In Vivo and In Vitro Accuracy Analysis of Static Computer-Assisted Implant Surgery in an Edentulous Patient
Abstract
:1. Introduction
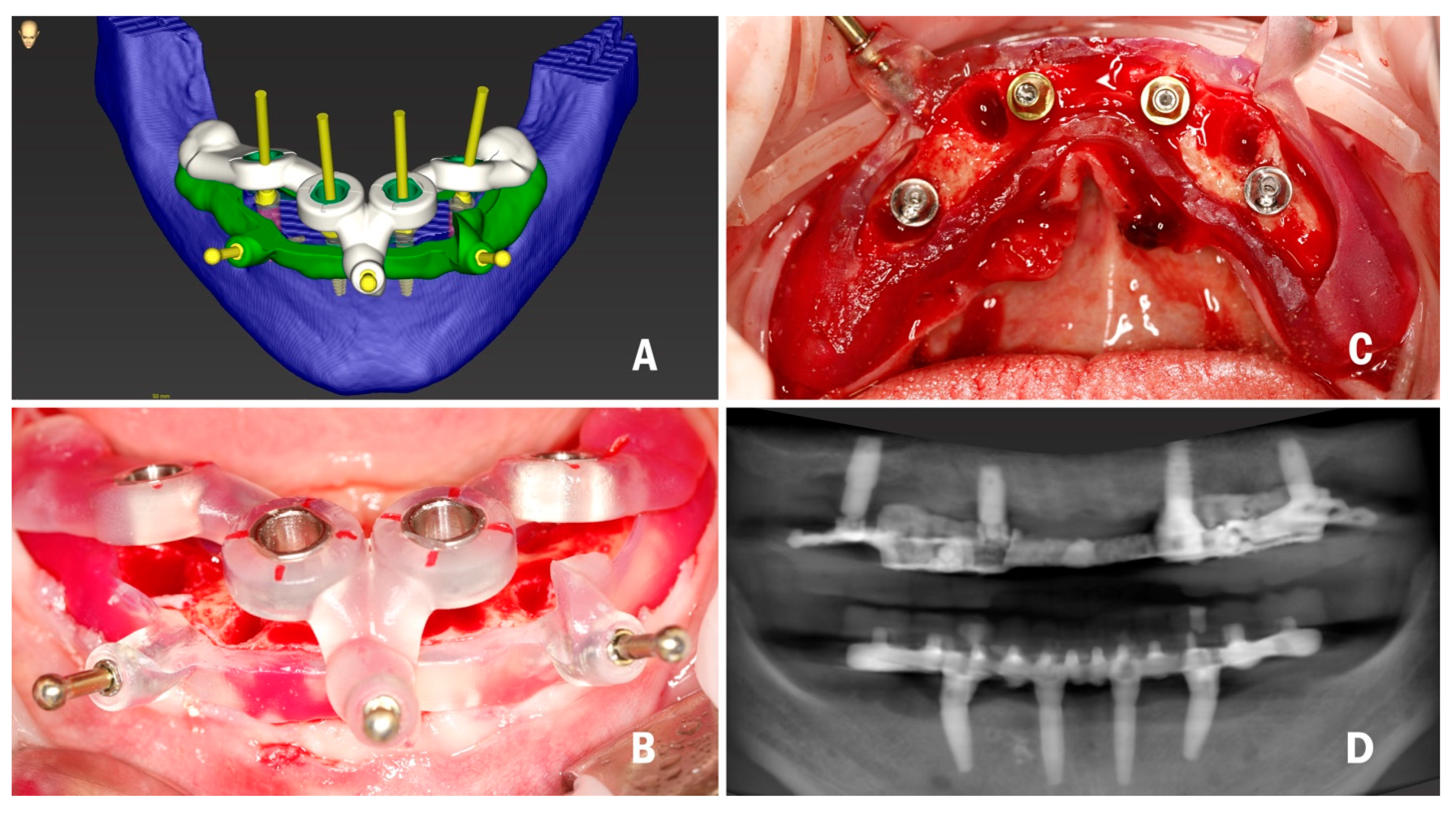
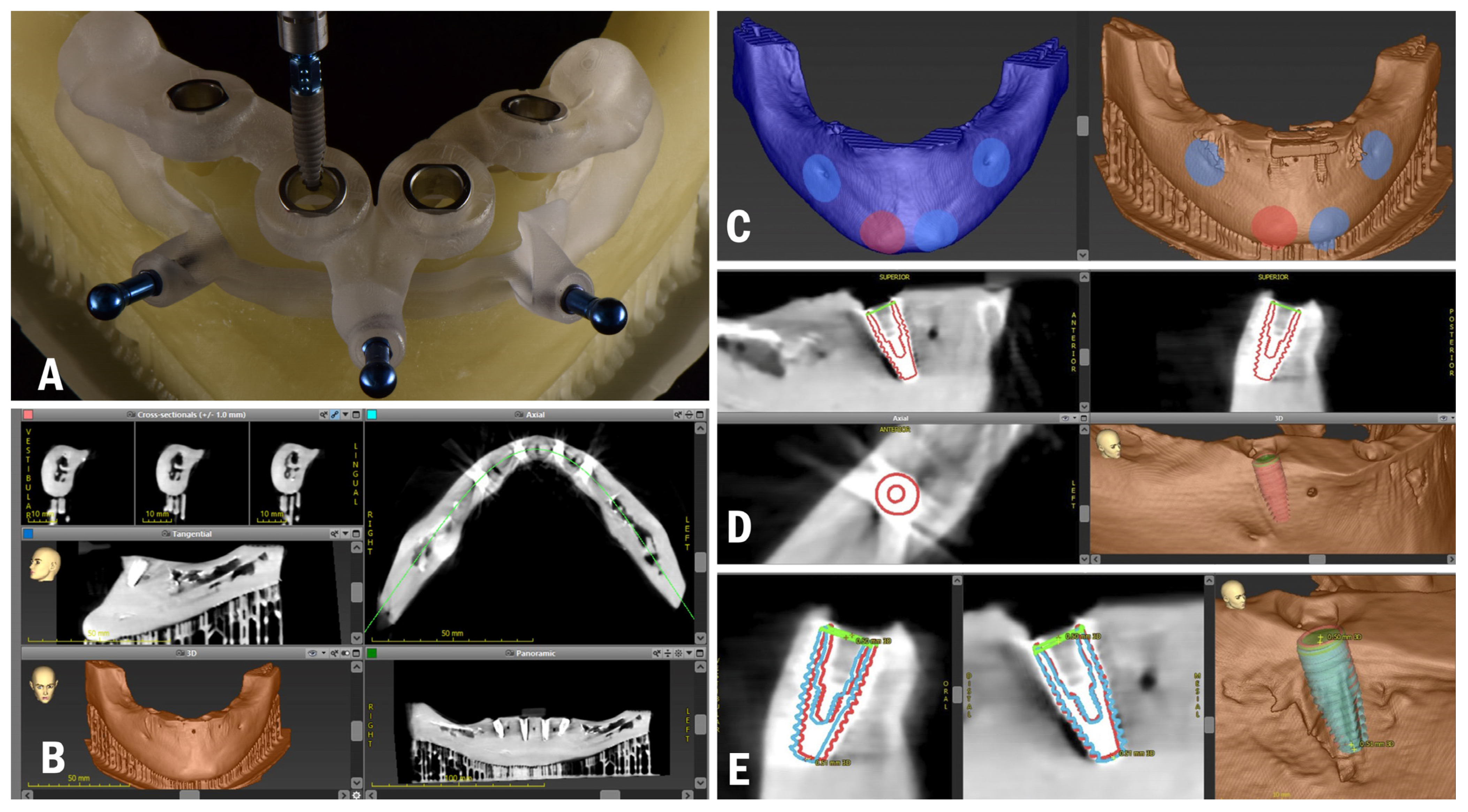
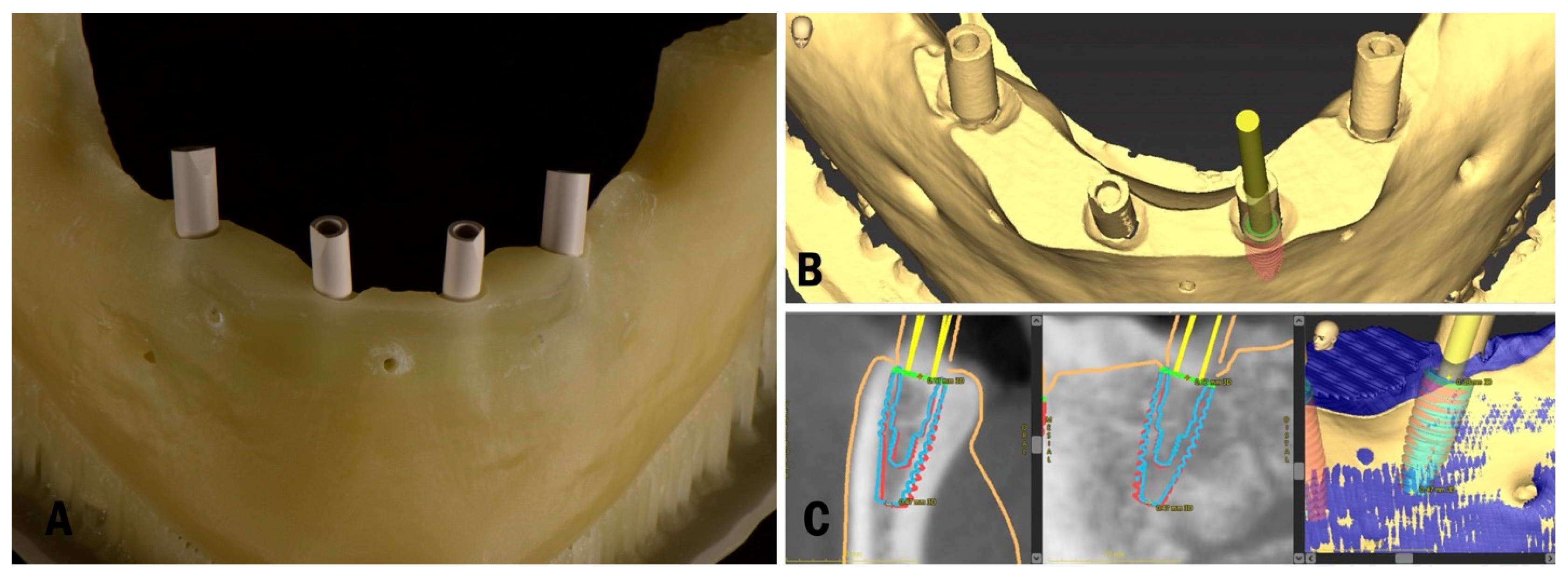
2. Materials and Methods
2.1. Planning and Surgery
2.2. Time and Cost Analysis
- Duration of planning (min) 30 min
- Duration of surgery (min) 45 min
- Preoperative fee: cost for the CBCT (€120).
- Surgical fee: cost for implants, their surgical installation, and the clinician’s fee (€1000 per implant).
- Prosthetic fee: cost for all prosthetic components, their installation, the dental laboratory fee, and the clinician’s fee (€1500 for immediate loading and €4500 for definitive prosthesis).
- Guide fee: cost of the specific surgical template (€400) and extra components (€20 per sleeve).
3. Results
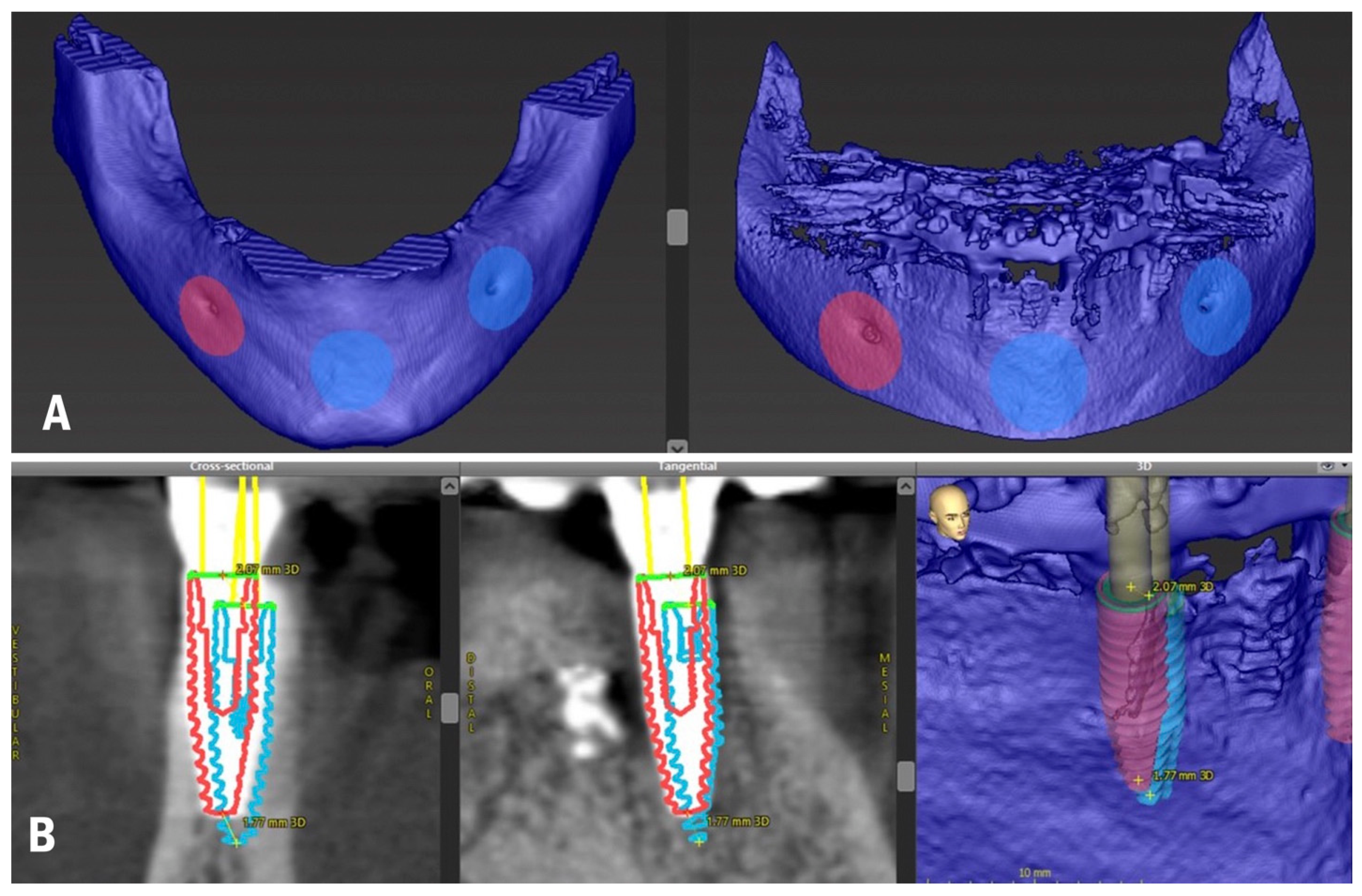
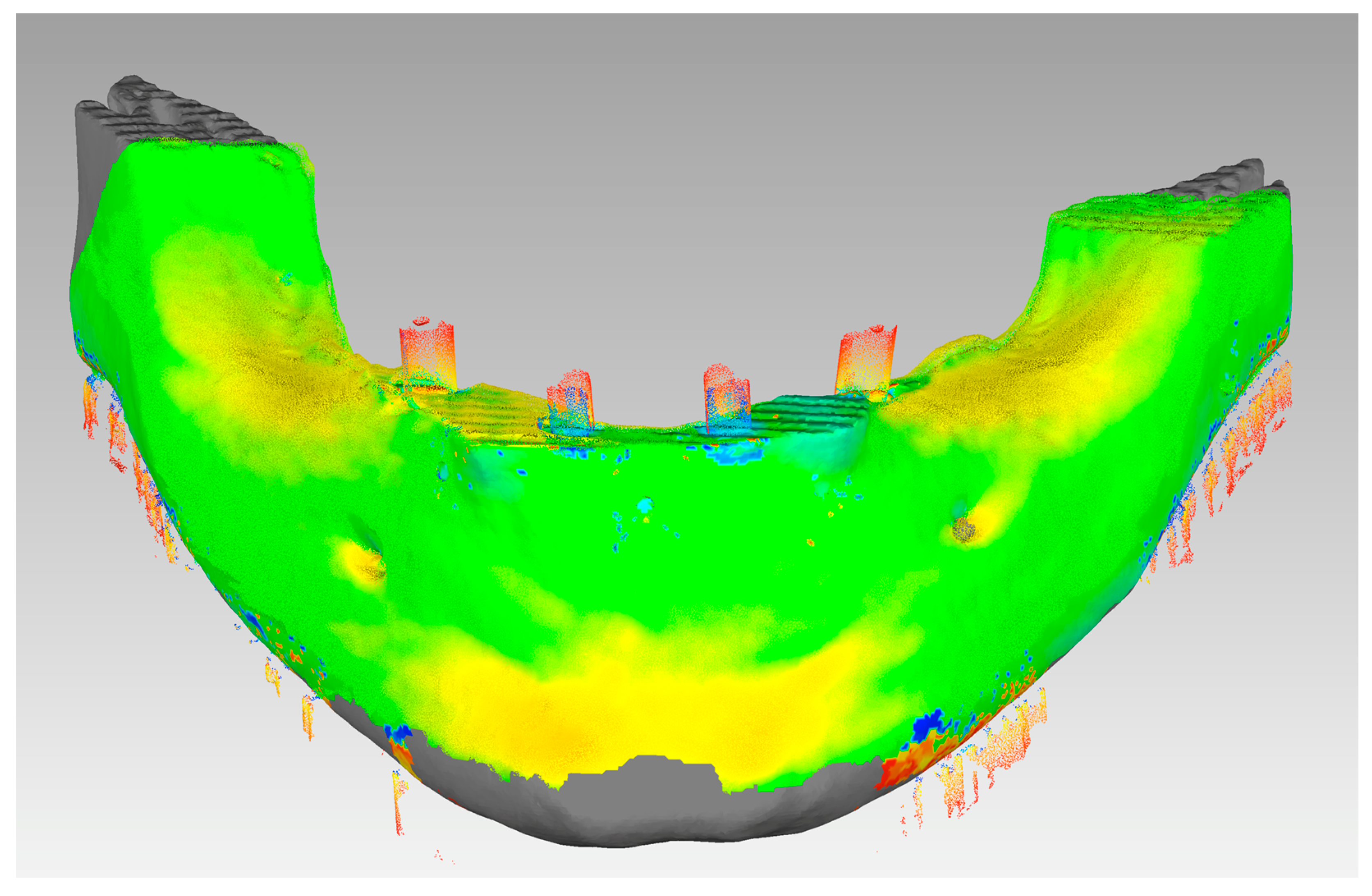
3.1. In Vivo Treatment Evaluation
3.2. In Vitro Treatment Evaluation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Mangano, C.; Luongo, F.; Migliario, M.; Mortellaro, C.; Mangano, F.G. Combining Intraoral Scans, Cone Beam Computed Tomography and Face Scans: The Virtual Patient. J. Craniofacial Surg. 2018, 29, 2241–2246. [Google Scholar] [CrossRef] [PubMed]
- Papi, P.; Di Murro, B.; Penna, D.; Pompa, G. Digital prosthetic workflow during COVID-19 pandemic to limit infection risk in dental practice. Oral Dis. 2021, 27 (Suppl. S3), 723–726. [Google Scholar] [CrossRef] [PubMed]
- Jokstad, A.; Pjetursson, B.E.; Muhlemann, S.; Wismeijer, D.; Wolfart, S.; Fehmer, V.; Guth, J.F.; Holtzman, L.P.; Hammerle, C.H.F.; Makarov, N.; et al. Fabrication, workflow and delivery of reconstruction: Summary and consensus statements of group 4. The 6th EAO Consensus Conference 2021. Clin. Oral Implant. Res. 2021, 32 (Suppl. S21), 336–341. [Google Scholar] [CrossRef] [PubMed]
