Abstract
Introduction: Diabetic foot is the infection, ulceration or destruction of the deep tissues of the foot in patients with diabetes mellitus. This pathology occurs when there are high levels of glucose in the blood, as well as other factors such as high blood pressure and hypercholesterolemia. These factors cause damage to the vessels and nerves, producing medium and long-term complications. This is a health problem that affects diabetic patients throughout their lives. Objective: To know the different techniques and strategies that allow to carry out an appropriate management of the diabetic foot. Methodology: A narrative review was carried out between November 2021 and July 2022 in the different databases of Pubmed (Medline), Scielo, Scopus and Web of Science (WOS), with a search string that combined the keywords derived from thesauri, namely Descriptors of Health Sciences (DeCS) and Medical Subject Headings (MeSH), combined with the Boolean operators “AND”, “NOT” and “NOT”. Results: After applying the article selection criteria and evaluating the quality of the methodology, a total of 22 articles were obtained. The results affirm the existence of promising therapies for the treatment of diabetic foot ulcers such as negative-pressure therapy and hyperbaric oxygen therapy. It is highlighted that the use of therapeutic footwear and health education are deficient aspects that must be reinforced. Conclusions: After comparing the different articles, it was possible to determine that negative-pressure therapy and hyperbaric oxygen therapy should be promoted as they are suitable for the treatment of diabetic foot ulcers. In addition, therapeutic footwear is a baseline in the diabetic foot approach. On the other hand, it is necessary to reinforce interdisciplinary work in this area and health education for patients suffering from this disease.
1. Introduction
Diabetic foot is known as the set of syndromes in which neuropathy, ischemia and infection cause tissue alterations or ulcers secondary to microtrauma. When talking about diabetic foot, we refer to a foot that has wounds or ulcers, typical of a person with diabetes. It arises from a dysfunction of the peripheral nerves in this type of patient [1].
Diabetic foot harms diabetic patients throughout their lives and is an important complication that worsens the patient’s clinical condition, in addition to reducing their quality of life and producing a great socioeconomic impact. The existing probabilities of amputation of a limb in diabetic patients are high [2].
For this reason, early diagnosis of this pathology is crucial, as is the identification and management of foot ulcers. In this way, morbidity, long hospital stays and amputations could be reduced. It must be approached from a multidisciplinary point of view as it is a health problem with a high prevalence and associated complications. It requires the involvement of various professions such as nursing, orthopedics, podiatry and medicine [1,2].
Diabetes mellitus (DM) is a set of metabolic disorders characterized by hyperglycemia, insufficient insulin secretion or excessive glucagon secretion. It is a non-communicable chronic disease of multifactorial origins. This pathology is the cause of the greatest disability and mortality in adults [2,3].
We can talk about two types of diabetes. Type 1 diabetes is characterized by an autoimmune disorder in which there is destruction of the beta cells of the pancreas, whereas in type 2 diabetes, there is a problem in the regulation of glucose due to the dysfunction of the beta cells of the pancreas and insulin resistance [2,3].
DM has intensified in recent decades, thus causing a global epidemic. Therefore, it has become one of the most frequent and serious medical conditions to face [2,3].
Unfortunately, a large percentage of diabetic patients will end up suffering from chronic complications of DM: retinopathy, nephropathy, peripheral neuropathy and atherosclerotic vascular disease. Among these complications is the diabetic foot, with a percentage of 15%. It is a serious complication of diabetes, which worsens the patient’s clinical condition, reduces their quality of life and generates a high socioeconomic impact [2,3].
Diabetic foot is defined as the infection, ulceration or destruction of the deep tissues of the foot, located in the lower extremities and related to neuropathy or peripheral arterial disease. Foot complications are the most costly and serious of DM; on the other hand, they involve more hospitalizations than any other complication [3].
A foot at risk is one that meets certain risk factors such as foot deformity, peripheral artery disease, anterior ulceration and amputation. These individuals are at increased risk. Other risk factors are male gender, diabetes for more than 10 years, advanced age of patients, high body mass index and other comorbidities such as retinopathy, diabetic peripheral neuropathy, peripheral vascular disease, glycosylated hemoglobin levels (HbA1C), high plantar pressure, heart failure, infections and inadequate foot self-care habits [2,3].
1.1. Epidemiology
The prevalence of diabetic foot varies according to age, gender and place of origin. In the diabetic population, the prevalence of foot ulcers is 4–10%. It is more common in older patients. Around 15% of diabetics will suffer from foot ulcers, and up to 85% of patients with ulcers will end up facing amputation [1,2].
The risk of developing a diabetic foot ulcer (DFU) and amputation increases with age and the duration of diabetes [1,2].
Among the most important risk factors for ulceration are diabetic neuropathy, peripheral arterial disease and foot trauma. Those people who manifest these factors must follow a medical control [1,4].
1.2. Clinic
Foot infections involve the most common soft tissue infection in the diabetic foot, which can cause osteomyelitis, amputation or death [1,2,3].
Among the clinical manifestations are ulcers, arthropathic foot or Charcot arthropathy, digital necrosis, cellulitis and lymphangitis, necrotizing soft-tissue infection and osteomyelitis [1,2].
1.3. Classification
There are several classification systems for diabetic foot. The best known systems are the Meggitt–Wagner classification, composed of six categories, and the University of Texas classification, which is the first type of two-dimensional classification. Similarly, there are other classifications such as the foot infection classification system (WIfI), in saving the extremity of the diabetic foot, or the PEDIS classification that analyzes the five parameters of irrigation, extension, depth, infection and sensitivity [2,5].
1.4. Diagnosis
When faced with a diabetic patient, the main thing is to assess the skin, since it is an indication of the existence of an ulcer or signs of infection. The examination consists of the inspection of the foot, appreciating its appearance, temperature, coloration, hyperkeratosis and joint deformities [1,2].
Diabetic people have atrophic and hairless skin as well as brittle nails that are prone to subungual hematomas. The skin and soft tissues of the sole of the foot have the characteristic of viscoelasticity. As a result of hyperglycemia, these skin tissues harden and progressively lose these properties, thus provoking a predisposition to hyperkeratosis in pressure areas, which can generate ulcers [1,2].
