.; Boggs, J.W. Ultrasound-guided percutaneous peripheral nerve stimulation for analgesiafollowing total knee arthroplasty: A prospective feasibility study. J. Orthop. Surg. Res. 2017, 12, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ilfeld, B.M.; Said, E.T.; Finneran, J.J.; Sztain, J.F., IV; Abramson, W.B.; Gabriel, R.A.; Khatibi, B.; Swisher, M.W.; Jaeger, P.; Covey, D.C.; et al. Ultrasound-Guided Percutaneous Peripheral Nerve Stimulation: Neuromodulation of the Femoral Nerve for Postoperative Analgesia Following Ambulatory Anterior Cruciate Ligament Reconstruction: A Proof of Concept Study. Neuromodulation 2019, 22, 621–629. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valera-Garrido, F.; Minaya-Muñoz, F. Fisioterapia Invasiva; Elsevier SL: Barcelona, España, 2016. [Google Scholar]
- García-Bermejo, P.; Romero-Morales, C.; De-la-Cruz-Torres, B. Effect of ultrasound-guided percutaneous neuromodulation on the femoral nerve on pain and range of motion in patients with anterior knee pain: Case studies. Rev. Fisioter. Invasiva 2020, 3, 30–34. [Google Scholar]
- Álvarez-Plats, D.; Carvajal-Fernández, O.; Pérez-Mellada, N.; Minaya-Muñoz, F. Changes in Maximal Isometric Quadriceps Strength after the Application of Ultrasound-Guided Percutaneous Neuromodulation of the Femoral Nerve: A Case Series. Rev. Fisioter. Invasiva 2019, 2, 39–45. [Google Scholar]
- Chaouachi, A.; Padulo, J.; Kasmi, S.; Othmen, A.B.; Chatra, M.; Behm, D.G. Unilateral static and dynamic hamstrings stretching increases contralateral hip flexion range of motion. Clin. Physiol. Funct. Imaging 2017, 37, 23–29. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Killen, B.S.; Zelizney, K.L.; Ye, X. Crossover effects of unilateral static stretching and foam rolling on contralateral hamstring flexibility and strength. J. Sport Rehabil. 2018, 15, 1–27. [Google Scholar] [CrossRef]
- Halperin, I.; Copithorne, D.; Behm, D.G. Unilateral isometric muscle fatigue decreases force production and activation of contralateral knee extensors but not elbow flexors. Appl. Physiol. Nutr. Metab. 2014, 39, 1338–1344. [Google Scholar] [CrossRef]
- Kawamoto, J.A.; Abbodarda, S.J.; Behm, D.G. Effect of differing intensities of fatiguing dynamic contractions on contralateral homologous muscle performance. J. Sport Sci. Med. 2014, 13, 836–845. [Google Scholar]
- Regueme, S.C.; Barthelemy, J.; Nicol, C. Exhaustive stretch-shortening cycle exercise: No contralateral effects on muscle activity in maximal motor performances. Scand. J. Med. Sci. Sports 2007, 17, 547–555. [Google Scholar] [CrossRef]
- De-la-Cruz-Torres, B.; Minaya-Muñoz, F.; Romero-Morales, C. Crossover effects of ultrasound-guided percutaneous neuromodulation on controlateral hamstring flexibility. Acupunct. Med. 2020, 0964528420920283. [Google Scholar]
- Brosseau, L.; Balmer, S.; Tousignant, M.; O’Sullivan, J.P.; Goudreault, C.; Goudreault, M.; Gringras, S. Intra-and intertester reliability and criterion validity of the parallelogram and universal goniometers for measuring maximum active knee flexion and extension of patients with knee restrictions. Arch. Phys. Med. Rehabil. 2001, 82, 396–402. [Google Scholar] [CrossRef] [PubMed]
- Norkin, C.C.; White, D.J. Measurement of Joint Motion: A Guide to Goniometry, 4th ed.; publisher Davis, F.A.: Philadelphia, PA, USA, 2016. [Google Scholar]