- Henprasert, P.; Dawson, D.V.; El-Kerdani, T.; Song, X.; Couso-Queiruga, E.; Holloway, J.A. Comparison of the Accuracy of Implant Position Using Surgical Guides Fabricated by Additive and Subtractive Techniques. J. Prosthodont. 2020, 29, 534–541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tahmaseb, A.; Wu, V.; Wismeijer, D.; Coucke, W.; Evans, C. The accuracy of static computer-aided implant surgery: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 416–435. [Google Scholar] [CrossRef] [Green Version]
- Makarov, N.; Pompa, G.; Papi, P. Computer-assisted implant placement and full-arch immediate loading with digitally prefabricated provisional prostheses without cast: A prospective pilot cohort study. Int. J. Implant. Dent. 2021, 7, 80. [Google Scholar] [CrossRef]
- Di Murro, B.; Papi, P.; Passarelli, P.C.; D’Addona, A.; Pompa, G. Attitude in Radiographic Post-Operative Assessment of Dental Implants among Italian Dentists: A Cross-Sectional Survey. Antibiotics 2020, 9, 234. [Google Scholar] [CrossRef]
- Papi, P.; Di Murro, B.; Pranno, N.; Bisogni, V.; Saracino, V.; Letizia, C.; Polimeni, A.; Pompa, G. Prevalence of peri-implant diseases among an Italian population of patients with metabolic syndrome: A cross-sectional study. J. Periodontol. 2019, 90, 1374–1382. [Google Scholar] [CrossRef]
- Di Murro, B.; Pranno, N.; Raco, A.; Pistilli, R.; Pompa, G.; Papi, P. Knowledge and Attitude towards Retrograde Peri-Implantitis among Italian Implantologists: A Cross-Sectional Survey. Int. J. Environ. Res. Public Health 2020, 17, 8356. [Google Scholar] [CrossRef]
- Bornstein, M.M.; Al-Nawas, B.; Kuchler, U.; Tahmaseb, A. Consensus statements and recommended clinical procedures regarding contemporary surgical and radiographic techniques in implant dentistry. Int. J. Oral Maxillofac. Implant. 2014, 29, 78–82. [Google Scholar] [CrossRef]
- Tahmaseb, A.; Wismeijer, D.; Coucke, W.; Derksen, W. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implant. 2014, 29, 25–42. [Google Scholar] [CrossRef] [Green Version]