1.5. Prevention
The prevention of diabetic foot can be carried out through five basic elements: identification of the foot at risk; regular inspection and examination; patient, family and health-care provider education; use of adequate footwear; and treatment of pre-ulcerative signs [2,5].
1.6. Treatment
Antibiotic treatment alone is not enough to eliminate the infectious process. Key to the treatment of diabetic foot ulcers are wound debridement, infection management, revascularization procedures and ulcer offloading. There are also a few complementary therapies that have had positive results such as hyperbaric oxygen therapy, the use of advanced wound-healing products and negative-pressure wound therapy (TPWT) [2,5].
The objective of this study is to demonstrate and update the management of diabetic foot in patients older than 65 years. In the same way, it is pursued to analyze the knowledge in health education and self-care practices as objectives towards the patient. We also want to analyze TPWT and hyperbaric oxygen therapy (HBOT) for the treatment of DFUs, together with the benefits of therapeutic footwear in diabetic foot.
2. Materials and Methods
The preparation of this work was carried out through a systematic bibliographic review of the articles found by searching the following databases: Medline/Pubmed, WOS, Scielo, Scopus and Google Scholar. To find the best possible scientific evidence, a series of inclusion and exclusion criteria were applied.
The keywords for this review are: Diabetic foot, Pressure ulcer, Aged, Diabetes mellitus, Feet diabetic, foot ulcer diabetic, Bed sore, Pressure sore, Elderly and Glucose intolerance. To carry out the bibliographic search, different keywords in English were used, such as: “Diabetic foot”, “Pressure ulcer”, “Aged”, “Diabetes mellitus”, “Feet diabetic”, “foot ulcer diabetic”, “Bed sore” “Pressure sore”, “Elderly” and “Glucose intolerance”. These have been validated by the DeCS and MeSH. Once selected, the corresponding Boolean operators were used: AND/OR, as well as the necessary parentheses and quotation marks. The final search string is as follows: (Feet diabetic OR Foot ulcer diabetic) AND (Bedsore OR Pressure sore) AND (Aged OR Elderly) AND (Diabetes mellitus OR Glucose intolerance). The criteria that were taken into account for the selection of the relevant studies were the following. Inclusion criteria: the period between 2015 and 2022; article type: article review and article research; field: medicine; English language; age: 65 years or older; and studies that provided scientific evidence justified by the level of indexing of articles in journals according to the latest certainties. Exclusion criteria: articles prior to 2015; language: not English; studies in which the population constituted minors; studies that did not provide scientific evidence justified by the level of indexing of articles in journals according to the latest certainties.
For the methodological evaluation of the individual studies and the detection of possible biases, the evaluation was carried out using the PEDro evaluation scale. This scale consists of 11 items, providing one point for each element that is fulfilled. The articles that obtained a score of 9–10 points have an excellent quality, those between 6 and 8 points have a good quality, those that obtained 4–5 points have an intermediate quality and, finally, those articles that obtained less than 4 points have a poor methodological quality article (Table A1) [6].
The Scottish Intercollegiate Guidelines Network classification was used in the data analysis and assessment of the levels of evidence, which focused on the quantitative analysis of systematic reviews and the reduction of systematic error. Although it took into account the quality of the methodology, it did not assess the scientific or technological reality of the recommendations (Table A2) [7].
3. Results
The research question was constructed following the PICO format (population/patient, intervention, comparator and outcomes/outcomes). Detailed as P (population): people older than 65 years with diabetes mellitus; I (intervention): techniques to prevent diabetic foot; C (comparison): not applicable; O (results): achieve the greatest possible evidence available. (Scheme 1).
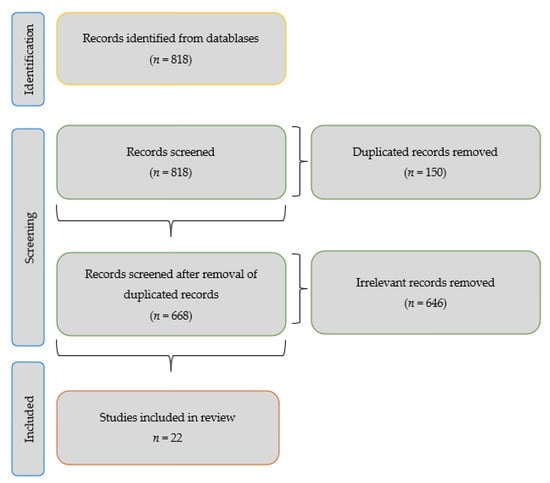
Scheme 1.
Flow diagram.
Below is a table that shows the search strategy used to select the 22 articles selected from the 5 databases, following the criteria of identified studies, duplicate studies, title, abstract, full text and valid studies of a definitive nature (Table 1). The total number of valid articles is summarized in Table A3.

Table 1.
Databases consulted.
In the studies by Fosuhemaa, Alshammari, Liu, Sari, Ramírez and Sigaud, it is shown in reference to the educational level that 117 patients have not received education, 62 patients attended basic education and 813 had primary education [8,9,10,11,12,13,14]. In the study by Alshmmari, Liu, Sari, Brilhante, Ramirez and Sigaud, it was observed that 281 people had a good level of knowledge, 127 people had a moderate level, 258 people had a poor level and 77 people had a low level [9,10,11,12,13,14]. In the study by Alshmmari, Liu, Sari and Ramirez, it was shown that 29 people have good foot care, 377 people had poor foot care and 4 people had inadequate foot care [9,10,11,13]. In the study by Alshammari, Liu, Sari and Brilhante, it was observed in relation to self-care practices that 154 of the participants performed a foot exam, 112 people applied cream, 147 people had dry feet and 119 users reported walking barefoot [9,10,11,12].
