Design of a Sandwich Hierarchically Porous Membrane with Oxygen Supplement Function for Implantable Glucose Sensor
Abstract
:Featured Application
Abstract
1. Introduction
2. Materials and Methods
2.1. Preparation of the Glucose Biosensor
2.2. Glucose Sensor Performance Test
3. Results
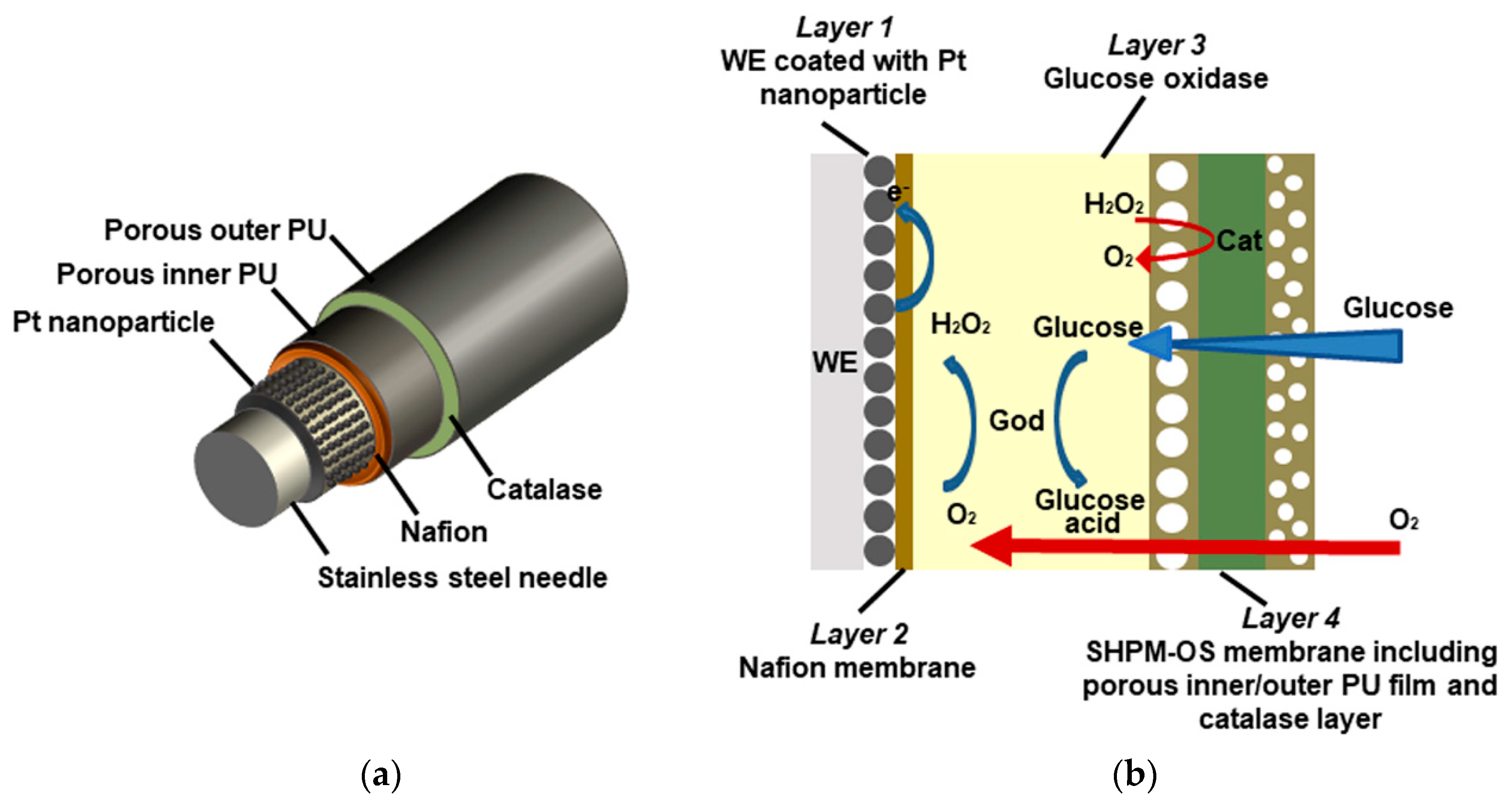
3.1. Principle and Design of the Glucose Sensor
3.2. Morphology of the New Sensor Electrode
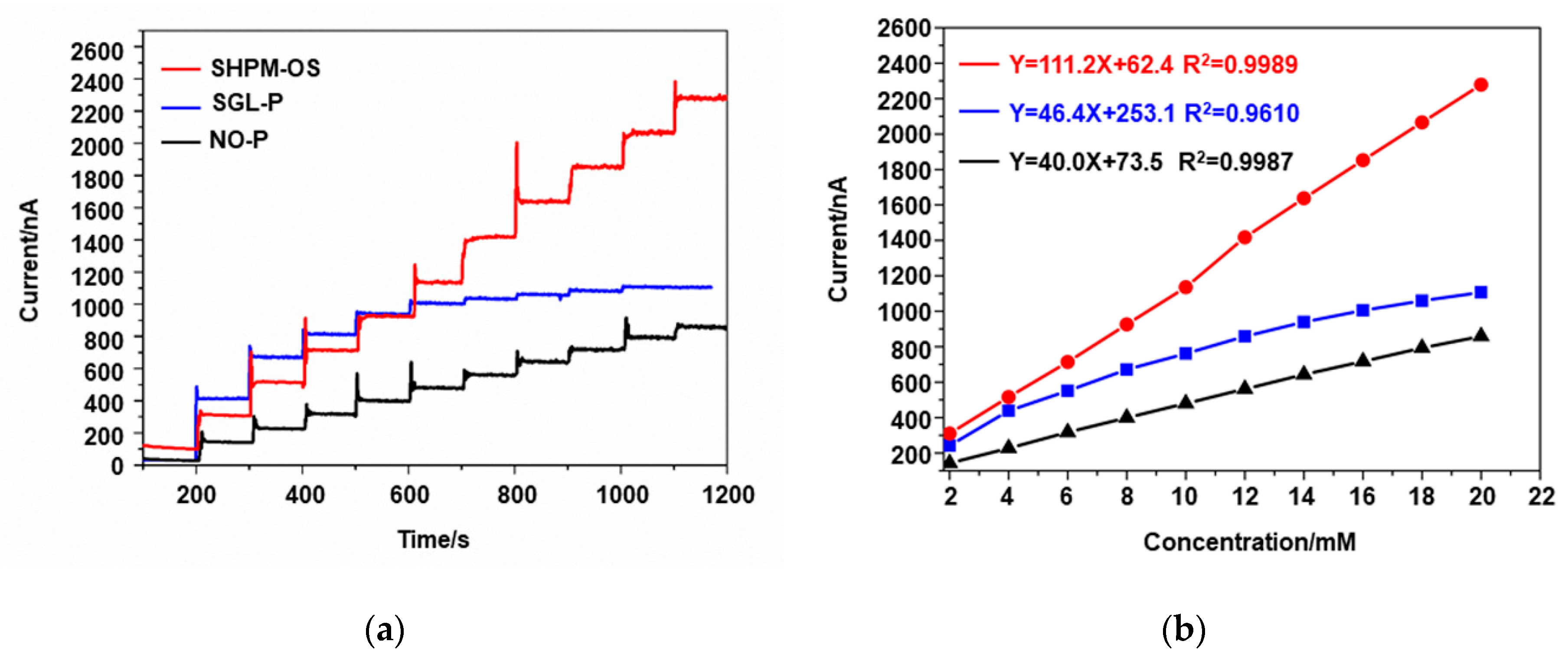
3.3. Linearity and Sensitivity of the Glucose Sensor
3.4. Response Time of the Glucose Sensor
3.5. Long Time Stability of the Glucose Sensor
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- van Hooijdonk, R.T.M.; Leopold, J.H.; Winters, T.; Binnekade, J.M.; Juffermans, N.P.; Horn, J.; Fischer, J.C.; van Dongen-Lases, E.C.; Schultz, M.J. Point accuracy and reliability of an interstitial continuous glucose-monitoring device in critically ill patients: A prospective study. Crit. Care 2015, 19, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, F.; Signal, M.; Chase, J.G. Using Continuous Glucose Monitoring Data and Detrended Fluctuation Analysis to Determine Patient Condition: A Review. J. Diabetes Sci. Technol. 2015, 9, 1327–1335. [Google Scholar] [CrossRef] [PubMed]
- van Enter, B.J.; Von, H.E. Challenges and perspectives in continuous glucose monitoring. Chem. Commun. 2018, 54, 5032. [Google Scholar] [CrossRef]
- Cappon, G.; Acciaroli, G.; Vettoretti, M.; Facchinett, A.; Sparacino, G. Wearable continuous glucose monitoring sensors: A revolution in diabetes treatment. Electronics 2017, 6, 65. [Google Scholar] [CrossRef] [Green Version]
- Scholten, K.; Meng, E. A review of implantable biosensors for closed-loop glucose control and other drug delivery applications. Int. J. Pharm. 2018, 544, 319–334. [Google Scholar] [CrossRef]
- van Beers, C.A.J.; Kleijer, S.J.; Serné, E.H.; Geelhoed-Duijvestijn, P.H.; Snoek, F.J.; Kramer, M.H.; Diamant, M. Design and rationale of the in control trial: The effects of real-time continuous glucose monitoring on glycemia and quality of life in patients with type 1 diabetes mellitus and impaired awareness of hypoglycemia. BMC Endocr. Disord. 2015, 15, 42. [Google Scholar] [CrossRef] [Green Version]