- Carosi, P.; Lorenzi, C.; Lio, F.; Cardelli, P.; Pinto, A.; Laureti, A.; Pozzi, A. Accuracy of Computer-Assisted Flapless Implant Placement by Means of Mucosa-Supported Templates in Complete-Arch Restorations: A Systematic Review. Materials 2022, 15, 1462. [Google Scholar] [CrossRef]
- Romandini, M.; Ruales-Carrera, E.; Sadilina, S.; Hammerle, C.H.F.; Sanz, M. Minimal invasiveness at dental implant placement: A systematic review with meta-analyses on flapless fully guided surgery. Periodontol. 2000 2022. [Google Scholar] [CrossRef]
- Mijiritsky, E.; Ben Zaken, H.; Shacham, M.; Cinar, I.C.; Tore, C.; Nagy, K.; Ganz, S.D. Variety of Surgical Guides and Protocols for Bone Reduction Prior to Implant Placement: A Narrative Review. Int. J. Environ. Res. Public Health 2021, 18, 2341. [Google Scholar] [CrossRef]
- Tonellini, G.; Saez Vigo, R.; Novelli, G. Double Guided Surgery in All-on-4((R)) Concept: When Ostectomy Is Needed. Int. J. Dent. 2018, 2018, 2672549. [Google Scholar] [CrossRef] [Green Version]
- Carosi, P.; Ferrigno, N.; Arcuri, C.; Laureti, M. Computer-Aided Surgery and Immediate Loading to Rehabilitate Complete Arch with Four Dental Implants and Fixed Screw-Retained Prosthesis Up to 4 Years in Function: A Retrospective Study. Int. J. Oral Maxillofac. Implant. 2021, 36, 1180–1187. [Google Scholar] [CrossRef]
- Faeghi Nejad, M.; Proussaefs, P.; Lozada, J. Combining guided alveolar ridge reduction and guided implant placement for all-on-4 surgery: A clinical report. J. Prosthet. Dent. 2016, 115, 662–667. [Google Scholar] [CrossRef]
- Gaeta-Araujo, H.; Alzoubi, T.; Vasconcelos, K.F.; Orhan, K.; Pauwels, R.; Casselman, J.W.; Jacobs, R. Cone beam computed tomography in dentomaxillofacial radiology: A two-decade overview. Dento Maxillo Facial Radiol. 2020, 49, 20200145. [Google Scholar] [CrossRef]
