Abstract
Background: Dental aesthetic procedures aim to rectify flaws in dental elements’ shape, alignment, or overly dark color. One of the most common dental aesthetic procedures is tooth whitening. This study attempts to introduce key aspects of bleaching and describe the different techniques and the mechanism of action of bleaching agents, focusing on the clinical implications in orthodontic and on composite restorations. Methods: The research was performed on PubMed, Web of Science, and Science Direct databases for articles on our topic published between 2017 and 2023, and we found a total of 1512 studies. In total, 57 papers were considered for the qualitative analysis in the review. Results: This study found that both carbamide peroxide and hydrogen peroxide were clinically effective, although patients’ level of tooth sensitivity seemed to be lessened by the latter. However, the latter appears to be more effective at reducing patient-experienced tooth sensitivity. Conclusion: Carbamide and hydrogen peroxide based whitening techniques were shown to be equally successful at treating tooth discoloration after bracket composite removal, with no discernible differences between them. To increase the effectiveness of whitening on composites, more research is needed. To achieve the desired results and avoid the negative effects of whitening gels on teeth and soft tissue, a patient-specific approach is advised.
1. Introduction
Aesthetics is becoming increasingly important in our society today. The growing attention to aesthetics inevitably also involves the care of the smile, thanks to the models proposed by magazines, social media, and social networks. It is essential that the aesthetics of the smile, although subordinate to function, meets the patient’s expectations [1,2].
Aesthetic dental treatments are aimed at resolving imperfections related to the shape, incorrect position, or excessively dark color of dental elements. For this reason, tooth whitening has found wide popularity, becoming one of the most popular and successful aesthetic treatments [3].
Tooth discoloration can be divided into intrinsic and extrinsic. Intrinsic discoloration is due to age (yellowing of dentine due to wear), genetics, post-traumatic formation abnormalities, fluorosis, antibiotics, and systemic diseases such as hepatitis. The intrinsic color of a tooth depends on how light is scattered and absorbed on the surface and within the tooth structures. Enamel does not completely cover the color of the underlying dentine, which therefore plays an important role in determining tooth color. It also has a certain porosity that makes it penetrable to particles capable of changing the color of the enamel and dentine itself. Extrinsic discoloration, on the other hand, is due to environmental factors such as smoke, food pigments, amalgam, endodontic cement, and restorations: colored composites can be absorbed in the acquired film or on the tooth surface, resulting in pigmentation [4,5,6].
Food and smoke particles bind much more with mature plaque and tartar than with enamel, which is why extrinsic pigmentations can be removed by the abrasive action of an ultrasonic scaler and controlled by good oral hygiene [7,8,9].
Modern bleaching systems are based on peroxides, namely hydrogen peroxide (HP) and carbamide peroxide (CP), that can be applied to or within the tooth. Oxygen penetrates the dental tissues and breaks up the large pigment molecules, making them shorter and uncolored, also resulting in desaturation of the yellow shade. However, the treatment is not recommended for children under the age of 14 and for pregnant or lactating women. After treatment, one should avoid food, colored drinks, and smoking for at least 24 h [10,11,12]. Nowadays, common concerns of patients relate to discoloration. Patients request a dental visit precisely because they are dissatisfied with their teeth color are therefore more interested in dental aesthetics. It is known how this problem has an impact on the patient’s social life, affecting their self-esteem and behaviors such as laughing, talking, and showing teeth without embarrassment [13].
The treatment option for this type of problem is tooth bleaching. The dentist or hygienist during patient history must identify all patients who are contraindicated to dental bleaching treatment. The principal contraindications of bleaching are prosthetic rehabilitation, pregnancy, diabetes, respiratory disease, photoreactive drugs, and allergy to peroxides (Table 1).

Table 1.
Contraindications of dental bleaching.
The purpose of this review is to introduce key aspects of bleaching and describe the different techniques and the mechanism of action of bleaching agents, focusing on the clinical implications in orthodontic patients and composite restorations.
2. Materials and Methods
2.1. Protocol and Registration
This review was conducted in accordance with the guidelines for Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) literature searches [14], and it was submitted to PROSPERO with a temporary number (391265).
2.2. Search Processing
We conducted searches in PubMed, Web of Science, and ScienceDirect to find articles that addressed our issue that were published between 2017 and 2023. The following Boolean keywords were incorporated into the search strategy because they perfectly matched the aim of our investigation, which primarily focuses on the characteristics of various peroxide types, their applications, positive and negative effects, and the maintenance of the result over time: (“dental bleaching” AND “peroxide”); (“tooth bleaching” AND “peroxide”) (Table 2).

Table 2.
Database search indicators.
2.3. Inclusion and Exclusion Criteria
The inclusion criteria were: (1) studies only on humans; (2) studies only in vivo; (3) studies only in English; (4) open access studies; (5) clinical trials or case reports; and (6) studies relating to the use of HP and CP and their comparison, their impact on composite restorations, and their use in orthodontics.
2.4. Data Processing
Author disagreements on the choice of articles were discussed and settled.
3. Results
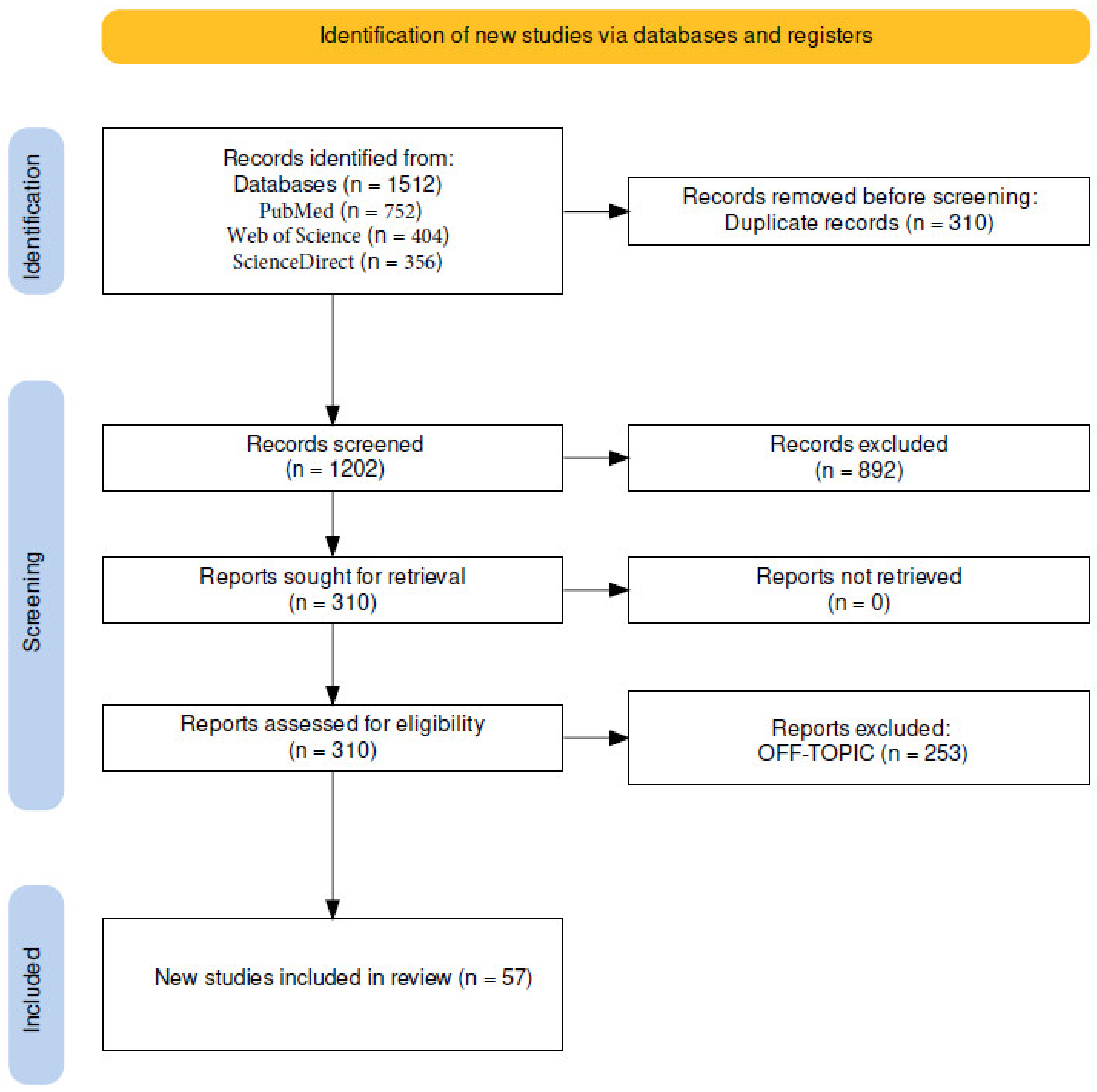
The electronic database search identified a total of 1512 studies (PubMed n = 752, Web of Science n = 404, and ScienceDirect n = 356) from the electronic searches, resulting in 1202 studies that remained after removing 310 duplicates. In total, 892 articles were excluded because of the title and abstract analysis. The last 310 reports were successfully obtained and after passing the retrieval stage; 253 publications in all had their discussion requests denied because off-topic; and 57 papers in all were considered in the review for qualitative analysis (Figure 1).
