Relationship between Craniocervical Posture and Sagittal Position of the Mandible: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Selection Criteria
2.3. Data Extraction
2.4. Assessment of Risk of Bias
2.5. PICOs
- Population:
- Intervention:
- Comparison:
- Outcomes:
- Study design:
3. Results
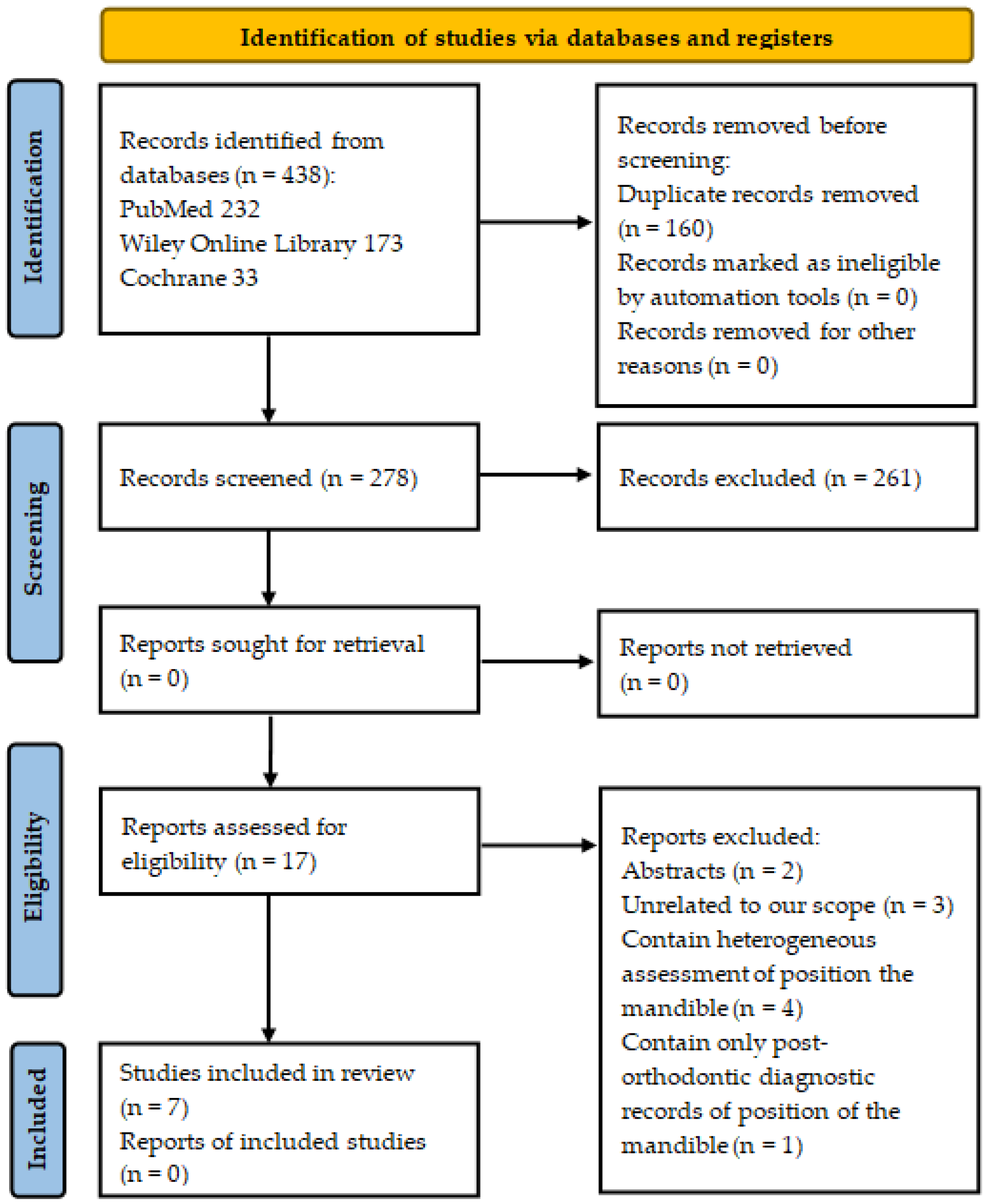
3.1. Search Results
3.2. Study Characteristics
3.2.1. Design
3.2.2. Outcome Measures
3.2.3. Risk of Bias
3.3. Main Outcomes
3.3.1. Craniocervical Posture and SN-RL Angle
3.3.2. Craniocervical Posture and SNB Angle
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Solow, B.; Tallgren, A. Head posture and craniofacial morphology. Am. J. Phys. Anthr. 1976, 44, 417–435. [Google Scholar] [CrossRef] [PubMed]
- Batistão, M.V.; Moreira, R.d.F.C.; Coury, H.J.C.G.; Salasar, L.E.B.; Sato, T.d.O. Prevalence of postural deviations and associated factors in children and adolescents: A cross-sectional study. Fisioter. Mov. 2016, 29, 777–786. [Google Scholar] [CrossRef] [Green Version]
- Szczygieł, E.; Fudacz, N.; Golec, J.; Golec, E. The impact of the position of the head on the functioning of the human body: A systematic review. Int. J. Occup. Med. Environ. Health 2020, 33, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, N.F.; Hassan, K.A.; Abdelmajeed, S.F.; Moustafa, I.M.; Silva, A.G. The Relationship Between Forward Head Posture and Neck Pain: A Systematic Review and Meta-Analysis. Curr. Rev. Musculoskelet. Med. 2019, 12, 562–577. [Google Scholar] [CrossRef]
- Ashok, K.; Purushothaman, V.K.; Muniandy, Y. Prevalence of Forward Head Posture in Electronic Gamers and Associated Factors. Int. J. Aging Health Mov. 2020, 2, 19–27. [Google Scholar]
- Verma, S.; Shaikh, J.; Mahato, R.; Sheth, M. Prevalence of forward head posture among 12–16 year old school going students—A cross sectional study. Appl. Med. Res. 2018, 4, 18. [Google Scholar] [CrossRef]
- Singh, I.; Kumar, K.K.; Raj, P.; Babu, R.H.; Pithani, N.; Thekiya, A.H. Cephalometric Evaluation of Natural Head Position in Lingayat Population of Karnataka. J. Pharm. Bioallied Sci. 2019, 11 (Suppl. 1), S59–S66. [Google Scholar] [CrossRef]
- Lee, Y.-J.; Park, J.-H.; Lee, S.-J.; Ryu, H.-M.; Kim, S.; Lee, Y.-J.; Yoon, H.-M.; Jang, S.-H.; Song, C.-H.; Kim, C.-H. Systematic Review of the Correlation Between Temporomandibular Disorder and Body Posture. J. Acupunct. Res. 2017, 34, 159–168. [Google Scholar] [CrossRef] [Green Version]
- Lippold, C.; Danesh, G.; Schilgen, M.; Drerup, B.; Hackenberg, L. Relationship between thoracic, lordotic, and pelvic inclination and craniofacial morphology in adults. Angle Orthod. 2006, 76, 779–785. [Google Scholar] [CrossRef]
- Abdolalizadeh, M.; Jahanimoghadam, F. Musculoskeletal Disorders in Dental Practitioners and Ergonomic Strategies. Anat. Sci. J. 2015, 12, 161–166. [Google Scholar]
