Artifactual Lung Ultrasonography: It Is a Matter of Traps, Order, and Disorder
Abstract
Featured Application
Abstract
1. Introduction
2. Terminology
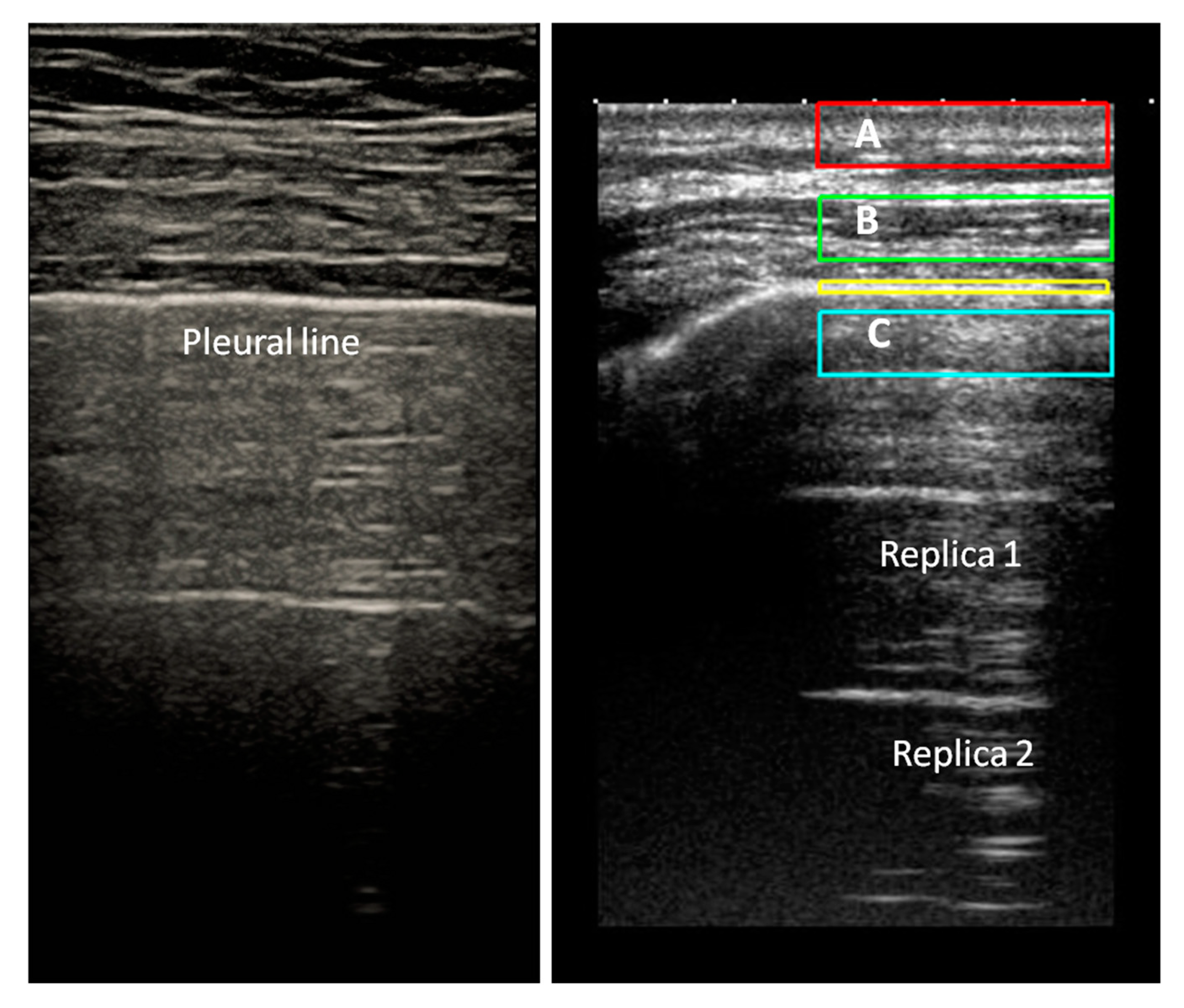
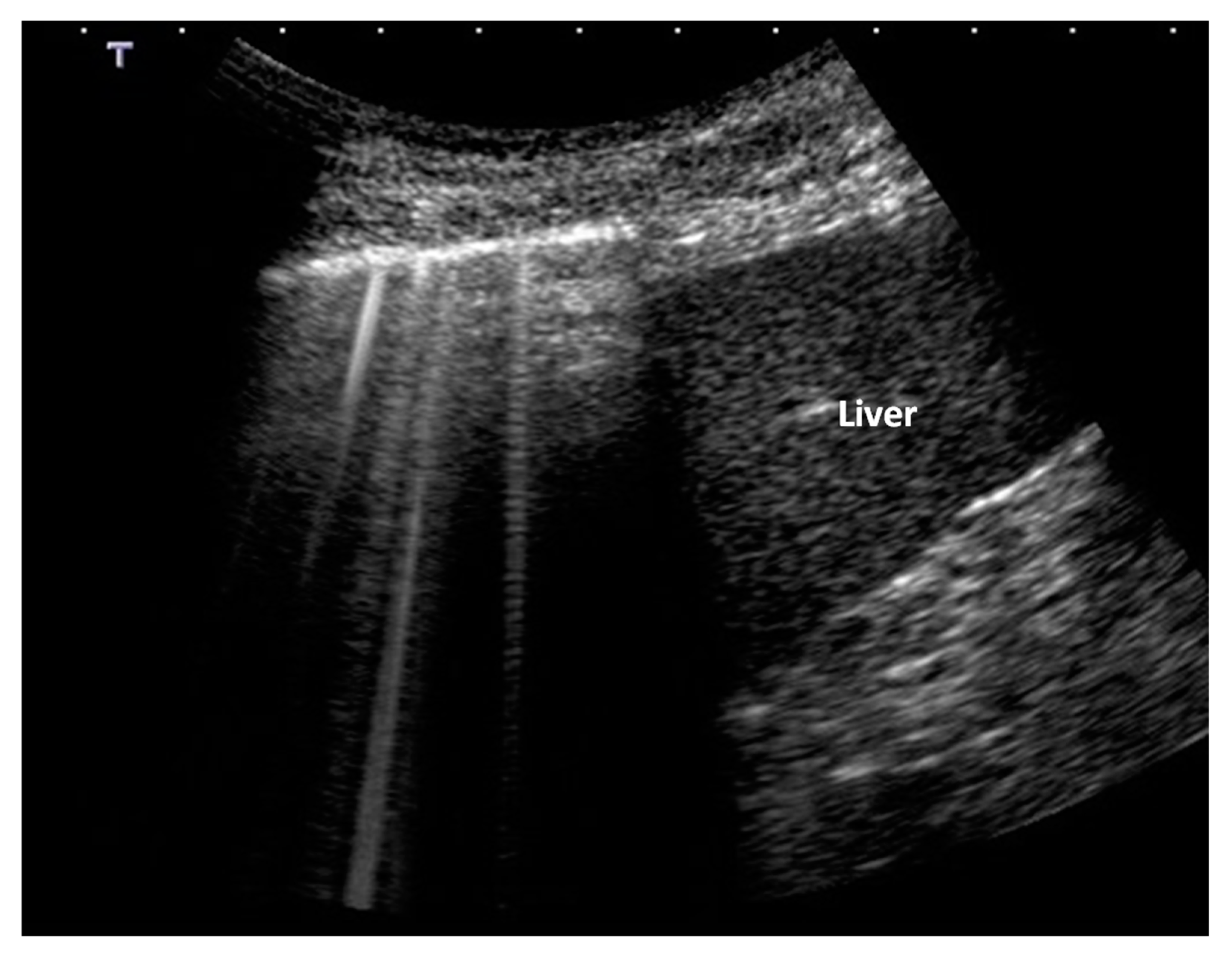
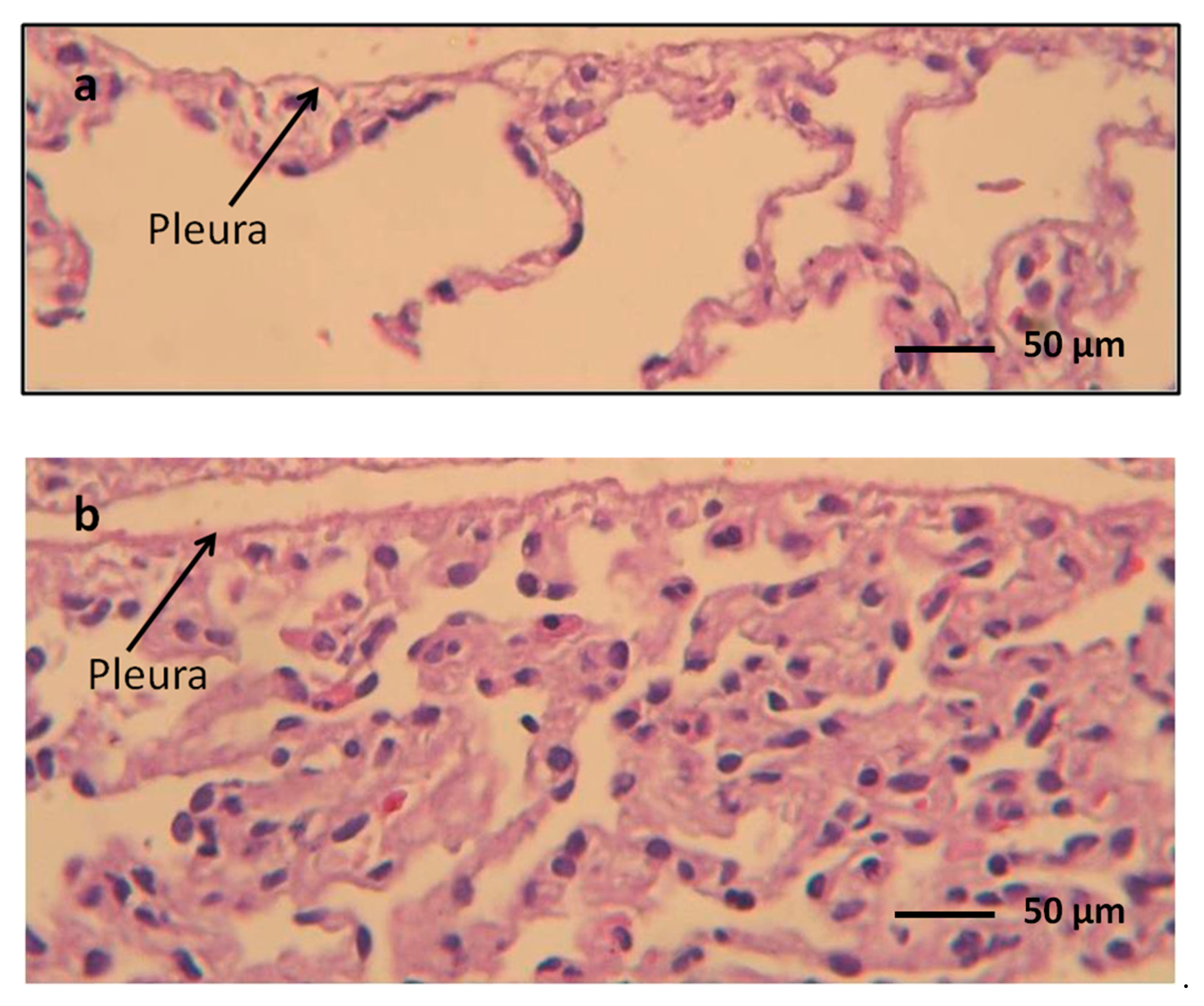
3. How Normal Anatomy of Pleural Plane is Represented in Ultrasound Images
4. Acoustic Behavior of the Diseased Pleura
5. How Acoustic Traps Work
6. Future Perspectives
Author Contributions
Funding
Conflicts of Interest
References
- Volpicelli, G.; Elbarbary, M.; Blaivas, M.; Lichtenstein, D.A.; Mathis, G.; Kirkpatrick, A.W.; Melniker, L.; Gargani, L.; Noble, V.E.; Via, G.; et al. International Liaison Committee on Lung Ultrasound (ILC-LUS) for the International Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012, 38, 577–591. [Google Scholar] [CrossRef]
- Sekiguchi, H.; Schenck, L.A.; Horie, R.; Suzuki, J.; Lee, E.H.; McMenomy, B.P. Critical care ultrasonography differentiates ARDS, pulmonary edema, and other causes in the early course of acute hypoxemic respiratory failure. Chest 2015, 148, 912–918. [Google Scholar] [CrossRef] [PubMed]
- Vignon, P.; Repessè, X.; Vieillard Baron, A.; Maury, E. Critical care ultrasonography in acute respiratory failure. Crit. Care 2016, 20, 228. [Google Scholar] [CrossRef] [PubMed]
- Soldati, G.; Demi, M.; Smargiassi, A.; Inchingolo, R.; Demi, L. The role of ultrasound lung artifacts in the diagnosis of respiratory diseases. Expert Rev. Respir. Med. 2019, 13, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Koegelenberg, C.F.; von Groote-Bidlingmaier, F.; Bolliger, C.T. Transthoracic ultrasonography for the respiratory physician. Respiration 2012, 84, 337–350. [Google Scholar] [CrossRef]
- Mayo, P.H.; Copetti, R.; Feller-Kopman, D.; Mathis, G.; Maury, E.; Mongodi, S.; Mojoli, F.; Volpicelli, G.; Zanobetti, M. Thoracic ultrasonography: A narrative review. Intensive Care Med. 2019, 45, 1200–1211. [Google Scholar] [CrossRef]