To assess the magnitude of self-care practices, the criteria used were diet, physical exercise, adherence to medication, self-monitoring of blood glucose and foot care. In Gebre’s article, it was observed that 10.3% of users had blood insulin control, 59.5% had poor glycemic control and 15.1% had adequate glucose-control practices. In addition, 67.1% of the patients had little knowledge about diabetes. Regarding food, 69.4% had a dietary plan. In the exercise, 63.5% of the patients presented adequate management, and 82.9% of users complied with proper foot care. On the other hand, 60.7% of users showed good self-care. Regarding medication, 22.6% of users were taking metformin, 63.1% were using insulin, 4% were using insulin plus metformin and 8.3% were using metformin plus enclamide [15]. In the article by Ehab, a positive attitude towards diabetes self-management practices was observed, with 20% self-monitoring their blood glucose levels. Their understanding of the importance of foot care and diabetes management was poor. A total of 20% of the patients acknowledged having a healthy diet, and 24% practiced physical exercise. Moreover, 56% of patients took medications, 36% used insulin alone, 36% took oral antidiabetic drugs and 28% used insulin plus metformin. Most adhered well to medications. Only 16% performed foot-care practices [16]. In the article by Dagmawitn, in general, the participants did not control their blood glucose levels on a regular basis, and those who had a glucometer at home reported measuring their sugar once every 4–6 weeks. There was an irregularity in sugar control; they stated that the lack of information and knowledge about the diet was one of the causes of their lack of compliance. In reference to exercise, most admitted not practicing physical exercise on a regular basis. In general, they claimed to comply more with the indications related to medications before other practices. Foot self-care was largely underrecognized [17]. In the article by Mohandas, it was observed that 92.3% had not tested their blood sugar in the last week, 3% measured their blood sugar for three days and 4.7% measured their blood sugar for one or two days. Moreover, 25% did not practice a diet, 39.3% did not practice physical activity even once day and 80.4% had not performed foot care on a single day in the last week [18].
In the study by Jira, after 10 sessions, a significant reduction in the lesion surface with complete healing was observed. After completing 20 sessions, healing was obtained in 70% of the patients, while 25% suffered amputations due to the extension of tissue necrosis and bone infection due to poor vascular status and significant metabolic alteration [19]. In the article by Vinkel, 53% of the patients received 30 sessions, of which 24% were referred more than once for the treatment of a diabetic foot ulcer, which indicates that the sessions were temporarily separated by two or more THOB cycles. A total of 40% complied with the treatment protocol. The median survival was 4.6 years, and the cumulative mortality was 1 and 5 years (14.2%) [20]. In the study by Chen-Yu, wounds treated with THOB and routine care after 10 sessions showed signs of healing. Within 20 sessions, the state of the wounds began to show clear improvements. Two weeks after therapy, they improved even more. Wounds treated with only routine care showed little change and early deterioration [21]. In the article by C. W. Chau, a clinical case of a patient with DFU with HBOT is presented. Following this therapy, the wound healed completely 2 months after starting therapy [22]. In these three studies, it was observed that 100 of the patients had arterial hypertension, 47 patients had cerebrovascular disease, 69 nephropathy and 55 others.
In the Borys study, patients with DM2 were treated with TPWT. In the TPWT group (those with noninfected neuropathic ulcers of area > 1 cm2 on one foot), the duration of the wound was 21.1 ± 24.7 weeks, and in the comparison group (those with ulcers of area ≤ 1 cm2 or Bilateral SLE) it was 14.4 ± 14.3 weeks. Regarding the wound area, the TPWT group was 15.7 ± 14.6 cm2 and the comparison group 2.9 ± 4.4 cm2. The reduction in wound area after 8 days was 1.1 ± 1.7 and 0.3 ± 0.7 cm2. However, the reduction in wound area after 8 days (%) was 10.2 ± 14.41 and 18.0 ± 15.7. Complete resolution of the ulcer occurred in one year in the NPWT group, 55.1%, and in the comparison group, 73.7%. On the other hand, the appearance of the ulcer occurred a year after its complete resolution, 29.2% and 31.3%. Major amputations did not occur in the TPWT group and only one in the comparison group. Finally, as for the deceased, in the TPWT group there was three and in the comparison group two [23]. The Lim et al. study is a retrospective analysis in which patients are treated at home with TPWT. Cure of the ulcer was observed in 61% of the patients. An additional split skin graft treatment was required in 8.5%, debridement in 8.5%, minor amputation in 9.3% and major amputation in 20.3%. The death rate was 0.9%. The need for VAC extension (negative-pressure-assisted closure) was observed in 8.5%. An unplanned readmission of 30 days was observed in 14.8%. Lastly, a one-year survival rate was observed in 89% [24]. In the article by Liu S, a systematic review in which the Cochran library, Medline, Embase, Ovid and Chinese Biological medicine databases were searched, the following results were obtained. Compared to standard dressings, TPWT had a higher rate of complete ulcer healing, shorter healing time and a greater reduction in ulcer depth. The amputation rate was lower. It also had no incidence of treatment-related adverse effects [25]. The article by Z Liu et al., a systematic review in which the databases the Cochrane, Ovid Medline, central and Ovid Embase databases were searched, compared to standard dressings, TPWT was found to have a higher healing rate, shorter time and greater efficacy in postoperative wound healing [26].