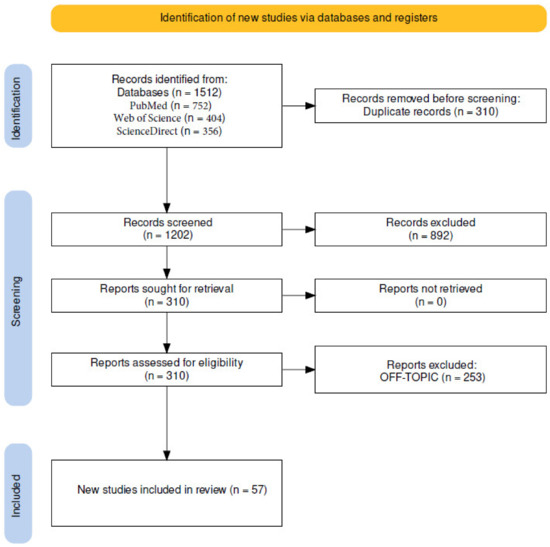
Figure 1.
Identification of studies via databases and registers (PRISMA flow-chart).
4. Discussion
Today’s most popular bleaching agents for both vital teeth and teeth subjected to root canal treatments are HP and CP, whose primary mechanism of action is based on their ability to oxidize the pigment molecules that cause discoloration [15]. In the following paragraphs, the different techniques of bleaching followed by the clinical implications in orthodontic and restorative dentistry are described.
4.1. Bleaching with Carbamide Peroxide
Tooth bleaching with CP is widely used in dentistry. For at-home bleaching treatment, the 10% CP concentration is regarded as the gold standard because of its extensive usage in at-home bleaching and the literature’s extensive documentation of its efficiency and safety [16].
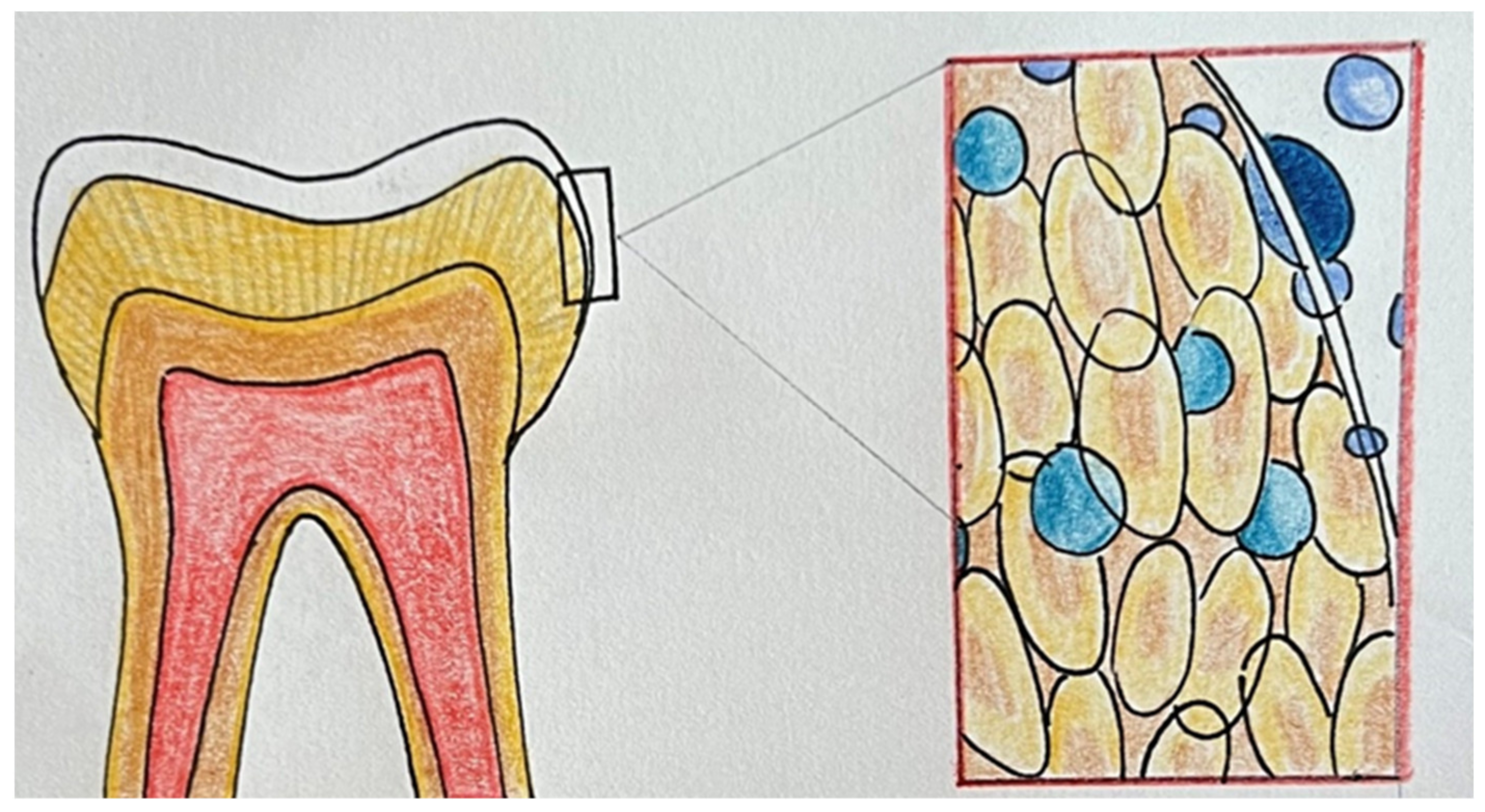
The CP can penetrate the enamel and dentin because of its low molecular weight. The primary mechanism by which the whitener works is by the oxidation of organic chemicals found in the tooth structure, which produces carbon dioxide and water. They release oxygen and free radicals when they come into contact with hard tissues, which oxidizes the pigments. The liberated oxygen permeates the dentinal tubules and acts by splitting the complex, highly colored carbon ring chains into smaller chains, creating the appearance of lighter structures [17].
When 37% CP was administered, increased gingival aggression and tooth sensitivity (TS) was anticipated. However, both may be lessened by reducing the daily usage time [16].
The tooth whitening with 37% CP used for 30 min each day exhibited an equivalent whitening effect to that of 10% CP used for 4 h each day, without increasing TS or causing gingival irritation. Therefore, using 37% CP for 30 min each day can be a practical solution to shorten the time needed to utilize a bleaching tray for at-home tooth whitening [16].
It has been also shown that there are no differences between trays whether reservoirs are present or not [18].
Some studies have pointed out that the quality of life and aesthetic impression of patients did not change significantly after using 10% CP at-home; however, a reduction of psychological distress was noticed [17] (Table 3).

Table 3.
Reported studies about bleaching with carbamide peroxide (CP).
4.2. Bleaching with Hydrogen Peroxide
Hydrogen peroxide (HP) is an active agent widely used during the procedure of external tooth bleaching, both in professional and in at-home-administered products [19,20].