- Reissig, A.; Copetti, R.; Mathis, G.; Mempel, C.; Schuler, A.; Zechner, P.; Aliberti, S.; Neumann, R.; Kroegel, C.; Hoyer, H. Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: A prospective, multicenter, diagnostic accuracy study. Chest 2012, 142, 965–972. [Google Scholar] [CrossRef]
- Lichtenstein, D.; Goldstein, I.; Mourgeon, E.; Cluzel, P.; Grenier, P.; Rouby, J.J. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 2004, 100, 9–15. [Google Scholar] [CrossRef]
- Brogi, E.; Bignami, E.; Sidoti, A.; Shawar, M.; Gargani, L.; Vetrugno, L.; Volpicelli, G.; Forfori, F. Could the use of bedside lung ultrasound reduce the number of chest x-rays in the intensive care unit? Cardiovasc. Ultrasound 2017, 13, 23. [Google Scholar] [CrossRef]
- Smargiassi, A.; Inchingolo, R.; Chiappetta, M.; Ciavarella, L.P.; Lopatriello, S.; Corbo, G.M.; Margaritora, S.; Richeldi, L. Agreement between chest ultrasonography and chest X-ray in patients who have undergone thoracic surgery: Preliminary results. Multidiscip. Respir. Med. 2019, 4, 9. [Google Scholar] [CrossRef]
- Agricola, E.; Arbelot, C.; Blaivas, M.; Bouhemad, B.; Copetti, R.; Dean, A.; Dulchavsky, S.; Elbarbary, M.; Gargani, L.; Hoppmann, R.; et al. Ultrasound performs better than radiographs. Thorax 2011, 66, 828–829. [Google Scholar] [CrossRef] [PubMed]
- Reissig, A.; Kroegel, C. Sonographic diagnosis and follow-up of pneumonia: A prospective study. Respiration 2007, 74, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, D.; Mezière, G.; Seitz, J. The dynamic air bronchogram. A lung ultrasound sign of alveolar consolidation ruling out atelectasis. Chest 2009, 135, 1421–1425. [Google Scholar] [CrossRef] [PubMed]
- Sartori, S.; Postorivo, S.; Vece, F.D.; Ermili, F.; Tassinari, D.; Tombesi, P. Contrast-enhanced ultrasonography in peripheral lung consolidations: What’s its actual role? World J. Radiol. 2013, 28, 372–380. [Google Scholar] [CrossRef]
- Soni, N.J.; Franco, R.; Velez, M.I.; Schnobrich, D.; Dancel, R.; Restrepo, M.I.; Mayo, P.H. Ultrasound in the diagnosis and management of pleural effusions. J. Hosp. Med. 2015, 10, 811–816. [Google Scholar] [CrossRef]
