Multiscale Evaluation of Jaw Geometry Reproduction Obtained Via the Use of Selected Orthodontic Materials in Dental Implants and Orthodontics—In Vitro Case Study
Abstract
:1. Introduction
2. Materials and Methods
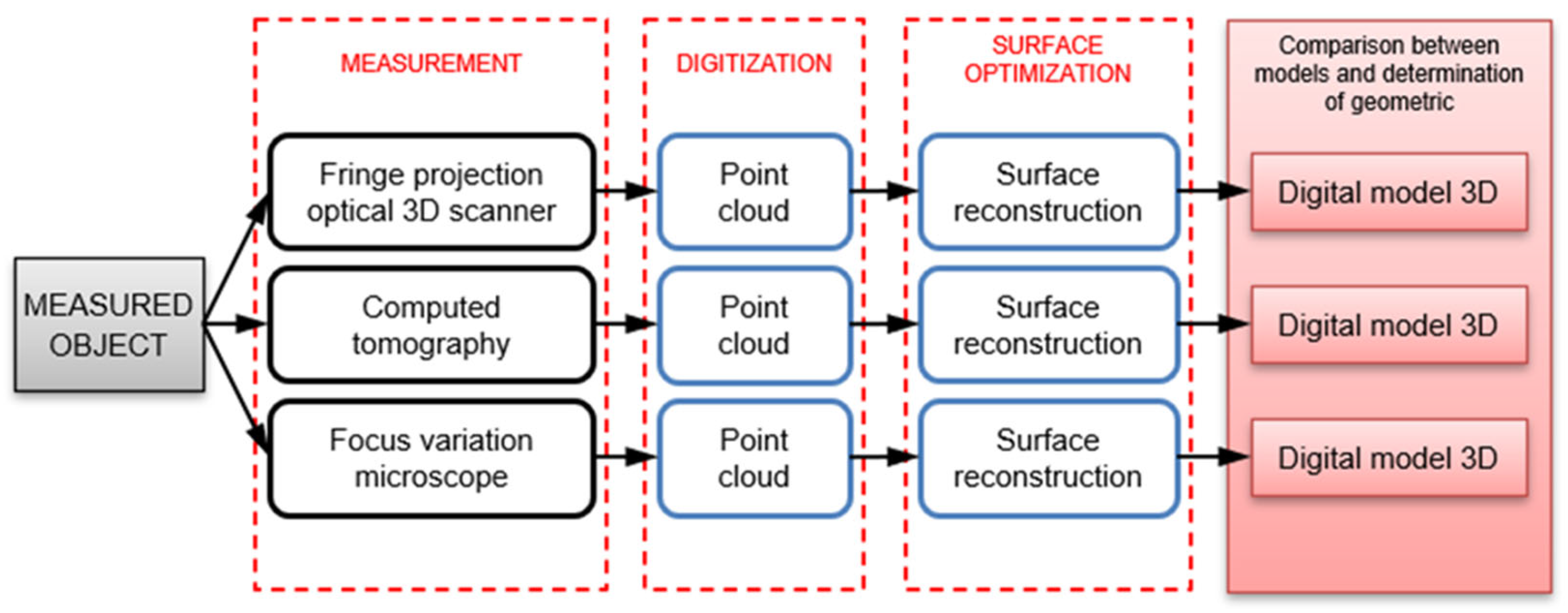
- Measurements of the jaw model geometry (photogrammetric method, micro-CT);
- Preparation of impressions with selected types of orthodontic impression compounds;
- Measurements of the impression geometry obtained using the photogrammetric method;
- Application of reverse engineering to obtain digital models of the examined jaws;
- Application of rapid prototyping technology (3D printing) to obtain models;
- Casting of plaster models of the jaws using dental plaster;
- Measurements of impression geometry obtained using nonmedical computed tomography;
- Measurements of the obtained plaster models and models obtained via 3D printing;
- Surface structure measurements of selected dental impressions and gypsum models.
