Abstract
In recent decades, extensive attention has been paid to the study and development of robotic devices specifically designed for hand rehabilitation. Accordingly, a many concepts concerning rigid, soft, and hybrid types have emerged in the literature, with significant ongoing activity being directed towards the development of new solutions. In this context, the paper focuses on the technical features of devices conceived for the robotic rehabilitation of the hand with reference to the three kinds of exoskeleton architecture and the clinical requirements demanded by the target impairment of the end-user. The work proposes a roadmap (i) for both the design and selection of exoskeletons for hand rehabilitation, (ii) to discriminate among the peculiarities of soft, rigid, and hybrid devices, and (iii) with an impairment-oriented rationale. The clinical requirements expected for an exoskeleton are identified by applying a PICO-inspired approach focused on the impairment analysis; the technical features are extracted from a proposed design process for exoskeletons combined with a narrative literature review. A cross-analysis between device families and features is presented to provide a supporting tool for both the design and selection of exoskeletons according to an impairment-oriented rationale.
1. Introduction
Robot-based hand therapy, training, or assistance is increasingly being used to treat or support various impairments related to pathologies, accidents, or advancing age. Meanwhile, through pilot studies, numerous authors have shown the effectiveness of this approach for improving neuromotor recovery [1,2,3,4].
From a technical design perspective, the literature presents several works on robotic exoskeletons for the human hand for medical purposes, namely rehabilitation and assistive applications, and not for performance augmentation or haptic and sensing [5]. Literature reviews especially tend to focus on specific kinds of hand exoskeleton or applications, e.g., active robotic exoskeletons for hand rehabilitation, since the functional domain heavily influences the design constraints of these devices [6]. In previous years, particular attention has been paid to soft exoskeletons [7,8,9,10].
Most of these review papers investigate, through the literature, the state-of-the-art hand exoskeletons and classify these devices according to a set of parameters, mainly related to technical characteristics, such as performance specifications or design architecture. For instance, typical evaluated aspects are the presence and number of actuators or actuated degrees of freedom (DOFs), the number of actuated fingers, the kinds of allowed movements, the actuation technology, or the presence of sensors.
In a review by du Plessis et al. [5] of 2021, these characteristics are further classified into general requirements, common to all devices of the analyzed category, and specific requirements, i.e., those characteristics related to a specific application. This work depicts, in particular, an interesting overview of active hand exoskeletons developed for the specific purpose of rehabilitation and assistance in the last decade. The analysis is performed by describing the requirements captured by the investigation of hand exoskeletons currently mentioned in the literature. The limited time frame of the analysis allows the devices and their technologies to be compared, providing a general overview of these specifications with an observational approach.
The same distinction between general and application-specific requirements is presented in a paper published in 2019 by Sarac et al. [11]. The focus of this work is slightly different, since the authors aim to identify guidelines and best practices for the design of generic exoskeletons, i.e., purpose-independent devices. Coherent with this final goal, the main design requirements are extracted by the analysis of exoskeletons in the literature, and then a selection of design solutions to fulfill those requirements is proposed.
The same deductive approach was adopted by Troncossi et al. [6] in a paper published in 2016. In their work, the authors present an original classification strategy based on three alternative parameters, i.e., the number of actuated DOFs, the number of mechanical connections between the subject and the device, and the mechanism architecture (namely external, internal, or lateral). These parameters are recognized by the authors as being particularly relevant for the mechanism synthesis, and therefore, they are drivers for the definition of the most proper technical solutions. As for the work by Sarac et al., the paper by Troncossi et al. aims to provide the designer with indications for the design phase but focuses, in this case, on the synthesis of the mechanism itself.
In 2020, Boser et al. [12] instead published a paper focused on the definition of the design requirements of hand exoskeletons for assistive purposes based on end-user needs and expectations. The study investigated both qualitative and quantitative data through surveys to clinicians and patients on one side and through experimental measurements on the other. Among the paper’s findings, the authors conclude that some preliminary criteria do exist, but the differences and peculiarities of patients demand tailored requirements, translating into custom solutions.
The clinical perspective offers a different approach toward these devices. In most cases, in fact, the clinician (or the end-user themselves in fewer cases) needs to select the most proper exoskeleton for a patient within a set of suitable candidates. Nevertheless, the choice is driven by the clinical picture of the end-user and their functional and structural impairments especially. Accordingly, the requirements assessed by the clinician may not necessarily overlap with the technical features typically adopted to describe the performance of an exoskeleton in a design context. For instance, the clinician might look for solutions to counteract the strength reduction in grasping, whereas the designer will describe the force generated by the motors.
Given these core differences in the approach to exoskeletons, a mismatch between technical requirements and clinical needs inevitably occurs. In this context, the mapping of technical features and clinical specifications is necessary to enable a proper understanding of these two worlds, although according to the authors’ knowledge, no investigations in this sense seem to be present in current literature.
Research in the healthcare field is currently grounded on the principles and guidelines advocated by the Evidence-Based Medicine (EBM) approach with the aim of improving the quality of medical studies and, consequently, the reliability and confidence of clinical decision-making. According to EBM, formulating a proper and well-framed research question represents the initial and crucial step to conducting valid and valuable research. In this view, EBM recommends that a research question is formulated by using a specialized framework known as PICO [13]. PICO is an acronym that stands for Population/Problem, Intervention, Comparison, and Outcome.
In this work, we decided to adopt the PICO framework to organize the information retrieved from the analyzed studies in view of technical–clinical feature mapping. In particular, we primarily focused our attention on the problem intended to be the specific structural/functional impairment belonging to a given health condition.
Within this context, the current paper aims to provide a roadmap (i) for both design and selection of exoskeletons for hand rehabilitation, (ii) to discriminate among the peculiarities of soft, rigid, and hybrid devices, and (iii) with an impairment-oriented rationale.
To reach this goal, the mapping of technical features and clinical specifications expected for the exoskeleton is outlined. For this analysis, a PICO-inspired approach is applied to identify the clinical requirements from the impairment analysis; this approach is also integrated into the proposed exoskeleton design process, which enables the identification of the technical requirements of a device.
The development process of the work began with an in-depth analysis of the state-of-the-art technology related to rigid, soft, and hybrid devices. An initial selection of articles was based on a search of the Scopus database, proceeding with subsequent searches for each device family using specific keywords. Based on the analysis of the papers found in this initial phase and the step-by-step definition of the roadmap with impairment-oriented rationale for device design and selection, further searches were conducted, aiming at an in-depth analysis dealing with specific aspects, for instance, control, wearability, or applications in specific clinical scenarios. This process resulted in an analysis of more than 100 papers.
In this context, a clarification of the definitions of rigid, hybrid, and soft exoskeletons that we adopted for device classification is necessary. There is no well-established classification among rigid, soft, and hybrid exoskeletons. Various authors have proposed and explained their own classifications in review papers. De la Tejera et al. [14] distinguished between two classes of exoskeleton based on their structures: rigid when they are made with rigid structural elements (metal or plastic) and soft when they are made from textiles. Du Plessis et al. [5] stated that “There are mainly two types of hand exoskeletons developed over the years, which are classified as rigid and soft exoskeletons or a combination of the two”, but they fundamentally identified two classes: rigid, in which the forces or torques are transmitted to the required joints through a mechanical structure, and soft, with flexible materials or elastic structures to transmit the forces to the joints of the fingers. Instead, Güçlü and Cora [15] distinguished three classes: rigid (linkage-based), cable-driven, and soft exoskeletons. Exoskeletons in which the movement produced by the actuator is transferred to the joints with hard and inelastic materials are rigid. If the movement produced by the actuators is transferred to the joints with the help of cables and pulleys, the exoskeletons are hybrid; this also occurs for tendon-driven exoskeletons. They defined soft exoskeletons as devices that are made from materials compatible with the human anatomy. Chu and Patterson [9] reviewed soft exoskeletons and defined them as robots made from easily deformable materials such as fluids, gels, and soft polymers that have better biomimetic properties due to their greater compliance and versatility while conforming to the contours of the human body. Specific definitions of hybrid exoskeletons can be found in articles presenting specific solutions for hybrid devices. For Lin et al. [16], hybrid soft–rigid exoskeletons use deformable materials in combination with a rigid frame. For Haghshenas et al. [17], an exoskeleton that integrates soft–rigid hybrid actuators consisting of flexible elements and rigid or semi-rigid elements is also considered hybrid.
Our definition of the different typologies does not fully coincide with any of those existing in the literature but integrates the definitions proposed by different authors. We agree with the definition of “rigid” in [15] as linkage-based exoskeletons, i.e., with rigid transmission mechanisms. For the “soft” class, we agree with the definition of Chu and Patterson [9], the exoskeletons formed by easily deformable materials, but with the addition of textile materials to the list of specified materials. The definition of “hybrid”, in our view, merges the definitions proposed by [15,17]. We classify hybrid cable or tendon-drive exoskeletons or exoskeletons with soft–rigid hybrid actuators.