- Smargiassi, A.; Pasciuto, G.; Pedicelli, I.; Lo Greco, E.; Calvello, M.; Inchingolo, R.; Schifino, G.; Capoluongo, P.; Patriciello, P.; Manno, M.; et al. Chest ultrasonography in health surveillance of asbestos-related lung diseases. Toxicol. Ind. Health 2017, 33, 537–546. [Google Scholar] [CrossRef]
- Smargiassi, A.; Inchingolo, R.; Zanforlin, A.; Valente, S.; Soldati, G.; Corbo, G.M. Description of free-flowing pleural effusions in medical reports after echographic assessment. Respiration 2013, 85, 439–441. [Google Scholar] [CrossRef]
- Lichtenstein, D.; Mezière, G.; Biderman, P.; Gepner, A.; Barrè, O. The comet-tail artifact: An ultrasound sign of alveolar interstitialsyndrome. Am. J. Respir. Crit. Care Med. 1997, 156, 1640–1646. [Google Scholar] [CrossRef]
- Dietrich, C.F.; Mathis, G.; Blaivas, M.; Volpicelli, G.; Seibel, A.; Wastl, D. Lung B-line artefacts and their use. J. Thorac. Dis. 2016, 8, 1356–1365. [Google Scholar] [CrossRef]
- Reissig, A.; Copetti, R.; Kroegel, C. Current role of emergency ultrasound of the chest. Crit. Care Med. 2011, 39, 839–845. [Google Scholar] [CrossRef]
- Dulchavsky, S.A.; Schwarz, K.L.; Kirkpatrick, A.W.; Billica, R.D.; Williams, D.R.; Diebel, L.N.; Campbell, M.R.; Sargysan, A.E.; Hamilton, D.R. Prospective evaluation of thoracic ultrasound in the detection of pneumothorax. J. Trauma 2001, 50, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Lichtenstein, D.A.; Mezière, G.A. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: The BLUE protocol. Chest 2008, 134, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Smargiassi, A.; Inchingolo, R.; Soldati, G.; Copetti, R.; Marchetti, G.; Zanforlin, A. The role of chest ultrasonography in the management of respiratory diseases: Document II. Multidiscip. Respir. Med. 2013, 8, 55. [Google Scholar] [CrossRef] [PubMed]
- Soldati, G.; Smargiassi, A.; Inchingolo, R.; Sher, S.; Nenna, R.; Valente, S. Lung ultrasonography may provide an indirect estimation of lung porosity and airspace geometry. Respiration 2014, 88, 458–468. [Google Scholar] [CrossRef]