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Vogel, A.B.; Kilic, F.; Schmidt, F.; Rübel, S.; Lapatki, B.G. Optical 3D scans for orthodontic diagnostics performed on full-arch impressions. Completeness of surface structure representation. J. Orofac. Orthop. 2015, 76, 493–507. [Google Scholar] [CrossRef] [PubMed]
- Ma, T.; Li, J.; Li, Z.; Li, Y. Improvement and Application of Mass Spring Model in Simulation of Gingi-val Soft Tissue Deformation. J. Comput.-Aided Des. Comput. Graph. 2020, 32, 325–333. [Google Scholar]
- Palczewska-Komsa, M.O.; Gapiński, B.; Nowicka, A. The Influence of New Bioactive Materials on Pulp-Dentin Complex Regeneration in the Assessment of Cone Bone Computed Tomography (CBCT) and Computed Micro-Tomography (Micro-CT) from a Present and Future Perspective—A Systematic Review. J. Clin. Med. 2022, 11, 3091. [Google Scholar] [CrossRef] [PubMed]
- Dobrzanski, L.A.; Dobrzanski, L.B. Dentistry 4.0 Concept in the Design and Manufacturing of Prosthetic Dental Restorations. Processes 2020, 8, 525. [Google Scholar] [CrossRef]
- Gonzalez, J. The Evolution of Dental Materials for Hybrid Prosthesis. Open Dent. J. 2014, 8, 85–94. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wriedt, S.; Foersch, M.; Muhle, J.D.; Schmidtmann, I.; Wehrbein, H. Multibracket appliance: Impression defaults and their reduction by blocking-out—A three-dimensional study. Clin. Oral Investig. 2016, 20, 365–372. [Google Scholar] [CrossRef]
- Erbe, C.; Ruf, S.; Wöstmann, B.; Balkenhol, M. Dimensional stability of contemporary irreversible hydrocolloids: Humidor versus wet tissue storage. J. Prosthet. Dent. 2012, 108, 114–122. [Google Scholar] [CrossRef]
- Faria, A.C.L.; Rodrigues, R.C.S.; Macedo, A.P.; Mattos, M.G.C.; Ribeiro, R.F. Accuracy of stone casts obtained by different impression materials. Braz. Oral Res. 2008, 22, 293–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marquezan, M.; Jurach, E.M.; Guimarães, V.D.; Valentim, R.G.A.; Nojima, L.I.; da Cunha Gonçalves Nojima, M. Does the contact time of alginate with plaster cast influence its properties? Braz. Oral Res. 2012, 26, 197–201. [Google Scholar] [CrossRef] [Green Version]
- Nandini, V.V.; Venkatesh, K.V.; Nair, K.C. Alginate impressions: A practical perspective. J. Conserv. Dent. 2008, 11, 37–41. [Google Scholar] [CrossRef]
- Reisbick, M.H.; Johnston, W.M.; Rashid, R.G. Irreversible hydrocolloid and gypsum interactions. Int. J. Prosthodont. 1997, 10, 7–13. [Google Scholar]
- Liczmanski, K.; Stamm, T.; Sauerland, C.; Blanck-Lubarsch, M. Accuracy of intraoral scans in the mixed dentition: A prospective non-randomized comparative clinical trial. Head Face Med. 2020, 16, 11. [Google Scholar] [CrossRef] [PubMed]
- Chalmers, E.V.; McIntyre, G.T.; Wang, W.; Gillgrass, T.; Martin, C.B.; Mossey, P.A. Intraoral 3D scanning or dental impressions for the assessment of dental arch relationships in cleft care: Which is superior? Cleft Palate–Craniofacial J. 2016, 53, 568–577. [Google Scholar] [CrossRef] [Green Version]
- AL-Meraikhi, H.; Yilmaz, B.; McGlumphy, E.; Brantley, W.A.; Johnston, W.M. Distortion of CAD-CAM-fabricated implant-fixed titanium and zirconia complete dental prosthesis frameworks. J. Prosthet. Dent. 2018, 119, 116–123. [Google Scholar] [CrossRef]