The mechanism of action of HP is based on complex oxidation that causes the release of active oxygen species and the breakdown of pigments located in enamel and dentin. The active oxygen species formed by HP can permeate through the enamel prisms and reach the dentin, breaking down organic molecules [21].
The smaller and lighter compounds derived from the decomposition of organic molecules are responsible for the reflection of less color resulting in a whitening effect [22]. However, clinical studies reported that HP could reach the pulp chamber, causing adverse side effects. Biochemical changes in the dentin–pulp complex in response to bleaching agents are responsible for TS [23,24]. In vivo studies demonstrated that HP could cause oxidative stress to human dental pulp cells, interfering with odontoblastic differentiation. The presence of peroxides and their subproducts could activate the TRPA1 channel (transient receptor potential cation channel with ankyrin domain-type), which is associated with pain. In the same study, the authors demonstrated that the ozone therapy associated with HP does not interfere with bleaching and can reduce the side effects [21]. A study by Barbosa et al. revealed that remineralizing pastes, based on casein phospho-peptide–amorphous calcium phosphate (CPP–ACP), in association with 35% HP bleaching gel, could promote a significant reduction of pulp inflammation after bleaching [25]. Direct contact with HP could induce genotoxic effects on oral mucosa cells and gingival irritation [26]. In vivo, studies showed an increase of cytotoxic biomarkers in saliva, directly related to nuclear and oxidative DNA damage of oral mucosa cells directly exposed to HP-based products. These data suggest that caustic side effects could be due to a cellular protective mechanism of gingival and lip mucosa cells [27].
Changes in the enamel micro-hardness and increasing surface roughness because of bleaching products are effects reported in the literature [28]. The diffusion of HP on the hard tissue could depend on the concentration and contact time [29].
Many alternative methods in conjunction with HP products have been proposed to increase the biocompatibility of bleaching therapy. Several bleaching systems, application protocols, contact time, and different concentrations of HP gels were compared to detect the efficacy in terms of color and the risk of TS.
A clinical trial on 78 patients, carried out by Chemin et al., revealed that 10% HP increased the intensity of TS rather than 4% HP concentrations during at-home bleaching [23]. The risk of TS appears higher for 35% HP than for 15% HP after in-office bleaching treatment, according to the study by Lima et al. [30].
A study by Terra et al. showed that 30 min/day of 4% HP trays at-home application whitened teeth similarly to the recommended 120 min/day application time and significantly reduced TS [31].
In-office bleaching performed by 38% HP gel applied under different time protocols did not show differences in terms of efficacy whether the bleaching agent was used in a 40-min application or two 20-min applications, according to the results by Martins et al. [29].
Based on the study by Kim et al., a strip system of 2.9% HP was significantly more effective than the paint-on-type during at-home treatment [26].
At-home dental bleaching performed with 10% HP gel applied on the lingual surfaces seemed to promote worse results in bleaching efficacy rather than the application of gel on buccal surfaces [19].
A clinical trial on twenty-eight patients was carried out to assess the 1-year color stability produced by the different pH of HP gels when used as in-office treatments. No significant differences were obtained between the applications of neutral and acid gels [32].
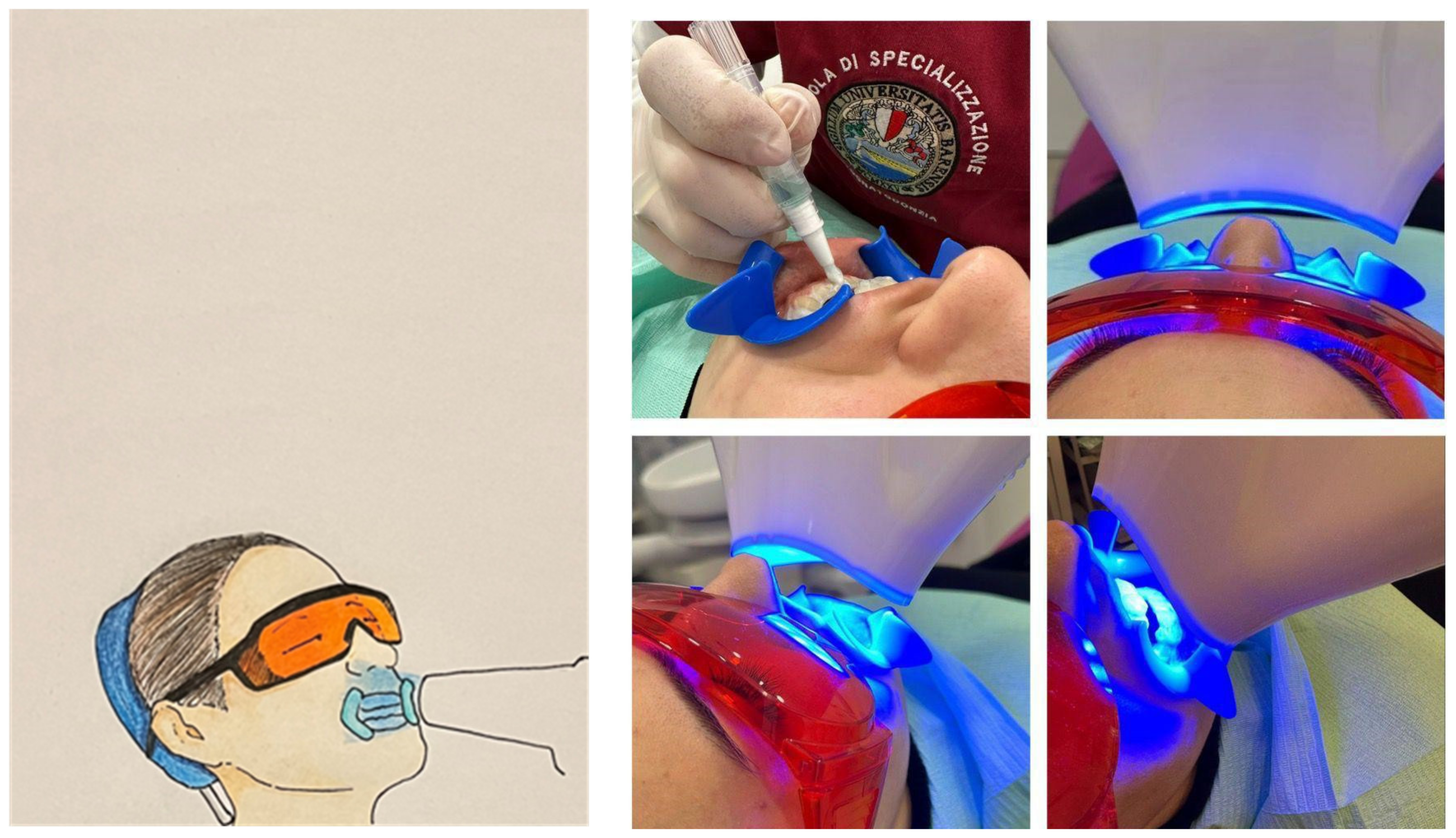
The use of LED/Laser irradiation on in-office dental bleaching did not show better results compared with the technique without a light source but seemed to give an advantage in the TS and in the activation time [33] (Figure 2).
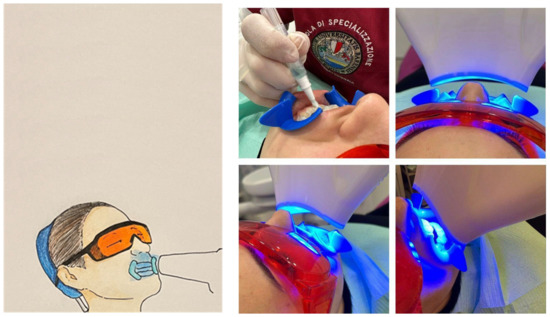
Figure 2.
The use of LED/Laser irradiation on in-office dental bleaching.
Several studies point out the use of in-office 6% HP gel with nitrogen titanium dioxide (TiO2) nanoparticles activated by LED/Laser source as efficient for dental bleaching. Bersezio et al. reported that there were no differences in the efficacy of a single application of 72 min of 6% HP with nitrogen TiO2 nanoparticles or two applications of 36 min [34] (Table 4).

Table 4.
Reported studies about bleaching with hydrogen peroxide [HP: hydrogen peroxide, IL: interleukine, TS: tooth sensitivity].