In the article by B. J. Zwaferink, the plantar pressures of patients are measured during a walk. They use four shoe conditions. The first concept A (Shoe-A; Insole A) is based on science, made by hand and with optimization by plantar pressure of the shoe. Condition B (Insole B) uses a barefoot plantar pressure, and the design and manufacture are by a computer focused on the shape of the foot in 3D. Condition C (Insole C) is based on an insole that uses the pressure barefoot and in-shoe plantar, and the design and optimization are by a computer based on the shape of the foot in 3D. All shoe concepts showed lower plantar metatarsal head pressures relative to therapeutic shoes; the reduction was from 17% to 53%. The mean number of rounds of shoe modification required by the patient to achieve the pressure criterion for optimization was 0.6 for shoe A, 0.8 for insole A and 1.3 for insole B. Insole B had the highest score for walking comfort at 7.2 and shoe fit at 7.7. Regarding the weight of the footwear, 8.3 was observed for the C insole and in the appearance of the footwear and 6.9 for the A footwear [27]. In the article by López-Moral, patients with a plantar ulcer were randomly assigned into two groups: therapeutic shoes with a semi-rigid sole (control) or therapeutic shoes with a rigid tilting sole (experimental). In A, 23% of patients in the experimental group and 64% in the control group had recurrence. In the control group, 37.5% had recurrence in the first metatarsal head, 12.5% in the second metatarsal head, 6.25% in the third metatarsal head, 25% in the fourth metatarsal head, 12.5% recurred in the interphalangeal joint of the hallux and 6.25% in the head of the fifth metatarsal. However, in the experimental group, 16.6% of the patients had recurrence in the second metatarsal head, 33.3% in the third metatarsal head, 16.6% in the fourth metatarsal head and 33.3% in the fourth metatarsal head. In the head of the fifth metatarsal, the relative risk reduction in the use of the rigid rocker sole compared to the semi-rigid was 64%. The number needed to treat was 2.43 [28]. In the article by Caroline et al., patients wore an innovative insole system that measured plantar pressure in their shoe on a daily basis for the duration of the study. In the intervention group, the intelligent insole system consisted of a watch that alerted when excessive pressure was detected, and in the control group a watch that did not alert was used. Regarding the results, a reduction in the recurrence of diabetic foot ulcers is observed through this insole system. Diabetic foot ulcer recurrence at the 18-month follow-up was reduced by 71%. There was a recurrence of the ulcer in patients with a daily use of this device of 86%, 17% ulcerated. At 18 months, 68% of patients in the control group and 78% in the intervention group were ulcer-free. The time to ulceration was prolonged in patients with the active device. No significant change was observed in the decrease in the number of patients who had re-ulceration [29].
4. Discussion
Several authors conclude that the majority of the population has little knowledge about diabetic foot disease, as well as its consequences and the importance of foot care. According to Fosuhemaa, patients have good knowledge of their disease but not about complications [8]. However, Alshammari found that the surveyed population had some knowledge and practice regarding diabetic foot and foot care but had a poor attitude toward foot care [9]. On the other hand, Sigaud affirms that the people surveyed have poor knowledge as a result of the fact that the information received was incomplete, highlighting the non-inspection of the feet by the doctor [14].
According to Brilhante, the patients with the highest level of knowledge were the ones who most adhered to self-care practices [12]. On the other hand, Sari also considers age, educational level, anxiety about diabetes and family support as predictors of self-care [11]. In addition, Ramirez included the age group, data collection sites, level of schooling, marital status, gender and health education [13]. In general, most authors agree that there is a correlation between the level of knowledge and self-care practices. In other words, patients with a moderate level of knowledge have a greater tendency to carry out self-care practices.
Regarding the education received, according to Fosuhemaa, it focused a lot on medication and dietary aspects and less on foot-care activities [8]. On the other hand, Alshammari et al. found in their study that few patients received formal education about the foot and its care [9]. Furthermore, Liu concluded that foot-specific education was poorly implemented [10]. These studies advocate the creation of programs that provide education on diabetes, its complications and foot care as a preventive method, with the aim of improving knowledge and self-care practices.
One of the ways to obtain information about the health status of patients is to assess their self-management practices. Focusing on aspects of glycemic control, diet, exercise and medication adherence. In general, the self-care practices analyzed were deficient. In the case of Gebre et al., blood glucose control stands out as the deficient aspect in the practice of self-care [15]. However, Mohandas highlights diet as the deficient factor [18]. On the contrary, in the case of Dagmawit, it was determined that patients have good adherence to drug recommendations before any other type of recommendation [17]. Yet in the study by Ehab, despite the failure in self-care in all aspects, patients had a positive attitude towards self-control practices; the problem is the lack of knowledge as a result of the lack of educational programs about self-control of diabetes [16].
Hyperbaric oxygen therapy is a therapeutic procedure used in the treatment of diabetic foot. In both studies, the results show positive evidence resulting from this therapy. Jira observed a significant reduction in the surface of the lesion with complete healing after 10 sessions of this therapy. These reduction and healing results improve after 20 sessions [19]. In contrast, Chen-Yu suggests that a minimum of 20 HBOT sessions is necessary to optimize the beneficial effects. After 10 sessions of treatment, signs of healing are already shown, but it is at 20 sessions when clear improvements are already observed in the wounds [21]. On the other hand, C. W. Chau presented a clinical case of a patient with DFU being treated with HBOT, determining that it is worth promoting this therapy as a short-term treatment for DFUs, but as a long-term treatment, more experience and evaluation are necessary. [22]. However, although Jira et al. determined that it is an advance for the management of foot injuries, they stated that it remains difficult to evaluate due to the absence of a control group of patients treated with a conventional method before HBOT [19]. This was the case of Vinkel, who supported the need for a large-scale randomized controlled trial to define a target group of patients with DFUs sensitive to THOB [20].
TPWT is an effective form of treatment for diabetic foot ulcers. It has been associated with fewer amputations and a higher rate of healing. Borys et al. found NPWT to be suitable for the treatment of non-ischemic, non-infected, neuropathic plantar ulcers in patients with type 2 diabetes mellitus. Wound healing was achieved in 55% of patients [23]. In contrast, Lim et al. show that 61% of patients healed DFUs with TPWT performed at home [24]. Both Z. Liu and Lui S. confirmed that TPWT has better results in terms of the healing rate and healing time compared to standard dressings [25,26]. However Liu S. states that further robust RCT studies are needed to support this treatment [25].
As for therapeutic footwear, several studies agree on its beneficial effects on patients with diabetic foot. In these studies, several models of insoles and different footwear are proposed, but they all reach the same conclusion: therapeutic footwear is a line in the treatment and prevention of diabetic foot. B. J. Zwaferink et al. show the efficacy of a science-based approach and measurement of plantar pressures for the creation of customized footwear to decrease maximum plantar pressures [27]. For López-Moral, the appropriate therapeutic footwear is the one that consists of a rigid tilting insole in the recurrence of DFUs [28]. In contrast to Carolina, who presents an innovative system of an intelligent insole that measures the plantar pressure in one’s footwear on a daily basis, this template decreases the recurrence of DFUs [29].
