Spectrophotometric Analysis of 3D Printed and Conventional Denture Base Resin after Immersion in Different Colouring Agents—An In Vitro Study
Abstract
1. Introduction
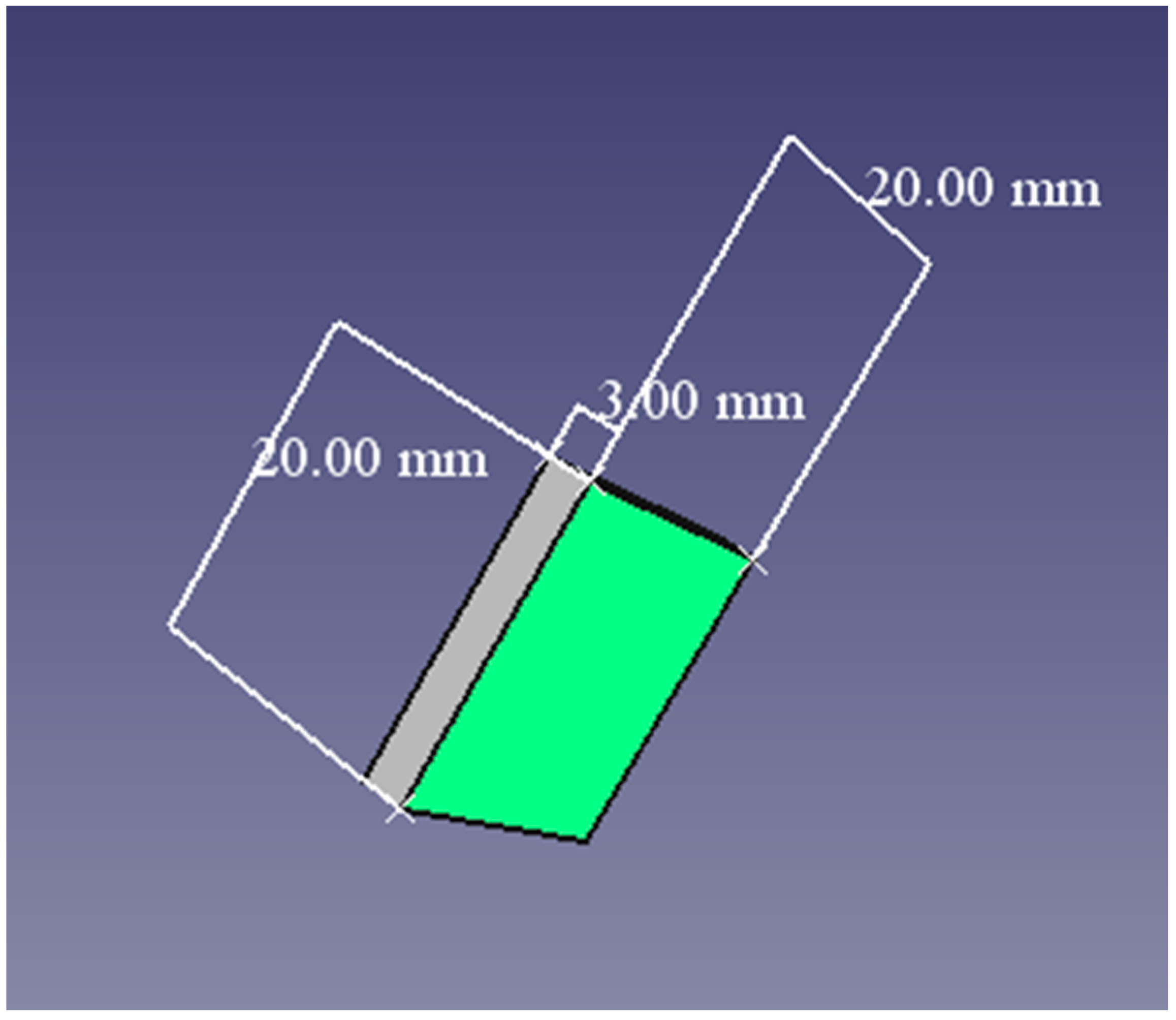
2. Materials and Methods
- Two-sample or independent t-test
3. Results
4. Discussion
5. Conclusions
- The red wine and coke had the most significant impact.