- Heo, Y.J.; Kim, S.-H. Toward Long-Term Implantable Glucose Biosensors for Clinical Use. Appl. Sci. 2019, 9, 2518. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.; Zhao, X.L.; Li, Z.H.; Zhu, Z.G.; Qian, S.H.; Flewitt, A.J. Current and Emerging Technology for Continuous Glucose Monitoring. Sensors 2017, 17, 182. [Google Scholar] [CrossRef] [Green Version]
- Zhai, D.; Liu, B.; Shi, Y.; Pan, L.; Wang, Y.; Li, W.; Zhang, R.; Yu, G. Highly Sensitive Glucose Sensor Based on Pt Nanoparticle/Polyaniline Hydrogel Heterostructures. ACS Nano 2013, 7, 3540–3546. [Google Scholar] [CrossRef]
- Fang, Y.; Wang, S.; Liu, Y.; Xu, Z.; Zhang, K.; Guo, Y. Development of Cu nanoflowers modified the flexible needle-type microelectrode and its application in continuous monitoring glucose in vivo. Biosens. Bioelectron. 2018, 110, 44–51. [Google Scholar] [CrossRef]
- Abdulbari, H.A.; Basheer, E.A.M. Electrochemical Biosensors: Electrode Development, Materials, Design, and Fabrication. Chembioeng Rev. 2017, 4, 92–105. [Google Scholar] [CrossRef] [Green Version]
- Witkowska, N.E.; Kundys, M.; Jeleń, P.S.; Jönsson-Niedziółka, M. Electrochemical Glucose Sensing: Is There Still Room for Improvement? Anal. Chem. 2016, 88, 11271–11282. [Google Scholar] [CrossRef] [PubMed]
- Zulkifli, Z.A.; Ridhuan, N.S.; Nor, N.M.; Zakaria, N.D.; Razak, K. The effect of gold nanoparticles modified electrode on the glucose sensing performance. In Proceedings of the International Conference of Global Network for Innovative Technology, Penang, Malaysia, 27–29 January 2016; 2017. [Google Scholar]
- Stine, K.J. Biosensor Applications of Electrodeposited Nanostructures. Appl. Sci. 2019, 9, 797. [Google Scholar] [CrossRef] [Green Version]
- Xu, G.; Adeloju, S.B.; Wu, Y.; Zhang, X. Modification of polypyrrole nanowires array with platinum nanoparticles and glucose oxidase for fabrication of a novel glucose biosensor. Anal. Chim. Acta 2012, 755, 100–107. [Google Scholar] [CrossRef] [PubMed]
- German, N.; Ramanavicius, A.; Ramanaviciene, A. Amperometric Glucose Biosensor Based on Electrochemically Deposited Gold Nanoparticles Covered by Polypyrrole. Electroanalysis 2017, 29, 1267–1277. [Google Scholar] [CrossRef]
- Chen, D.; Wang, C.; Chen, W.; Chen, Y.; Zhang, X. PVDF-Nafion nanomembranes coated microneedles for in vivo transcutaneous implantable glucose sensing. Biosens. Bioelectron. 2015, 74, 1047–1052. [Google Scholar] [CrossRef]