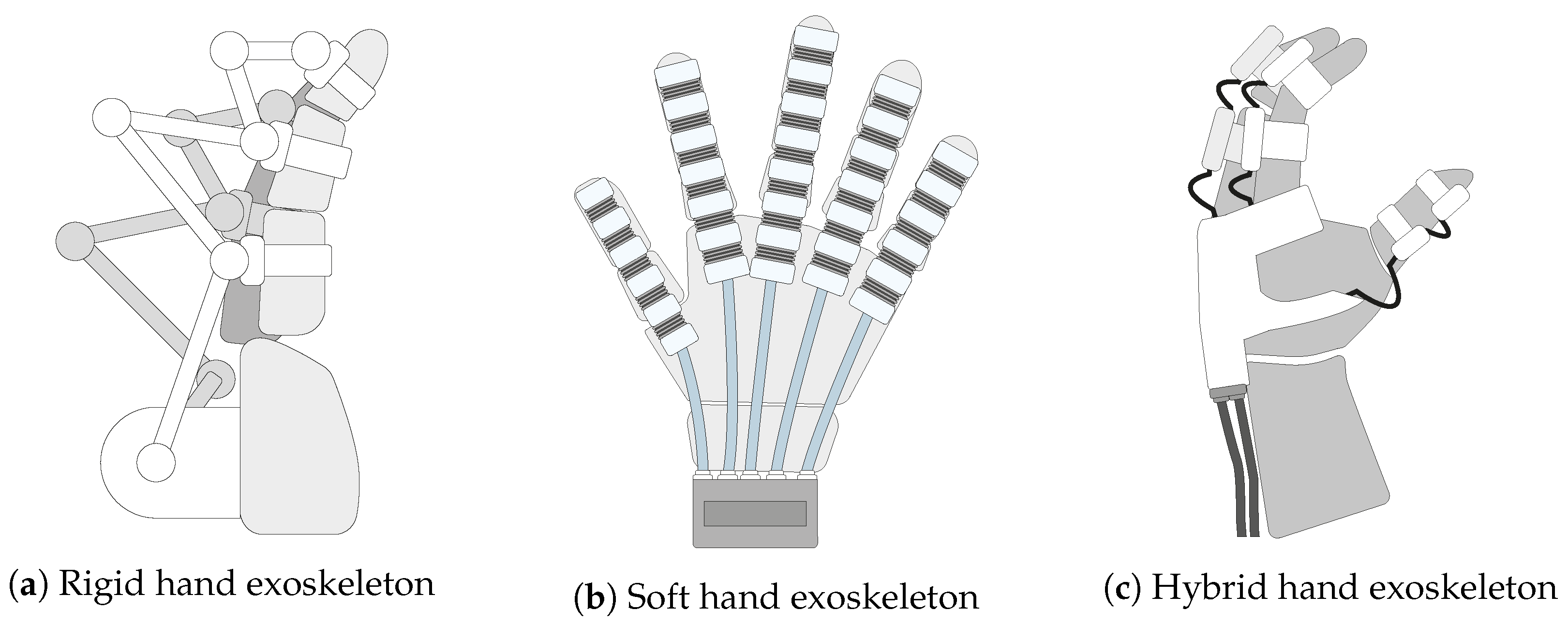
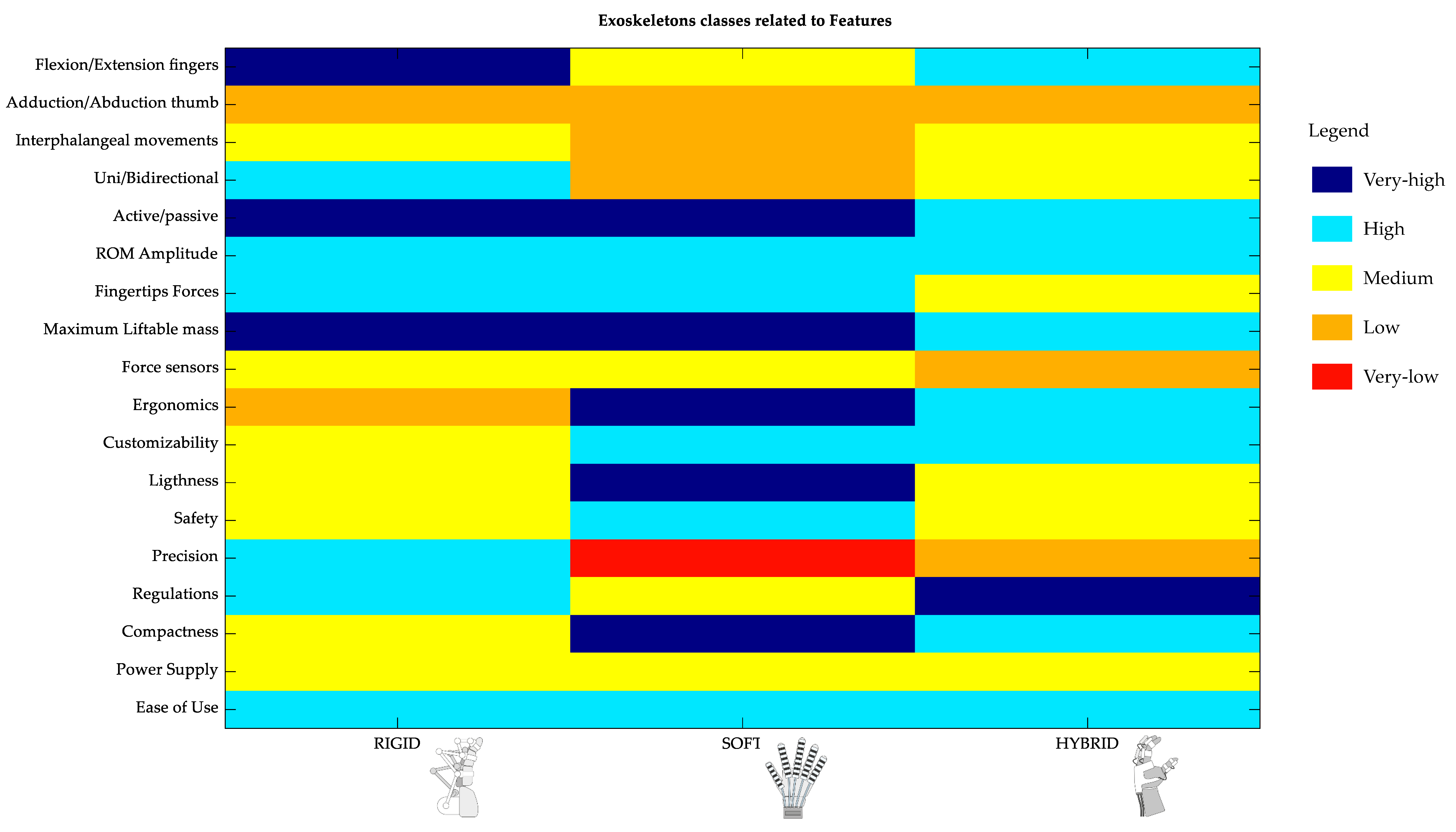
After the investigation of the main technical features unique to each exoskeleton family, namely rigid, soft, and hybrid architectures (Figure 1), a cross-analysis between device families and features is presented to provide a supporting tool for both the design and selection of exoskeletons, according to an impairment-oriented rationale.
Figure 1.
Schematic representation of the three classes of robotic hand rehabilitation exoskeletons: (a) rigid, (b) soft, and (c) hybrid.
The main technical features were divided into two main categories: functional features and interactive experience features. The functional features are related to the main motor functions of the hand, and among these, we identified the following: movements performed by the exoskeleton, the ROM allowing for the different movements, and forces. The interactive experience features concern the performance of the interaction of the user with the device, and among these, we include the following: wearability, control mode/possibility, and portability.
The rest of the paper is organized as follows: Section 2 describes the PICO model and the proposed impairment-based approach for the design and selection of a robotic exoskeleton for hand rehabilitation. A detailed description of the impairment-based design process is presented in Section 3. Section 4, Section 5 and Section 6 provide a detailed overview of the state-of-the-art technology for the three classes of robotic hand exoskeletons: rigid, soft, and hybrid. The analysis focuses primarily on the functional features and interactive experience features discussed in Section 3 to determine how the different device classes relate to these features. It should be noted that the analysis of the different devices presented in the literature shows great heterogeneity in terms of the characteristics, even among devices of the same class. The framework that we try to establish aims to highlight both the opportunities offered by each technology and the main trends that characterize each class for the different features. A summary of this analysis is discussed in Section 7, and the results are divided into two different forms: those that may be useful for engineers designing exoskeletons on the one hand and medical personnel who need to select an exoskeleton to treat a specific impairment on the other. Section 8 provides concluding remarks on the proposed approach. A list of the abbreviations used in the manuscript is also reported at the end of the paper.
2. PICO-Inspired Impairment Analysis for Hand Exoskeletons
The PICO model represents a method for formulating search questions and characterizing meta-analyses or clinical studies [18].
Several variants of the method have been proposed over the years, all slightly modifying the original version, which is grounded on four elements that designate the potential components of a clinical question: population/problem, intervention, comparison, and outcome.
The first element (P) describes the main target of the study, identifying the characteristics of the population or the problem. In the current study, the investigated problem is the kind of impairment of the patient, as the hand exoskeleton end-user.
The second component (I) defines the intervention (e.g., physical therapy, pharmacological treatment) under consideration for the specific population, whereas the third element (C) focuses on the comparison between the proposed intervention and possible alternatives (e.g., from placebo to surgery). Both of these aspects can offer interesting insights for the researcher: the analysis of the intervention can, for instance, highlight additional unexpected but relevant requirements for the design of new devices [19]. The comparison with competitors can instead provide precious hints for the development of a device, for example in the demonstration of equivalence, which represents a mandatory step of the clinical evaluation of a medical device for marketing in European countries [20].
Finally, the fourth element (O) of the PICO model defines the outcome considered relevant to assess the effectiveness of the intervention. These outcomes could be of various natures, from clinical assessments with instrumented measurement tools like dedicated sensors, to clinical scales, as well as economic factors (e.g., the number of accesses to the hospital or to medical examinations) or humanistic end-points, such as quality of life or patient satisfaction with the performed intervention. In our analysis, which focuses on device design and selection, outcomes play a very important role. In particular, outcomes that involve the measurement of specific hand functions can drive the decision to include certain sensors and/or tracking systems in the device during the design phase. For example, outcome measures that involve the use of goniometers could lead to sensors being integrated into the device for angular measurement. A correlation can also be found between outcomes and the main features of the exoskeleton. The strength outcome, which can be measured either with ergometers or with clinical scales, such as the Medical Research Council (MRC) scale, is indeed related to the functional feature of force. This leads to the following logic: the outcomes used to assess the effectiveness of a treatment are related to the features, and the more or less pronounced predisposition of an exoskeleton with respect to the features makes it more or less suitable for a given impairment.
Table 1 collects the P and O elements of the PICO model for the current investigation, i.e., the possible impairments described in the literature for the end-user of a hand exoskeleton and the referring outcomes. Since the final aim of this analysis step is to enable the identification of the clinical requirements for mapping with the technical features, the I and C components of PICO are not reported in this first stage.

Table 1.
The P (problem) and O (outcome) elements of the PICO model for the current study: the first two columns present the lists of the identified impairments and typologies, respectively. The third column describes the measures typically used to assess the outcomes.