- The period with the highest colour changes was 21 days.
- There was a significant interaction between the periods of observation and the type of staining solution, as both groups of specimens demonstrated changes in colour stability at T1 compared to T3.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AM | additive manufacturing |
| CAD/CAM | computer-aided design/computer-aided manufacturing |
| PMMA | polymer polymethyl methacrylate |
| SLA | stereolithography |
| 3D | three-dimensional |
References
- Zampetti, P. Storia dell’implantologia. In Proceedings of the 1st National Congress of Multidisciplinary Implantology; Istituto Padre Monti: Saronno, Italy, 2004; p. 135. [Google Scholar]
- Apostolov, N. Role of Prosthetic Adhesives in Treatment with Goals Prostheses. Ph.D. Thesis, Sofia Medical University, Sofia, Bulgaria, 2015; pp. 28–30. [Google Scholar]
- Official Webpage of Artisticd. Available online: https://artisticd.com/dentures-throughout-history/ (accessed on 19 November 2022).
- Zafar, M.S. Prosthodontic Applications of Polymethyl Methacrylate (PMMA): An Update. Polymers 2020, 12, 2299. [Google Scholar] [CrossRef] [PubMed]
- Gandini, A.; Lacerda, T.M. Monomers and Macromolecular Materials from Renewable Resources: State of the Art and Perspectives. Molecules 2021, 27, 159. [Google Scholar] [CrossRef] [PubMed]
- Schneiderman, D.K.; Hillmyer, M.A. 50th Anniversary perspective: There is a great future in sustainable polymers. Macromolecules 2017, 50, 3733–3749. [Google Scholar] [CrossRef]
- John, G.; Nagarajan, S.; Vemula, P.K.; Silverman, J.R.; Pillai, C.K.S. Natural monomers: A mine for functional and sustainable materials–Occurrence, chemical modification and polymerization. Progr. Polym. Sci. 2019, 92, 158–209. [Google Scholar] [CrossRef]
- Scholten, B.V.; Moatsou, D.; Detrembleur, C.; Meier, M.A.R. Progress toward sustainable reversible deactivation radical polymerization. Macromol. Rapid Commun. 2020, 41, 2000266. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Antonietti, M. The sleeping giant: A polymer view on humic matter in synthesis and applications. Progr. Polym. Sci. 2020, 100, 101182. [Google Scholar] [CrossRef]
- Anadioti, E.; Musharbash, L.; Blatz, M.B.; Papavasiliou, G.; Kamposiora, P. 3D printed complete removable dental prostheses: A narrative review. BMC Oral Health 2020, 20, 343. [Google Scholar] [CrossRef]
- Gruber, S.; Kamnoedboon, P.; Özcan, M.; Srinivasan, M. CAD/CAM complete denture resins: An in vitro evaluation of color stability. J Prosthodont. 2021, 30, 430–439. [Google Scholar] [CrossRef]
- Stoqnova, D.; Peev, S.; Sapundzhiev, N. 3D Printed Models Application In Training of Endoscopically Navigated Maxillary Sinus Floor Augmentation Procedure. IJSR 2022, 11, 329–333. [Google Scholar] [CrossRef]
- Oguz, S.; Mutluay, M.M.; Dogan, O.M.; Bek, B. Color Change Evaluation of Denture Soft Lining Materials in Coffee and Tea. Dent. Mater. J. 2007, 26, 209–216. [Google Scholar] [CrossRef]
- Chan, K.H.S.; Mai, Y.; Kim, H.; Tong, K.C.T.; Ng, D.; Hsiao, J.C.M. Review: Resin Composite Filling. Materials 2010, 3, 1228–1243. [Google Scholar] [CrossRef]
- Paolone, G.; Formiga, S.; De Palma, F.; Abbruzzese, L.; Chirico, L.; Scolavino, S.; Goracci, C.; Cantatore, G.; Vichi, A. Color stability of resin-based composites: Staining procedures with liquids-A narrative review. J. Esthet. Restor. Dent. 2022, 6, 865–887. [Google Scholar] [CrossRef] [PubMed]