- Lopes, I.C.; Zebda, A.; Vadgama, P. New directions in membrane designs for biosensors. Curr. Opin. Electrochem. 2018, 12, 107–112. [Google Scholar] [CrossRef]
- Wang, N.; Burugapalli, K.; Song, W.; Halls, J.; Moussy, F.; Ray, A.; Zheng, Y. Electrospun fibro-porous polyurethane coatings for implantable glucose biosensors. Biomaterials 2013, 34, 888–901. [Google Scholar] [CrossRef] [Green Version]
- Yang, W.; Xue, H.; Carr, L.R.; Wang, J.; Jiang, S. Zwitterionic poly(carboxybetaine) hydrogels for glucose biosensors in complex media. Biosens. Bioelectron. 2011, 26, 2454–2459. [Google Scholar] [CrossRef]
- Koh, A.; Nichols, S.P.; Schoenfisch, M.H. Glucose sensor membranes for mitigating the foreign body response. J. Diabetes Sci. Technol. 2011, 5, 1052–1059. [Google Scholar] [CrossRef] [Green Version]
- Mercado, R.C.; Moussy, F. In vitro and in vivo mineralization of Nafion membrane used for implantable glucose sensors. Biosens. Bioelectron. 1998, 13, 133–145. [Google Scholar] [CrossRef]
- Moattisirat, D.; Poitout, V.; Thome, V.; Gangnerau, M.N.; Zhang, Y.; Hu, Y.; Wilson, G.S.; Lemonnier, F.; Klein, J.C.; Reach, G. Reduction of acetaminophen interference in glucose sensors by a composite Nafion membrane—Demonstration in rats and man. Diabetologia 1994, 37, 610–616. [Google Scholar] [CrossRef]
- Brazell, M.P.; Kasser, R.J.; Renner, K.J.; Feng, J.; Moghaddam, B.; Adams, R.N. electrocoating carbon-fiber microelectrodes with Nafion improves selectivity for electroactive neurotransmitters. J. Neurosci. Methods 1987, 22, 167–172. [Google Scholar] [CrossRef]
- Yu, B.; Wang, C.; Ju, Y.; West, L.; Harmon, J.; Moussy, Y.; Moussy, F. Use of hydrogel coating to improve the performance of implanted glucose sensors. Biosens. Bioelectron. 2008, 23, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yu, B.; Knudsen, B.; Harmon, J.; Moussy, F.; Moussy, Y. Synthesis and performance of novel hydrogels coatings for implantable glucose sensors. Biomacromolecules 2008, 9, 561–567. [Google Scholar] [CrossRef]
- Fang, L.; Liang, B.; Yang, G.; Hu, Y.; Zhu, Q.; Ye, X. A needle-type glucose biosensor based on PANI nanofibers and PU/E-PU membrane for long-term invasive continuous monitoring. Biosens. Bioelectron. 2017, 97, 196–202. [Google Scholar] [CrossRef]