- Peng, L.; Chen, L.; Harris, B.T.; Bhandari, B.; Morton, D.; Lin, W.-S. Accuracy and reproducibility of virtual edentulous casts created by laboratory impression scan protocols. J. Prosthet. Dent. 2018, 120, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Nagata, K.; Fuchigami, K.; Okuhama, Y.; Wakamori, K.; Tsuruoka, H.; Nakashizu, T.; Hoshi, N.; Atsumi, M.; Kimoto, K.; Kawana, H. Comparison of digital and silicone impressions for single-tooth implants and two and three-unit implants for a free-end edentulous saddle. BMC Oral Health 2021, 21, 464. [Google Scholar] [CrossRef] [PubMed]
- Glisica, O.; Hoejbjerrea, L.; Sonnesenb, L. A comparison of patient experience, chair-side time, accuracy of dental arch measurements and costs of acquisition of dental models. Angle Orthod. 2019, 89, 868–875. [Google Scholar] [CrossRef] [Green Version]
- Dastoori, M.; Bouserhal, J.P.; Halazonetis, D.J.; Athanasiou, A.E. Anterior teeth root inclination prediction derived from digital models: A comparative study of plaster study casts and CBCT images. J. Clin. Exp. Dent. 2018, 10, 1069–1074. [Google Scholar] [CrossRef] [PubMed]
- Martin, C.B.; Chalmers, E.V.; McIntyre, G.T.; Cochrane, H.; Mossey, P.A. Orthodontic scanners: What is available? J. Orthod. 2015, 42, 136–143. [Google Scholar] [CrossRef]
- Bosio, J.A.; Rozhitsky, F.; Jiang, S.S.; Conte, M.; Mukherjee, P.; Cangialosi, T.J. Comparison of scanning times for different dental cast materials using an intraoral scanner. J. World Fed. Orthod. 2017, 6, 11–14. [Google Scholar] [CrossRef]
- Shah, N.; Bansal, N.; Logani, A. Recent advances in imaging technologies in dentistry. World J. Radiol. 2014, 6, 794–807. [Google Scholar] [CrossRef] [PubMed]
- Elnaghy, R.; Amin, S.; Hasanin, M. Concepts and Clinical Applications of Intraoral 3D Scanning in the Management of Patients with Orofacial Clefts. In Recent Advances in the Treatment of Orofacial Clefts; Palone, M., Ed.; IntechOpen: London, UK, 2021. [Google Scholar]
- Pereira, M.M.A.; Dini, C.; Souza, J.G.S.; Barão, V.A.R.; de Avila, E.D. Industry support for dental implant research: A metatrend study of industry partnership in the development of new technologies. J. Prosthet. Dent. 2022; in press. [Google Scholar] [CrossRef]
- Burzynski, J.A.; Firestone, A.R.; Beck, F.M.; Fields, H.W., Jr.; Deguchi, T. Comparison of digital intraoral scanners and alginate impressions: Time and patient satisfaction. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Aly, P.; Mohsen, C. Comparison of the Accuracy of Three-Dimensional Printed Casts, Digital, and Conventional Casts: An In Vitro Study. Eur. J. Dent. 2020, 14, 189–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ahn, J.S.; Park, A.; Kim, J.W.; Lee, B.H.; Eom, J.B. Development of Three-Dimensional Dental Scanning Apparatus Using Structured Illumination. Sensors 2017, 17, 1634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Javaid, M.; Haleem, A.; Kumar, L. Current status and applications of 3D scanning in dentistry. Clin. Epidemiol. Glob. Health 2019, 7, 228–233. [Google Scholar] [CrossRef] [Green Version]
- Faot, F.; Chatterjee, M.; de Camargos, G.V.; Duyck, J.; Vandamme, K. Micro-CT analysis of the rodent jaw bone micro-architecture: A systematic review. Bone Rep. 2015, 2, 14–24. [Google Scholar] [CrossRef] [Green Version]
