A Three-Year Prospective Study Comparing Stereolithography Printed Models to Classical Impression and Plaster Cast Models in Orthodontic Therapy: A 3D Objectification Approach
Abstract
:1. Introduction
- Fused-deposition modeling (FDM): This 3D printing method still has relatively low resolution and is primarily used as an auxiliary method. FDM 3D printers heat a thermoplastic filament to create each layer;
- Stereolithography (SLA) or digital light processing (DLP): These technologies use similar principles but differ in the wavelength of light used;
- PolyJet 3D printing: This method involves the layering of liquid polymers;
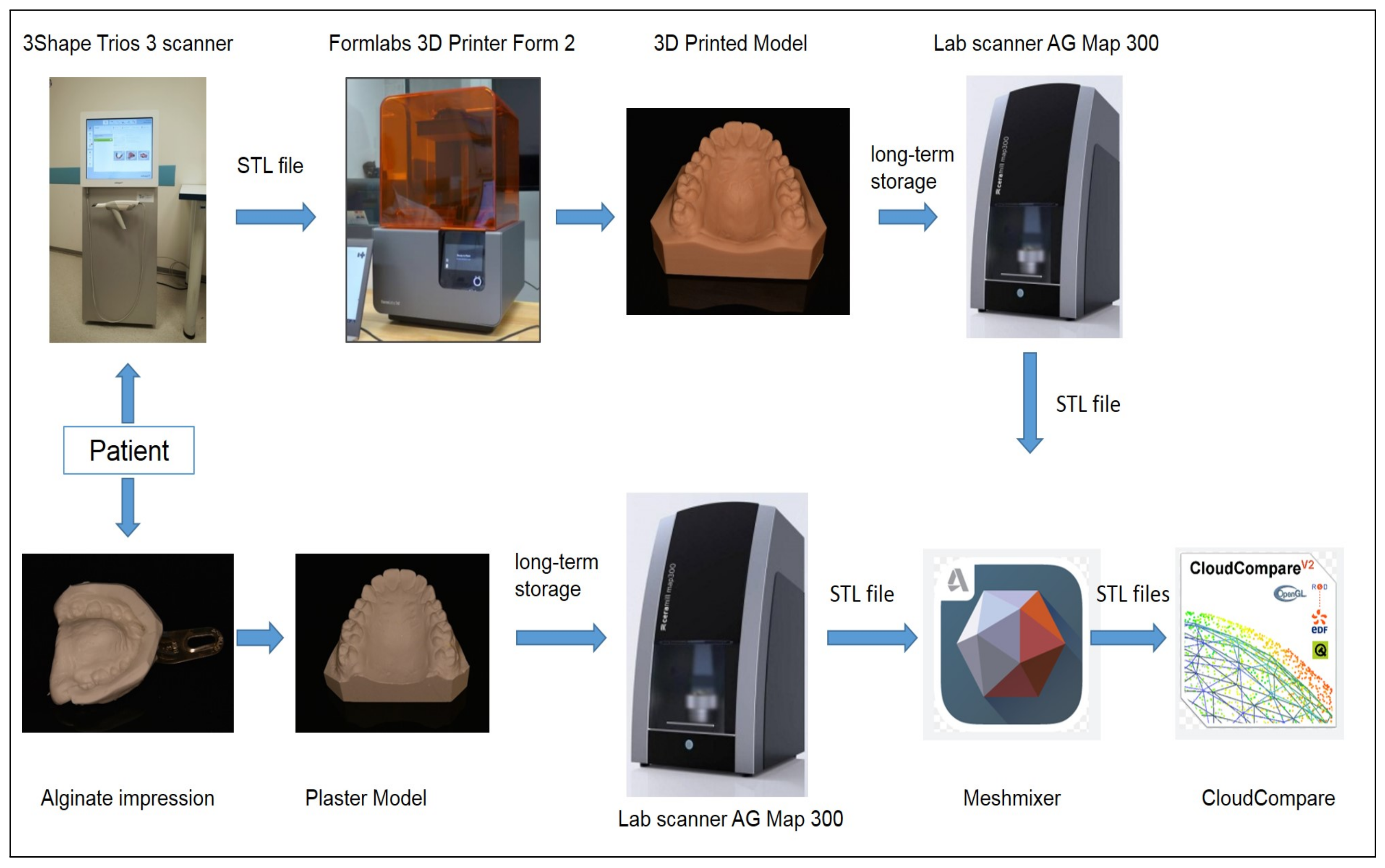
2. Materials and Methods
2.1. Subject
2.2. Analyzing Methods and Measuring Instruments
2.3. The Stereolithography Printer
2.4. Surface Profile and Structure Analysis
3. Results
3.1. Evaluation of Classical and 3D Model Precision
3.2. Surface Profile and Structure Characterization: An Analysis of Dental Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grunheid, T.; Patel, N.; De Felippe, N.; Wey, A.; Gaillard, P.; Larson, B.E. Accuracy, reproducibility, and time efficiency of dental measurements using different technologies. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 157–164. [Google Scholar] [CrossRef]
- Stevens, D.; Flores-Mir, C.; Nebbe, B.; Raboud, D.; Heo, G.; Major, P. Validity, reliability, and reproducibility of plaster vs digital study models: Comparison of peer assessment rating and Bolton analysis and their constituent measurements. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 794–803. [Google Scholar] [CrossRef] [PubMed]
- Hernandez-Alfaro, F.; Guijarro-Martinez, R. On a definition of the appropriate timing for surgical intervention in orthognathic surgery. Int. J. Oral Maxillofac. Surg. 2014, 43, 846–855. [Google Scholar] [CrossRef] [PubMed]
- Ahlholm, P.; Sipila, K.; Vallittu, P.; Jakonen, M.; Kotiranta, U. Digital Versus Conventional Impressions in Fixed Prosthodontics: A Review. J. Prosthodont. 2018, 27, 35–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kašparová, M.; Gráfová, L.; Dvořák, P.; Dostálová, T.; Procházka, A.; Eliášová, H.; Pruša, J.; Kakawand, S. Possibility of reconstruction of dental plaster cast from 3D digital study models. Biomed. Eng. Online 2013, 12, 49:1–49:11. [Google Scholar]