4.3. Comparison between the Use of Carbamide Peroxide and Hydrogen Peroxide
In a 6 month follow-up study conducted in 2017, Aka and Celik examined the bleaching efficiency of two at-home bleaching systems using preloaded trays with 6% HP and custom trays with 10% CP on teeth of varied colors [38].
Ninety-two patients were randomly assigned to one of three groups: no bleaching agent application (control group), patients treated with a custom-made tray containing 10% CP (10% CP/PF) (Opalescence PF), and patients treated with a pre-loaded tray containing 6% HP (6% HP/Go) (Opalescence Go). The color values were assessed at the beginning, after 10 and 14 days, and after 6 months of bleaching. When compared to the control group, both bleaching systems were clinically effective and produced higher bleaching efficacy [39].
The 10% CP/PF showed higher bleaching efficacy than the 6% HP/Go; the higher bleaching efficacy of 10% CP/PF may be related to the longer application duration despite its lower HP concentration [39].
Ana Rita Barcessat et al., analyzed the dental color stabilization of upper incisors and canines in 60 patients undergoing different bleaching techniques: group 1 (35% HP in-office bleaching), group 2 (in-office application of 3% HP followed by in-office bleaching using 35% HP), group 3 (3% HP in-office bleaching), and group 4 (10% CP at-home-bleaching) [40].
Differences in canine’s chroma were noted in a short-term evaluation (after the 3rd session for groups 1, 2, and 3, and 7 days after at-home bleaching): in group 1 and group 2, canine’s chroma was significantly lower than in group 4. However, lightness increased in all groups with no statistical difference 60 days after treatment [40]
Concerning TS, it is strongly linked to the presence of peroxides and their reaction products reaching the pulpal chamber causing an inflammatory response [41]. As a result of the lower concentration of HP available, CP can be used to reduce TS (Figure 3).
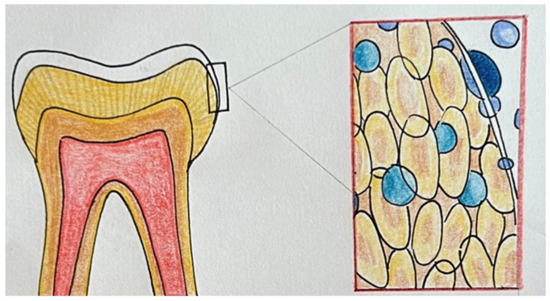
Figure 3.
Chemical mechanism of bleaching systems.
Peixoto et al., compared the effectiveness of whitening and its effect on TS of two different at-home bleaching techniques: 37% CP and 35% HP [41].
The results of this clinical study demonstrated that when used in a single 40 min in-office application, high concentrations of CP (37%) effectively achieve satisfactory bleaching effects [41].
Despite producing less color change than 35% HP, 37% CP reduced significantly both the risk and level of TS experienced by patients [41].
HP and CP are used in high concentrations for endodontically treated teeth (non-vital teeth) [42].
Cristian Bersezio et al. evaluate the psychosocial impact and aesthetic perceptions of 42 patients undergoing non-vital tooth bleaching with HP (35%) and CP (37%). The color change (ΔE) has been evaluated at 1 week, 1 month, and 3 months after bleaching [42].
The results of the current study demonstrate that both gels were highly effective, and the color change lasts at least three months [42] (Table 5).

Table 5.
Reported studies about comparison between the use of carbamide peroxide and hydrogen peroxide [CP: carbamide peroxide, HP: hydrogen peroxide, TS: tooth sensitivity].
4.4. Comparison between In-Office and At-Home Dental Bleaching
The use of low bleaching agent concentrations (10–16% CP or 6% HP) applied for at least two weeks is indicated for at-home bleaching [41].
For in-office procedures, bleaching agents (HP 25–40% or CP 35%) are applied for shorter amounts of time with or without light activation [41].
It can be performed at-home or in-office with a wide range of techniques. At-home-bleaching treatment tray-based system uses trays built on an impression and prepared in the laboratory, the bleaching gel is placed inside the trays and used for a few hours during the day or overnight for a few days (from two to three weeks) [42,43] (Figure 4).

Figure 4.
Home bleaching, trays built.
On the other hand, in-office bleaching is performed chairside and uses a bleaching gel with higher concentrations of hydroxide placed on the tooth for minutes, activated by an LED light [18] (Figure 5 and Figure 6).

Figure 5.
(a) Dental bleaching in dental clinic with a liquid dam is an advantage to avoid gingival tissue irritation. (b) Before the treatment, and (c) after the treatment.

Figure 6.
Clinical case of bleaching before and after the treatment.
Different bleaching protocols based on HP and CP concentrations have been proposed in the literature [44].The classic at home-bleaching was described by Chemin in 2018. He used a bleaching gel containing 10% calcium hydroxide inside trays using for 30 min, twice daily for 2 weeks. After one month of follow-up, the bleaching was significant [45]. Maran and Fraga Briso proposed an at-home bleaching protocol with a 10% HP gel containing a desensitizing gel (3% potassium nitrate and 0.2% sodium fluoride) inside it. The authors compared it with a gel of the same HP concentration but without desensitizer. Both were used for 3 h a day for 21 days. There was no difference reported in either TS or color [46,47]. In addition, Martini stated that the presence of a reservoir in a bleaching tray did not influence the effectiveness of the treatment, TS, and gingival irritation [48]. Sutil compared two at-home techniques using bleaching gels (10% versus 37% CP). Both were used for 3 weeks. The first group (CP 10%) used it for 4 h a day, and the second group (CP 37%) used it for 30 min a day. The result was the same. Therefore, the authors suggest using bleaching gel containing a higher percentage of CP but took less time to use [16]. The most widely used protocol for at-home bleaching is described by López Darriba. He used low concentrations of CP (10%) overnight [49]. The same author in another study compared the same concentration of CP (10%) for 14 and 21 days and he deduced that 3 weeks is the best duration to obtain good bleaching [50]. Vildósola et al. showed in-office bleaching mode. In his study, he compared a concentration of HP (6%) with an application of 36 min for a session versus 3 applications of 12 min for a session. The authors proved the moderate efficacy and similar TS [51]. Ermis, in his study, suggested that the efficacy of treatment is affected by tooth decalcification and the trayless system type, while the trayless system influenced the duration of the treatment [52]. Piknjač’s used 40% HP for 3 applications every 20 min in a single session and showed the significant efficacy of the bleaching over the 6 month follow-up period [52]. Matteo Kury used a purple LED without any bleaching gel and he obtained a good long-term result (with a follow-up of 6 to 12 months) [53]. Saeger Meireles showed how in-office bleaching using 37.5% HP in two sessions of 8 min allowed the same degree of bleaching with less TS than 3 sessions of 8 min [54]. Vaez proposed the combination of both techniques: 35% HP in office for 45 min and 10% CP for 1 h at-home, reducing the time needed for satisfactory treatment but increasing TS [55]. In Mayer Santos’ work, a hybrid treatment is proposed using 35% HP with different modes of use (between at-home and in-office bleaching) with effective treatment and less TS [56,57].
In conclusion, both bleaching techniques are effective. Specifically, in-office-bleaching uses a high concentration of molecules (HP and CP) obtaining immediate treatment but with high TS. On the other hand, at-home-bleaching uses low concentrations obtaining lower TS but equal or even higher bleaching efficacy [58]. The prolonged treatment can cause gingival irritation due to the over-edge of the gel over trays; this is difficult to obtain in-office bleaching with the use of a liquid dam [59,60]. Mounika and Rodrigues, in their experimental studies, did not find a significant difference in efficacy between in-office or at-home bleaching [61]. In addition, some authors combine the two techniques to determine higher efficacy and lower TS [62]. It is recommended to assess the patient’s needs and choose the best treatment for each patient, avoiding the worsening of the tooth and soft tissue health due to the side effects of bleaching gels [63] (Table 6).

Table 6.
Reported studies about comparison between in office and at-home dental bleaching [CP: carbamide peroxide, HP: hydrogen peroxide, TS: tooth sensitivity].