- Shibli, J.A.; Grassi, S.; de Figueiredo, L.C.; Feres, M.; Marcantonio, E., Jr.; Iezzi, G.; Piattelli, A. Influence of implant surface topography on early osseointegration: A histological study in human jaws. J. Biomed. Mater. Res. 2007, 80, 377–385. [Google Scholar] [CrossRef]
- Uklejewski, R.; Winiecki, M.; Patalas, A.; Rogala, P. Bone Density Micro-CT Assessment during Embedding of the Innovative Multi-Spiked Connecting Scaffold in Periarticular Bone to Elaborate a Validated Numerical Model for Designing Biomimetic Fixation of Resurfacing Endoprostheses. Materials 2021, 14, 1384. [Google Scholar] [CrossRef]
- Emara, A.; Sharma, S.; Halbeisen, F.S.; Msallem, B.; Thieringer, F.M. Comparative evaluation of digitization of diagnostic dental cast (plaster) models using different scanning technologies. Dent. J. 2020, 8, 79. [Google Scholar] [CrossRef]
- Latham, J.; Ludlow, M.; Mennito, A.; Kelly, A.; Evans, Z.; Renne, W. Effect of scan pattern on complete-arch scans with 4 digital scanners. J. Prosthet. Dent. 2020, 123, 85–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimmermann, M.; Koller, C.; Rumetsch, M.; Ender, A.; Mehl, A. Precision of guided scanning procedures for full-arch digital impressions in vivo. J. Orofac. Orthop. 2017, 78, 466–471. [Google Scholar] [CrossRef] [PubMed]
- Schenz, N.; Schwarz, V.; Hörmann, R.; Crismani, A.G. Impression material accuracy for palatal orthodontic miniscrews. J. Orofac. Orthop. 2020, 81, 427–439. [Google Scholar] [CrossRef]
- Morris, R.S.; Hoye, L.N.; Elnagar, M.H.; Atsawasuwan, P.; Galang-Boquiren, M.T.; Caplin, J.; Viana, G.C.; Obrez, A.; Kusnoto, B. Accuracy of Dental Monitoring 3D digital dental models using photograph and video mode. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 420–428. [Google Scholar] [CrossRef]
- Lasi, H.; Fettke, P.; Kemper, H.G.; Feld, T.; Hoffmann, M. Industry 4.0. Bus. Inf. Syst. Eng. 2014, 6, 239–242. [Google Scholar] [CrossRef]
- Dietrich, C.A.; Ender, A.; Baumgartner, S.; Mehl, A. A validation study of reconstructed rapid prototyping models produced by two technologies. Angle Orthod. 2017, 87, 782–787. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sfondrini, M.F.; Gandini, P.; Malfatto, M.; Di Corato, F.; Trovati, F.; Scribante, A. Computerized Casts for Orthodontic Purpose Using Powder-Free Intraoral Scanners: Accuracy, Execution Time, and Patient Feedback. BioMed Res. Int. 2018, 2018, 4103232. [Google Scholar] [CrossRef] [Green Version]
- Kroma, A.; Mendak, M.; Jakubowicz, M.; Gapiński, B.; Popielarski, P. Non-Contact Multiscale Analysis of a DPP 3D-Printed Injection Die for Investment Casting. Materials 2021, 14, 6758. [Google Scholar] [CrossRef]
- Hassan, W.N.W.; Yusoff, Y.; Mardic, N.A. Comparison of reconstructed rapid prototyping models produced by 3-dimensional printing and conventional stone models with different degrees of crowding. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 209–218. [Google Scholar] [CrossRef] [Green Version]
- Joffe, L. Current Products and Practices OrthoCADTM: Digital models for a digital era. J. Orthod. 2004, 31, 344–347. [Google Scholar] [CrossRef] [PubMed]