Table 2 presents a first attempt at mapping between impairments and pathologies. Only the most common diseases for this context was evaluated in this phase with the main aim of providing an overview of the complex relation between diseases and derived impairments for the inexperienced observer. With this purpose, cancer was also included, although the great potential variability of this disease (e.g., in type and location) prevents a generally valid mapping with impairments.

Table 2.
Schematic overview of the relation between the P-problem of the PICO model (as identified impairments and typologies) and the most common pathologies requiring the use of hand exoskeletons. In the table, CNS and PNS denote the central and peripheral nervous systems, respectively; brackets indicate possible but non necessarily present match between impairment and pathology.
3. Robotic Hand Rehabilitative Exoskeleton Design Approach
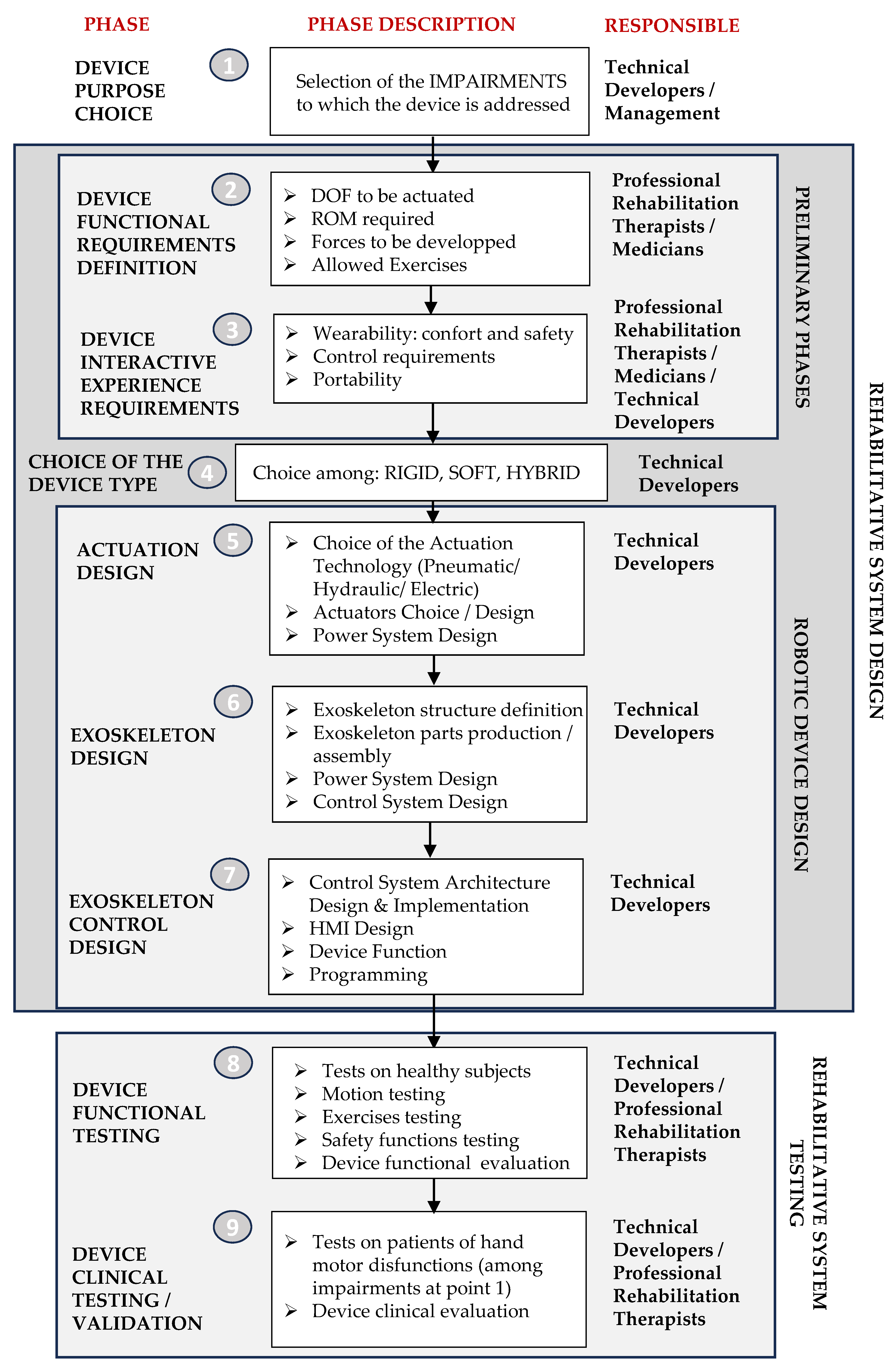
An impairment-oriented design process of a robotic exoskeleton for hand rehabilitation could be schematically described by the flowchart presented in Figure 2.

Figure 2.
General design flow-chart for a robotic exoskeleton device for hand rehabilitation with the indication of the professional figures responsible for each phase and with the identification of the macro-phases.
For each phase, the diagram includes the name of the phase, a description, and the people responsible for that phase. The starting point of the process (Phase 1) is the selection of the purpose, that is, the choice of impairments to which the device is devoted. The approach we propose for the design and, as we will see below, also for the selection of an exoskeletal rehabilitation device (based on the technology of PICO) is therefore based on impairments. The choice in Phase 1 is a strategic decision made by management with the support of technical developers, who can provide feedback on the real possibility of implementing the project. A schematic summary of the key impairments shown in Table 1 represents essential information for Phase 1 of the design process. Impairments are, of course, related to pathologies or other causes (see Table 2), but focusing the project on impairments rather than pathologies allows for greater generality, as the same impairment may be associated with different pathologies or external causes. In accordance with the structure of the PICO model, Table 1 also shows the methods used to measure the outcomes, which are usually adopted for each impairment. Knowledge of the tests/measures performed in the clinical validation phase of the device is also essential in the design phase, as targeted decisions are made to integrate appropriate sensors where possible.
The preparatory activities of the system design are dedicated to the definition of the design requirements, which are divided into functional requirements and interactive experience requirements. Functional requirements (defined in Phase 2) include the movements to be performed, i.e., the number of DOFs of the device, the range of motion (ROM) required for each movement, the forces to be developed, and the exercises allowed. Professional therapists or physicians who are experts in rehabilitation provide this information. The requirements for the interactive experience of the device (defined in Phase 3) represent the characteristics that the device must have in order to make the interaction with the individual as good as possible. They therefore concern the wearability, which determines the comfort and ease of use of the device, but also the safety during use, the control needs, and the portability in terms of the ability to use the device outside the hospital for rehabilitation at home. As far as functional requirements are concerned, physiotherapists and physicians are involved in this phase, but so are technical developers, as they help to define the boundaries within which the requirements are feasible.
By analyzing the design features, such as the actuated movement, range of motion, force, wearability, control, and portability, from different points of view, a fundamental decision must be made about the type of device to be developed, i.e., whether a rigid, soft, or hybrid (soft/rigid) exoskeleton is chosen (Phase 4). Additional aspects could be included in the analysis as well, like the concepts of transparency or reversibility of the device, but these characteristics and their importance for the overall design process of the exoskeleton are strongly dependent on the kind of architecture under consideration. Some comments about these aspects are therefore presented in the following sections with special reference to the specific exoskeleton type.
This decision will depend on the functional requirements of the device, as the three exoskeleton families may meet these requirements in different ways. A clearer and more complete picture of how the three classes of exoskeletons perform according to the requirements is extremely useful for this very delicate phase of the project. The analysis presented in the following sections aims precisely to extrapolate a functional framework for this choice. Numerous works in the literature related to each of the three families of exoskeletons have conducted analyses in detail from the point of view of their ability to meet the requirements for functionality and interactive experience so that a final picture presented in the discussion can be extrapolated. The analysis of the different devices presented in the literature shows great heterogeneity in terms of characteristics, even between devices of the same class. The framework we try to establish aims to highlight both the possibilities that each technology allows and the main trends that characterize each class for the different features.
The following phases of system design (Phases 5, 6, and 7) are the familiar phases of design for most mechatronic systems, and they are here declined with respect to hand exoskeletons. In Phase 5, after the choice of device type, a more specific decision must be made about the actuators to be used, since each class of drive technologies has subclasses of actuators. In the case of exoskeletons, new types of actuators are sometimes developed that are better suited for these types of devices and their close interactions with humans due to their specific characteristics. In Phase 6, the functional design of the device is conducted with the identification of its structure and its main structural components, and it is followed by the execution project. Once the structural and mechanical part of the device has been created, in Phase 7, the control and the HMI subsystems are designed and created, and programming is performed. Depending on the type of exoskeleton (rigid, soft, or hybrid), these three phases may be distinct, partially overlapping, or in some cases, indistinguishable. In rigid exoskeletons, as in most mechatronic systems, they are clearly distinguishable. In soft exoskeletons, on the other hand, the distinction between the actuator system and device is not so clearly defined; there are often cases where the actuators are structural parts of the exoskeleton, especially when they are pneumatic. In these cases, a clear distinction between these phases is not possible, especially for phases 5 and 6. This is also the case for some hybrid devices.
Once the device design is complete and a prototype has been built, the testing phases are initiated, which include both experimental (Phase 8) and clinical (Phase 9) validation. Phase 8 involves testing the device in collaboration with healthy volunteers to verify that the exoskeleton adequately meets functional and interactive experience requirements. Clinical validation, on the other hand, involves testing on subjects suffering from the impairments selected in Phase 1 and those to which the device is targeted.
In the following sections, some eminent examples of rigid, soft, and hybrid exoskeletons available in the literature are revised based on the criteria introduced in Phases 2 and 3, i.e., functional features and interactive experience features. The analysis highlights the main characteristics of each type of exoskeleton, their strengths, and their limits.
4. Rigid Robotic Exoskeletons for Hand Rehabilitation
Rigid robotic hand exoskeletons were the first solutions developed in the framework of robotic devices for rehabilitation and assistive applications from a chronological point of view due to their ability to transmit high forces with high precision through rigid mechanical transmission systems [21]. Rigid transmission mechanisms, i.e., systems composed of rigid links connected by joints are the earliest and simplest methods of transmitting actuator motions to the required human joints. The exoskeleton mechanisms were designed to establish a direct and rigid connection between the actuator motion space and the corresponding human joint motion space. In fully actuated systems, direct and inverse kinematic relationships can be established and, as a result, any measurements, such as encoder signals, current, or torque obtained from the actuator can be used to evaluate, with suitable accuracy, the corresponding state of the fingers. This inherent correspondence between the actuator and the hand joints allows for intuitive and easy hand control and no further tracking systems are needed in most cases.