- Wanderley, V.A.; de Faria Vasconcelos, K.; Leite, A.F.; Pauwels, R.; Shujaat, S.; Jacobs, R.; Oliveira, M.L. Impact of the blooming artefact on dental implant dimensions in 13 cone-beam computed tomography devices. Int. J. Implant. Dent. 2021, 7, 67. [Google Scholar] [CrossRef]
- Pettersson, A.; Komiyama, A.; Hultin, M.; Nasstrom, K.; Klinge, B. Accuracy of virtually planned and template guided implant surgery on edentate patients. Clin. Implant. Dent. Relat. Res. 2012, 14, 527–537. [Google Scholar] [CrossRef]
- Schnutenhaus, S.; Edelmann, C.; Rudolph, H.; Luthardt, R.G. Retrospective study to determine the accuracy of template-guided implant placement using a novel nonradiologic evaluation method. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2016, 121, e72–e79. [Google Scholar] [CrossRef] [PubMed]
- Nickenig, H.J.; Eitner, S. An alternative method to match planned and achieved positions of implants, after virtual planning using cone-beam CT data and surgical guide templates--a method reducing patient radiation exposure (part I). J. Cranio-Maxillofac. Surg. 2010, 38, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Monaco, C.; Arena, A.; Corsaletti, L.; Santomauro, V.; Venezia, P.; Cavalcanti, R.; Di Fiore, A.; Zucchelli, G. 2D/3D accuracies of implant position after guided surgery using different surgical protocols: A retrospective study. J. Prosthodont. Res. 2020, 64, 424–430. [Google Scholar] [CrossRef] [PubMed]
- Vandenberghe, B. The digital patient—Imaging science in dentistry. J. Dent. 2018, 74 (Suppl. S1), S21–S26. [Google Scholar] [CrossRef] [PubMed]
- Komuro, A.; Yamada, Y.; Uesugi, S.; Terashima, H.; Kimura, M.; Kishimoto, H.; Iida, T.; Sakamoto, K.; Okuda, K.; Kusano, K.; et al. Accuracy and dimensional reproducibility by model scanning, intraoral scanning, and CBCT imaging for digital implant dentistry. Int. J. Implant. Dent. 2021, 7, 63. [Google Scholar] [CrossRef]
- Son, K.; Huang, M.Y.; Lee, K.B. A method to evaluate the accuracy of dental implant placement without postoperative radiography after computer-guided implant surgery: A dental technique. J. Prosthet. Dent. 2020, 123, 661–666. [Google Scholar] [CrossRef]