4.5. Effect of Dental Bleaching in Orthodontic Treatment
Bleaching during and after orthodontic treatment was investigated in vivo only in a few articles and must be examined more.
Levrini et al. demonstrated that at-home bleaching using orthodontic aligners or thermoformed bleaching trays with reservoirs was equally effective using spectrophotometry. In this study, a finite element analysis reported that the distribution of 2 m3 of gel at the center of the vestibular surfaces of teeth is sufficient to distribute it to all the vestibular surface while wearing aligners [63,65].
The association between at-home dental bleaching with 10% CP and the removal of bonded material leftovers using a super fine, tapered diamond bur followed using an enamel micro abrasion product after orthodontic bracket debonding is shown in the clinical case reports by Pavani et al. [65,66].
The suggested procedure significantly enhanced aesthetics and successfully eliminated grooves left behind when the bonding composite was removed, leaving a smooth enamel surface.
Gomes reported two case reports of in-office bleaching treatment conducted using two or three 40 min sessions using 35% HP. The teeth were successfully bleached despite the presence of brackets fulfilling patients’ expectations of straightened and whitened teeth [66].
In a randomized clinical trial of Ahrari et al. investigating different bleaching techniques on patients a maximum of three months after fixed multibracket appliance removal, the individuals were divided into four groups according to the way of bleaching [67]. While individuals in group 1 got at-home bleaching, patients in groups 2 through 4 underwent in-office bleaching utilizing a diode laser, a plasma arc, and no light source, respectively. At-home bleaching resulted in a positive color change. Laser-assisted bleaching should be regarded as the finest alternative among in-office procedures because it delivered effective outcomes with the least amount of TS and in the shortest amount of time [68] (Table 7).

Table 7.
Reported studies about the effect of dental bleaching in orthodontic treatment.
4.6. Effects of Dental Bleaching on Composite Restorations
In the literature, the effect of bleaching on composites has been evaluated in a few randomized controlled trials, which examined mainly microhybrid resins and nanocomposites. Composites are resin-based monomeric materials, which have now replaced metal and amalgam, in dental restoration procedures after caries removal. Composites are made up of two or more materials useful to provide more performing characteristics or to add additional functionality to the original components [69,70,71]. With the development of micro/nano-science and technology, other filling materials and natural minerals in various shapes and sizes have been added to the traditional composite resins made of quartz filler and strontium or barium glass, resulting in an improvement in mechanical qualities [70]. The materials used as filler in nanofilled are Zirconia/Silica and nanosilica, while hybrid composite resin is a combination of macrofilled and microfilled [72,73].
The randomized controlled clinical trial of Elhoshy et al. analyzed the effect of 15% CP bleaching gel for at-home use on two types of composite resin restorations, namely nanocomposite and microhybrid. The parameters evaluated when taking digital photographs are color patterns, opacity, and fluorescence. At 2 weeks, microhybrid composites show superiority in terms of color patterns. On the other hand, the mean opacity and fluorescence values show no statistically significant differences [72].
Mereiles et al. also evaluated the at-home bleaching procedure with 10% CP in a randomized controlled trial on anterior maxillary teeth. The parameters analyzed this time was color changes and TS, comparing decayed teeth and non-decayed teeth at week 2 after whitening. The authors concluded that there is a lower degree of whiteness in teeth that had undergone a restoration compared to healthy ones. On the other hand, regarding TS being the most frequent side effect of a bleaching procedure, they did not detect any statistically significant difference [74] (Table 8).

Table 8.
Reported studies about effects of dental bleaching on composite restorations.
From these works, it can be assumed that it is not rational to change the type of restoration after a bleaching procedure in the absence of aesthetic problems and that it may be necessary, after bleaching, to replace the restorations to achieve better aesthetic results.
5. Conclusions
The use of CP at 37% increases gingival inflammation and TS, and exhibits an equal effect to that of 10%. HP could damage the dentin–pulp complex causing pain and TS and shows a cytotoxic effect on the oral mucosa. To increase the biocompatibility of HP, many alternatives have been proposed as different concentrations and time protocols, or the association with LED irradiation, which do no demonstrate significant amelioration. Regarding the comparation of the two systems, the investigation revealed that both gels were clinically effective although CP seems to reduce the level of TS in the patients. No significant differences between at-home and in-office bleaching have been found, and the combination of both techniques improves the efficacy, also reducing the time needed for satisfactory treatment. Concerning at-home bleaching, the addition of a desensitizing gel does not report benefits in either TS or color and the presence of a reservoir in the tray does not influence the results. Orthodontic aligners could be used as a tray for this technique. It has been demonstrated that after orthodontic treatment, the teeth were successfully bleached, and all methods seem to be effective in managing tooth discoloration after the removal of the bracket’s composite. The efficacy of bleaching on composites needs further research to be improved; however, at the current state, microhybrid composites seem to show superiority in terms of colors compared to nanocomposites.
A tailored approach is advised to evaluate each patient’s needs and select the best protocol to obtain the required outcomes and prevent the adverse effects of bleaching gels on the tooth and soft tissues.
Author Contributions
Conceptualization, A.D.I., A.M.I., G.M., F.P., A.P. and C.D.P.; methodology, A.M.C., G.P., E.X. and E.d.R., software, A.M.C., G.G., V.S., F.I. and G.D.; validation, E.X., G.M., I.R.B., A.P., D.D.V., F.P., V.S., F.I. and G.D.; formal analysis, A.D.I., F.P., A.P., A.M.C., I.R.B., D.D.V., F.I. and G.D.; resources, A.D.I., A.M.I., G.M., C.D.P., C.L. and S.B.; data curation, G.M., I.R.B., G.G., F.I. and G.D.; writing—original draft preparation, A.D.I., A.M.I., E.d.R., S.B., C.L., G.P., G.L., E.X., V.S., D.D.V., E.X., F.I. and G.D.; writing—review and editing, A.P., A.M.C., G.P., E.d.R., I.R.B. and S.B. visualization, G.P.,C.D.P., G.L., F.I., A.P., V.S. and I.R.B.; supervision, A.D.I., A.M.I., F.P., G.M., D.D.V., F.I. and G.D.; project administration, G.G., C.L., I.R.B., F.I. and G.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CP | Carbamide peroxide |