In this context, two main types of actuation can be distinguished: direct drive and geared systems. Direct drive refers to systems where the actuators are directly connected to the structure [22,23,24,25,26,27,28,29,30,31,32], while geared systems use a gear train to connect the actuator to the structure [33,34,35,36,37]. In fewer applications, the two approaches are merged [38].
The general principle for wearable robots and specifically for rigid hand exoskeletons is to position and connect the actuators in the proximal part of the actuated limb or finger to limit the inertia and avoid user fatigue. Usually, in hand exoskeletons, the motors are positioned on the back side of the hand to ensure portability, minimize the device’s complexity, and reduce transmission losses during joint movements. However, this solution does increase the overall weight on the user’s hand due to the actuator’s mass and size. Rigid hand exoskeletons weigh, on average, 500 g and have a relatively large volume compared to the human hand size [39]. Keeping the device portable while employing an actuator for each hand DOF is nearly impossible. To limit the device weight and complexity, most rigid exoskeletons for the hand are characterized by few actuators, and joint motions are coupled by a mechanical transmission system [40]. Various types of mechanical transmission and coupling systems have been designed and implemented [5]. These structures can actuate multiple DOFs simultaneously, in a controlled manner, using a single actuator. Based on this concept, different transmission systems can be identified: four-bar linkage mechanisms [23,31,41,42,43,44], remote center of rotation [22,28,45], serial links mechanisms (suitable if the device needs to fit various users) [24,27,34,36], and matched-axis mechanical structures [46,47,48]. Each of these proposed solutions allows the actuation of the hand DOFs while maintaining the device’s portability and functionality. However, notwithstanding design solutions, these devices are often bulky and heavy, and most of them do not adequately account for a misalignment between the robot’s and the user’s joints [49]. For example, in [32] a revised version of the four-bar linkage mechanisms is presented. When the exoskeleton is not worn on the finger, it has three DOFs and an actuator; therefore, it is underactuated, while when it is worn, the finger biomechanical structure closes the mechanism and reduces the number of DOFs to one. In this way, the remote center of motion for the metacarpophalangeal joint is no longer necessary, leading to a significant simplification of the mechanical structure.
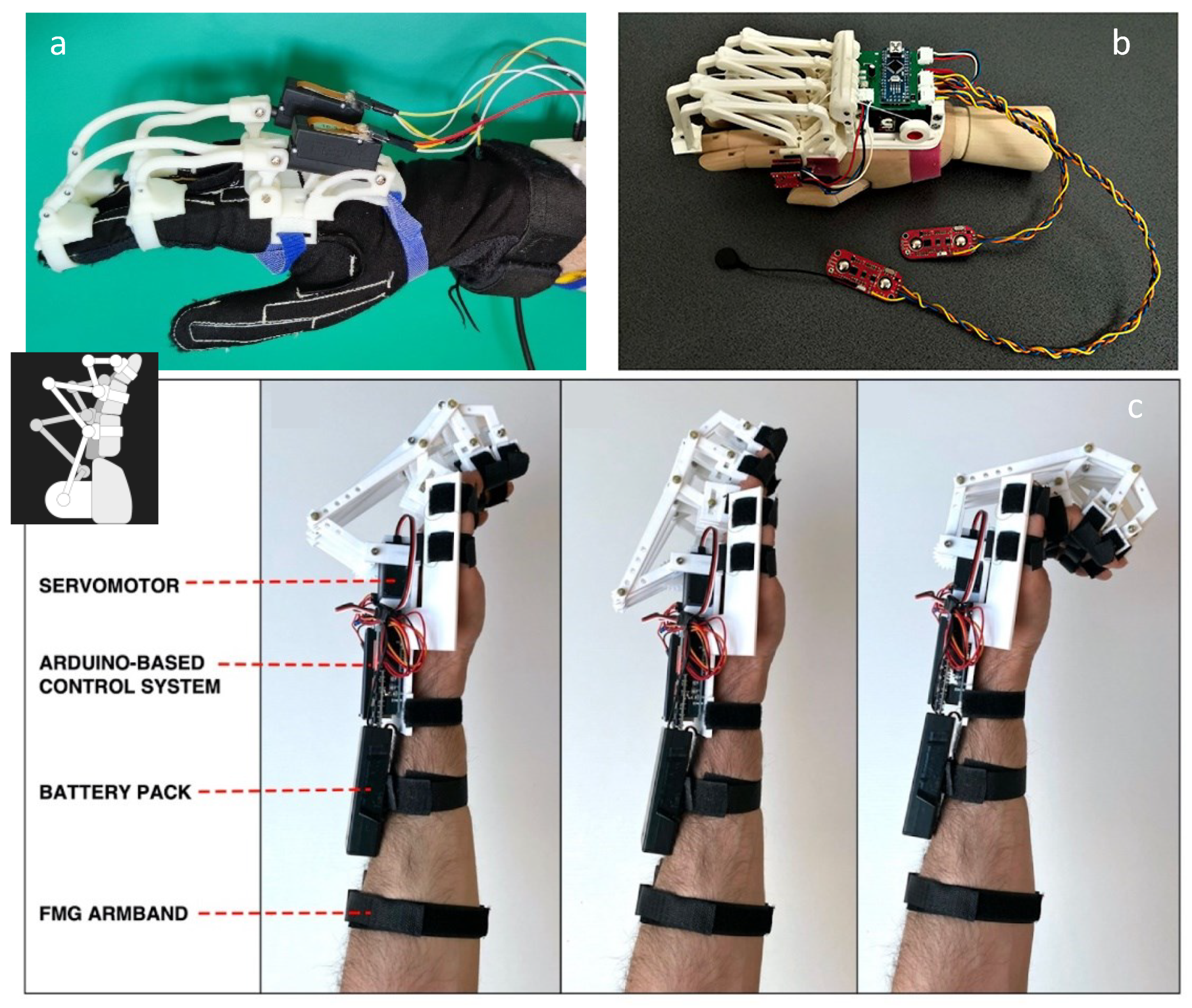
Some examples of rigid hand exoskeletons are shown in Figure 3. In the following, we present a more thorough analysis of rigid hand exoskeletons used for rehabilitation in terms of actuation and functional features.
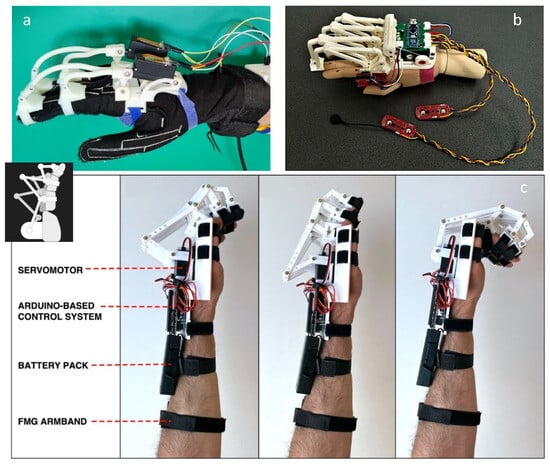
Figure 3.
Examples of rigid hand exoskeletons. (a) Modular exoskeleton for finger flexion/extension movement support, actuated by linear actuators [32]. (b) Hand exoskeleton for assistive and rehabilitative purposes developed by Secciani et al. [44]. (c) Rigid hand exoskeleton proposed by Esposito et al. [37].
4.1. Actuation System
Rigid hand exoskeleton devices mainly rely on electric motors for actuating human hand joints. Several types of actuators can be found in the literature, i.e., DC motors, linear actuators, servo motors, and brushless DC motors. DC motors are the most widely used due to their ease of use, backdrivability, and low torques at high speeds. Therefore, these types of motors are accompanied by a gearbox to increase the torque by reducing the motor speed [24,28,34,35,36,38,46,47,50]. Linear actuators are another type of system employed in rigid hand exoskeleton actuation units [22,23,25,29,32,40,51,52]. This kind of technology consists of DC motors connected to a lead screw assembly which allows the rotational motion to be converted into linear motion. Linear actuators are typically used in combination with the four-bar linkage mechanisms, enabling the structure to realize both flexion and extension motions of the actuated joint. Other works present rehabilitative hand devices that employ brushless DC motors. These motors offer advantages with respect to standard DC motors in terms of size, noise, and efficiency [53,54].
In other applications, servo motors are used to actuate hand exoskeletons [37,41,42,47]. These types of motors are limited geared DC motors that are controlled via pulse width modulation signals. They are very popular due to their easy control, and compared to DC motors, they do not suffer from the backdrivability problem.
Overall, selecting a suitable motor for the exoskeleton actuation unit always involves a trade-off among different criteria and depends on specific requirements in terms of the force, range of motion, power consumption, and weight characteristics that the device should satisfy.
4.2. Functional Features
- Actuated movements. Most of the rigid hand exoskeleton devices focus on replicating human finger flexion/extension movements by neglecting the abduction/adduction motions. Typically, each finger is actuated using at least one motor and presents the same mechanical structure, except for the thumb. The thumb presents a more complex and particular kinematic structure compared to the other fingers [55]. The literature review shows that the thumb exoskeletons vary depending on the specific design requirements and there are no rigid hand exoskeletons capable of performing the three movements of the thumb, i.e., flexion/extension, abduction/adduction, and opposition. In some applications, the thumb is designed to perform flexion/extension and abduction/adduction motions by using two actuators [53]. In other cases, the thumb exoskeleton is able to perform flexion/extension, while abduction/adduction motions are performed passively or not included at all [22,27,29,32,33,34,35,36,42,45,46,52]. There are also examples where the thumb is entirely passive or not considered in the rigid hand exoskeleton design [37,41,47].In order to let the user perform natural and coordinated hand movements, the concept of synergies introduced by Santello et al. [56] is exploited in some solutions in the design phase of the exoskeleton [32,48].