- Soldati, G.; Inchingolo, R.; Smargiassi, A.; Sher, S.; Nenna, R.; Inchingolo, C.D.; Valente, S. Ex vivo lung sonography: Morphologic-ultrasound relationship. Ultrasound Med. Biol. 2012, 38, 1169–1179. [Google Scholar] [CrossRef]
- Beckh, S.; Bolcskei, P.L.; Lessnau, K.D. Real time chest ultrasonography: A comprehensive review for the pulmonologist. Chest 2000, 122, 1759–1773. [Google Scholar] [CrossRef]
- Leslie, K.; Wick, M. Practical Pulmonary Pathology. A Diagnostic Approach, 1st ed.; Churchill-Livingstone: Philadelphia, PA, USA, 2005. [Google Scholar]
- Soldati, G.; Demi, M.; Inchingolo, R.; Smargiassi, A.; Demi, L. On the Physical Basis of Pulmonary Sonographic Interstitial Syndrome. J. Ultrasound Med. 2016, 35, 2075–2086. [Google Scholar] [CrossRef]
- Slavin, G.; Kreel, L.; Herbert, A.; Sandin, B. Pulmonary oedema at necropsy: A combined pathological and radiological method of study. J. Clin. Path 1975, 28, 357–366. [Google Scholar] [CrossRef]
- Raghu, G.; Remy-Jardin, M.; Myers, J.L.; Richeldi, L.; Ryerson, C.J.; Lederer, D.J. Diagnosis of Idipatic Pulmonary Fibrosis. An official, ATS/ERS/JRS/ALAT Clinical Practice Gudeline. Am. J. Respir. Crit. Care Med. 2018, 198, 44–68. [Google Scholar] [CrossRef]
- Leslie, K.O. Pathology of interstitial lung disease. Clin. Chest Med. 2004, 25, 657–703. [Google Scholar] [CrossRef]
- Leslie, K.O. My approach to interstitial lung disease using clinical, radiological and histopathological patterns. J. Clin. Pathol. 2019, 62, 387–401. [Google Scholar] [CrossRef] [PubMed]
- Demi, M.; Prediletto, R.; Soldati, G.; Demi, L. Physical mechanisms providing clinical informations from ultrasound lung images: Hypothesis and early confirmations. IEEE Trans. Ultrason. Ferroelectr. Freq. Control 2019. [CrossRef] [PubMed]
- Milne, E.N.; Pistolesi, M.; Miniati, M.; Giuntini, C. The radiologic distinction of cardiogenic and non cardiogenic edema. AJR 1985, 144, 879–894. [Google Scholar] [CrossRef] [PubMed]