- Guzm, J.F.G.; Teramoto Ohara, A. Evaluation of three-dimensional printed virtual setups. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 288–295. [Google Scholar]
- Möhlhenrich, S.C.; Brandt, M.; Kniha, K.; Bock, A.; Prescher, A.; Hölzle, F.; Modabber, A.; Danesh, G. Suitability of virtual plaster models superimposed with the lateral cephalogram for guided paramedian orthodontic mini-implant placement with regard to the bone support. J. Orofac. Orthop. 2020, 81, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Zilberman, O.; Huggare, J.A.V.; Konstantinos, A.P.A. Evaluation of the validity of tooth size and arch width measurements using conventional and three-dimensional virtual orthodontic models. Angle Orthod. 2003, 73, 301–306. [Google Scholar] [PubMed]
- Yuan, T.; Wang, Y.; Hou, Z.; Wang, J. Tooth segmentation and gingival tissue deformation framework for 3D orthodontic treatment planning and evaluating. Med. Biol. Eng. Comput. 2020, 58, 2271–2290. [Google Scholar] [CrossRef] [PubMed]
- Swojak, N.; Wieczorowski, M.; Jakubowicz, M. Assessment of selected metrological properties of laser triangulation sensors. Measurement 2021, 176, 109190. [Google Scholar] [CrossRef]
- Kihara, T.; Yoshimi, Y.; Taji, T.; Murayama, T.; Tanimoto, K.; Nikawa, H. Accuracy of a three-dimensional dentition model digitized from an interocclusal record using a non-contact surface scanner. Eur. J. Orthod. 2016, 38, 435–439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pacheco-Pereira, C.; De Luca Canto, G.; Major, P.W.; Flores-Mird, C. Variation of orthodontic treatment decision-making based on dental model type: A systematic review. Angle Orthod. 2015, 85, 501–509. [Google Scholar] [CrossRef]
- Mullen, S.R.; Martin, C.A.; Ngan, P.; Gladwin, M. Accuracy of space analysis with emodels and plaster models. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 346–352. [Google Scholar] [CrossRef]
- Baan, F.; Bruggink, R.; Nijsink, J.; Maal, T.J.J.; Ongkosuwito, E.M. Fusion of intra-oral scans in cone-beam computed tomography scans. Clin. Oral Investig. 2021, 25, 77–85. [Google Scholar] [CrossRef]
- Gapiński, B.; Janicki, P.; Marciniak-Podsadna, L.; Jakubowicz, M. Application of the computed tomography to control parts made on additive manufacturing process. Procedia Eng. 2016, 149, 105–121. [Google Scholar] [CrossRef] [Green Version]
- Prakoso, A.T.; Basri, H.; Adanta, D.; Yani, I.; Ammarullah, M.I.; Akbar, I.; Ghazali, F.A.; Syahrom, A.; Kamarul, T. The Effect of Tortuosity on Permeability of Porous Scaffold. Biomedicines 2023, 11, 427. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Lee, G.-H.; Moon, D.-N.; Kim, J.-C.; Park, M.; Lee, K.-M. A digital approach to the evaluation of mandibular position by using a virtual articulator. J. Prosthet. Dent. 2021, 125, 849–853. [Google Scholar] [CrossRef] [PubMed]
- Dąbrowski, M.; Rogala, P.; Uklejewski, R.; Patalas, A.; Winiecki, M.; Gapiński, B. Subchondral Bone Relative Area and Density in Human Osteoarthritic Femoral Heads Assessed with Micro-CT before and after Mechanical Embedding of the Innovative Multi-Spiked Connecting Scaffold for Resurfacing THA Endoprostheses: A Pilot Study. J. Clin. Med. 2021, 10, 2937. [Google Scholar] [CrossRef] [PubMed]