- Storelli, S.; Palandrani, G.; Amorfini, L.; Scanferla, M.; Ausenda, F.; Romeo, E. A digital workflow for computer-guided implant surgery integrating CBCT, model scanning, and CAD/CAM for a complete edentulism implant-supported prosthesis: A technique procedure. Int. J. Comput. Dent. 2020, 23, 269–279. [Google Scholar]
- Shujaat, S.; Bornstein, M.M.; Price, J.B.; Jacobs, R. Integration of imaging modalities in digital dental workflows—Possibilities, limitations, and potential future developments. Dento Maxillo Facial Radiol. 2021, 50, 20210268. [Google Scholar] [CrossRef]
- Yang, J.W.; Liu, Q.; Yue, Z.G.; Hou, J.X.; Afrashtehfar, K.I. Digital Workflow for Full-Arch Immediate Implant Placement Using a Stackable Surgical Guide Fabricated Using SLM Technology. J. Prosthodont. 2021, 30, 645–650. [Google Scholar] [CrossRef]
- Costa, A.J.M.; Teixeira Neto, A.D.; Burgoa, S.; Gutierrez, V.; Cortes, A.R.G. Fully Digital Workflow with Magnetically Connected Guides for Full-Arch Implant Rehabilitation Following Guided Alveolar Ridge Reduction. J. Prosthodont. 2020, 29, 272–276. [Google Scholar] [CrossRef]
- Flugge, T.; Derksen, W.; Te Poel, J.; Hassan, B.; Nelson, K.; Wismeijer, D. Registration of cone beam computed tomography data and intraoral surface scans—A prerequisite for guided implant surgery with CAD/CAM drilling guides. Clin. Oral Implant. Res. 2017, 28, 1113–1118. [Google Scholar] [CrossRef]
- Cassetta, M.; Di Mambro, A.; Giansanti, M.; Stefanelli, L.V.; Cavallini, C. The intrinsic error of a stereolithographic surgical template in implant guided surgery. Int. J. Oral Maxillofac. Surg. 2013, 42, 264–275. [Google Scholar] [CrossRef]
- Zhou, W.; Liu, Z.; Song, L.; Kuo, C.L.; Shafer, D.M. Clinical Factors Affecting the Accuracy of Guided Implant Surgery—A Systematic Review and Meta-analysis. J. Evid.-Based Dent. Pract. 2018, 18, 28–40. [Google Scholar] [CrossRef]