- Copetti, R.; Soldati, G.; Copetti, P. Chest sonography: A useful tool to differentiate acute cardiogenic pulmonary edema from Acute respiratory distress syndrome. Cardiovasc. Ultrasound 2008, 6, 16. [Google Scholar] [CrossRef]
- Soldati, G.; Demi, M. The use of lung ultrasound images for the differential diagnosis of pulmonary and cardiac interstitial pathology. J. Ultrasound 2017, 20, 91–96. [Google Scholar] [CrossRef]
- Kolb, M.; Bondue, B.; Pesci, A.; Miyazaki, Y.; Song, J.W.; Bhatt, N.Y. Acute exacerbations of progressive-fibrosing interstitial lung diseases. Eur. Respir. Rev. 2018, 27. [Google Scholar] [CrossRef]
- Dalle Carbonare, L.; Valenti, M.T.; Bertoldo, F.; Zanatta, M.; Zenari, S.; Realdi, G. Bone microarchitecture evaluated by histomorphometry. Micron 2005, 36, 609–616. [Google Scholar] [CrossRef]
- Demi, L.; van Hoeve, W.; van Sloun, R.J.G.; Soldati, G.; Demi, M. Determination of a potential quantitative measure of the state of the lung using lung ultrasound spectroscopy. Sci. Rep. 2017, 7, 12746. [Google Scholar] [CrossRef]
- Demi, L.; Egan, T.; Muller, M. Lung ultrasound imaging, a technical review. Appl. Sci. 2020, 10, 462. [Google Scholar] [CrossRef]
- Demi, L.; Demi., M.; Smargiassi, A.; Inchingolo, R.; Faita, F.; Soldati, G. Ultrasonography in lung pathologies: New perspectives. Multidiscip. Respir. Med. 2014, 9, 27. [Google Scholar] [CrossRef]
- Reissig, A.; Kroegel, C. Transthoracic sonography of diffuse parenchimal lung disease: The role of comet tail artifacts. J. Ultrasound Med. 2003, 22, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Hasan, A.A.; Makhlouf, H.A. B-lines: Transthoracic chest ultrasound signs useful in assessment of interstitial lung diseases. Ann. Thorac. Med. 2014, 9, 99–103. [Google Scholar]
- Singh, A.K.; Mayo, P.H.; Koenig, S.; Talwar, A.; Narasimhan, M. The Use of M-Mode Ultrasonography to Differentiate the Causes of B Lines. Chest 2018, 153, 689–696. [Google Scholar] [CrossRef] [PubMed]
- Child, S.Z.; Hartman, C.L.; Schery, L.A.; Carstensen, E.L. Lung damage from exposure to pulsed ultrasound. Ultrasound Med. Biol. 1990, 16, 817–825. [Google Scholar] [CrossRef]