- Elizagaray-Garcia, I.; Beltran-Alacreu, H.; Angulo-Díaz, S.; Garrigós-Pedrón, M.; Gil-Martínez, A. Chronic Primary Headache Subjects Have Greater Forward Head Posture than Asymptomatic and Episodic Primary Headache Sufferers: Systematic Review and Meta-analysis. Pain Med. 2020, 21, 2465–2480. [Google Scholar] [CrossRef] [PubMed]
- Alsheikho, H.O.; Jomah, D.H.; Younes, M.; Tizini, M.; Hassan, H.; Khalil, F. Evaluation of head and cervical spine posture after functional therapy with Twin-Block and Bionator appliances: A pilot randomized controlled trial. Cranio J. Craniomandib. Pract. 2021, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Patwardhan, A.G.; Khayatzadeh, S.; Havey, R.M.; Voronov, L.I.; Smith, Z.A.; Kalmanson, O.; Ghanayem, A.J.; Sears, W. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur. Spine J. 2018, 27, 25–38. [Google Scholar] [CrossRef] [PubMed]
- Lopatiene, K.; Smailiene, D.; Sidlauskiene, M.; Cekanauskas, E.; Valaikaite, R.; Pribuisiene, R. An Interdisciplinary Study of Orthodontic, Orthopedic, and Otorhinolaryngological Findings in 12–14-Year-Old Preorthodontic Children. Medicina 2013, 49, 75. [Google Scholar] [CrossRef] [Green Version]
- Darnell, M.W. A Proposed Chronology of Events for Forward Head Posture. J. Craniomandib. Pract. 1983, 1, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, A.M. Kopfhaltung und Kiefer. Z. Stomatol. 1926, 24, 669–744. [Google Scholar]
- Springate, S.D. A re-investigation of the relationship between head posture and craniofacial growth. Eur. J. Orthod. 2012, 34, 397–409. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kerbrat, A.; Schouman, T.; Decressain, D.; Rouch, P.; Attali, V. Interaction between posture and maxillomandibular deformity: A systematic review. Int. J. Oral Maxillofac. Surg. 2021, 51, 104–112. [Google Scholar] [CrossRef]
- Trevisan, M.E.; Weber, P.; Ries, L.G.K.; Corrêa, E.C.R. Relação da atividade elétrica dos músculos supra e infra-hióideos durante a deglutição e cefalometria. Rev. CEFAC 2013, 15, 895–903. [Google Scholar] [CrossRef] [Green Version]
- Lippold, C.; Danesh, G.; Hoppe, G.; Drerup, B.; Hackenberg, L. Sagittal Spinal Posture in Relation to Craniofacial Morphology. Angle Orthod. 2006, 76, 625–631. [Google Scholar] [CrossRef]
- Kulczynski, F.Z.; de Oliveira Andriola, F.; Deon, P.H.; da Silva Melo, D.A.; Pagnoncelli, R.M. Postural assessment in class III patients before and after orthognathic surgery. Oral Maxillofac. Surg. 2018, 22, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Hellsing, E.; McWilliam, J.; Reigo, T.; Spangfort, E. The relationship between craniofacial morphology, head posture and spinal curvature in 8, 11 and 15-year-old children. Eur. J. Orthod. 1987, 9, 254–264. [Google Scholar] [CrossRef] [PubMed]
- Moola, S.; Munn, Z.; Tufanaru, C.; Aromataris, E.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Qureshi, R.; Mattis, P.; et al. Chapter 7: Systematic reviews of etiology and risk. In Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, SA, Australia, 2020. [Google Scholar]