In view of the lack of a specific drug-sustained release system that responds to chronic diabetic foot wounds, hydrogel dressings based on the dynamic double bond of the Schiff base and phenylboronate ester were constructed. This demonstrated that the hydrogel promotes wound healing by reducing inflammation and enhancing angiogenesis in a type II diabetic foot model [30,31].
5. Conclusions
In relation to the main objective of evidencing the management of diabetic foot in patients over 65 years of age, it has been proven that there are promising therapies for its treatment such as negative-pressure therapy and hyperbaric oxygen therapy. In addition, therapeutic footwear and health education are important aspects that should be reinforced. Regarding the analysis of knowledge in health education and self-care practices of diabetic patients, it has been shown that the diabetic population has a low level of knowledge about their disease; this may be caused by educational level, age, family support or the education they receive. As a result, self-care practices are poor. For this reason, it is urgent to establish programs in which education is imparted and thus improve self-care knowledge and practices. In addition, after the analysis of negative-pressure therapy and hyperbaric oxygen therapy for the treatment of DFU, promising results have been obtained. As for TPWT, it was shown to be an effective, safe and beneficial therapy for the treatment of UPD. Compared to standard dressings, it has better results in terms of healing. On the other hand, THOB is an advance for the management of diabetic foot injuries, since it promotes healing and reduces the rate of amputation. Likewise, after studying the benefits of therapeutic footwear, it has been concluded that it has beneficial effects on the health of diabetic patients. Footwear is a key factor in the treatment and prevention of DFUs. Although several models of insoles and footwear are observed in these studies, they all affirm the need to use therapeutic footwear for this type of patient.
Author Contributions
Conceptualization, B.G.-M. and V.G.T.; methodology, Á.A.-P.; software, B.G.-M. and M.L.-S.; validation, B.G.-M., J.J.-P.; P.C.-M. and Á.A.-P.; formal analysis, Á.A.-P.; investigation, J.J.-P. and Á.A.-P.; resources, P.C.-M.; data curation, B.G.-M.; writing—original draft preparation, Á.A.-P.; writing—review and editing, Á.A.-P.; visualization, B.G.-M.; supervision, Á.A.-P.; project administration, Á.A.-P. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| DFU | diabetic foot ulcer |
| DM | diabetes mellitus |
| TPWT | negative-pressure wound therapy |
| THOB | hyperbaric oxygen therapy |
Appendix A

Table A1.
PEDro Evaluation Scale—Articles Table.
Table A1.
PEDro Evaluation Scale—Articles Table.
| Article Criteria | Alyssa M. F. et al., 2018 | Mateo L. M. et al., 2019 | Carolina A. A. et al., 2019 |
|---|---|---|---|
| The selection criteria are specified. | YES | YES | YES |
| Subjects were randomly assigned to groups. | YES | YES | YES |
| The allocation was hidden. | NO | NO | NO |
| The groups were similar with respect to the most important indicators. | YES | YES | YES |
| All subjects were blinded. | NO | NO | NO |
| All individuals administering therapy were blinded. | NO | NO | NO |
| All assessors were blinded. | NO | NO | NO |
| At least one of the key results was obtained in more than 85% of the subjects. | YES | YES | YES |
| Results for all subjects were presented. | YES | YES | YES |
| Comparisons of at least one key outcome were obtained. | YES | YES | YES |
| The study provides point and variability measures for at least one key outcome. | NO | YES | YES |
| Result | 7 | 7 | 7 |

Table A2.
Scottish Intercollegiate Guidelines Network (SIGN).
Table A2.
Scottish Intercollegiate Guidelines Network (SIGN).
| Item Criteria | Item/Criterion/Description | Item |
|---|---|---|
| Experimental (randomized controlled trials) | 1++ Meta-analysis of RCTs and SRs of high-quality RCTs or RCTs with very low risk of bias | Carolina A. A. et al., 2019. |
| 1+ Meta-analysis of RCTs and SRs of well-conducted RCTs or RCTs with low risk of bias | Mateo L. M. et al., 2019. | |
| 1− Meta-analysis of RCTs and SRs of RCTs or RCTs with high risk of bias | Alyssa M. F. et al., 2018. | |
| Observational Analytics (cases and controls or cohorts) | 2++ High-quality SR of case–control studies, or high-quality case–control studies or cohorts with very low risk of confounding, bias, or chance and a probability that the relationship is causal. | AG Sigaud Brust et al., 2017. |
| 2+ Cohort or case–control studies or studies of well-conducted diagnostic tests with low risk of bias and with a moderate probability of establishing a causal relationship. | Jerome Patry et al., 2021. | |
| 2 Cohort or case–control studies with high risk of bias. | Jerome Patry et al., 2020. | |
| Descriptive | 3. Non-analytical studies, for example, case series or case descriptions. | Claudia Ramirez-Perdomo et al., 2019. |
| 4. Expert opinion. | Zainab J. Alshammari et al., 2019. |

Table A3.
Selected Scientific Articles Table.
Table A3.