- Zhekov, J.; SAlexandrov Hr Kisov EFirkova, S. Arutyunov-Possibilities of CAD/CAM technology in splinting of periodontally damaged teeth—Scientific papers of the Union of Scientists in Bulgaria-Plovdiv. Ser. D. Med. Pharm. Dent. 2020, 14, 331–335. [Google Scholar]
- Gogushev, K.; Abadjiev, M. Conventional vs Digital Impression Technique for Manufacturing of Three-unit Zirconia Bridges: Clinical Time Efficiency. J. IMAB 2021, 27, 3765–3771. [Google Scholar] [CrossRef]
- Papathanasiou, I.; Papavasiliou, G.; Kamposiora, P.; Zoidis, P. Effect of staining solutions on color stability, gloss and surface roughness of removable partial dental prosthetic polymers. J. Prosthodont. 2021, 31, 65–71. [Google Scholar] [CrossRef]
- Chuchulska, B.; Hristov, I.; Dochev, B.; Raychev, R. Changes in the Surface Texture of Thermoplastic (Monomer-Free) Dental Materials Due to Some Minor Alterations in the Laboratory Protocol-Preliminary Study. Materials 2022, 15, 6633. [Google Scholar] [CrossRef]
- Ragain, J.C. A review of color science in dentistry: Shade matching in the contemporary dental practice. J. Dent. Oral Disord. Ther. 2016, 4, 1–5. [Google Scholar] [CrossRef]
- Chuchulska, B.; Zlatev, S. Linear Dimensional Change and Ultimate Tensile Strength of Polyamide Materials for Denture Bases. Polymers 2021, 13, 3446. [Google Scholar] [CrossRef]
- Aschheim, K.W. Esthetic Dentistry: A Clinical Approach to Techniques and Materials; Elsevier Health Science: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Dayan, C.; Guven, M.C.; Gencel, B.; Bural, C. A comparison of the color stability of conventional and CAD/CAM polymethyl methacrylate denture base materials. Acta Stomatol. Croat. 2019, 53, 158–167. [Google Scholar] [CrossRef]
- Kattadiyil, M.T.; Goodacre, C.J.; Baba, N.Z. CAD/CAM complete dentures: A review of two commercial fabrication systems. J. Calif. Dent. Assoc. 2013, 41, 407–416. [Google Scholar]
- Revilla-León, M.; Özcan, M. Additive manufacturing technologies used for processing polymers: Current status and potential application in prosthetic dentistry. J. Prosthodont. 2019, 28, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Hada, T.; Kanazawa, M.; Iwaki, M.; Arakida, T.; Soeda, Y.; Katheng, A.; Otake, R.; Minakuchi, S. Effect of printing direction on the accuracy of 3D-printed dentures using stereolithography technology. Materials 2020, 13, e3405. [Google Scholar] [CrossRef] [PubMed]
- Koh, E.S.; Cha, H.S.; Kim, T.H.; Ahn, J.S.; Lee, J.H. Color stability of three dimensional-printed denture teeth exposed to various colorants. J Korean Acad. Prosthodont. 2020, 58, 1–6. [Google Scholar] [CrossRef]
- Todorov, R.; Peev, T.; Zlatev, S. Shade guides used in the dental practice. J. IMAB 2020, 26, 3168–3173. [Google Scholar] [CrossRef]
- Sarafianou, A.; Iosifidou, S.; Papadopoulos, T.; Eliades, G. Color Stability and Degree of Cure of Direct Composite Restoratives After Accelerated Aging. Oper. Dent. 2007, 32, 406–411. [Google Scholar] [CrossRef]
- Yılmaz, M.N.; Gul, P. Susceptibility to discoloration of dental restorative materials containing dimethacrylate resin after bleaching. Odontology 2022. [Google Scholar] [CrossRef]
- Dimitrova, M.; Corsalini, M.; Kazakova, R.; Vlahova, A.; Barile, G.; Dell’Olio, F.; Tomova, Z.; Kazakov, S.; Capodiferro, S. Color Stability Determination of CAD/CAM Milled and 3D Printed Acrylic Resins for Denture Bases: A Narrative Review. J. Compos. Sci. 2022, 6, 201. [Google Scholar] [CrossRef]