- Dostalova, T.; Prochazka, A.; Urbanova, P.; Eliasova, H. 3D Stereolithography Print (SLA) in Clinical Orthodontic and Dental Applications; Lasers in Dentistry XXVIII; Rechmann, P., Fried, F., Eds.; International Society for Optics and Photonics, SPIE: Bellingham, WA, USA, 2022; Volume 11942, p. 1194207. [Google Scholar]
- Khorsandi, D.; Fahimipour, A.; Abasian, P.; Saber, S.; Seyedi, M.; Ghanavati, S.; Ahmad, A.; Amoretti, A.; De Stephanis, A.; Taghavinezhaddilami, F.; et al. 3D and 4D printing in dentistry and maxillofacial surgery: Printing techniques, materials, and applications. Acta Biomater. 2021, 122, 26–49. [Google Scholar] [CrossRef]
- Eliášová, H.; Dostálová, T.; Jelínek, M.; Remsa, J.; Bradna, P.; Procházka, A.; Kloubcová, M. Surface Morphology of Three-Dimensionally Printed Replicas of Upper Dental Arches. Appl. Sci. 2020, 10, 5708. [Google Scholar] [CrossRef]
- Dostalova, T.; Kasparova, M.; Chleborad, K.; Jelínek, M.; Bradna, P.; Mendricky, R. Intraoral Scanner and Stereographic 3D Print in Orthodontics; Lasers in Dentistry XXV; Rechmann, P., Fried, F., Eds.; International Society for Optics and Photonics, SPIE: Bellingham, WA, USA, 2019; Volume 10857, p. 1085706. [Google Scholar]
- Dawood, A.; Marti, B.; Suaret-Jackson, V.; Darwood, A. 3D printing in dentistry. Br. Dent. J. 2015, 219, 521–529. [Google Scholar] [CrossRef]
- Dostálova, T.; Kašparová, M.; Kříž, P.; Halamová, S.; Jelínek, M.; Bradna, P.; Medřický, R. Intraoral scanner and stereographic 3D print in dentistry—Quality and accuracy of model—New laser application in clinical practice. Laser Phys. 2018, 28, 125602. [Google Scholar] [CrossRef]
- Reddy, M.; Shetty, S.; Shetty, R.; Vannala, V.; Shakeei, S.; Rajasekar, S. Focus on periodontal engineering by 3D printing technology—A systematic review. J. Oral Res. 2020, 9, 522–531. [Google Scholar] [CrossRef]
- Turkyilmaz, I.; Wilkins, N. 3D printing in dentistry—Exploring the new horizons. J. Dent. Sci. 2021, 16, 1037–1038. [Google Scholar] [CrossRef]
- Piedra-Cascón, W.; Methani, M.; Quesada-Olmo, N.; Jiménez-Martínez, M.; Revilla-León, M. Scanning Accuracy of Nondental Structured Light Extraoral Scanners Compared with That of a Dental-Specific Scanner. J. Prosthet. Dent. 2021, 126, 110–114. [Google Scholar] [CrossRef]
- Nulty, A. A Comparison of Full Arch Trueness and Precision of Nine Intra-Oral Digital Scanners and Four Lab Digital Scanners. Dentistry 2021, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Son, K.; Lee, W.; Lee, K. Effect of Different Software Programs on the Accuracy of Dental Scanner Using Three-Dimensional Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8449. [Google Scholar] [CrossRef] [PubMed]