- Range of motion. The combination of ROM and stretching exercises is essential for patients during the rehabilitation process. ROM maintenance plays an important role in preventing complications such as finger contractures [57,58]. Therefore, achieving a suitable ROM is a key feature when designing hand exoskeleton devices. Ideally, such rehabilitative devices would cover the complete hand ROM and all of the DOFs. However, in practice, the solutions presented in the state-of-the-art technology are always a trade-off between size, wearability, weight, strength, and the specific type of movement actuated. As a result, rigid hand exoskeletons able to cover all hand ROMs and DOFs are currently unavailable, as can be observed in Table 3. In the literature, various works lack explicit information about ROM data [23,25,33,38]. In other cases, only partial details are provided regarding the ROM of the device [22,29,30,46]. Meanwhile, some studies provide more comprehensive insights and detailed information [24,27,28,31,32,42].
 Table 3. Actuator type and ROM achieved by rigid exoskeletons presented in the literature. FF: finger flexion; TF: thumb flexion; DIP: DIP fingers; PIP: PIP fingers; MCP: MCP fingers; CMC: CMC thumb; MCP: MCP thumb; IP: IP thumb.
Table 3. Actuator type and ROM achieved by rigid exoskeletons presented in the literature. FF: finger flexion; TF: thumb flexion; DIP: DIP fingers; PIP: PIP fingers; MCP: MCP fingers; CMC: CMC thumb; MCP: MCP thumb; IP: IP thumb. - Force. Force is another aspect to consider when designing a hand exoskeleton. Human hands can exert various types of force and adjust their grip strength depending on the object to be grasped. In exoskeleton devices, the force is typically measured through force sensors at the fingertips [27]. Solutions exploiting other points on the exoskeleton are presented in the literature, for example, embedded into the linear actuator supports [32].Usually, the information provided by the sensor is used as feedback for the therapist, enabling a constant analysis of the rehabilitation process. In rigid hand exoskeletons, such as those with a remote center of rotation or those employing consecutive link mechanisms, the force is applied perpendicular to the contact point between the device and the phalanges. This force may not be uniformly distributed, depending on the number of activated DOFs.According to the literature review, the minimum force needed in grasping and manipulation tasks ranges between 10 N and 13 N. Meanwhile, for daily life activities, a force value of 20 N is usually indicated [8,29]. The device presented in the work by Moreno et al. [31] exhibits a force output of 10 N, whereas the devices in other papers [27,29,30] can exert maximum forces of 8, 15, and 30 N, respectively. However, in most of the works analyzed in the literature review, there are no data and tests regarding the maximum force exerted by the devices. Usually, the authors prefer to use actuators able to deliver more than 20 N in order to be able to use the device for daily life activities [23,32,52].
4.3. Interactive Experience Features
- Wearability. The wearability of rigid exoskeletons is consistently regarded as a fundamental requirement by researchers in the field: keeping the exoskeleton worn and used for prolonged periods of time reflects a lot on the rehabilitation process and the user’s autonomy [25,59].Addressing the wearability requirement necessitates careful consideration of various factors. One important aspect is the choice of materials for exoskeleton manufacturing, as these should guarantee a long-lasting performance over time. For instance, in the work by Tong et al. of 2010 [22], the authors used a combination of materials, i.e., Acrylonitrile Butadiene Styrene (ABS) and aluminum. In alternative cases [32,38], the device is made in ABS, while in others [31,32], a combination of plastic and flexible materials is used. Furthermore, to guarantee the wearability, the weight of the exoskeleton should be as limited as possible by choosing the appropriate actuators and defining the best position for the actuation unit.In rigid exoskeletons, the actuation unit tends to be positioned on the back of the hand to minimize interference as much as possible during the activities of daily living by connecting the actuators directly to the mechanical structures. The mechanical structure responsible for finger movement is designed to have a limited height and length and should not exceed the size of the user’s fingers.The works analyzed in the literature review show that certain types of finger movement, such as finger abduction/adduction, are often restricted with respect to others, i.e., finger flexion/extension. This choice allows the number of required actuators to be limited. Furthermore, often, the thumb is partially implemented or excluded completely from the design due to its complex kinematic structure. There are also solutions aimed at limiting the number of actuators per finger, e.g., the one presented in the work by Dragusanu et al. [40] where a differential mechanism is employed to couple the motion of two adjacent fingers.In human/exoskeleton interaction contexts, a device is defined as transparent when it does not modify the nominal behavior of the user in terms of the end-effector, joint trajectories, and patterns of muscle activation [60]. Transparency can be obtained in rigid exoskeletons by employing suitable control strategies. For instance, Topini et al. [61] proposed a device in which an admittance control with a real-time varying admittance model is implemented to effectively support the patient’s desired motion.Reversibility is another desirable property of exoskeletons. Firstly, a mechanically reversible device is efficient from the energy consumption point of view. Reversibility enhances device safety since the device can be always forced by the user in case of issues and allows the user’s interaction to be detected. Reversibility can be obtained by choosing high-efficiency actuators and properly designing the transmission systems [45]. When the employed actuators do not allow this property, for instance, linear actuators, which usually have lower efficiency levels, the reversibility can be obtained by the device sensing and control system [32].Rigid hand or finger exoskeletons are usually connected to the hand by flexible and adaptable fabric components. The actuators are usually positioned on the back of the hand [34,44,52] or on the forearm [25]. Usually, a rigid support for the actuators is present, connected to the hand palm or to the forearm with flexible and adaptable Velcro straps or similar systems. The parts of the exoskeleton activating the fingers are connected to the phalanges through rigid or flexible rings. In some cases, the structure is connected directly to the fingertip through a thimble [34].
- Control. Often, in rigid hand exoskeletons, the control system consists of a microcontroller that processes information, such as sensor data, and generates commands for the actuation unit. Additionally, an auxiliary data processing unit, for example, a tablet or a computer, accessible to both the user and specialist is used to monitor the user’s activities and progress [32]. In the state-of-the-art technology, different control methods are employed in the rigid hand exoskeleton to provide various forms of rehabilitation, like active, passive, resistive, and active-assisted. The most common types of control are those based on force, position, or torque control. Other control signals can be used, such as bio-signals, voice signals [28], and simple trigger signals. Rigid hand exoskeletons mostly rely on position and force control. Meanwhile, others incorporate bio-signal-based controls. The trigger control exploits buttons to activate specific exercises for the user’s rehabilitation. Usually, these exercises consist of pre-defined actions such as opening/closing the hand and grasping an object [46,47].Force-based control is an interactive modality that aims to create an active rehabilitation tailored to the user. In this case, rigid hand exoskeletons are actuated on the basis of the force exerted by the user. By using this approach, the users are actively engaged, allowing them to improve their hand skills throughout the rehabilitation process: the exercises employed enhance the manipulation of objects and help to increase the hand grip force. Consequently, this type of exoskeleton control is also used in active-assistive rehabilitation, based on the specific user’s needs. For instance, Topini et al. [61] implemented an admittance control system for a hand exoskeleton to be applied in Virtual Reality (VR)-based rehabilitation tasks, which varies the control parameters to properly render the force sensation and to adapt to the user’s motion intentions.Position-based control is usually implemented by using pre-defined inputs to obtain desired exoskeleton motions. This method is preferred for the passive rehabilitation modality, where the exercises are conducted by giving an input command to the controller, which is then processed and consequently sent to the actuators, which are controlled in terms of their positions. Current research in the field of rigid hand exoskeleton indicates that PID (Proportional-Integral-Derivative) and PD controllers are predominantly employed [23,24,25,27,30,34,36,41,53]. Among the different control models, position-based control and force-based control are the most commonly used approaches [31,32,35,43,45].The literature analysis shows that, apart from force sensors, the force exerted by the user can be measured through bio-signals. These signals are employed as control inputs for the exoskeleton device. Current research indicates that the bio-signals commonly used for controlling rigid hand exoskeletons are electromyography (EMG) signals, electroencephalography (EEG) signals, and electrooculography (EOG) signals [22,28,29,33,37,38,42]. These signals can be obtained through non-invasive procedures, allowing clear interactions between the user and the device. The primary purpose of these technologies is to discern the patient’s intentions. Studies have demonstrated that incorporating user interactions with training can enhance the recovery and promote cognitive function [25]. Furthermore, the current trend in this field is to integrate bio-signals with artificial intelligence techniques.
- Portability. Portability is considered one of the emerging key features in rehabilitative hand devices and it turns out to be a relevant aspect in rigid hand exoskeletons. This feature allows end-users to independently wear and use the exoskeleton, possibly with limited support or without the support of specialists or assistants. The literature review shows that portability is an important feature to be considered: over time, in the field of rigid exoskeletons, there has been a shift in the design from grounded solutions that were challenging to wear and limited to specialized centers, like those presented in the work by Schabowsky et al. [53], to more easy-to-wear and friendly solutions, such as those proposed by Dragusanu et al. [52].Currently, there is a growing emphasis on user-centered design solutions [62], where the user plays a central role in the development of the whole device. This approach gives the user a deeper impact on the design, as they are involved in all of the main design and prototyping phases. It is worth noting that the rehabilitative device, in this case, the rigid hand exoskeleton, ought to be accepted and adopted into everyday practice by the users. To accomplish this, it is crucial to understand the specific users’ needs and expectations, including aspects such as quality of life, sense of control, dignity, and independence. Participatory design processes involving end-users might overcome the conflicting values and expectations of developers and end-users [63,64] in terms of the device portability. In [32], a rigid hand exoskeleton designed for a specific user is discussed, allowing them to create their own rehabilitation program. Similarly, in [37], the authors prioritize the aspect of a lightweight design, aiming to enhance portability.