- Jiang, L.; Koinkar, P.; Fuchiwaki, Y.; Yasuzawa, M. A fine pointed glucose oxidase immobilized electrode for low-invasive amperometric glucose monitoring. Biosens. Bioelectron. 2016, 86, 90–94. [Google Scholar]
- Vaddiraju, S.; Burgess, D.J.; Jain, F.C.; Papadimitrakopoulos, F. The role of H2O2 outer diffusion on the performance of implantable glucose sensors. Biosens. Bioelectron. 2009, 24, 1557–1562. [Google Scholar] [CrossRef] [Green Version]
- Kuwahara, T.; Ogawa, K.; Sumita, D.; Kondo, M.; Shimomura, M. Amperometric glucose sensing with polyaniline/poly(acrylic acid) composite film bearing glucose oxidase and catalase based on competitive oxygen consumption reactions. J. Electroanal. Chem. 2018, 811, 62–67. [Google Scholar] [CrossRef]
- Lucisano, J.; Routh, T.; Lin, J.; Gough, D. Glucose Monitoring in Individuals with Diabetes using a Long-Term Implanted Sensor/Telemetry System and Model. IEEE Trans. Bio-Med. Eng. 2017, 64, 1982–1993. [Google Scholar] [CrossRef] [Green Version]
- Vaddiraju, S.; Legassey, A.; Wang, Y.; Qiang, L.; Burgess, D.; Jain, F.; Papadimitrakopoulos, F. Design and fabrication of a high-performance electrochemical glucose sensor. J. Diabetes Sci. Technol. 2011, 5, 1044–1051. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vaddiraju, S.; Legassey, A.; Qiang, L.; Wang, Y.; Burgess, D.J.; Papadimitrakopoulos, F. Enhancing the sensitivity of needle-implantable electrochemical glucose sensors via surface rebuilding. J. Diabetes Sci. Technol. 2013, 7, 441–451. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, Y.-J.; Saviers, K.R.; Fisher, T.S.; Irazoqui, P.P. Continuous glucose monitoring with a flexible biosensor and wireless data acquisition system. Sens. Actuators B-Chem. 2018, 275, 237–243. [Google Scholar] [CrossRef]
- Yosefi, G.; Mirzakuchaki, S.; Raissi, F. New Programmable CMOS Fuzzifier and C2V Circuits Applicable in FLC Chip for Signal Processing of MEMS Glucose Sensors. Appl. Sci. 2015, 5, 402–414. [Google Scholar] [CrossRef]
- Ward, W.K.; Jansen, L.B.; Anderson, E.; Reach, G.; Klein, J.C.; Wilson, G.S. A new amperometric glucose microsensor: In vitro and short-term in vivo evaluation. Biosens. Bioelectron. 2002, 17, 181–189. [Google Scholar] [CrossRef]