- Babikir, M.; Gilada, M.W.; Fahmy, F.; AIsmail, I.; Alhajj, M.N.; Fadul, A.; Elasyouti, A. Effect of Commonly Consumed Beverages on Color Stability of Polymethyl Methacrylate Denture Base Material. Compend. Contin. Educ. Dent. 2019, 40, e1–e8. [Google Scholar]
- Hristov, I.L. Modern Analysis of Soft Rebasing Materials and Ways to Deal with Their Shortcomings. Ph.D. Thesis, Faculty of Dental Medicine, Plovdiv, Bulgaria, 2017. [Google Scholar]
- Öztürk, C.; Çelik, E.; Özden, A.N. Influence of bleaching agents on the color change and translucency of resin matrix ceramics. J. Esthet. Restor. Dent. 2020, 32, 530–535. [Google Scholar] [CrossRef]
- Waldemarin, R.F.; Terra, P.C.; Pinto, L.R.; Faot, F.; Camacho, G.B. Color change in acrylic resin processed in three ways after immersion in water, cola, coffee, mate and wine. Acta Odontológica Latinoam. 2013, 26, 138–143. [Google Scholar]
- Sari, M.E.; Koyutürk, A.E.; Çankaya, S. Color effect of frequently used food and beverage consumption of children on different filling materials. Turk. Klin. J. Dent. Sci. 2011, 17, 140–146. [Google Scholar]
- Official Web Page of NextDent. Available online: https://nextdent.com/products/denture-3dplus/ (accessed on 10 September 2022).
- Official Web Page of SpectroShade. Available online: https://spectroshade.us/products/spectroshade-micro-ii?variant=30872332364 (accessed on 14 September 2022).
- Al Amri, M.D.; Labban, N.; Alhijji, S.; Alamri, H.; Iskandar, M.; Platt, J.A. In vitro evaluation of translucency and color stability of CAD/CAM polymer-infiltrated ceramic materials after accelerated aging. J. Prosthodont. 2021, 30, 318–328. [Google Scholar] [CrossRef]
- Elsaka, S.; Taibah, S.; Elnaghy, A. Effect of staining beverages and bleaching on optical properties of a CAD/CAM nanohybrid and nanoceramic restorative material. BMC Oral Health 2022, 22, 96. [Google Scholar] [CrossRef] [PubMed]
- Official Webpage of Formlabs. Available online: https://formlabs.com/uk/store/materials/castable-wax-40-resin/ (accessed on 19 November 2022).
- Da Costa, G.C.; Aras, M.A.; Chalakkal, P. Shade guide for the fabrication of acrylic denture based on mucosal colour. J. Clin. Diagn. Res. 2017, 11, ZD12–ZD13. [Google Scholar] [CrossRef]
- Official Web Page of ISO. Available online: https://www.iso.org/standard/69046.html (accessed on 28 August 2022).
- Catelan, A.; Briso, A.; Sundfeld, R.H.; Goiato, M.; dos Santos, P.H. Color stability of sealed composite resin restorative materials after ultraviolet artificial aging and immersion in staining solutions. J. Prosthet. Dent. 2011, 105, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Singh, K.; Suvarna, S.; Agnihotri, Y.; Sahoo, S.; Kumar, P. Color stability of aesthetic restorative materials after exposure to commonly consumed beverages. Eur. J. Prosthodont. 2014, 2, 15–22. [Google Scholar] [CrossRef]
- Shin, J.W.; Kim, J.E.; Choi, Y.J.; Shin, S.H.; Nam, N.E.; Shim, J.S.; Lee, K.W. Evaluation of the Color Stability of 3D-Printed Crown and Bridge Materials against Various Sources of Discoloration: An In Vitro Study. Materials 2020, 13, 5359. [Google Scholar] [CrossRef]
- Dimitrova, M.; Chuchulska, B.; Zlatev, S.; Kazakova, R. Colour Stability of 3D-Printed and Prefabricated Denture Teeth after Immersion in Different Colouring Agents-An In Vitro Study. Polymers 2022, 14, 3125. [Google Scholar] [CrossRef]