- Higgins, J.P.T.; Green, S.; Cochrane Collaboration. Cochrane Handbook for Systematic Reviews of Interventions; Wiley-Blackwell: Chichester, UK; Hoboken, NJ, USA, 2008. [Google Scholar]
- Sandoval, C.; Díaz, A.; Manríquez, G. Relationship between craniocervical posture and skeletal class: A statistical multivariate approach for studying Class II and Class III malocclusions. Cranio J. Craniomandib. Pract. 2019, 39, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Sun, X.; Chen, Y.; Hu, M.; Hou, X.; Liu, C. Relationships of sagittal skeletal discrepancy, natural head position, and craniocervical posture in young Chinese children. Cranio J. Craniomandib. Pract. 2016, 34, 155–162. [Google Scholar] [CrossRef] [PubMed]
- El Aouame, A.; Daoui, A.; El Quars, F.F. Nasal breathing and the vertical dimension: A cephalometric study. Int. Orthod. 2016, 14, 491–502. [Google Scholar] [CrossRef]
- Kamal, A.T.; Fida, M. Evaluation of cervical spine posture after functional therapy with twin-block appliances: A retrospective cohort study. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 656–661. [Google Scholar] [CrossRef] [Green Version]
- Vukicevic, V.; Petrovic, D. Relationship between head posture and parameters of sagittal position and length of jaws. Med. Pregl. 2016, 69, 288–293. [Google Scholar] [CrossRef]
- Chambi-Rocha, A.; Cabrera-Domínguez, M.E.; Domínguez-Reyes, A. Breathing mode influence on craniofacial development and head posture. J. Pediatr. 2018, 94, 123–130. [Google Scholar] [CrossRef]
- D’Attilio, M.; Caputi, S.; Epifania, E.; Festa, F.; Tecco, S. Evaluation of Cervical Posture of Children in Skeletal Class I, II, and III. Cranio J. Craniomandib. Pract. 2005, 23, 219–228. [Google Scholar] [CrossRef]
- Lin, X.; Edwards, S.P. Changes in natural head position in response to mandibular advancement. Br. J. Oral Maxillofac. Surg. 2017, 55, 471–475. [Google Scholar] [CrossRef]
- Smailienė, D.; Intienė, A.; Dobradziejutė, I.; Kušleika, G. Effect of Treatment with Twin-Block Appliances on Body Posture in Class II Malocclusion Subjects: A Prospective Clinical Study. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2017, 23, 343–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deda, M.R.d.C.; de Mello-Filho, F.V.; Xavier, S.P.; Trawitzki, L.V.V. Postura de cabeça nas deformidades dentofaciais classe II e classe III. Rev. CEFAC 2011, 14, 274–280. [Google Scholar] [CrossRef] [Green Version]
- Sabatucci, A.; Raffaeli, F.; Mastrovincenzo, M.; Luchetta, A.; Giannone, A.; Ciavarella, D. Breathing pattern and head posture: Changes in craniocervical angles. Minerva Stomatol. 2015, 64, 59–74. [Google Scholar] [PubMed]
- Kang, J.H.; Sung, J.; Song, Y.-M.; Kim, Y.-H. Heritability of the airway structure and head posture using twin study. J. Oral Rehabil. 2018, 45, 378–385. [Google Scholar] [CrossRef]