- Czajkowska, M.; Walejewska, E.; Zadrozny, L.; Wieczorek, M.; Swieszkowski, W.; Wagner, L.; Mijiritsky, E.; Markowski, J. Comparison of Dental Stone Models and Their 3D Printed Acrylic Replicas for the Accuracy and Mechanical Properties. Materials 2020, 13, 4066. [Google Scholar] [CrossRef]
- Gholinia, F.; Dalili, Z.; Nahvi, A.; Sigaroudi, A. Reliability and validity of dental measurements made on digital and stone orthodontic models. J. Dentomaxillofac. Radiol. Pathol. Surg. 2012, 1, 26–33. [Google Scholar] [CrossRef] [Green Version]
- Yuzbasioglu, E.; Kurt, H.; Turunc, R.; Bilir, H. Comparison of digital and conventional impression techniques: Evaluation of patients’ perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health 2014, 14, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gráfová, L.; Kašparová, M.; Kakawand, S.; Procházka, A.; Dostálová, T. Study of Edge Detection Task in Dental Panoramic X-ray Images. Dentomaxillofac. Radiol. 2013, 42, 20120391:1–20120391:12. [Google Scholar] [CrossRef]
- Procházka, A.; Kašparová, M.; Yadollahi, M.; Vyšata, O.; Grajciarová, L. Multi-Camera Systems Use for Dental Arch Shape Measurement. Visual Comput. 2015, 31, 1501–1509. [Google Scholar] [CrossRef]
- Yadollahi, M.; Procházka, A.; Kašparová, M.; Vyšata, O. The Use of Combined Illumination in Segmentation of Orthodontic Bodies. Signal Image Video Process. 2015, 9, 243–250. [Google Scholar] [CrossRef]
- Kašparová, M.; Halamová, S.; Dostálová, T.; Procházka, A. Intra-Oral 3D Scanning for the Digital Evaluation of Dental Arch Parameters. Appl. Sci. 2018, 8, 1838. [Google Scholar] [CrossRef] [Green Version]
- Park, M.; Shin, S. Three-dimensional comparative study on the accuracy and reproducibility of dental casts fabricated by 3D printers. J. Prosthet. Dent. 2018, 119, 861.e1–861.e7. [Google Scholar] [CrossRef] [PubMed]
- Procházka, A.; Vyšata, O.; Mařík, V. Integrating the Role of Computational Intelligence and Digital Signal Processing in Education. IEEE Signal Process. Mag. 2021, 38, 154–162. [Google Scholar] [CrossRef]
- Kašparová, M.; Procházka, A.; Gráfová, L.; Yadollahi, M.; Vyšata, O.; Dostálová, T. Evaluation of Dental Morphometrics During the Orthodontic Treatment. Biomed. Eng. Online 2014, 14, 68:1–68:13. [Google Scholar] [CrossRef] [Green Version]