5. Soft Robotic Exoskeletons for Hand Rehabilitation
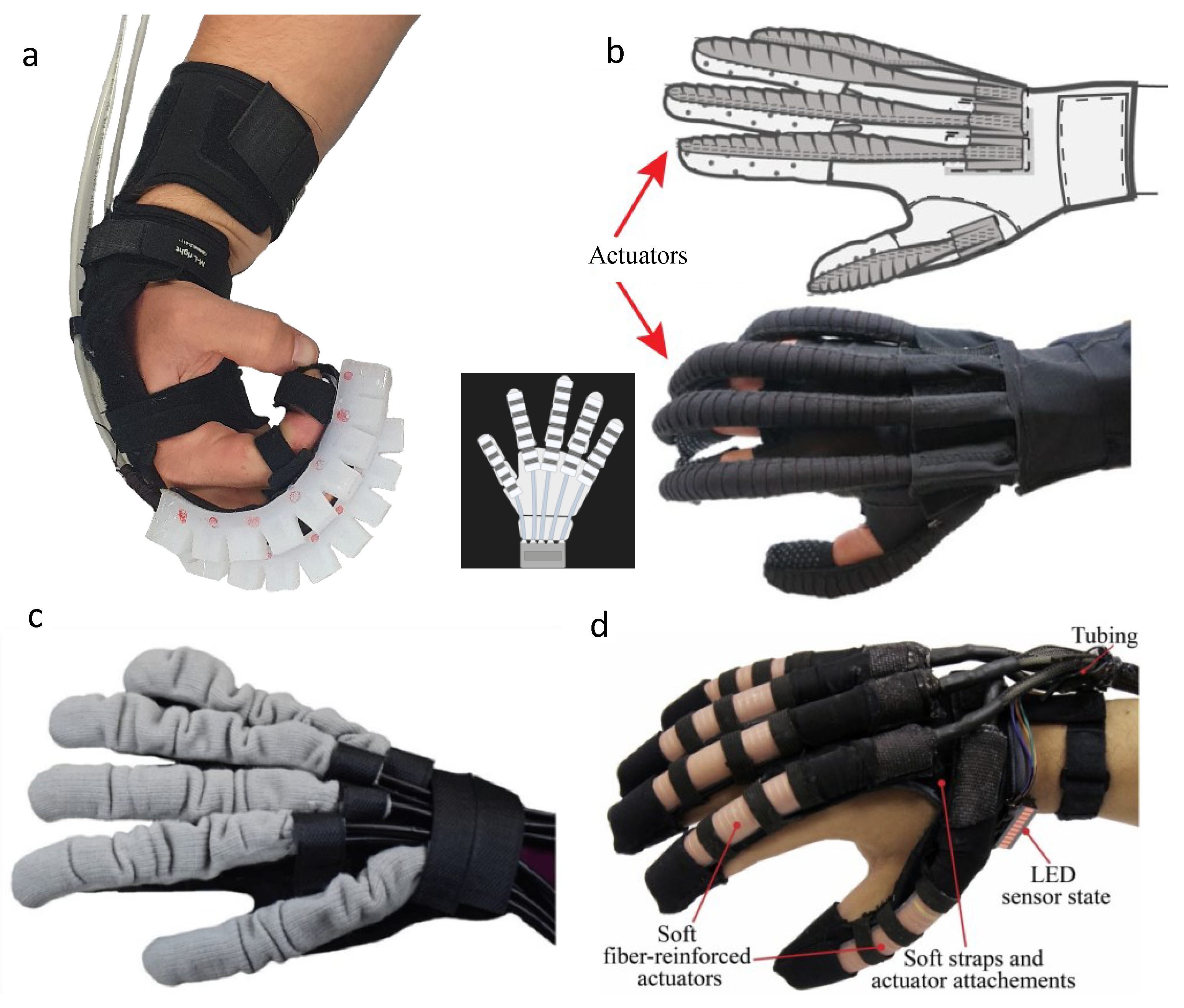
In recent years, the development of soft robotics rehabilitation systems based on soft actuation has increased significantly. Figure 4 collects some examples of these devices. Soft actuators (SAs), or semi-soft tendon-driven actuators, have characteristics that make them particularly suitable for robotic rehabilitation compared to rigid actuators. The intrinsic compliance of these systems allows for safer interaction with the limb being rehabilitated; they can also be lighter. Exoskeletons with soft actuators are generally defined as soft gloves [65].
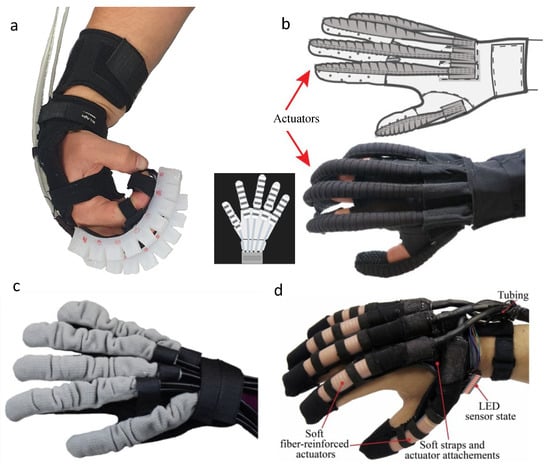
Figure 4.
Examples of soft hand exoskeletons. (a) Soft exoskeleton with Pneu-Nets soft actuators. Source: Tiboni et al., 2023 [66]. (b) Example of a fabric-based soft exoskeleton. Source: Cappello et al., 2018 [67]. (c) Wearable exoskeleton with Machine-Knitted Seamless Pneumatic Actuators. Source: Elmoughni et al., 2021 [68]. (d) Soft robotic glove with actuators consisting of molded elastomeric chambers with fiber reinforcements. Source: Polygerinos et al., 2015, open manuscript [69].
5.1. Soft Robotic Exoskeletons Actuation
Pneumatics is the predominant actuation technology used in robotic gloves [70], which are therefore mainly based on pneumatic actuators (PAs). The choice of actuator type has a decisive impact on the final structure of the device. Different categories of soft actuators have been developed and presented in the literature for the actuation of soft gloves. Pneu-Nets Soft Actuators (PNSAs) made of elastomers, whose first concept goes back to Polygerinos [71], have been studied by several authors and used in a considerable number of soft glove solutions [66,72,73,74,75,76]. Pneu-Nets soft actuators move the finger joints directly by positioning them over the fingers. Different constructive versions have been developed to improve the movement and thrust and to achieve a movement of the fingers that is as close as possible to the physiological one. In [72], Wang X. et al. present an optimized design of Pneu-Nets soft actuators based on the finite element analysis. Using material tensile tests, they first determined the hyperelastic constitutive model, which was then used in the FEM analysis. From the optimization, they concluded that a geometry with a semicircular chamber has a better performance than one with a conventional rectangular cross-section. The authors also presented an innovative design for a soft rehabilitation glove consisting of adaptable parts and newly developed soft actuators. The new actuator can move each finger joint, because it is small enough to be attached to the knuckle of the glove. PNSA structures with variable levels of stiffness were designed to achieve bending at the finger joints and straight behavior at the segments, according to the skeletal characteristics of the human hand [73]. Two different technological processes are usually used in the production of Pneu-Nets: casting in a mold or direct 3D printing. Curing of the silicone in a plastic mold made by additive manufacturing is the most common process, but recently, with the continuous innovations in 3D printing, direct printing of the silicone-based actuator has also been applied. This has greater simplicity and speed of production (since the actuator is made in a single body), but it has the disadvantages of a limited choice of materials and expensive equipment. The bending motion of this family of soft actuators is due to the presence of a strain-limiting layer. The classical solution for casting in a foundry process involves fabricating the strain-limiting layer separately from the actuator body and then bonding it. Some authors propose solutions for monolithic cast-in-a-mold fabrication processes, in which a core of wax is inserted and then removed by heating [66] or a soluble TPU. PNSAs bend well and easily, but can only exert relatively low forces, around the 1–2 N range. Fiber-reinforced actuators belong to another category of soft actuators. They have a compact structure and can provide high forces, reaching values of 8 N, compared to Pneu-Nets. Fabrication based on a lost-wax process allows monolithic molding, and the use of an inverse-flow injection (IFI) method reduces unwanted bubbles in the final actuator [77]. A soft glove designed with fiber-reinforced actuators can be more compact than one using Pneu-Nets or other categories of soft actuators [78,79,80,81]. Positive-negative pneumatic actuators (PNPAs) are another category of soft actuators [82,83] that allow active control of both flexion and extension when used in a soft glove, as opposed to the previous types that allow the active implementation of bending motion only. Bellows are the main element of PNPAs. Positive and negative pressure are used to expand and contract the bellows, which are placed on the back of the hand, and a strain-limiting layer is used to achieve active flexion and extension, respectively, causing the closing and opening of the fingers. In [82], Hu et al. achieved a maximum initial force of 4.6 N for extension and 1.9 N for flexion. Because of their flexibility, lightness, wearability, and inherent anisotropy, tissues are used as materials of construction in another category of soft actuators, SFPAs [84], i.e., soft tissue-based pneumatic actuators. The operation of a finger extension SFPA is based on the change in body stiffness. The finger extension SFPA is flexible enough to adapt to the curved finger when the air is released. The finger extension SFPA generates an extension force and moment after inflation, as it stiffens and tends to straighten. Feng et al. introduced a subclass in [85], which they called high-force fabric-based PAs (HFFPAs). Two independent textile layers are fabricated, two sealing edges which are attached to the dorsal side of the glove to form the eccentric solid shaft of the asymmetric chamber. With a pressure of 150 kPa and a constructive geometry based on semicircular chambers, they achieved a blocked force of about 13 N. Recently, several soft wearable gloves with fabric-based PAs (FPAs) have been developed [9,65,86].
For each of the categories described, a considerable number of papers can be found in the literature. There are particular types of SAs proposed by a single author or a very limited number of authors, such as Thin McKibben Muscles [87] or PAs with a Jamming Structure [88].
5.2. Functional Features
- Actuated movements. Most soft robot gloves with pneumatic actuation are designed to move all five fingers [74,75,89] so that the entire hand can be opened and closed. Soft gloves can allow the activation of only flexion, only extension, or both. The most important option is the movement of three fingers, namely the thumb, index, and middle finger. The movement of these three fingers allows the execution of a large number of important ADLs and gestures. Very few devices allow the actuation of one or two fingers, and in those cases where this is the case, it is performed to demonstrate the feasibility of the actuation system. There is a clear trend in the literature toward solutions in which both flexion and extension are activated, but flexion is often activated actively and extension passively. The proportion of gloves in which only one of the two actions is triggered also shows this preference for flexion over extension. Moving the thumb presents a more complex challenge than the other fingers. The most common choice is to implement only flexion and extension movements with an actuator similar to the actuator used for the other fingers, of course with smaller dimensions. In some cases, solutions have been proposed that also implement the adduction movement [79,82] with specially developed actuators.