- Kim, M.S.; Cha, Y.-J.; Choi, J.-D. Correlation between forward head posture, respiratory functions, and respiratory accessory muscles in young adults. J. Back Musculoskelet. Rehabil. 2017, 30, 711–715. [Google Scholar] [CrossRef]
- Meiyappan, N.; Tamizharasi, S.; Senthilkumar, K.; Janardhanan, K. Natural head position: An overview. J. Pharm. BioAllied Sci. 2015, 7 (Suppl. 2), 424–427. [Google Scholar] [CrossRef]
- Wilke, J.; Krause, F.; Vogt, L.; Banzer, W. What Is Evidence-Based About Myofascial Chains: A Systematic Review. Arch. Phys. Med. Rehabil. 2016, 97, 454–461. [Google Scholar] [CrossRef]
- Kahn, S.; Ehrlich, P.; Feldman, M.; Sapolsky, R.; Wong, S. The Jaw Epidemic: Recognition, Origins, Cures, and Prevention. Bioscience 2020, 70, 759. [Google Scholar] [CrossRef]
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–122. [Google Scholar] [CrossRef]

| Database | No. of Papers | Keywords and Combinations of Them |
|---|---|---|
| PubMed | 35 | craniocervical posture OR head posture AND “Cephalometry” [Mesh] |
| 20 | craniocervical posture OR head posture AND cephalogram | |
| 48 | head position AND mandible AND three dimensional | |
| 14 | craniocervical posture AND cephalometry | |
| 5 | craniocervical posture OR head posture AND SNB | |
| 75 | head position AND mandible AND “Cephalometry” [Mesh] | |
| 5 | head and cervical spine posture AND “Cephalometry” [Mesh] | |
| 27 | head position AND mandible AND cephalogram | |
| 3 | craniocervical posture AND three dimensional | |
| Total | 232 | |
| Wiley Online Library | 8 | craniocervical posture AND cephalometry |
| 61 | head posture AND cephalometry | |
| 58 | craniocervical posture AND three dimensional | |
| 39 | head and cervical spine posture AND SNB | |
| 7 | craniocervical posture AND SNB | |
| Total | 173 | |
| Cochrane | 1 | craniocervical posture in All Text AND cephalometry in All Text-(Word variations have been searched) |
| 11 | head position in All Text AND cephalometry in All Text-(Word variations have been searched) | |
| 19 | head posture in All Text AND three dimensional in All Text-in Trials (Word variations have been searched) | |
| 1 | head and cervical spine posture in All Text AND SNB in All Text-in Trials (Word variations have been searched) | |
| 1 | head position in All Text AND mandible in All Text AND three dimensional in All Text-in Trials (Word variations have been searched) | |
| Total | 33 |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Clinical studies, evaluating craniocervical posture and mandible position in the sagittal plane | |
| Lateral cephalograms or head CT scans evaluated | Digital photographs evaluated |
| Studies with the control group or pre-orthodontic diagnostic records of craniocervical posture and position of the mandible | Studies with patients who have craniofacial syndromes or clefts, previous surgical, orthodontic, or physical therapy treatment |