- Procházka, A.; Dostálová, T.; Kašparová, M.; Vyšata, O.; Charvátová, H.; Sanei, S.; Marík, V. Augmented Reality Implementations in Stomatology. Appl. Sci. 2019, 9, 2929. [Google Scholar] [CrossRef] [Green Version]
- Eliášová, H.; Dostálová, T.; Procházka, A.; Šedivá, E.; Horáček, M.; Urbanová, P.; Hlinakova, P. Comparison of 2D OPG Image versus Orthopantomogram from 3D CBCT from the Forensic Point of View. J. Leg. Med. 2021, 48, 101802. [Google Scholar] [CrossRef] [PubMed]
- Sanda, M.; Miyoshi, K.; Baba, K. Trueness and precision of digital implant impressions by intraoral scanners: A literature review. Int. J. Implant. Dent. 2021, 7, 2–25. [Google Scholar] [CrossRef]
- Ender, A.; Zimmermann, M.; Mehl, A. Accuracy of complete- and partial-arch impressions of actual intraoral scanning systems in vitro. Int. J. Comput. Dent. 2019, 22, 11–19. [Google Scholar]
- Ender, A.; Attin, T.; Mehl, A. In vivo precision of conventional and digital methods of obtaining complete-arch dental impressions. J. Prosthet. Dent. 2016, 115, 313–320. [Google Scholar] [CrossRef] [Green Version]
- Joda, T.; Matthisson, L.; Zitzmann, U. Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation. J. Clin. Med. 2020, 9, 1436. [Google Scholar] [CrossRef]
- Sabbah, A.; Romanos, G.; Delgado-Ruiz, R. Impact of Layer Thickness and Storage Time on the Properties of 3D-Printed Dental Dies. Materials 2021, 14, 509. [Google Scholar] [CrossRef] [PubMed]
- Tahayeri, A.; Morgan, M.; Fugolin, A.; Bompolaki, D.; Athirasala, A.; Pfeifer, C.; Ferracane, J.; Bertassoni, L. 3D printed versus conventionally cured provisional crown and bridge dental materials. Dent. Mater. 2018, 34, 192–200. [Google Scholar] [CrossRef] [PubMed]






| Surface Difference Comparison | ||||||||
|---|---|---|---|---|---|---|---|---|
| Individual | Upper Jaw | Bottom Jaw | ||||||
| Points | Median | Mean | Std | Points | Median | Mean | Std | |
| 05 | 239,340 | 0.0060 | 0.0128 | 0.1317 | 222,690 | 0.0168 | 0.0163 | 0.1282 |
| 08 | 181,522 | −0.0122 | −0.0121 | 0.2163 | 187,267 | −0.0041 | −0.0081 | 0.1684 |
| 09 | 234,314 | −0.0166 | −0.0209 | 0.1212 | 209,048 | 0.0443 | 0.0330 | 0.1433 |
| 12 | 197,424 | −0.0172 | −0.0261 | 0.2311 | 208,471 | 0.0114 | 0.0057 | 0.1748 |
| 15 | 228,273 | −0.0047 | −0.0292 | 0.2155 | 220,984 | −0.0353 | −0.0845 | 0.3617 |
| 16 | 236,978 | −0.0424 | −0.0317 | 0.2742 | 232,064 | 0.0128 | 0.0051 | 0.1504 |
| 17 | 278,309 | −0.0316 | −0.0470 | 0.3280 | 256,598 | −0.0213 | −0.0315 | 0.2336 |