- Hernandez-Sanchez, S.; Hidalgo, M.D.; Gomez, A. Cross-cultural adaptation of VISA-P score for patellar tendinopathy in Spanish population. J. Orthop. Sports Phys. Ther. 2011, 41, 581–591. [Google Scholar] [CrossRef] [PubMed]
- Visentini, P.J.; Khan, K.M.; Cook, J.L.; Kiss, Z.S.; Harcourt, P.R.; Wark, J.D. The VISA score: An index of severity of symptoms in patients with jumper’s knee (patellar tendinosis). J. Sci. Med. Sport 1998, 1, 22–28. [Google Scholar] [CrossRef]
- Gil-Gámez, J.; Pecos-Martín, D.; Kujala, U.M.; Martínez-Merinero, P.; Montañez-Aguilera, F.J.; Romero-Franco, N.; Gallego-Izquierdo, T. Validation and cultural adaptation of “Kujala Score” in Spanish. Knee Surg. Sports Traumatol. Arthrosc. 2016, 24, 2845–2853. [Google Scholar] [CrossRef]
- Negahban, H.; Pouretezad, M.; Yazdi, M.J.S. Persian translation and validation of the Kujala Patellofemoral Scale in patients with patellofemoral pain syndrome. Disabil. Rehabil. 2012, 34, 2259–2263. [Google Scholar] [CrossRef]
- De-la-Cruz-Torres, B.; Barrera-García-Martín, I.; Romero-Morales, C. Comparative effects of one-shot electrical stimulation on performance of the flexor hallucis longus muscle in professional dancers: Percutaneous versus transcutaneous? Neuromodulation 2019, in press. [Google Scholar] [CrossRef]
- Hassenbusch, S.J.; Stanton-Hicks, M.; Schoppa, D.; Walsh, J.G.; Covington, E.C. Long-term results of peripheral nerve stimulation for reflex sympathetic dystrophy. J. Neurosurg. 1996, 84, 415–423. [Google Scholar] [CrossRef] [Green Version]
- Picaza, J.A.; Hunter, S.E.; Cannon, B.W. Pain suppression by peripheral nerve stimulation. Chronic effects of implanted devices. Appl. Neurophysiol. 1977, 40, 223–234. [Google Scholar]
- Rakel, B.A.; Zimmerman, M.B.; Geasland, K.; Embree, J.; Clark, C.R.; Noiseux, N.O.; Callaghan, J.J.; Herr, K.; Walsh, D.; Sluka, K.A. Transcutaneous electrical nerve stimulation for the control of pain during rehabilitation after total knee arthroplasty: A randomized, blinded, placebo-controlled trial. PAIN® 2014, 155, 2599–2611. [Google Scholar] [CrossRef] [Green Version]
- Ferreira-Dos-Santos, G.; Hurdle, M.F.B.; Gupta, S.; Clendenen, S.R. Ultrasound-guided percutaneous peripheral nerve stimulation for the treatment of lower extremity pain: A rare case report. Pain Pract. 2019, 19, 861–865. [Google Scholar] [CrossRef]
- Gilmore, C.; Ilfeld, B.; Rosenow, J.; Li, S.; Desai, M.; Hunter, C.; Rauck, R.; Kapural, L.; Nader, A.; Mak, J.; et al. Percutaneous peripheral nerve stimulation for the treatment of chronic neuropathic postamputation pain: A multicenter, randomized, placebo-controlled trial. Reg. Anesth. Pain Med. 2019, 44, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Gilmore, C.A.; Kapural, L.; McGee, M.J.; Boggs, J.W. Percutaneous Peripheral Nerve Stimulation (PNS) for the Treatment of Chronic Low Back Pain Provides Sustained Relief. Neuromodulation 2019, 22, 615–620. [Google Scholar] [CrossRef] [PubMed]
- Arias-Buría, J.L.; Cleland, J.A.; El Bachiri, Y.R.; Plaza-Manzano, G.; Fernández-de-Las-Peñas, C. Ultrasound-guided percutaneous electrical nerve stimulation of the radial nerve for a patient with lateral elbow pain: A case report with a 2-year follow-up. J. Orthop. Sports Phys. Ther. 2019, 49, 347–354. [Google Scholar] [CrossRef] [PubMed]
- De-la-Cruz-Torres, B. Ultrasound-guided percutaneous neuromodulation in patients with unilateral refractory lateral epycondilitis. J. Manip. Physiol. Ther. 2019, in press. [Google Scholar]