- Miller, D.L. Induction of pulmonary hemorrhage in rats during diagnostic ultrasound. Ultrasound Med. Biol. 2012, 38, 476–482. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.L.; Dou, C.; Raghavendran, K. Pulmonary Capillary Hemorrhage Induced by Fixed-Beam Pulsed Ultrasound. Ultrasound Med. Biol. 2015, 41, 2212–2219. [Google Scholar] [CrossRef] [PubMed]
- Haar, G. Ultrasonic imaging: Safety considerations. Interface Focus 2011, 1, 686–697. [Google Scholar] [CrossRef]


| Hystopatologic Pattern | Expected Artefacts | Examples of Pathology |
|---|---|---|
| Near normal lung | No artefacs No artefact or rare artifacts from secondary hypoventilation No artefacts Bright isolated vertical artefacts, with or without internal structure, showing tendentially high native frequencies (about 6 MHz) Bilateral expression of artifacts without spared areas | Pulmonary hypertension Airway diseases Emphysema Air cysts Early and moderate cardiogenic pulmonary edema |
| Fibrosis | Irregular pleura (cobblestone), vertical merged artifacts prevalent at the lung basis, multiform artifacts in middle and lower fields, generally without internal structure, with tendentially low native frequencies (about 3 MHz).Some artifacts fade quickly. Many different types of vertical artifacts that are unevenly distributed in the lung areas typical of individual pathologies, irregular pleura depending on the disease | Idiopatic pulmonary fibrosis Connective tissue diseases Chronic hypersensitivity pneumonitis Chronic cardiac congestion Drug toxicity |
| Acute lung injury | Appearance similar to the Fibrosis pattern. Inhomogeneous artefactual pattern characterized by more than one native frequency, with spared areas. Possible presence of thin, brilliant and internally structured artifacts in inhomogeneous distribution. Relative representation of coalescent artifacts and white lung, showing inhhomogeneous and variable arrangement | Diffuse alveolar damage Infections Acute aspiration Diffuse alveolar hemorrhage Early ARDS Late cardiogenic pulmonary edema (alveolar flooding) |