- Barteaux, L.; Daelemans, P.; Malevez, C. A surgical stent for the Branemark Novum bone reduction procedure. Clin. Implant. Dent. Relat. Res. 2004, 6, 210–221. [Google Scholar] [CrossRef]
- Schnutenhaus, S.; Groller, S.; Luthardt, R.G.; Rudolph, H. Accuracy of the match between cone beam computed tomography and model scan data in template-guided implant planning: A prospective controlled clinical study. Clin. Implant. Dent. Relat. Res. 2018, 20, 541–549. [Google Scholar] [CrossRef]
- Shujaat, S.; Shaheen, E.; Novillo, F.; Politis, C.; Jacobs, R. Accuracy of cone beam computed tomography-derived casts: A comparative study. J. Prosthet. Dent. 2021, 125, 95–102. [Google Scholar] [CrossRef]
- Meglioli, M.; Naveau, A.; Macaluso, G.M.; Catros, S. 3D printed bone models in oral and cranio-maxillofacial surgery: A systematic review. 3D Print. Med. 2020, 6, 30. [Google Scholar] [CrossRef]
- Nomura, Y.; Watanabe, H.; Manila, N.G.; Asai, S.; Kurabayashi, T. Evaluation of streak metal artifacts in cone beam computed tomography by using the Gumbel distribution: A phantom study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2021, 131, 494–502. [Google Scholar] [CrossRef]
- Tallarico, M.; Xhanari, E.; Kim, Y.J.; Cocchi, F.; Martinolli, M.; Alushi, A.; Baldoni, E.E.; Meloni, S.M. Accuracy of computer-assisted template-based implant placement using conventional impression and scan model or intraoral digital impression: A randomised controlled trial with 1 year of follow-up. Int. J. Oral Implantol. (Berl.) 2019, 12, 197–206. [Google Scholar]
- Wismeijer, D.; Joda, T.; Flugge, T.; Fokas, G.; Tahmaseb, A.; Bechelli, D.; Bohner, L.; Bornstein, M.; Burgoyne, A.; Caram, S.; et al. Group 5 ITI Consensus Report: Digital technologies. Clin. Oral Implant. Res. 2018, 29 (Suppl. S16), 436–442. [Google Scholar] [CrossRef] [Green Version]
- Suese, K. Progress in digital dentistry: The practical use of intraoral scanners. Dent. Mater. J. 2020, 39, 52–56. [Google Scholar] [CrossRef] [Green Version]