- De-la-Cruz-Torres, B.; Barrera-García-Martín, I.; Albornoz-Cabello, M. Immediate effects of ultrasound-guided percutaneous neuromodulation versus physical exercise on performance of the flexor hallucis longus muscle in professional dancers: A randomised clinical trial. Acupunct. Med. 2019, 37, 91–97. [Google Scholar] [CrossRef]

| Data | Asymptomatic Knee Group (n = 15) | Symptomatic Knee Group (n = 15) | p-Value |
|---|---|---|---|
| Age (years) | 37.0 ± 9.6 | 39.3 ± 9.5 | 0.52 |
| Weight (kg) | 71.7 ± 8.9 | 65.6 ± 9.5 | 0.09 |
| Height (m) | 1.68 ± 0.09 | 1.65 ± 0.06 | 0.30 |
| BMI (kg/m2) | 25.5 ± 3.5 | 24.0 ± 2.7 | 0.26 |
| Injury time (months) | 7.0 ± 2.6 | 7.2 ± 2.7 | 0.82 |
| Gender (F/M) | 11/4 | 10/5 | N/A |
| Dominance side (R/L) | 14/1 | 12/3 | N/A |
| Pathological side (R/L) | 13/2 | 12/3 | N/A |
| ROM (o) | 129.0 ±11.70 | 133.5 ± 6.4 | 0.228 |
| NRS | 56.4 ± 14.56 | 56.9 ± 18.88 | 0.939 |
| Kujala | 78.8 ± 10.60 | 73.2 ± 6.70 | 0.116 |
| VISA-P score | 59.0 ± 12.90 | 50.2 ± 18.90 | 0.102 |
| Intrasubject Effects | ||||
|---|---|---|---|---|
| Measure | Asymptomatic Knee Group (n = 15) | Symptomatic Knee Group (n = 13) | Time Value F (Df); P (Eta2) | Intervention X Time F (Df); P (Eta2) |
| ROM (°) | F (3,78) = 47.998; p = 0.001 (0.649) | F (3,78) = 0.387; p = 0.70 (0.763) | ||
| Baseline | 129.0 ± 11.70 | 133.5 ± 6.4 | ||
| Post-intervention | 137.0 ± 6.50 * | 140.6 ± 5.70 * | ||
| 24 h | 142.2 ± 7.19 * | 147.0 ± 5.10 * | ||
| 1 week | 146.2 ± 6.50 * | 148.5 ± 4.50 * | ||
| NRS | F (3,78) = 11.562; p = 0.001(0.308) | F (3,78) = 0.725; p = 0.54 (0.027) | ||
| Baseline | 56.4 ± 14.56 | 56.9 ± 18.88 | ||
| Post-intervention | 48.3 ± 17.19 | 45.8 ± 23.08 | ||
| 24 h | 42.8 ± 17.64 | 40.6 ± 16.77 | ||
| 1 week | 42.3 ± 23.10 | 33.1 ± 21.05 * | ||
| Kujala score | F (3,78) = 6.835; p = 0.001 (0.208) | F (3,78) = 3.043; p = 0.05 (0.105) | ||
| Baseline | 78.8 ± 10.60 | 73.2 ± 6.70 | ||
| Post-intervention | 80.8 ± 10.90 | 77.2 ± 8.96 | ||
| 24 h | 82.7 ± 9.90 | 80.0 ± 10.70 | ||
| 1 week | 82.9 ± 12.00 | 84.5 ± 9.10 * | ||
| VISA-P score | F (3, 78) = 4.054; p = 0.01 (0.135) | F (3,78) = 2.044; p = 0.11 (0.073) | ||
| Baseline | 59.0 ± 12.90 | 50.2± 18.90 | ||
| Post-intervention | 66.7 ± 13.30 | 55.1 ± 15.30 | ||
| 24 h | 66.1 ± 11.40 | 52.9 ± 14.40 | ||
| 1 week | 63.4 ± 16.20 | 60.9 ± 17.50 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
García-Bermejo, P.; De-la-Cruz-Torres, B.; Romero-Morales, C. Ultrasound-Guided Percutaneous Neuromodulation in Patients with Unilateral Anterior Knee Pain: A Randomized Clinical Trial. Appl. Sci. 2020, 10, 4647. https://doi.org/10.3390/app10134647
García-Bermejo P, De-la-Cruz-Torres B, Romero-Morales C. Ultrasound-Guided Percutaneous Neuromodulation in Patients with Unilateral Anterior Knee Pain: A Randomized Clinical Trial. Applied Sciences. 2020; 10(13):4647. https://doi.org/10.3390/app10134647
Chicago/Turabian StyleGarcía-Bermejo, Paula, Blanca De-la-Cruz-Torres, and Carlos Romero-Morales. 2020. "Ultrasound-Guided Percutaneous Neuromodulation in Patients with Unilateral Anterior Knee Pain: A Randomized Clinical Trial" Applied Sciences 10, no. 13: 4647. https://doi.org/10.3390/app10134647
APA StyleGarcía-Bermejo, P., De-la-Cruz-Torres, B., & Romero-Morales, C. (2020). Ultrasound-Guided Percutaneous Neuromodulation in Patients with Unilateral Anterior Knee Pain: A Randomized Clinical Trial. Applied Sciences, 10(13), 4647. https://doi.org/10.3390/app10134647