Selected Scientific Articles Table.
| Authors; Year | Type of Study | Patients | Conclusions |
|---|---|---|---|
| Fosuhemaa et al., 2021 [8] | Applied phenomenological study | 20 people who had been diagnosed with diabetes for at least the last 6 months. | Patients with diabetes were aware of this disease but not about its complications. Foot-care practices are essential for the early detection and reduction of disabilities associated with foot ulcers. Diabetes education should promote self-management practices, specifically foot care and clear dietary guidelines. |
| Alshmmari et al., 2019 [9] | Descriptive cross-sectional study | 368 diabetic patients constituting 11 men and 257 women. | A high percentage of the population had good foot-care knowledge and practice but a poor attitude. It claims the need for an awareness program for patients to improve their knowledge and self-care practices and adopt a positive attitude. |
| Liu et al., 2020 [10] | Cross-sectional quantitative study | 200 patients with diabetes were recruited from the endocrinology clinic of a tertiary hospital in Beijing. | People with diabetes have low levels of knowledge about foot care. This exposes the need to educate patients in a more optimal way. |
| Sari et al., 2020 [11] | Transversal study | 546 people. | Foot care in Indonesia is insufficient. This study shows that age, educational level, diabetes distress, family support and foot self-care knowledge are predictors of foot self-care behavior in Indonesia. |
| Brilhante et al., 2020 [12] | Cross-sectional descriptive study | 197 patients. | There is a relationship between the level of knowledge and the self-care practices carried out. |
| Ramirez et al., 2019 [13] | Descriptive study of transverse cut | 304 people with type 2 diabetes. | The results on diabetic foot prevention knowledge and practices are not very encouraging. Therefore, primary care programs are crucial, in which nurses offer effective education to correct the behavior of people with diabetes mellitus. |
| Sigaud et al., 2017 [14] | Observational, descriptive cross-sectional study | 228 participants, of whom 54.4 were women, 52.2 were over 60 years old and 42.1 had a secondary education level. | Due to the low academic level of the population, the lack of interest and the short time of the consultations, foot checks are not carried out or certain recommendations are not taken into account. For this reason, the integration of national programs on the care, education and continuous evaluation of the feet in diabetic patients is important. |
| Gebre et al., 2019 [15] | Cross-sectional study | 252 participants. | The self-care practices of the patients in this study were poor. Control of blood glucose tests for self-care practice was poor, but foot care was relatively good. |
| Ehab et al., 2019 [16] | Qualitative study | 25 interviews with 12 male and 13 female patients. | Iraqi diabetic patients’ self-care practices are inadequate. The main obstacle was the lack of knowledge as a result of the lack of educational programs on diabetes self-management. |
| Dagmawit T. et al., 2017 [17] | Qualitative study | 13 interviews with patients who had diabetes for at least 5 years. | Self-care in terms of guidance and support is poor. Improving patient education and diabetes clinics to provide better care practices and to prevent complications are paramount. |
| Mohandas et al., 2018 [18] | Transversal study | Diabetic patients older than 20 years, resident in Nand Nagri for more than 6 months. | The level of self-care practices in the patients in this study was low. There is an urgent need to create continuous care-education programs. |
| Jira et al., 2018 [19] | Retrospective study | 80 diabetic patients. | HBOT is an advance in the therapeutic management of diabetic foot lesions. |
| Vinkel et al., 2019 [20] | Cohort study | 148 patients. | The results of this study support the need for a randomized trial with a group of patients sensitive to the use of hyperbaric oxygen therapy with diabetic foot ulcers to investigate its use (HBOT) based on evidence and to reduce the risk of excessive use. |
| Chen-Yu C. et al., 2017 [21] | Prospective, randomized, open and controlled study | 38 patients with non-healing DFUs who were considered poor candidates for vascular surgery. | HBOT improved the healing rate of patients with DFU. The therapy reduced the risk of amputation. |
| C. W. Cheu et al., 2021 [22] | Clinical case | Patient with a diabetic foot injury who is treated with THOB. | This therapy was successful. It is worth proposing this treatment to patients with chronic UPD. |
| Borys et al., 2018 [23] | Prospective observational study | 75 patients with type 2 diabetes mellitus (DM2). | NPWT is suitable for the treatment of neuropathic, non-ischemic, non-infected plantar ulcers in patients with type 2 diabetes mellitus. |
| Lim et al., 2020 [24] | retrospective study | 118 patients with type 2 diabetes mellitus. | Home NPWT is effective in wound healing in diabetic patients. |
| Liu S. et al., 2017 [25] | Systematic review | Searches of the Cochran library, Medlin, Embase, Ovid and Chinese Biological medicine databases. | The results showed that NPWT is effective, safe and beneficial for the treatment of DFUs. |
| Liu Z. et al., 2018 [26] | Systematic review | Database searches: Cochrane, Ovid Medline, Central, Ovid Embase and EBSCOCINAHL. | NPWT is found to be effective for the treatment of DFUs compared to dressings in relation to the healing of debrided foot ulcers and postoperative amputation wounds in diabetic patients. |
| B. J. Zwaferink et al., 2020 [27] | Transversal study | 24 neuropathic patients with a high risk of foot ulceration. | It shows the effectiveness of a science-based approach and the measurement of plantar pressures for the creation of personalized footwear and thus achieves the reduction of maximum plantar pressures in diabetic patients at risk of ulceration. It supports its implementation to improve the diabetic patient’s footwear and thus prevent the risk of ulcer appearance. |
| López-Moral et al., 2019 [28] | Randomized controlled trial | 51 patients with diabetic neuropathy and a plantar ulcer were randomly assigned into 2 groups: therapeutic shoes with a semi-rigid sole (control) or therapeutic shoes with a rigid tilting sole (experimental). | There is evidence that the rigid tilting sole is more appropriate to attenuate the risk of plantar recurrence in patients with diabetes, polyneuropathy and a history of diabetic foot ulcer, compared to the semi-rigid tilting sole. |
| Carolina et al., 2019 [29] | Prospective study | 90 patients were selected and 58 carried out the study. | Beneficial effects are observed in the use of this innovative insole system for the reduction of the recurrence of foot ulcers in diabetic patients. |
References
- Del Castillo, T.R.A.; Fernández, L.J.A.; Del Castillo, T.F.J. Diabetic foot clinical practice guide. iMedPub J. 2014, 10, 1–17. [Google Scholar]
- Echeverría, G.V.; Sotomayor, L.C.; Norambuena, G.M.; Vidal, V.P.; Campos, G.A. Diabetic foot. Rev. Hosp. Clin. Univ. Chile 2016, 27, 207–219. Available online: https://www.redclinica.cl/Portals/0/Users/014/14/14/999.pdf (accessed on 10 February 2022).