| Studies of children and adults | |
| Articles in English and Lithuanian | |
| Articles published from January 2016 to January 2021 | |
| Full text available |
| Reference Line/Point | Description |
|---|---|
| SN | Nasion-sella line. Line through Nasion and Sella points |
| OPT | Odontoid process tangent. Posterior tangent to the odontoid process through the most posterior and inferior point on the corpus of the second cervical vertebra |
| CVT | Cervical tangent. Posterior tangent to the most posterior and inferior point on the corpus of the second and fourth cervical vertebra |
| RL | Ramus line. Tangent to the posterior border of the mandibular ramus |
| B | The deepest point on the anterior contour of the mandible |
| Parameter for craniocervical posture | |
| OPT-SN | Angle describes the upper craniocervical posture. It is formed by SN and OPT |
| CVT-SN | Angle describes the middle craniocervical posture. It is formed by SN and CVT |
| Parameter for position of the mandible | |
| SNB | Angle describes prognathism of the mandible. It is formed by SN and B |
| SN-RL | Angle describes rotation of the mandibular ramus in relation to cranium. It is formed by SN and RL |
| Author, Year, Journal | Design of a Study | Sample Description | Cephalometric Measurements | Main Outcomes (Mean Values and SD 1, Pearson’s r Value and p-Value at the Baseline) |
|---|---|---|---|---|
| Subjects classified by class of malocclusion | ||||
| Sandoval C. et al., 2019, CRANIO [25] | retrospective | 65 (34 for Class II and 31 for Class III); From 18 years (min 3) | OPT-SN; CVT-SN; SN-RL | OPT-SN: Class II (101.89° ± 7.95) > Class III (98.55° ± 8.49), n.s. 2 CVT-SN: Class II (105.49° ± 8.39) > Class III (102.88° ± 7.7), n.s. SN-RL: Class II (92.79° ± 5.50) > Class III (85.22°± 6.46), p < 0.001; SN-RL vs. CVT-SN: Class II (0.38, p < 0.05), Class III (−0.071, n.s.) |
| Liu Y. et al., 2016, CRANIO [26] | retrospective | 90 (30 for Class I, II, and II each); 11–14 years (min–max 4) | OPT-SN; CVT-SN; SN-RL | OPT-SN: Class II (98.22° ± 6.80) > Class III (95.55° ± 5.66) > Class I (95.42° ± 6.38), n.s. CVT-SN: Class II (106.00° ± 8.10) > Class III (101.52° ± 7.18), p < 0.05; Class I (103.03° ± 7.77), n.s. SN-RL: Class II (93.06° ± 4.11) > Class III (90.43° ± 3.79), p < 0.05, Class I (91.13° ± 5.06), n.s. |
| Vukićević V, et al., 2016, Med Pregl [29] | cross-sectional | 90 (30 for Class I, II, and II each); 8–14 years (min–max) | OPT-SN; SNB | OPT-SN: Class II (100.80° ± 11.10) > Class I (94.06° ± 1.81) and Class III (94.59° ± 1.80), p < 0.05 SNB: Class III (79.56° ± 0.69) > Class I (75.98° ± 0.52) and Class II (75.87° ± 0.31), p < 0.01 SNB vs OPT-SN: Class I (0.44, n.s.), Class II (−0.005, n.s.), Class III (0.179, n.s.) |
| Subjects classified by breathing pattern | ||||