- Faul, F.; Buchner, A. Power analysis for categorical methods. In Encyclopedia of Statistics in Behavioral Science; Everitt, B.S., Howell, D.C., Eds.; Wiley: Chichester, UK, 2005; pp. 1565–1570. [Google Scholar]
- Alp, G.; Johnston, W.M.; Yilmaz, B. Optical properties and surface roughness of prepolymerized poly(methyl methacrylate) denture base materials. J. Prosthet. Dent. 2018, 121, 347–352. [Google Scholar] [CrossRef]
- Mortazavi, H.; Baharvand, M.; Khodadoustan, A. Colors in tooth discoloration: A new classification and literature review. Int. J. Clin. Dent. 2014, 7, 17–28. [Google Scholar]
- Kerby, R.E.; Knobloch, L.A.; Schricker, S.; Gregg, B. Synthesis and evaluation of modified urethane dimethacrylate resins with reduced water sorption and solubility. Dent. Mater. 2009, 25, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Hipólito, A.C.; Barão, V.A.; Faverani, L.P.; Ferreira, M.B.; Assunção, W.G. Color degradation of acrylic resin denture teeth as a function of liquid diet: Ultra-violet-visible reflection analysis. J. Biomed. Opt. 2013, 18, 105005. [Google Scholar] [CrossRef] [PubMed]
- Sarkis, E. Color change of some aesthetic dental materials: Effect of immersion solutions and finishing of their surfaces. Saudi Dent. J. 2012, 24, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Gregorius, W.C.; Kattadiyil, M.T.; Goodacre, C.J.; Roggenkamp, C.L.; Powers, J.M.; Paravina, R.D. Effects of ageing and staining on color of acrylic resin denture teeth. J. Dent. 2012, 40, e47–e54. [Google Scholar] [CrossRef]
- Tango, R.N.; Todorović, A.; Stamenković, D.; Karasan, D.N.; Sailer, I.; Paravina, R.D. Effect of Staining and Aging on Translucency Parameter of CAD-CAM Materials. Acta Stomatol. Croat. 2021, 55, 2–9. [Google Scholar] [CrossRef]
- Zuo, W.; Feng, D.; Song, A.; Gong, H.; Zhu, S. Effects of organic-inorganic hybrid coating on the color stability of denture base resins. J. Prosthet. Dent. 2016, 115, 103–108. [Google Scholar] [CrossRef]
- Craig, R.G. Restorative Dental Materials, 12th ed.; The CV Mosby Co: St Louis, MO, USA, 2012; pp. 91–92, 125–162, 537–539. [Google Scholar]
- Mousavi, S.; Narimani, S.; Hekmatfar, S.; Jafari, K. Colour stability of various types of acrylic teeth exposed to coffee, tea and cola. J. Dent. Biomater. 2016, 3, 335. [Google Scholar]
- Imirzalioglu, P.; Karacaer, O.; Yilmaz, B.; Ozmen MSc, I. Color stability of denture acrylic resins and a soft lining material against tea, coffee, and nicotine. J. Prosthodont. 2010, 19, 118–124. [Google Scholar] [CrossRef]
- Barszczewska-Rybarek, I.M. Characterization of urethane-dimethacrylate derivatives as alternative monomers for the restorative composite matrix. Dent. Mater. 2014, 30, 1336–1344. [Google Scholar] [CrossRef]
- Soares-Geraldo, D.; Scaramucci, T.; Steagall, W., Jr.; Braga, S.R.; Sobral, M.A. Interaction between staining and degradation of a composite resin in contact with colored foods. Braz. Oral. Res. 2011, 25, 366–369. [Google Scholar] [CrossRef]
- Tanthanuch, S.; Kukiattrakoon, B.; Peerasukprasert, T.; Chanmanee, N.; Chaisomboonphun, P.; Rodklai, A. The effect of red and white wine on color changes of nanofilled and nanohybrid resin composites. Restor. Dent. Endod. 2016, 41, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Koksal, T.; Dikbas, I. Color Stability of Different Denture Teeth Materials against Various Staining Agents. Dent. Mater. J. 2008, 27, 139–144. [Google Scholar] [CrossRef]