- Gapinski, B.; Wieczorowski, M.; Mietliński, P.; Mathia, T.G. Verification of Computed Tomograph for Dimensional Measurements. In Lecture Notes in Mechanical Engineering; Springer: Cham, Switzerland, 2022; pp. 142–155. [Google Scholar] [CrossRef]
- Wieczorowski, M.; Yago, I.P.; Alejandro, P.D.; Gapiński, B.; Budzik, G.; Diering, M. Comparison of Measurements Realized on Computed Tomograph and Optical Scanners for Elements Manufactured by Wire Arc Additive Manufacturing. In Lecture Notes in Mechanical Engineering; Springer: Cham, Switzerland, 2022; pp. 127–141. [Google Scholar] [CrossRef]
- Surowska, B.; Ostapiuk, M.; Tarczydło, B. Micro-CT analysis of molar teeth restored by combining conventional and glass fibre reinforced composites. Eng. Biomater. 2016, 19, 13–19. [Google Scholar]
- Schmeidl, K.; Wieczorowski, M.; Grocholewicz, K.; Mendak, M.; Janiszewska Olszowska, J. Frictional properties of the tinbtazro orthodontic wire—A laboratory comparison to popular archwires. Materials 2021, 14, 6233. [Google Scholar] [CrossRef]














| Surface Structure Parameters | Impression | Plaster Model |
|---|---|---|
| Sq (Root Mean Square Height) | 2.97 µm | 2.86 µm |
| Ssk (Skewness) | −1.12 | 0.0587 |
| Sku (Kurtosis) | 60.8 | 32.0 |
| Sp (Maximum peak height) | 50.4 µm | 331 µm |
| Sv (Maximum pit height) | 184 µm | 26 µm |
| Sz (Maximum height) | 234 µm | 357 µm |
| Sa (Arithmetical mean height) | 2.12 µm | 2.13 µm |
| Surface Structure Parameters | Impression | Plaster Model |
|---|---|---|
| Sq (Root Mean Square Height) | 1.18 µm | 9.04 µm |
| Ssk (Skewness) | 0.0732 | −3.84 |
| Sku (Kurtosis) | 6.32 | 50.7 |
| Sp (Maximum peak height) | 40.6 µm | 117 µm |
| Sv (Maximum pit height) | 11.1 µm | 165 µm |
| Sz (Maximum height) | 51.7 µm | 282 µm |
| Sa (Arithmetical mean height) | 0.884 µm | 4.23 µm |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jakubowicz, M.; Gapiński, B.; Marciniak-Podsadna, L.; Mendak, M.; Mietliński, P.; Wieczorowski, M. Multiscale Evaluation of Jaw Geometry Reproduction Obtained Via the Use of Selected Orthodontic Materials in Dental Implants and Orthodontics—In Vitro Case Study. Appl. Sci. 2023, 13, 6932. https://doi.org/10.3390/app13126932
Jakubowicz M, Gapiński B, Marciniak-Podsadna L, Mendak M, Mietliński P, Wieczorowski M. Multiscale Evaluation of Jaw Geometry Reproduction Obtained Via the Use of Selected Orthodontic Materials in Dental Implants and Orthodontics—In Vitro Case Study. Applied Sciences. 2023; 13(12):6932. https://doi.org/10.3390/app13126932
Chicago/Turabian StyleJakubowicz, Michał, Bartosz Gapiński, Lidia Marciniak-Podsadna, Michał Mendak, Patryk Mietliński, and Michał Wieczorowski. 2023. "Multiscale Evaluation of Jaw Geometry Reproduction Obtained Via the Use of Selected Orthodontic Materials in Dental Implants and Orthodontics—In Vitro Case Study" Applied Sciences 13, no. 12: 6932. https://doi.org/10.3390/app13126932
APA StyleJakubowicz, M., Gapiński, B., Marciniak-Podsadna, L., Mendak, M., Mietliński, P., & Wieczorowski, M. (2023). Multiscale Evaluation of Jaw Geometry Reproduction Obtained Via the Use of Selected Orthodontic Materials in Dental Implants and Orthodontics—In Vitro Case Study. Applied Sciences, 13(12), 6932. https://doi.org/10.3390/app13126932