| El Aouame A. et al., 2016, Int.Orthod. [27] | retrospective | 53 (23 for Oral breathers and 30 for Nasal breathers); Oral breathers: 16.8 years (mean), Nasal breathers: 14.4 years (mean) | OPT-SN; CVT-SN; SNB | OPT-SN: Nasal breathers (111.16° ± 8.3) > Oral breathers (110.17° ± 6.89), n.s. CVT-SN: Nasal breathers (115.26° ± 8.004) > Oral breathers (114.13 ± 7.75), n.s. SNB: Oral breathers (73.47° ± 4.86) > Nasal breathers (73.46° ± 3.57), n.s. |
| Chambi-Rocha A. et al., 2018, Jornal de Pediatria [30] | cross-sectional | 98 (56 for Oral breathers G1 and G2; 42 for Nasal breathers G1 and G2); G1: 7–9 years (min-max), G2: 10–16 years (min-max) | OPT-SN; CVT-SN; SNB | OPT-SN: Nasal breathers G1 (83.813° ± 9.94) > Oral breathers G1 (83.361° ± 12.15), n.s. and Oral breathers G2 (85.808° ± 9.72) > Nasal breathers G2 (79.944° ± 9.26), n.s. CVT-SN: Oral breathers G1 (106.194° ± 10.75) > Nasal breathers G1 (105.875° ± 7.94), n.s. and Oral breathers G2 (108.115° ± 10.22) > Nasal breathers G2 (101.444° ± 7.48), n.s. SNB: Nasal breathers G1 (77.500° ± 4.50) > Oral breathers G1 (77.353° ± 3.81), n.s. and Nasal breathers G2 (77.688° ± 2.65) > Oral breathers G2 (74.250° ± 3.18), n.s. |
| Subjects divided into ortho-treatment groups and controls | ||||
| Alsheikho H. O. et al., 2021, CRANIO [12] | A pilot randomized controlled trial | 30 (10 for Control, Twin Block, and Bionator each); 9–13 years (min–max) | OPT-SN; CVT-SN; SNB | OPT-SN: Control (99.69° ± 5.34) > Twin Block (99.26° ± 5.2) >Bionator (98.30° ± 5.9), n.s. CVT-SN: Control (105.9° ± 4.60) >Bionator (103.0° ± 5.22) > Twin Block (102.4° ± 5.3), n.s. SNB:Control (75.65° ± 1.15) >Bionator (75.37° ± 2.18) > Twin Block (74.91° ± 1.25), n.s. |
| Kamal A. T. et al., 2019, AJO-DO [28] | retrospective cohort | 60 (30 for Twin Block and Control each); Twin Block: 11.8 years (mean), Control: 11.6 years (mean) | OPT-SN; CVT-SN; SNB | Median values and interquartile range for: OPT-SN: Twin Block (105.0° (100.0–110.5)), Control (95.0° (88.0–101.5)) CVT-SN: Twin Block (104.5° (100.8–113.0)), Control (100.0° (96.7–108.2)) SNB: Twin Block (75.0° (73.0–77.0)), Control (77.0° (75.0–77.0)) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zokaitė, G.; Lopatienė, K.; Vasiliauskas, A.; Smailienė, D.; Trakinienė, G. Relationship between Craniocervical Posture and Sagittal Position of the Mandible: A Systematic Review. Appl. Sci. 2022, 12, 5331. https://doi.org/10.3390/app12115331
Zokaitė G, Lopatienė K, Vasiliauskas A, Smailienė D, Trakinienė G. Relationship between Craniocervical Posture and Sagittal Position of the Mandible: A Systematic Review. Applied Sciences. 2022; 12(11):5331. https://doi.org/10.3390/app12115331
Chicago/Turabian StyleZokaitė, Gintarė, Kristina Lopatienė, Arūnas Vasiliauskas, Dalia Smailienė, and Giedrė Trakinienė. 2022. "Relationship between Craniocervical Posture and Sagittal Position of the Mandible: A Systematic Review" Applied Sciences 12, no. 11: 5331. https://doi.org/10.3390/app12115331