- Nulty, A.B. A Comparison of Full Arch Trueness and Precision of Nine Intra-Oral Digital Scanners and Four Lab Digital Scanners. Dent. J. 2021, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Skjerven, H.; Olsen-Bergem, H.; Ronold, H.J.; Riis, U.H.; Ellingsen, J.E. Comparison of postoperative intraoral scan versus cone beam computerised tomography to measure accuracy of guided implant placement—A prospective clinical study. Clin. Oral Implant. Res. 2019, 30, 531–541. [Google Scholar] [CrossRef] [PubMed]
- Arisan, V.; Karabuda, Z.C.; Ozdemir, T. Accuracy of two stereolithographic guide systems for computer-aided implant placement: A computed tomography-based clinical comparative study. J. Periodontol. 2010, 81, 43–51. [Google Scholar] [CrossRef] [PubMed]
- Jung, R.E.; Schneider, D.; Ganeles, J.; Wismeijer, D.; Zwahlen, M.; Hammerle, C.H.; Tahmaseb, A. Computer technology applications in surgical implant dentistry: A systematic review. Int. J. Oral Maxillofac. Implant. 2009, 24, 92–109. [Google Scholar]
- Wei, S.M.; Zhu, Y.; Wei, J.X.; Zhang, C.N.; Shi, J.Y.; Lai, H.C. Accuracy of dynamic navigation in implant surgery: A systematic review and meta-analysis. Clin. Oral Implant. Res. 2021, 32, 383–393. [Google Scholar] [CrossRef]
- Pozzi, A.; Hansson, L.; Carosi, P.; Arcuri, L. Dynamic navigation guided surgery and prosthetics for immediate loading of complete-arch restoration. J. Esthet. Restor. Dent. 2021, 33, 224–236. [Google Scholar] [CrossRef]
| Tooth Position | Angle | 3D Offset (Base) | Distal (Base) | Vestibular (Base) | Apical (Base) | 3D Offset (Tip) | Distal (Tip) | Vestibular (Tip) | Apical (Tip) |
|---|---|---|---|---|---|---|---|---|---|
| 35 | 2.4 | 2.55 | −2.14 | 0.93 | −1.03 | 2.21 | −1.73 | 0.93 | −1.02 |
| 32 | 5.3 | 2.61 | −1.86 | 0.61 | −1.72 | 3.47 | −2.98 | 0.62 | −1.67 |
| 42 | 2.3 | 2.07 | 0.79 | 1.11 | −1.55 | 1.77 | 0.5 | 0.72 | −1.54 |