- Chen, X.H.; Matsumoto, N.; Hu, Y.; Wilson, G. Electrochemically mediated electrodeposition/electropolymerization to yield a glucose microbiosensor with improved characteristics. Anal. Chem. 2002, 74, 368–372. [Google Scholar] [CrossRef]
- Bindra, D.S.; Zhang, Y.; Wilson, G.S.; Sternberg, R.; Thévenot, D.R.; Moatti, D.; Reach, G. Design and in vitro studies of a needle-type glucose sensor for subcutaneous monitoring. Anal. Chem. 1991, 63, 1692. [Google Scholar] [CrossRef] [Green Version]
- Yu, B.Z.; Moussy, Y.; Moussy, F. Coil-type implantable glucose biosensor with excess enzyme loading. Front. Biosci. Landmark 2005, 10, 512–520. [Google Scholar] [CrossRef] [Green Version]
- Guo, M.; Fang, H.; Wang, R.; Yang, Z.; Xu, X. Electrodeposition of chitosan-glucose oxidase biocomposite onto Pt–Pb nanoparticles modified stainless steel needle electrode for amperometric glucose biosensor. J. Mater. Sci. Mater. Med. 2011, 22, 1985–1992. [Google Scholar] [CrossRef]
- Croce, R.A., Jr.; Vaddiraju, S.; Kondo, J.; Wang, Y.; Zuo, L.; Zhu, K.; Lslam, S.k.; Burgess, D.J.; Papadimitrakopoulos, F.; Jain, F.C. A miniaturized transcutaneous system for continuous glucose monitoring. Biomed. Microdevices 2013, 15, 151–160. [Google Scholar]
- Yu, B.Z.; Long, N.; Moussy, Y.; Moussy, F. A long-term flexible minimally-invasive implantable glucose biosensor based on an epoxy-enhanced polyurethane membrane. Biosens. Bioelectron. 2006, 21, 2275–2282. [Google Scholar] [CrossRef] [PubMed]
- Koh, A.; Lu, Y.; Schoenfisch, M.H. Fabrication of Nitric Oxide-Releasing Porous Polyurethane Membranes Coated Needle-Type Implantable Glucose Biosensors. Anal. Chem. 2013, 85, 10488–10494. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, T.; Gao, J.; Qin, X.; Zhang, X.; Xue, H. A Novel Glucose Biosensor Based on Hierarchically Porous Block Copolymer Film. Polymers 2018, 10, 723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Narayan, R.J.; Jin, C.; Menegazzo, N.; Mizaikoff, B.; Gerhardt, R.; Andara, M.; Agarwal, A.; Shih, C.C.; Shih, C.M.; Lin, S.J.; et al. Nanoporous hard carbon membranes for medical applications. J. Nanosci. Nanotechnol. 2007, 7, 1486–1493. [Google Scholar] [CrossRef] [PubMed]
- Fang, L.; Liang, B.; Yang, G.; Hu, Y.; Zhu, Q.; Ye, X. Study of glucose biosensor lifetime improvement in 37 °C serum based on PANI enzyme immobilization and PLGA biodegradable membrane. Biosens. Bioelectron. 2014, 56, 91–96. [Google Scholar] [CrossRef]