| CPP–ACP | Casein phospho-peptide–amorphous calcium phosphate |
| FEA | Finite element analysis |
| HP | Hydrogen peroxide |
| SGU | Shade guide units |
| TiO2 | Nitrogen titanium dioxide |
| TS | Tooth sensitivity |
References
- Isiekwe, G.I.; Sofola, O.O.; Onigbogi, O.O.; Utomi, I.L.; Sanu, O.O.; daCosta, O.O. Dental Esthetics and Oral Health-Related Quality of Life in Young Adults. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 627–636. [Google Scholar] [CrossRef]
- Cantore, S.; Ballini, A.; Farronato, D.; Malcangi, G.; Dipalma, G.; Assandri, F.; Garagiola, U.; Inchingolo, F.; De Vito, D.; Cirulli, N. Evaluation of an Oral Appliance in Patients with Mild to Moderate Obstructive Sleep Apnea Syndrome Intolerant to Continuous Positive Airway Pressure Use: Preliminary Results. Int. J. Immunopathol. Pharmacol. 2016, 29, 267–273. [Google Scholar] [CrossRef] [PubMed]
- Van der Geld, P.; Oosterveld, P.; Van Heck, G.; Kuijpers-Jagtman, A.M. Smile Attractiveness. Self-Perception and Influence on Personality. Angle Orthod. 2007, 77, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Carey, C.M. Tooth Whitening: What We Now Know. J. Evid. Based Dent. Pract. 2014, 14, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, C.; Di Bartolo, I.; Santantonio, M.; Coscia, M.F.; Monno, R.; De Vito, D.; Ruggeri, F.M.; Rizzo, G. Epidemiological and Virological Investigation of a Norovirus Outbreak in a Resort in Puglia, Italy. BMC Infect. Dis. 2007, 7, 135. [Google Scholar] [CrossRef] [PubMed]
- De Vito, D.; Monno, R.; Nuccio, F.; Legretto, M.; Oliva, M.; Coscia, M.F.; Dionisi, A.M.; Calia, C.; Capolongo, C.; Pazzani, C. Diffusion and Persistence of Multidrug Resistant Salmonella Typhimurium Strains Phage Type DT120 in Southern Italy. BioMed Res. Int. 2015, 2015, 265042. [Google Scholar] [CrossRef] [PubMed]
- Halabi, S.; Matsui, N.; Nikaido, T.; Abdo, A.; Burrow, M.F.; Tagami, J. Effect of Two Bleaching Regimens on Enamel Bonding Performance. Dent. Mater. J. 2020, 39, 984–991. [Google Scholar] [CrossRef]
- Coscia, M.F.; Monno, R.; Ballini, A.; Mirgaldi, R.; Dipalma, G.; Pettini, F.; Cristallo, V.; Inchingolo, F.; Foti, C.; de Vito, D. Human Papilloma Virus (HPV) Genotypes Prevalence in a Region of South Italy (Apulia). Ann. Ist. Super Sanita 2015, 51, 248–251. [Google Scholar] [CrossRef]
- Farronato, M.; Boccalari, E.; Del Rosso, E.; Lanteri, V.; Mulder, R.; Maspero, C. A Scoping Review of Respirator Literature and a Survey among Dental Professionals. Int. J. Environ. Res. Public Health 2020, 17, 5968. [Google Scholar] [CrossRef]
- Kwon, S.R.; Wertz, P.W. Review of the Mechanism of Tooth Whitening. J. Esthet. Restor. Dent. 2015, 27, 240–257. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Fama, A.; Cavagnetto, D.; Abate, A.; Farronato, M. Treatment of Dental Dilacerations. J. Biol. Regul. Homeost. Agents 2019, 33, 1623–1627. [Google Scholar]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D Cephalometry on Reduced FOV CBCT: Skeletal Class Assessment through AF-BF on Frankfurt Plane—Validity and Reliability through Comparison with 2D Measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef]
- Pereira, R.; Silveira, J.; Dias, S.; Cardoso, A.; Mata, A.; Marques, D. Bleaching Efficacy and Quality of Life of Different Bleaching Techniques-Randomized Controlled Trial. Clin. Oral Investig. 2022, 26, 7167–7177. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Sutil, E.; da Silva, K.L.; Terra, R.M.O.; Burey, A.; Rezende, M.; Reis, A.; Loguercio, A.D. Effectiveness and Adverse Effects of At-Home Dental Bleaching with 37% versus 10% Carbamide Peroxide: A Randomized, Blind Clinical Trial. J. Esthet. Restor. Dent. 2022, 34, 313–321. [Google Scholar] [CrossRef]
- Tavarez, R.-R.-D.J.; Lima, S.-N.-L.; Malheiros, A.-S.; Menezes, L.-L.; Bandeca, M.-C.; de Miranda, R.C.-M.; Ferreira, M.-C. Assessment of the Aesthetic Impact and Quality of Life of Home Dental Bleaching in Adult Patients. J. Clin. Exp. Dent. 2021, 13, e440–e445. [Google Scholar] [CrossRef]
- Martini, E.C.; Favoreto, M.W.; de Andrade, H.F.; Coppla, F.M.; Loguercio, A.D.; Reis, A. One-Year Follow-up Evaluation of Reservoirs in Bleaching Trays for at-Home Bleaching. J. Esthet. Restor. Dent. 2021, 33, 992–998. [Google Scholar] [CrossRef]
- Silva, L.M.; da Costa Lacerda, Í.A.; Dos Santos, D.B.; Herkrath, F.J.; da Silva, K.L.; Loguercio, A.D.; de Moura Martins, L. Is the At-Home Bleaching Treatment Applied Only on the Lingual Surface as Effective as That on the Buccal Surface? A Randomized Clinical Trial. Clin. Oral Investig. 2022, 26, 1551–1560. [Google Scholar] [CrossRef] [PubMed]
- Estay, J.; Angel, P.; Bersezio, C.; Tonetto, M.; Jorquera, G.; Peña, M.; Fernández, E. The Change of Teeth Color, Whiteness Variations and Its Psychosocial and Self-Perception Effects When Using Low vs. High Concentration Bleaching Gels: A One-Year Follow-Up. BMC Oral Health 2020, 20, 255. [Google Scholar] [CrossRef] [PubMed]
- Tavares, N.R.N.O.; Galvão, A.d.M.; Dietrich, L.; Carvalho, R.F.; Silva, R.S.; Silva, A.L.F.E.; da Silva, G.R. Can Ozone or Violet Light Improve the Color Change or Physicochemical Properties of Hydrogen Peroxide-Bleached Tooth? Braz. Dent. J. 2021, 32, 19–30. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, D.; Moreira, A.; Cornacchia, T.; Magalhães, C. Evaluation of the Effect of Different Enamel Surface Treatments and Waiting Times on the Staining Prevention after Bleaching. J. Clin. Exp. Dent. 2017, 9, e677–e681. [Google Scholar] [CrossRef]
- Chemin, K.; Rezende, M.; Loguercio, A.D.; Reis, A.; Kossatz, S. Effectiveness of and Dental Sensitivity to At-Home Bleaching With 4% and 10% Hydrogen Peroxide: A Randomized, Triple-Blind Clinical Trial. Oper. Dent. 2018, 43, 232–240. [Google Scholar] [CrossRef]
- Bersezio, C.; Estay, J.; Jorquera, G.; Peña, M.; Araya, C.; Angel, P.; Fernández, E. Effectiveness of Dental Bleaching With 37.5% and 6% Hydrogen Peroxide and Its Effect on Quality of Life. Oper. Dent. 2019, 44, 146–155. [Google Scholar] [CrossRef]
- Barbosa, J.G.; Benetti, F.; de Oliveira Gallinari, M.; Carminatti, M.; da Silva, A.B.D.; Lopes, I.N.I.; Briso, A.L.F.; Cintra, L.T.A. Bleaching Gel Mixed with MI Paste Plus Reduces Penetration of H2O2 and Damage to Pulp Tissue and Maintains Bleaching Effectiveness. Clin. Oral Investig. 2020, 24, 1299–1309. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.M.; Ha, A.N.; Kim, J.W.; Kim, S.J. Double-Blind Randomized Study to Evaluate the Safety and Efficacy of Over-the-Counter Tooth-Whitening Agents Containing 2.9% Hydrogen Peroxide. Oper. Dent. 2018, 43, 272–281. [Google Scholar] [CrossRef]