| Chronic cellular infiltrates | Appearance similar to Acute lung injury pattern. White lung and merged, thin and modulated vertical artifacts may be absent as they tend to indicate an acute phase of disease | Viral and fungal infections Hypersensitivty pneumonitis Atypical mycobacterial infections Connective tissue diseases Lymphangitic carcinoma Lymphoid interstitial pneumonia and limphoma Smoking related disease |
| Alveolar filling | Combined aspect of vertical, variable, very heterogeneous artifacts, and subpleural consolidation. Many native frequencies | Organizing diffuse alveolar damage and infections Bacterial infections Pulmonary alveolar proteinosis Eosinophilic lung dieseases Drug toxicity ARDS |
| Nodules | Nodules can be visible using a linear probes if located at pleural level. They acquire suggestive locations depending on the disease and often appear like vertical artifacts with nodular and non-point-like origin | Carcinomas, sarcomas, melanoma Lymphoma Lymphoid interstitial pneumonia Necrotizing infections Granulomatous infections Sarcoidosis Pneumoconiosis |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soldati, G.; Smargiassi, A.; Demi, L.; Inchingolo, R. Artifactual Lung Ultrasonography: It Is a Matter of Traps, Order, and Disorder. Appl. Sci. 2020, 10, 1570. https://doi.org/10.3390/app10051570
Soldati G, Smargiassi A, Demi L, Inchingolo R. Artifactual Lung Ultrasonography: It Is a Matter of Traps, Order, and Disorder. Applied Sciences. 2020; 10(5):1570. https://doi.org/10.3390/app10051570
Chicago/Turabian StyleSoldati, Gino, Andrea Smargiassi, Libertario Demi, and Riccardo Inchingolo. 2020. "Artifactual Lung Ultrasonography: It Is a Matter of Traps, Order, and Disorder" Applied Sciences 10, no. 5: 1570. https://doi.org/10.3390/app10051570
APA StyleSoldati, G., Smargiassi, A., Demi, L., & Inchingolo, R. (2020). Artifactual Lung Ultrasonography: It Is a Matter of Traps, Order, and Disorder. Applied Sciences, 10(5), 1570. https://doi.org/10.3390/app10051570