- ROM of actuated movements. For the range of motion, some authors give the results obtained in general terms, without distinguishing between the fingers and the finger joints; others give the ranges for the different joints, again without distinguishing between the fingers; still others give precise data for the joints, distinguishing between the thumb and the other fingers. Table 4 summarizes the data on the ROM of some devices presented in the literature. Very often, the design features of the soft actuators used in soft exoskeletons allow the actuation of one degree of freedom for each finger without allowing the control of interphalangeal movements. In some cases, which are much rarer, the appropriately designed geometries of the soft actuators also allow motion control of the different phalanges. From the ROM analysis given by some authors and summarized in Table 4, it appears that for the proximal metacarpophalangeal joint of the finger (PIP), there is a considerable uniformity of values (between about 80 and 85), whereas for the other joints, there are considerable differences between the values obtained with the different devices. For example, for the proximal finger joint, there are values below 30, above 80, or around 58. The values obtained for PIP correspond to those of a normal hand; for the other joints, the values are comparable in some cases and much lower in others.
 Table 4. ROM achieved by soft exoskeletons presented in the literature. FF: finger flexion; TF: thumb flexion; DIP: DIP fingers; PIP: PIP fingers; MCP: MCP fingers; CMC: CMC thumb; MCP: MCP thumb; IP: IP thumb.
Table 4. ROM achieved by soft exoskeletons presented in the literature. FF: finger flexion; TF: thumb flexion; DIP: DIP fingers; PIP: PIP fingers; MCP: MCP fingers; CMC: CMC thumb; MCP: MCP thumb; IP: IP thumb. - Forces developed by the devices. In Table 5, the values of the maximum forces/maximum loads given by the authors of the analyzed publications in relation to the soft exoskeletons for the hand are listed. As can be seen from the large number of columns, there is great heterogeneity in the characterization of the devices in terms of the forces and load capacity. Some authors have characterized the device in terms of the maximum force that can be developed at the tip of a single finger. Others have used the maximum total force that can be developed at the fingertips, i.e., the maximum grip force. In other cases, they refer to the performance of the device in relation to the activity to be performed, i.e., the maximum value of the mass that can be lifted, gripped, or pinched. The range in which these quantities vary with the variations of the device is very large. The maximum force that can be developed by the fingers as a whole is 148.36 N, and this was obtained with textile actuators with TPE. Values of about 40 N can be achieved with fabric-reinforced soft actuators. With soft actuators with Pneu-Nets, the values of the force that can be developed are lower, between 10 and 19 N. The maximum mass that can be lifted ranges from 220 g for Pneu-Net soft actuators to 1000 g for textile actuators with TPE and even up to 3000 g for soft bending actuators. Of the analyzed papers, only one gave the grip force, which was about 42 N.
 Table 5. Forces achieved by soft exoskeletons presented in the literature. mFF: maximum fingertip force; mTF: maximum tip force; mGF: maximum grip force; mFGF: maximum frictional grip force; mLM: maximum liftable mass; mGL: maximum grasping load; mPL: maximum pinching load; TAP: test actuation pressure; weight: device weight.
Table 5. Forces achieved by soft exoskeletons presented in the literature. mFF: maximum fingertip force; mTF: maximum tip force; mGF: maximum grip force; mFGF: maximum frictional grip force; mLM: maximum liftable mass; mGL: maximum grasping load; mPL: maximum pinching load; TAP: test actuation pressure; weight: device weight.
5.3. Interactive Experience Features
- Wearability. Articles providing information on the portability and wearability are mainly papers describing clinical trials and results [99,100,101,102,103,104,105].The studies by Radder et al. [99,100,101] investigated user acceptance (e.g., perceived ease of use, motivation, system usability) and the effects of the soft robot glove system HiM (Handin- Mind) on the performance of activities of daily living (ADLs) by five chronic stroke patients. The System Usability Scale (SUS) was used to measure usability, and the Intrinsic Motivation Inventory (IMI) was used to measure motivation (in terms of interest/enjoyment, perceived competence, effort, perceived choices in performing a particular activity, experienced pressure/tension, and value/benefit). User acceptance measured by the SUS and IMI was scored high. Results were positive regarding the usability of the device, especially for gross motor activities, while performing fine motor tasks with the glove proved difficult. Poor performance in the motor task was also reported by Palmcrantz et al. [103]. Osuagwu et al. [104,105] showed that self-managed rehabilitation at home with the soft extra muscle (SEM) glove [106] is effective for improving and maintaining gross and fine motor skills in the hands of people with chronic spinal cord injuries or chronic tetraplegia. Thus, home-based rehabilitation may be possible and effective with soft robotic gloves. The wearability of an exoskeleton is significantly influenced by its weight. The soft exoskeletons presented in the literature have quite different weights; the ones analyzed have a weight that varies between about 100 g and 240 g [86,89,92,94,97]. They are therefore characterized by very good lightness. In soft gloves, soft actuators designed and developed ad hoc are used in most cases. From the analysis of the state-of-the-art technology, it appears that these are soft actuators with very compact and extremely adaptable geometries, which allow soft gloves with high potential in terms of ergonomics and adaptability to be obtained.The feature of transparency, which affects the wearability and safety of the device, is generally very rarely discussed when presenting soft exoskeletons. Only some authors have reported a few cases but without going into detail in the discussion. Wang et al. [92] developed a soft exoskeleton for the fingers and wrist. They considered transparency to be a fundamental feature in the development of wrist actuation. They designed a wrist brace that has adjustable tightness, adapts to the movements of the wrist, is comfortable to wear, and provides good transparency for the soft glove. The fabric-based robotic glove developed by Yap et al. [86] has five finger actuation pockets on the back. As it ensures that there is little mechanical resistance to finger movements and allows kinematic transparency when worn, the glove acts as a compliant interface between the actuators and the hand. In general, many actuator solutions for soft exoskeletons, in particular, actuators made from fabric or with thin artificial McKibben muscles [107], are characterized by their high transparency.Reversibility was never discussed in the examined articles. However, it should be pointed out that, in pneumatic systems with actuators made from flexible materials, reversibility is a feature that the actuation system itself guarantees.The long-lasting performance of soft exoskeletons could be a very important issue to address given the intrinsic compliance properties of the actuators most commonly used in these devices. However, no author has reported on the durability or long-term testing of the developed devices. It must be considered, however, that all of the devices presented in the literature are at the prototype development stage.Finally, regarding the attachment of a soft exoskeleton to the patient’s hand, the most commonly adopted solutions are either the use of Velcro straps connected to elements on the back of the hand to which the actuators are attached or the use of gloves to which the actuators are attached. In the case of fabric-based soft actuators, in some cases, the actuators are integrated directly into the glove. The choice of a particular solution has a significant impact on the comfort of wearing the exoskeleton.
- Control possibilities. Soft glove control can be implemented with different solutions. Model-based control is the most widespread, while control strategies based on the evaluation of EMG signals are growing strongly [93,108,109,110]. EMG signals are collected from the impaired hand and are used to record residual muscle activity for EMG-based control. Sometimes, machine learning algorithms are used to control these devices based on force feedback obtained by measuring EMG signals, as was performed in the paper published by Sierotowicz et al. [109]. In this work, the authors developed a soft wearable glove controlled by a machine-learning-based intent detection system applied to closed-loop sensed muscle activity. Soft exoskeletons are often equipped with sensors of various types that provide feedback to control movement. In some cases, these gloves have actuators that generate sensory feedback [111,112]. Bending sensors are the most common, followed by force or strain sensors, IMUs, pressure sensors, sEMG sensors, as well as soft sensors, often custom-made, which are used to detect motion and to control the device. The widespread use of flex sensors to detect the bending angle of the fingers or force or strain sensors corresponds exactly to the function of a soft glove. In the hand exoskeleton HEXOES [113], control is enabled by flex sensors over the actuated joints and force sensors on the linear actuators. Mirror therapy [114] and bilateral training are often combined with robotic gloves gloves (regardless of the rigid, soft or hybrid type), creating a system in which the movement of the healthy hand controls the robotic device on the impaired hand [110]. The combination of mirror therapy and robotic rehabilitation may result in even greater improvements than any single technique [115]. There are numerous papers in the literature dealing with the combined application of these techniques and soft exoskeletons. A hand rehabilitation system based on the concept of mirror therapy, in which a soft glove is controlled by machine learning algorithms applied to EMG signals from the unaffected hand, is presented in the work by Chen et al. [116]. For bilateral training, Yap et al. [86] developed a soft robotic glove that can be controlled by signals from flex sensors in a data glove worn on the healthy hand.The use of pressure sensors for air pressure in the actuators to control the developed force is very common in pneumatic gloves. This control has low precision, but simplicity is its strong point.The inherent compliance of soft gloves leads to a compromise between control precision, material flexibility, and lightness.The intrinsic compliance characteristics of actuators, thanks to the soft materials used for fabrication, allow for the intrinsic safety of soft exoskeletons. However, it is necessary to provide safety systems for use. Additional safety measures have been developed for a limited number of the devices described in the literature. This is probably due to their stage of development, which is still at an early stage [9]. One trend that can be observed is the inclusion of safety features in the control system to minimize the complexity of the device, the number of components, and the weight. Usually, feedback is inserted to control the movement and to avoid risky situations. In some cases, a maximum pressure value is set to avoid excessive forces or bending [95,117]. In other cases, bending sensors are used [118].
- Portability. Only a few devices have been developed with portability in mind, but we have observed an increasing trend in recent years toward the development of devices that are fully capable of being operated by the patient at home without the need for a clinician or technician [94,117]. Several devices have been observed to be portable thanks to the use of compact, battery-powered control units [118,119]. These are important features given the many benefits that can be achieved through home-based rehabilitation. A wearable soft robotic glove can significantly improve the rehabilitation process at home [76]. Devices can be cheaper compared to rigid-body devices because actuators and materials are cheap.