- Del Real García, J.F.; Saldaña-Velasco, F.R.; Sánchez-de la Rosa, S.V.; Ortiz-García, Y.M.; Morales-Velazquez, G.; Gómez-Meda, B.C.; Zúñiga-González, G.M.; Sánchez-Parada, M.G.; Zamora-Perez, A.L. In Vivo Evaluation of the Genotoxicity and Oxidative Damage in Individuals Exposed to 10% Hydrogen Peroxide Whitening Strips. Clin. Oral Investig. 2019, 23, 3033–3046. [Google Scholar] [CrossRef] [PubMed]
- Youssef, S.A.; Cunha, S.R.; Mayer-Santos, E.; Brito, S.A.; de Freitas, P.M.; Ramalho, J.; Morimoto, S.; Gonçalves, F.; Ramalho, K.M. Influence of 35% Hydrogen Peroxide Gel Renewal on Color Change during In-Office Dental Photobleaching with Violet LED: A Split-Mouth Randomized Controlled Clinical Trial. Photodiagnosis Photodyn. Ther. 2021, 36, 102509. [Google Scholar] [CrossRef] [PubMed]
- Martins, I.; Onofre, S.; Franco, N.; Martins, L.M.; Montenegro, A.; Arana-Gordillo, L.A.; Reis, A.; Loguercio, A.D.; da Silva, L.M. Effectiveness of In-Office Hydrogen Peroxide With Two Different Protocols: A Two-Center Randomized Clinical Trial. Oper. Dent. 2018, 43, 353–361. [Google Scholar] [CrossRef]
- Lima, S.N.L.; Ribeiro, I.S.; Grisotto, M.A.; Fernandes, E.S.; Hass, V.; de Jesus Tavarez, R.R.; Pinto, S.C.S.; Lima, D.M.; Loguercio, A.D.; Bandeca, M.C. Evaluation of Several Clinical Parameters after Bleaching with Hydrogen Peroxide at Different Concentrations: A Randomized Clinical Trial. J. Dent. 2018, 68, 91–97. [Google Scholar] [CrossRef]
- Terra, R.; da Silva, K.L.; Vochikovski, L.; Sutil, E.; Rezende, M.; Loguercio, A.D.; Reis, A. Effect of Daily Usage Time of 4% Hydrogen Peroxide on the Efficacy and Bleaching-Induced Tooth Sensitivity: A Single-Blind Randomized Clinical Trial. Oper. Dent. 2021, 46, 395–405. [Google Scholar] [CrossRef]
- Bersezio, C.; Martín, J.; Prieto, M.V.; Meneses, P.; Angel, P.; Eduardo Fernández, G.; Loguercio, A. One-Year Bleaching Efficacy Using Two HP Products with Different PH: A Double-Blind Randomized Clinical Trial. J. Esthet. Restor. Dent. 2019, 31, 493–499. [Google Scholar] [CrossRef] [PubMed]
- Mondelli, R.; Rizzante, F.; Rosa, E.R.; Borges, A.; Furuse, A.Y.; Bombonatti, J. Effectiveness of LED/Laser Irradiation on In-Office Dental Bleaching after Three Years. Oper. Dent. 2018, 43, 31–37. [Google Scholar] [CrossRef]
- Bersezio, C.; Pardo, C.; Miranda, S.; Medeiros Maran, B.; Jorquera, G.; Rosa da Silva, A.; Tonetto Rodrigues, M.; Fernández, E. Evaluation of the Effectiveness in Teeth Whitening of a Single Session with 6% Hydrogen Peroxide Laser/LED System. Photodiagnosis Photodyn. Ther. 2021, 36, 102532. [Google Scholar] [CrossRef]
- Angel, P.; Bersezio, C.; Estay, J.; Werner, A.; Retamal, H.; Araya, C.; Martin, J.; Fernández, E. Color Stability, Psychosocial Impact, and Effect on Self-Perception of Esthetics of Tooth Whitening Using Low-Concentration (6%) Hydrogen Peroxide. Quintessence Int. 2018, 49, 557–566. [Google Scholar] [CrossRef]
- Ferraz, N.K.L.; Nogueira, L.C.; Neiva, I.M.; Ferreira, R.C.; Moreira, A.N.; Magalhães, C.S. Longevity, Effectiveness, Safety, and Impact on Quality of Life of Low-Concentration Hydrogen Peroxides in-Office Bleaching: A Randomized Clinical Trial. Clin. Oral Investig. 2019, 23, 2061–2070. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, T.C.; Bortolatto, J.F.; Rizzi, G.; Meloto, B.T.; Dantas, A.A.R.; de Oliveira Junior, O.B. Clinical Performance of 6% Hydrogen Peroxide Containing TiO2N Nanoparticles Activated by LED in Varying Wavelengths-a Randomized Clinical Trial. Lasers Med. Sci. 2022, 37, 2017–2024. [Google Scholar] [CrossRef]
- Bersezio, C.; Martín, J.; Angel, P.; Bottner, J.; Godoy, I.; Avalos, F.; Fernández, E. Teeth Whitening with 6% Hydrogen Peroxide and Its Impact on Quality of Life: 2 Years of Follow-Up. Odontology 2019, 107, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Celik, E.U. Evaluation of the Efficacy and Color Stability of Two Different At-Home Bleaching Systems on Teeth of Different Shades: A Randomized Controlled Clinical Trial. J. Esthet. Restor. Dent. 2017, 29, 325–338. [Google Scholar] [CrossRef]
- Barcessat, A.R.; Gurgel-Juarez, N.C.; Wetter, N.U. Vital Tooth Bleaching Using Different Techniques: A Clinical Evaluation. Future Dent. J. 2018, 5, S2314718018300831. [Google Scholar] [CrossRef]
- Llena, C.; Collado-González, M.; García-Bernal, D.; Oñate-Sánchez, R.E.; Martínez, C.M.; Moraleda, J.M.; Rodríguez-Lozano, F.J.; Forner, L. Comparison of Diffusion, Cytotoxicity and Tissue Inflammatory Reactions of Four Commercial Bleaching Products against Human Dental Pulp Stem Cells. Sci. Rep. 2019, 9, 7743. [Google Scholar] [CrossRef]
- Peixoto, A.C.; Vaez, S.C.; Pereira, N.A.d.R.; da Silva Santana, C.N.; Soares, K.D.A.; Romão, A.C.T.R.; Ferreira, L.F.; Martins-Filho, P.R.S.; Faria-E-Silva, A.L. High-Concentration Carbamide Peroxide Can Reduce the Sensitivity Caused by in-Office Tooth Bleaching: A Single-Blinded Randomized Controlled Trial. J. Appl. Oral Sci. 2018, 26, e20170573. [Google Scholar] [CrossRef]
- Bersezio, C.; Martín, J.; Mayer, C.; Rivera, O.; Estay, J.; Vernal, R.; Haidar, Z.S.; Angel, P.; Oliveira, O.B.; Fernández, E. Quality of Life and Stability of Tooth Color Change at Three Months after Dental Bleaching. Qual. Life Res. 2018, 27, 3199–3207. [Google Scholar] [CrossRef]
- Mounika, A.; Mandava, J.; Roopesh, B.; Karri, G. Clinical Evaluation of Color Change and Tooth Sensitivity with In-Office and Home Bleaching Treatments. Indian J. Dent. Res. 2018, 29, 423. [Google Scholar] [CrossRef]
- Chemin, K.; Rezende, M.; Milan, F.M.; Dantas, T.B.; Gomes, K.d.N.; Kossatz, S. Clinical Evaluation of 10% Hydrogen Peroxide on Tooth Sensitivity and Effectiveness in at Home Dental Bleaching. J. Contemp. Dent. Pract. 2018, 19, 1376–1380. [Google Scholar] [CrossRef] [PubMed]
- Maran, B.M.; Vochikovski, L.; de Andrade Hortkoff, D.R.; Stanislawczuk, R.; Loguercio, A.D.; Reis, A. Tooth Sensitivity with a Desensitizing-Containing at-Home Bleaching Gel—A Randomized Triple-Blind Clinical Trial. J. Dent. 2018, 72, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Briso, A.L.F.; Rahal, V.; de Azevedo, F.A.; de Gallinari, M.O.; Gonçalves, R.S.; Frascino, S.M.B.; Santos, P.H.D.; Cintra, L.T.A. Neurosensory Analysis of Tooth Sensitivity during At-Home Dental Bleaching: A Randomized Clinical Trial. J. Appl. Oral Sci. 2018, 26, e20170284. [Google Scholar] [CrossRef]
- Martini, E.C.; Favoreto, M.W.; Coppla, F.M.; Loguercio, A.D.; Reis, A. Evaluation of Reservoirs in Bleaching Trays for At-Home Bleaching: A Split-Mouth Single-Blind Randomized Controlled Equivalence Trial. J. Appl. Oral Sci. 2020, 28, e20200332. [Google Scholar] [CrossRef] [PubMed]
- López Darriba, I.; Novoa, L.; de la Peña, V.A. Efficacy of Different Protocols for At-Home Bleaching: A Randomized Clinical Trial. Am. J. Dent. 2017, 30, 329–334. [Google Scholar]