| 45 | 2.8 | 1.32 | 0.49 | 1.23 | −0.02 | 1.01 | 0.65 | 0.78 | −0.01 |
| Tooth Position | Angle | 3D Offset (Base) | Distal (Base) | Vestibular (Base) | Apical (Base) | 3D Offset (Tip) | Distal (Tip) | Vestibular (Tip) | Apical (Tip) |
|---|---|---|---|---|---|---|---|---|---|
| 35 | 0 | 0.22 | 0.22 | 0 | 0.06 | 0.22 | 0.22 | 0 | 0.06 |
| 32 | 1.6 | 0.79 | 0.78 | 0.13 | 0.09 | 0.81 | 0.78 | −0.19 | 0.1 |
| 42 | 4 | 0.74 | −0.39 | −0.63 | 0.03 | 1.37 | 0 | −1.37 | 0.06 |
| 45 | 1.6 | 0.5 | −0.11 | −0.38 | −0.3 | 0.51 | 0.17 | −0.38 | −0.3 |
| Tooth Position | Angle | 3D Offset (Base) | Distal (Base) | Vestibular (Base) | Apical (Base) | 3D Offset (Tip) | Distal (Tip) | Vestibular (Tip) | Apical (Tip) |
|---|---|---|---|---|---|---|---|---|---|
| 35 | 3.1 | 0.13 | −0.07 | 0.08 | 0.06 | 0.47 | −0.02 | −0.46 | 0.08 |
| 32 | 3.2 | 0.71 | 0.17 | 0.38 | 0.57 | 0.83 | 0.55 | −0.18 | 0.59 |
| 42 | 5.1 | 0.62 | −0.35 | 0.06 | 0.51 | 1.1 | 0 | −0.95 | 0.55 |
| 45 | 4.1 | 0.4 | −0.18 | 0.08 | 0.35 | 0.64 | 0.43 | −0.28 | 0.38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Makarov, N.; Papi, P.; Santomauro, V.; Di Carlo, G.; Polimeni, A.; Di Murro, B.; Saccucci, M. In Vivo and In Vitro Accuracy Analysis of Static Computer-Assisted Implant Surgery in an Edentulous Patient. Appl. Sci. 2023, 13, 1185. https://doi.org/10.3390/app13021185
Makarov N, Papi P, Santomauro V, Di Carlo G, Polimeni A, Di Murro B, Saccucci M. In Vivo and In Vitro Accuracy Analysis of Static Computer-Assisted Implant Surgery in an Edentulous Patient. Applied Sciences. 2023; 13(2):1185. https://doi.org/10.3390/app13021185
Chicago/Turabian StyleMakarov, Nikolay, Piero Papi, Vincenzo Santomauro, Gabriele Di Carlo, Antonella Polimeni, Bianca Di Murro, and Matteo Saccucci. 2023. "In Vivo and In Vitro Accuracy Analysis of Static Computer-Assisted Implant Surgery in an Edentulous Patient" Applied Sciences 13, no. 2: 1185. https://doi.org/10.3390/app13021185