- Fang, L.; Liu, B.; Liu, L.; Li, Y.; Huang, K.; Zhang, Q. Direct electrochemistry of glucose oxidase immobilized on Au nanoparticles-functionalized 3D hierarchically ZnO nanostructures and its application to bioelectrochemical glucose sensor. Sens. Actuators B Chem. 2016, 222, 1096–1102. [Google Scholar] [CrossRef]
- Edagawa, K.; Fuchiwaki, Y.; Yasuzawa, M. In Vivo Evaluation of Fine Needle Amperometric Glucose Sensors Implanted in Rabbit’s Blood Vessel. J. Electrochem. Soc. 2014, 161, B3111–B3115. [Google Scholar] [CrossRef]
- Kim, K.B.; Lee, W.C.; Cho, C.H.; Park, D.S.; Cho, S.J.; Shim, Y.B. Continuous glucose monitoring using a microneedle array sensor coupled with a wireless signal transmitter. Sens. Actuators B Chem. 2019, 281, 14–21. [Google Scholar] [CrossRef]
- Liu, G.-S.; Kong, Y.; Wang, Y.; Luo, Y.; Fan, X.; Xie, X.; Yang, B.-R.; Wu, M.X. Microneedles for transdermal diagnostics: Recent advances and new horizons. Biomaterials 2020, 232, 119740. [Google Scholar] [CrossRef]
- Zeng, X.; Zhang, Y.; Du, X.; Li, Y.; Tang, W. A highly sensitive glucose sensor based on a gold nanoparticles/polyaniline/multi-walled carbon nanotubes composite modified glassy carbon electrode. New J. Chem. 2018, 42, 11944–11953. [Google Scholar] [CrossRef]
- Zdarta, J.; Meyer, A.S.; Jesionowski, T.; Pinelo, M. A General Overview of Support Materials for Enzyme Immobilization: Characteristics, Properties, Practical Utility. Catalysts 2018, 8, 92. [Google Scholar] [CrossRef] [Green Version]
- Semenova, D.; Silina, Y.E.; Koch, M.; Micheli, L.; Zubov, A.; Gernaey, K.V. Sensors for biosensors: A novel tandem monitoring in a droplet towards efficient screening of robust design and optimal operating conditions. Analyst 2019, 144, 2511–2522. [Google Scholar] [CrossRef] [PubMed]
- Fang, Y.; Zhang, D.; Guo, Y.; Guo, Y.M.; Chen, Q. Simple one-pot preparation of chitosan-reduced graphene oxide-Au nanoparticles hybrids for glucose sensing. Sens. Actuators B Chem. 2015, 221, 265–272. [Google Scholar] [CrossRef]
- Donahue, C.E.T.; Miller, D.R., Jr.; Beger, T.W.; Johann, T.W.; Keithley, R.B. Improved formation of electrically-deposited enzyme-embedded chitosan coatings onto carbon fiber microelectrodes. Anal. Methods 2018, 10, 1565–1576. [Google Scholar] [CrossRef]