- Seguel, G. Why should we worry about diabetic foot? Importance of the diabetic foot. Scielo 2013, 141, 1–3. Available online: https://scielo.conicyt.cl/scielo.php?pid=S003498872013001100014&script=sci_arttext&tlng=en (accessed on 10 February 2022).
- Paiva, M.O.; Rojas, S.N. Diabetic foot. Can we prevent it? Rev. Med. Clin. Condes. 2016, 27, 227–234. Available online: https://reader.elsevier.com/reader/sd/pii/S0716864016300128?token=89C76D7368B0329DA83F2219FCB151C7CBD0D5F2AB1D67524028056B8070B14CBE17C1365FA150C99E35B2FBB6A30760&originRegion=eu-west-1&originCreation=20211202143657 (accessed on 10 February 2022).
- Rincón, Y.; Gil, V.; Pacheco, J.; Benítez, I.; Sánchez, M. Diabetic foot evaluation and treatment. Scielo 2012, 10, 1–5. Available online: http://ve.scielo.org/scielo.php?script=sci_arttext&pid=S1690-31102012000300008 (accessed on 10 February 2022).
- Escala PEDro. Available online: https://pedro.org.au/spanish/resources/pedro-scale/ (accessed on 10 February 2022).
- SCImago (N.D) SJR. SCImago Journal and Country Rank. Available online: https://www.scimagojr.com/ (accessed on 10 February 2022).
- Fosuhema, J.I.; Dare, S.; Anyimah, O.B.; Kyei, B.P.; Kwadwo, H.T.; Elizabeth, N.J. Patients’ knowledge of diabetic foot complications and self-management practices in Ghana: A phenomenological study. PLoS ONE 2021, 16, e0256417. Available online: https://pubmed.ncbi.nlm.nih.gov/34432838/ (accessed on 10 February 2022).
- Alshammari, Z.J.; Alsaid, L.A.; Parameaswari, P.J.; Alzahrani, A.A. Attitude and knowledge about foot care among diabetic patients in Riyadh, Saudi Arabia. J. Fam. Med. Prim. Care 2019, 8, 2089–2094. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6618215/ (accessed on 10 February 2022). [CrossRef]
- Liu, J.; Lu, Q.; Pang, D.; Yang, P.; Jin, S.; Yuan, G.; Qi, X.; Wen, B.; Ding, Y.; Guo, X. Foot care education among patients with diabetes mellitus in china: A cross-sectional study. JWOCN 2020, 47, 276–283. Available online: https://pubmed.ncbi.nlm.nih.gov/32384530/ (accessed on 10 February 2022). [CrossRef]
- Sari, Y.; Upoyo, A.S.; Isworo, A.; Taufik, A.; Sumeru, A.; Anandari, D.; Sutrisna, E. Foot self-care behavior and its predictors in diabetic patients in Indonesia. BMC Res. Notes 2020, 13, 38. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6995081/ (accessed on 10 February 2022). [CrossRef]
- Batista, I.B.; Pascoal, L.M.; Gontijo, P.V.C.; Brito, P.D.S.; Sousa, M.A.D.; Santos, M.; Sousa, M.S. Association between knowledge and adherence to foot self-care practices performed by diabetics. Rev Bras Enferm. 2020, 73, e20190430. Available online: https://www.scielo.br/j/reben/a/y4tvqmV9RZr47mS5kNLhbxD/?lang=en (accessed on 10 February 2022). [CrossRef]
- Ramirez, P.C.; Perdomo, R.A.; Rodríguez, V.M. Knowledge and practices for foot prevention. Rev. Gaucha Enferm. 2019, 40, e20180161. Available online: https://www.scielo.br/j/rgenf/a/VjTCVf3YK3mybYQj9q9797f/?lang=pt (accessed on 10 February 2022).
- Sigaud-Brust, A.G.; JíménezChávez, J.D.; Espínola-Canata, M.; Ferreira-Gaona, M.I.; Díaz-Reissner, C.V. Diabetic foot prevention activities recommended by the doctor and carried out by patients treated in 2 reference hospitals. Rev. Salud Publica Parag. 2017, 7, 14–19. Available online: http://scielo.iics.una.py/scielo.php?pid=S2307-33492017000200014&script=sci_abstract (accessed on 10 February 2022). [CrossRef][Green Version]
- Gebre, D.M.; Mosisa, E.B.; Bayisa, W.G.; Fekadu, M.G.; Gamachu, L.B. Self-care practices regarding diabetes among diabetic patients in Western Ethiopia. BMC Res. Notes 2019, 12, 212. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6454742/ (accessed on 10 February 2022).
- Ehab, M.M.; Azmi, H.M.; Abdulrahman, H.S.; Shawky, N. Knowledge and Practice of Self-Care with Type 2 Diabetes Mellitus in Baghdad, Iraq: A Qualitative Study. Dovepress. 2019. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6301727/ (accessed on 10 February 2022).
- Dagmawit, T.; Yemane, B. Self-care practices among patients with diabetes in Addis Ababa: A qualitative study. PLoS ONE 2017, 12, e0169062. Available online: https://pubmed.ncbi.nlm.nih.gov/28045992/ (accessed on 10 February 2022).
- Mohandas, A.; Bhasin, S.K.; Upadhyay, M.; Madhu, S.V. Diabetes self-management activities among adults aged 20 years and older residing in a resettlement colony in East Delhi. Indian J. Public Health 2018, 62, 104–110. Available online: https://www.ijph.in/article.asp?issn=0019-557X;year=2018,volume=62;issue=2;spage=104;epage=110;aulast=Mohandas (accessed on 10 February 2022).
- Jira, M.; Ei, O.N.; Sekkach, Y.; Mekouar, F.; Amezyane, T. Hyperbaric oxygen therapy in the treatment of diabetic foot: Experience in the management of 80 cases in an internal medicine service. Pan Afr. Med. J. 2018, 30, 100. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6195238/ (accessed on 10 February 2022).