- Darriba, I.L.; Cabirta Melón, P.; García Sartal, A.; Ríos Sousa, I.; Alonso de la Peña, V. Influence of Treatment Duration on the Efficacy of At-Home Bleaching with Daytime Application: A Randomized Clinical Trial. Clin. Oral Investig. 2019, 23, 3229–3237. [Google Scholar] [CrossRef]
- Vildósola, P.; Vera, F.; Ramírez, J.; Rencoret, J.; Pretel, H.; Oliveira, O.; Tonetto, M.; Martín, J.; Fernández, E. Comparison of Effectiveness and Sensitivity Using Two In-Office Bleaching Protocols for a 6% Hydrogen Peroxide Gel in a Randomized Clinical Trial. Oper. Dent. 2017, 42, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Ermis, R.B.; Uzer Celik, E.; Yildiz, G.; Yazkan, B. Effect of Tooth Discolouration Severity on the Efficacy and Colour Stability of Two Different Trayless At-Home Bleaching Systems. J. Dent. Res. Dent. Clin. Dent. Prospects 2018, 12, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Piknjač, A.; Zlatarić, D.K. Clinical Evaluation of 6-Month Efficacy of 40% in-Office Whitening Treatment. Pesqui. Bras. Odontopediatria Clín. Integr. 2021, 21, e0236. [Google Scholar] [CrossRef]
- Kury, M.; Wada, E.E.; da Silva Palandi, S.; Picolo, M.Z.D.; Giannini, M.; Cavalli, V. Colorimetric Evaluation after In-Office Tooth Bleaching with Violet LED: 6- and 12-Month Follow-Ups of a Randomized Clinical Trial. Clin. Oral Investig. 2022, 26, 837–847. [Google Scholar] [CrossRef]
- Meireles, S.S.; Santos, M.E.; Lustosa, Í.M.C.; Leite, E.L.L. Effects of a Reduced In-office Bleaching Protocol with 37.5% Hydrogen Peroxide on Effectiveness and Tooth Sensitivity: A Double-blind Randomized Clinical Trial. J. Esthet. Restor. Dent. 2021, 33, 824–831. [Google Scholar] [CrossRef] [PubMed]
- Vaez, S.; Correia, A.; Santana, T.; Santana, M.; Peixoto, A.; Leal, P.; Faria-e-Silva, A. Is a Single Preliminary Session of In-Office Bleaching Beneficial for the Effectiveness of At-Home Tooth Bleaching? A Randomized Controlled Clinical Trial. Oper. Dent. 2019, 44, E180–E189. [Google Scholar] [CrossRef]
- Mayer-Santos, E.; Bachiega-Silva, B.; Twiaschor, C.V.; Shimokawa, C.A.K.; Marinho, G.B.; Junior, A.B.; Zanin, F.; Brugnera, A.P.; Ramalho, K.M.; de Freitas, P.M. Blinded, Parallel and Randomized Clinical Evaluation of in-Office Dental Bleaching with Violet LED (405–410 nm). Photodiagnosis Photodyn. Ther. 2022, 38, 102739. [Google Scholar] [CrossRef]
- Piknjač, A.; Soldo, M.; Ileš, D.; Knezović Zlatarić, D. Patients’ Assessments of Tooth Sensitivity Increase One Day Following Different Whitening Treatments. Acta Stomatol. Croat. 2021, 55, 280–290. [Google Scholar] [CrossRef] [PubMed]
- Donassollo, S.H.; Donassollo, T.A.; Coser, S.; Wilde, S.; Uehara, J.L.S.; Chisini, L.A.; Correa, M.B.; Cenci, M.S.; Demarco, F.F. Triple-Blinded Randomized Clinical Trial Comparing Efficacy and Tooth Sensitivity of in-Office and at-Home Bleaching Techniques. J. Appl. Oral Sci. 2021, 29, e20200794. [Google Scholar] [CrossRef] [PubMed]
- Dourado Pinto, A.V.; Carlos, N.R.; do Amaral, F.L.B.; França, F.M.G.; Turssi, C.P.; Basting, R.T. At-Home, in-Office and Combined Dental Bleaching Techniques Using Hydrogen Peroxide: Randomized Clinical Trial Evaluation of Effectiveness, Clinical Parameters and Enamel Mineral Content. Am. J. Dent. 2019, 32, 124–132. [Google Scholar]
- Rodrigues, J.L.; Rocha, P.S.; Pardim, S.L.d.S.; Machado, A.C.V.; Faria-e-Silva, A.L.; Seraidarian, P.I. Association Between In-Office And At-Home Tooth Bleaching: A Single Blind Randomized Clinical Trial. Braz. Dent. J. 2018, 29, 133–139. [Google Scholar] [CrossRef]
- Knezović Zlatarić, D.; Žagar, M.; Illeš, D. A Clinical Study Assessing the Short-term Efficacy of Combined In-office/At-home Whitening Treatment. J. Esthet. Restor. Dent. 2019, 31, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Mailart, M.C.; Sakassegawa, P.A.; Santos, K.C.; Torres, C.R.G.; Palo, R.M.; Borges, A.B. One-year Follow-up Comparing At-home Bleaching Systems Outcomes and the Impact on Patient’s Satisfaction: Randomized Clinical Trial. J. Esthet. Restor. Dent. 2021, 33, 1175–1185. [Google Scholar] [CrossRef] [PubMed]
- Levrini, L.; Paracchini, L.; Bakaj, R.; Diaconu, A.; Cortese, S. Dental Bleaching during Orthodontic Treatment with Aligners. Int. J. Esthet. Dent. 2020, 15, 44–54. [Google Scholar] [PubMed]
- Féliz-Matos, L.; Abreu-Placeres, N.; Hernandez, L.M.; Ruiz-Matuk, C.; Grau-Grullón, P. Evaluation of In-Office Vital Tooth Whitening Combined with Different Concentrations of At-Home Peroxides: A Randomized Double-Blind Clinical Trial. Open Dent. J. 2019, 13, 377–382. [Google Scholar] [CrossRef]
- Pavani, C.C.; Vieira, L.R.; Schott, T.C.; Sundfeld, D.; Pini, N.; Bertoz, A.; Pacheco, R.R.; Sundfeld, R.H. Case Reports of Enamel Microabrasion Associated with At-Home Dental Bleaching After Orthodontic Bracket Removal. Oper. Dent. 2021, 46, 237b–245. [Google Scholar] [CrossRef] [PubMed]
- Gomes, M.N.; Dutra, H.; Morais, A.; Sgura, R.; Devito-Moraes, A.G. In-Office Bleaching During Orthodontic Treatment. J. Esthet. Restor. Dent. 2017, 29, 83–92. [Google Scholar] [CrossRef]
- Ahrari, F.; Akbari, M.; Mohammadipour, H.S.; Fallahrastegar, A.; Sekandari, S. The Efficacy and Complications of Several Bleaching Techniques in Patients after Fixed Orthodontic Therapy. A Randomized Clinical Trial. Swiss Dent. J. 2020, 130, 493–501. [Google Scholar]
- Cho, K.; Rajan, G.; Farrar, P.; Prentice, L.; Prusty, B.G. Dental Resin Composites: A Review on Materials to Product Realizations. Compos. Part B Eng. 2022, 230, 109495. [Google Scholar] [CrossRef]
- German, M.J. Developments in Resin-Based Composites. Br. Dent. J. 2022, 232, 638–643. [Google Scholar] [CrossRef]
- Yadav, R.D.; Raisingani, D.; Jindal, D.; Mathur, R. A Comparative Analysis of Different Finishing and Polishing Devices on Nanofilled, Microfilled, and Hybrid Composite: A Scanning Electron Microscopy and Profilometric Study. Int. J. Clin. Pediatr. Dent. 2016, 9, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Libonati, A.; Marzo, G.; Klinger, F.G.; Farini, D.; Gallusi, G.; Tecco, S.; Mummolo, S.; De Felici, M.; Campanella, V. Embryotoxicity Assays for Leached Components from Dental Restorative Materials. Reprod. Biol. Endocrinol. 2011, 9, 136. [Google Scholar] [CrossRef] [PubMed]
- Elhoshy, A.Z.; Abouelenein, K.; Elbaz, M.A. Effect of 15% Carbamide Peroxide Bleaching Gel on Color of Class V Resin Composite Restoration. Future Dent. J. 2018, 4, 239–243. [Google Scholar] [CrossRef]
- Mummolo, S.; Mancini, L.; Quinzi, V.; D’Aquino, R.; Marzo, G.; Marchetti, E. Rigenera® Autologous Micrografts in Oral Regeneration: Clinical, Histological, and Radiographical Evaluations. Appl. Sci. 2020, 10, 5084. [Google Scholar] [CrossRef]
- Meireles, S.S.; Santos, I.S.; Bona, A.D.; Demarco, F.F. A Double-Blind Randomized Clinical Trial of Two Carbamide Peroxide Tooth Bleaching Agents: 2-Year Follow-Up. J. Dent. 2010, 38, 956–963. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).