- Vallejoheligon, S.G.; Brown, N.L.; Reichert, W.M.; Klitzman, B. Porous, Dexamethasone-Loaded Polyurethane Coatings Extend Performance Window of Implantable Glucose Sensors in vivo. Acta Biomater. 2016, 30, 106–115. [Google Scholar] [CrossRef] [Green Version]
- Vallejo-Heligon, S.G.; Klitzman, B.; Reichert, W.M. Characterization of porous, dexamethasone-releasing polyurethane coatings for glucose sensors. Acta Biomater. 2014, 10, 4629–4638. [Google Scholar] [CrossRef] [Green Version]
- Soto, R.J.; Privett, B.J.; Schoenfisch, M.H. In vivo analytical performance of nitric oxide-releasing glucose biosensors. Anal. Chem. 2014, 86, 7141–7149. [Google Scholar] [CrossRef] [Green Version]
- de la Oliva, N.; del Valle, J.; Delgado-Martinez, I.; Mueller, M.; Stieglitz, T.; Navarro, X. Long-Term Functionality of Transversal Intraneural Electrodes Is Improved by Dexamethasone Treatment. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 457–464. [Google Scholar] [CrossRef] [Green Version]



| Sensor Structure | Linear Range mM | Correlation Coefficient R2 | Reference |
|---|---|---|---|
| Pt/Cu-NFs/Nafion/GOD/PU | 0–20 | 0.99 | [10] |
| Pt/PANI/GOD/PU/E-PU | 0–20 | 0.9996 | [27] |
| Pt-Ir/Pt/GOD | 0–21 | 0.9986 | [28] |
| Au/Pt-Nps/PANI/GOD/PU/PLGA | 0–14 | 0.998 | [46] |
| SUS/Pt/PANI/GOD/PVDF/Nafion | 0–20 | 0.9988 | [17] |
| GCE/Au-ZnO/GOD | 1–20 | [47] | |
| Pt-Ir/Nafion/GOD/PU/ PDMS/Heparin | 0–22.4 | 0.98 | [48] |
| AuMN/pTCA-GOx/ Nafion | 0.05–20 | 0.99 | [49] |
| SUS/Pt-Nps/Nafion/ GOD/SHPM-OS | 0–20 | 0.9988 | This study |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, L.; Jia, Z.; Liu, H.; Pi, X.; Zhou, J. Design of a Sandwich Hierarchically Porous Membrane with Oxygen Supplement Function for Implantable Glucose Sensor. Appl. Sci. 2020, 10, 2848. https://doi.org/10.3390/app10082848
Huang L, Jia Z, Liu H, Pi X, Zhou J. Design of a Sandwich Hierarchically Porous Membrane with Oxygen Supplement Function for Implantable Glucose Sensor. Applied Sciences. 2020; 10(8):2848. https://doi.org/10.3390/app10082848
Chicago/Turabian StyleHuang, Lijuan, Ziru Jia, Hongying Liu, Xitian Pi, and Jiawen Zhou. 2020. "Design of a Sandwich Hierarchically Porous Membrane with Oxygen Supplement Function for Implantable Glucose Sensor" Applied Sciences 10, no. 8: 2848. https://doi.org/10.3390/app10082848