- Vinkel, J.; Lohse, N.; Hyldegaard, O. The clinical use of hyperbaric oxygen in the treatment of Danish patients with diabetic foot ulcers. Dan. Med. J. 2019, 66, A5528. Available online: https://pubmed.ncbi.nlm.nih.gov/30722823/ (accessed on 10 February 2022).
- Chen, C.-Y.; Wu, R.-W.; Hsu, M.-C.; Hsieh, C.-J.; Chou, M.-C. Adjuvant hyperbaric oxygen therapy for the healing of chronic diabetic foot ulcers. WOCN 2017, 44, 536–545. Available online: https://www.ingentaconnect.com/content/wk/won/2017/00000044/00000006/art00009 (accessed on 10 February 2022). [CrossRef]
- CWChau, J.; Leung, J.K.S. Case report: Treatment of chronic diabetic foot ulcer with Hyperbaric Oxygen Therapy. J. Orthop. 2021, 28, 1–5. Available online: https://www.scopus.com/record/display.uri?eid=2-s2.0-85114336657&origin=resultslist&sort=plf-f&src=s&st1=diabetic+foot+AND+aged+AND+management&nlo=&nlr=&nls=&sid=103657ce02cf7cdf93afbcd81e702315&sot=b&sdt=cl&cluster=scofreetoread%2c%22all%22%2ct%2bscopubyr%2c%222022%22%2ct%2c%222021%22%2ct%2c%222020%22%2ct%2c%222019%22%2ct%2c%222018%22%2ct%2c%222017%22%2ct%2bscolang%2c%22English%22%2ct%2c%22Spanish%22%2ct&sl=52&s=TITLE-ABS-KEY%28diabetic+foot+AND+aged+AND+management%29&relpos=65&citeCnt=0&searchTerm=&featureToggles=FEATURE_NEW_DOC_DETAILS_EXPORT:1 (accessed on 10 February 2022).
- Borys, S.; Hohendorff, J.; Koblik, T.; Witek, P.; Ludwig-Slomczynska, A.H.; Frankfurter, C.; Kiec-Wilk, B.; Malecki, M.T. Negative pressure wound therapy for the treatment of uninfected chronic neuropathic diabetic foot ulcerations: Short-term efficacy and long-term results. Endocrine 2018, 62, 611–616. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6244911/ (accessed on 10 February 2022). [CrossRef]
- Lim, K.; Lim, X.; Hong, Q.; Yong, E.; Chandrasekar, S.; Tan, G.W.; Lo, Z.J. Use of home negative pressure wound therapy in peripheral arterial disease and diabetic limb salvage. Int. Wound J. 2020, 17, 531–539. Available online: https://onlinelibrary.wiley.com/doi/10.1111/iwj.13307 (accessed on 10 February 2022). [CrossRef] [PubMed]
- Liu, S.; He, C.Z.; Cai, Y.T.; Xing, Q.P.; Guo, Y.Z.; Chen, Z.L.; Su, J.L.; Yang, L.P. Evaluation of negative pressure wound therapy for patients with diabetic foot ulcers: Systematic review and meta-analysis. Ther. Clin. Risk Manag. 2017, 13, 533. Available online: https://www.dovepress.com/getfile.php?fileID=36084 (accessed on 10 February 2022). [CrossRef] [PubMed]
- Liu, Z.; Dumville, J.C.; Hinchliffe, R.J.; Cullum, N.; Game, F.; Stubbs, N.; Sweeting, M.; Peinemann, F. Negative pressure wound therapy for the treatment of foot wounds in patients with diabetes mellitus. Cochrane Database Syst. Rev. 2018, 10, CD010318. Available online: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010318.pub3/full (accessed on 10 February 2022). [PubMed]
- Zwaferink, J.; Custers, W.; Paardekooper, I.; Berendsen, H.; Bus, S. Optimizing for the diabetic foot: Data-driven custom shoe concepts and their effect on pressure relief to prevent diabetic foot ulceration. PLoS ONE Collect. Drug Deliv. 2020, 23, e0224010. Available online: https://pubmed.ncbi.nlm.nih.gov/32324739/ (accessed on 10 February 2022).
- López-Moral, M.; Lázaro-Martínez, J.L.; García-Morales, E.; García-Álvarez, Y.; Álvaro-Afonso, F.J.; Molines-Barroso, R.J. Clinical efficacy of therapeutic footwear with rigid rocker soles in the prevention of recurrence in patients with diabetes mellitus and diabetic polyneuropathy: A randomized clinical trial. PLoS ONE 2019, 14, e0219537. Available online: https://pubmed.ncbi.nlm.nih.gov/31295292/ (accessed on 10 February 2022). [CrossRef]
- Abbott, C.A.; Chatwin, K.E.; Foden, P.; Hasan, A.N.; Sange, C.; Rajbhandari, S.M.; Reddy, P.N.; Vileikyte, L.; Bowling, F.L.; Boulton, A.J.; et al. Innovative Smart Insole System Reduces Diabetic Foot Ulcer Recurrence at Plantar Sites: A Prospective, Randomized, Proof-of-Concept Study. Lancet Digit. Health 2019, 1, e308–e318. Available online: https://pubmed.ncbi.nlm.nih.gov/33323253/ (accessed on 10 February 2022). [CrossRef]
- Liang, Y.; Li, M.; Yang, Y.; Qiao, L.; Xu, H.; Guo, B. pH/Glucose Dual Responsive Metformin Release Hydrogel Dressings with Adhesion and Self-Healing via Dual-Dynamic Bonding for Athletic Diabetic Foot Wound Healing. ACS Nano 2022, 16, 3194–3207. Available online: https://pubmed.ncbi.nlm.nih.gov/35099927/ (accessed on 10 February 2022). [CrossRef]
- Zhu, Y.; Cankova, Z.; Iwanaszko, M.; Lichtor, S.; Mrksich, M.; Ameer, G.A. Potent laminin-inspired antioxidant regenerative dressing accelerates wound healing in diabetes. Proc. Natl. Acad. Sci. USA 2018, 115, 6816–6821. Available online: https://pubmed.ncbi.nlm.nih.gov/29891655/ (accessed on 10 February 2022). [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).