| 18 | 206,480 | −0.0198 | −0.0228 | 0.1032 | 195,661 | 0.0227 | 0.0345 | 0.3595 |
| 19 | 275,752 | −0.0349 | −0.0280 | 0.2214 | 245,881 | 0.0008 | −0.0009 | 0.1412 |
| 20 | 253,589 | −0.0162 | −0.0189 | 0.1149 | 230,604 | −0.0220 | −0.0092 | 0.1402 |
| 21 | 254,839 | −0.0280 | −0.0264 | 0.1180 | 209,657 | −0.0028 | −0.0263 | 0.1248 |
| 22 | 269,743 | −0.0142 | −0.0190 | 0.1340 | 229,829 | −0.0060 | −0.0100 | 0.2710 |
| 23 | 280,864 | −0.0404 | −0.0174 | 0.2135 | 268,421 | −0.0018 | −0.0070 | 0.1566 |
| 25 | 227,458 | −0.0066 | 0.0032 | 0.0969 | 199,842 | −0.0018 | −0.0028 | 0.1550 |
| 28 | 242,926 | −0.0180 | −0.0248 | 0.1581 | 256,832 | −0.0018 | −0.0097 | 0.2219 |
| 29 | 235,302 | −0.0091 | −0.0046 | 0.2089 | 207,356 | 0.0036 | 0.0014 | 0.1285 |
| 30 | 198,720 | −0.0035 | −0.0080 | 0.1305 | 172,267 | −0.0059 | −0.0195 | 0.1338 |
| 32 | 253,200 | −0.0338 | −0.0466 | 0.1790 | 235,288 | −0.0309 | −0.0286 | 0.1612 |
| 34 | 243,778 | −0.0129 | 0.0978 | 0.5841 | 230,922 | −0.0163 | −0.0097 | 0.1345 |
| 36 | 237,367 | −0.0017 | −0.0095 | 0.1283 | 224,377 | −0.0131 | −0.0228 | 0.1982 |
| 37 | 237,520 | −0.0295 | −0.0268 | 0.0951 | 199,934 | −0.0031 | −0.0121 | 0.1382 |
| 40 | 268,848 | −0.0052 | −0.0083 | 0.1454 | 245,285 | 0.0216 | 0.0247 | 0.0954 |
| Mean | 240,116 | −0.0178 | −0.0143 | 0.1886 | 222,240 | −0.0013 | 0.0152 | 0.1695 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nocar, A.; Procházka, A.; Kloubcová, M.; Hyšpler, P.; Schatz, M.; Dostálová, T. A Three-Year Prospective Study Comparing Stereolithography Printed Models to Classical Impression and Plaster Cast Models in Orthodontic Therapy: A 3D Objectification Approach. Appl. Sci. 2023, 13, 7542. https://doi.org/10.3390/app13137542
Nocar A, Procházka A, Kloubcová M, Hyšpler P, Schatz M, Dostálová T. A Three-Year Prospective Study Comparing Stereolithography Printed Models to Classical Impression and Plaster Cast Models in Orthodontic Therapy: A 3D Objectification Approach. Applied Sciences. 2023; 13(13):7542. https://doi.org/10.3390/app13137542
Chicago/Turabian StyleNocar, Adam, Aleš Procházka, Magdaléna Kloubcová, Pavel Hyšpler, Martin Schatz, and Tatjana Dostálová. 2023. "A Three-Year Prospective Study Comparing Stereolithography Printed Models to Classical Impression and Plaster Cast Models in Orthodontic Therapy: A 3D Objectification Approach" Applied Sciences 13, no. 13: 7542. https://doi.org/10.3390/app13137542