- Ertas, E.; Gueler, A.U.; Yuecel, A.C.; Köprülü, H.; Güler, E. Color Stability of Resin Composites after Immersion in Different Drinks. Dent. Mater. J. 2006, 25, 371–376. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Roeder, L.B.; Lei, L.; Powers, J.M. Effect of Surface Roughness on Stain Resistance of Dental Resin Composites. J. Esthet. Restor. Dent. Off. Publ. Am. Acad. Esthet. Dent. 2005, 17, 102–108, Discussion 109. [Google Scholar] [CrossRef] [PubMed]



| Product | Composition | Detail | Manufacturer |
|---|---|---|---|
| NextDent Denture 3D+ | Methacrylate-based photopolymerized resin | 3D printing | NextDent, 3D Systems, Soesterberg, Netherlands |
| Vertex BasiQ 20 | PMMA | Heat curing | Vertex Dental, 3D Systems, Soesterberg, Netherlands |
| Type of Material | Period of Time (T) | Artificial Saliva ΔE (Mean) | Coffee ΔE (Mean) | Coca-Cola ΔE (Mean) | Red Wine ΔE (Mean) | SD (Standard Deviation) |
|---|---|---|---|---|---|---|
| NextDent Denture 3D+ | 7 days (T1) | 0.498 | 2.129 | 2.676 | 3.016 | 1.1160103 |
| Vertex BasiQ | 0.512 | 2.328 | 2.867 | 3.268 | 1.2170435 | |
| NextDent Denture 3D+ | 14 days (T2) | 0.471 | 2.194 | 2.722 | 3.163 | 1.1795063 |
| Vertex BasiQ | 0.484 | 2.576 | 2.966 | 3.508 | 1.3227450 | |
| NextDent Denture 3D+ | 21 days (T3) | 0.462 | 2.269 | 2.875 | 3.312 | 1.2535407 |
| Vertex BasiQ | 0.457 | 2.793 | 3.158 | 3.866 | 1.4764653 |
| Multiple Comparisons | ||||||
|---|---|---|---|---|---|---|
| Dependent Variable; ΔE Bonferroni Post-Hoc Test | ||||||
| (I) Period | (J) Period | Mean Difference (I-J) | Std. Error | P | 95% Confidence Interval | |
| Lower Bound | Upper Bound | |||||
| 7 | 14 | −0.098750 | 0.0685752 | 0.504 | −0.280817 | 0.083317 |
| 21 | −0.237250 * | 0.0685752 | 0.009 | −0.419317 | −0.055183 | |
| 14 | 7 | 0.098750 | 0.0685752 | 0.504 | −0.083317 | 0.280817 |
| 21 | −0.138500 | 0.0685752 | 0.178 | −0.320567 | 0.043567 | |
| 21 | 7 | 0.237250 * | 0.0685752 | 0.009 | 0.055183 | 0.419317 |
| 14 | 0.138500 | 0.0685752 | 0.178 | −0.043567 | 0.320567 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dimitrova, M.; Capodiferro, S.; Vlahova, A.; Kazakova, R.; Kazakov, S.; Barile, G.; Corsalini, M. Spectrophotometric Analysis of 3D Printed and Conventional Denture Base Resin after Immersion in Different Colouring Agents—An In Vitro Study. Appl. Sci. 2022, 12, 12560. https://doi.org/10.3390/app122412560
Dimitrova M, Capodiferro S, Vlahova A, Kazakova R, Kazakov S, Barile G, Corsalini M. Spectrophotometric Analysis of 3D Printed and Conventional Denture Base Resin after Immersion in Different Colouring Agents—An In Vitro Study. Applied Sciences. 2022; 12(24):12560. https://doi.org/10.3390/app122412560
Chicago/Turabian StyleDimitrova, Mariya, Saverio Capodiferro, Angelina Vlahova, Rada Kazakova, Stoyan Kazakov, Giuseppe Barile, and Massimo Corsalini. 2022. "Spectrophotometric Analysis of 3D Printed and Conventional Denture Base Resin after Immersion in Different Colouring Agents—An In Vitro Study" Applied Sciences 12, no. 24: 12560. https://doi.org/10.3390/app122412560
APA StyleDimitrova, M., Capodiferro, S., Vlahova, A., Kazakova, R., Kazakov, S., Barile, G., & Corsalini, M. (2022). Spectrophotometric Analysis of 3D Printed and Conventional Denture Base Resin after Immersion in Different Colouring Agents—An In Vitro Study. Applied Sciences, 12(24), 12560. https://doi.org/10.3390/app122412560