6. Hybrid Soft–Rigid Robotic Exoskeletons for Hand Rehabilitation
While rigid devices offer precise kinematics, strong force control, and efficient power transmission, they are often too heavy, bulky, and stiff for comfortable use by patients. To solve these issues, some rigid devices have elastic elements embedded into the mechanism to increase compliance. Hybrid soft-rigid exoskeletons use a combination of a rigid frame with deformable materials. These compliant materials make the device more comfortable and wearable, making it compatible with the natural movement of the human fingers and enhancing output forces [120]. Hybrid devices composed of alternating flexible joints and rigid links are prevalent design solutions, as reported for the state-of-the-art technology. Based on additive manufacturing, some solutions exploit monolithic designs [16,121,122] and modular structures [123,124,125]. Instead, to employ the potential of rigid devices, elastic spring elements are included [126]. Different technologies can be chosen to obtain a better controlled hybrid exoskeleton, such as soft pneumatic actuation, combining a rigid armor that wraps the flexible element or fiber-reinforced soft bending actuators [127,128]. In another study, Rose et al. designed a hand exoskeleton with a hybrid rigid–soft design that better supports and trains ADLs by combining rigid elements for power transmission and mechanically programmed safety features with soft interfaces for improved wearability [129].
In the area of tendon-driven actuators and soft exo-gloves (SEG), Randazzo et al. showed how an exoskeleton controls both flexion and extension of the fingers using a Bowden cable system [130]. Taking into consideration the criteria defined for the state-of-the-art technology, a classification can be drawn up. All devices have inherent customizability: indeed, each one allows the geometric parameters of the elements to be set according to the size of the patient’s limbs. In addition, the use of 3D scanning technologies allows for increased adaptability of exoskeletons to different anthropometric conditions [131,132]. All of those are equipped with sensors and designed with safety features, such as lightweight and flexible materials [121,124], ergonomic designs [123,126], and control systems [130]. The ROM of each joint can be limited by adjusting the stoppers on each passive slider mechanism on the outer spring for safety [121]. The advantage of the mechanism is that it is compact and lightweight, and most importantly, since the mechanism involves compliant elements, the device can be inherently safety compliant [121]. Therefore, the designed SEG device underwent a series of tests in order to prove its compliance with health, safety, and environmental protection requirements derived from the European Union (EU) Directives and to obtain the CE marking. For instance, the tests examined the device for electromagnetic compatibility (EMC test), electrical safety (low voltage directive—LVD test), and the Restriction of Hazardous Substances (RoHS evaluation) [129]. Every upper spring blade arrives at the endpoint of the respective limit to ensure the safety of patients wearing the exoskeleton [123]. All safety measures are addressed and any undesired shear forces are kept to a minimum during the exercises [126]. The power transmission, built from the rigid elements embedded in soft goods, provides torque through flexible Bowden cable transmission and ensures safety through the judicious placement of rigid elements [127]. The mechanical structure should prevent excessive joint flexion and extension. Moving parts have to be shielded to prevent tissue or body parts from being pinched [124]. To ensure the safety of the soft actuator (e.g., to prevent explosion), a relatively safe pressure was used (i.e., 216.67 kPa) to measure the contact force on the fingertip. Lastly, the soft actuator will not injure users’ fingers, even in the event of system failure. For example, when the air pressure exceeds the allowable pressure of the actuator, the soft actuator will leak rather than explode due to the use of fiber [130]. Overall, exoskeletons offer a safe and effective way to support patients in their recovery from injuries or neurological conditions. Long-lasting performance over time depends on the material properties, in particular, the fatigue life cycle of the device’s joints and cable, where the latter ones are used for tendon-driven actuation. Two kinds of hybrid exoskeletons for hand rehabilitation are shown in Figure 5.

Figure 5.
Examples of hybrid hand exoskeletons. (a) The device consists of pneumatic actuation, combined with rigid armor. Source: Kladovasilakis et al. [121]. (b,c) Global and bottom view, respectively, of a hybrid assistive hand exoskeleton for stroke patience: a rigid structure with flexible joints. Source: Vertongen et al. [127].
6.1. Functional Features
The present section involves an analysis of the available literature in terms of the key trends in functional features and the link between the accepted actuation solutions and functional needs in the process of developing a hybrid robotic exoskeleton. These developments and requirements are discussed in relation to the previous state-of-the-art section.
- Actuated movements. The main goal in the development of devices that integrate both flexible and rigid components involves facilitating the articulation of all fingers of the human hand. While tendon actuation is the prevailing method, there are instances where pneumatic is employed in conjunction with innovative design choices, as reported in [121,128]. In addition to the control of finger flexion and extension, a few studies integrate methodologies for thumb rotation (pronation and supination), hence enhancing the adaptability of the system to various rehabilitation approaches for users and operators [126,129]. Furthermore, the design of the device has been the subject of several studies, with particular emphasis on its portability and lightweight nature [130]. The device developed by Li et al. focuses on one finger, unlike the others, adding an additional degree of rotation of the index finger, mainly related to patients in post-stroke rehabilitation treatments [124].
- Range of motion. The ROM is one of the main parameters for device evaluation. Across different authors, ranges have been reported with a variety of values. Many studies have provided overall results without specifying variations between joints. Others have noted and validated specific thumb or finger ranges. This shortcoming stems from the different technologies adopted by the authors, both for the development of the device and the aim of the study. Some works do not indicate a specific movement range, other than the force values taken as a reference from the literature. Table 6 outlines the parameters of the ROMs for each of the developed devices examined.
 Table 6. ROM achieved by devices presented in the literature. FF: finger flexion; TF: thumb flexion; DIP: DIP fingers; PIP: PIP fingers; MCP: MCP fingers; CMC: CMC thumb; MCP: MCP thumb; IP: IP thumb.
Table 6. ROM achieved by devices presented in the literature. FF: finger flexion; TF: thumb flexion; DIP: DIP fingers; PIP: PIP fingers; MCP: MCP fingers; CMC: CMC thumb; MCP: MCP thumb; IP: IP thumb. - Force. The limited availability of force-related data in the publications examined in this section, which specifically investigated hybrid exoskeletons for rehabilitation purposes, highlights the distinctive difficulties presented by these novel technologies. The following papers present novel combinations of pliable and inflexible materials, including the complex integration of technical principles and biomechanical concepts. The evaluation and characterization of these hybrid exoskeletons, resulting from the unusual fusion, introduce additional levels of complexity to the investigation. The selected studies focus on examining the complex elements of exoskeleton functionality and its ability to support various types of movement. The focus placed on this matter is perceptive, since it acknowledges that the quantification of force in isolation fails to encompass the entirety of the case.
6.2. Interactive Experience Features
- Wearability. The wearability of exoskeletons is one of the most important factors to consider throughout a comparative examination of these devices. A major focus of these devices is their lightweight nature and ease of use. This approach is adopted with the objective of alleviating the degree of tiredness experienced by the user after extended periods of use. The implementation of a single actuator equipped with four fingers is a prevalent technique, presenting significant benefits in terms of its straightforwardness and effectiveness [120]. This methodology becomes beneficial as it enables the flexion and extension motions of the finger. In addition, the use of a Bowden cable system inside the wearable component of the exoskeleton facilitates weight reduction in such components, hence improving the overall comfort when using the device [16,124]. The prioritization of ergonomic concerns places emphasis on individual flexibility and seeks to provide a comfortable fit by customizing the design to accommodate anthropometric characteristics [123]. This claim carries substantial significance. Several devices offer efficient donning features, allowing persons with less prior experience to utilize them effectively for ordinary chores [126,127]. Furthermore, the water and dust resistance features of the devices, particularly in the region where the remote actuation unit is located, augment their practicality [126]. In the realm of extended activities, the attainment of comfort and safety is accomplished by incorporating many features, including but not limited to flexibility and mechanical safety components. Hybrid designs, characterized by integrating rigid components and flexible interfaces, effectively increase the scope of potential applications for these devices to aid in many activities pertaining to daily existence [128]. The proposed technique differentiates itself from other exoskeletons by enabling the active control of finger flexion and extension while also maintaining the inherent somatosensory sense in the palms and fingers [130]. This gives a significant advantage to wearable exoskeleton technologies.
- Control possibilities. There are several approaches to the implementation of hybrid exoskeleton control strategies. Electromyography (EMG) sensors are widely employed for their management, with an external control device such as a personal computer overseeing their operation [120,123]. Furthermore, a crucial feature that is common throughout all of these devices is the capacity to detect and evaluate the angular motion of the finger [121,124]. This facilitates the control unit to receive and process the acquired data more efficiently. In addition, certain devices are equipped with a potentiometer that enables the adjustment of the operational current of the linear actuator [129]. This feature allows for versatility in accommodating both passive and active exercise regimens, which may be customized to meet the unique needs of each patient. These systems include a diverse array of sensors, such as position and torque sensors, thus augmenting their capacity to identify and record human motions and efficiently react to such movements [124]. The integration of force feedback technology at the user’s fingertips is a prevalent characteristic that enhances the overall user experience by facilitating the modeling of typical grasping actions and by making it readily accessible to the user [128]. The combined application of a variety of sensors, such as motor encoders, linear position transducers, and low-profile buttons, allows a comprehensive understanding of hand movements involved in the act of grasping [130]. The main goal is to facilitate versatile and precise control of hand exoskeletons, with a specific focus on replicating natural hand movements and interactions.
- Portability. The devices that have been mentioned differ in terms of their mobility as well as the extent to which users may use them on their own. Some are made to be comfortable to wear and can be used independently without the assistance of an operator. Because of these features, they are appropriate for use in the comfort of one’s own home as assistive or therapeutic device for ADLs. On the other hand, several devices are not portable since they are dependent on connections to other systems such as pneumatic systems or computers, which restricts their ability to be used independently [120,121,123,124]. Among the alternatives, the HSRexo stands out due to its combination of intrinsic compliance and intelligible kinematics. It has benefits such as portability, wearability, and compliance, and it has the potential to reduce expenses while also broadening its usefulness in clinical and domestic settings [16]. Even if specific devices require additional, non-portable equipment, it is still possible to operate with them on their own, provided that at least one hand is not affected. Independent usage that does not require the assistance of medical professionals is made possible by a system that is worn as a backpack and contains motors, electronics, and batteries that are cabled to a hand module [130]. There are a wide range of preferences among users: some people appreciate designs that are stiffer, while others may select designs that are put on one finger at a time [129]. In general, the most important aspects to think about when designing these devices are how simple it is to put them on and take them off, how light they are, how many hard parts they have, and how streamlined their profile is [130]. This is to ensure that they are comfortable to use and that their interactions with their surroundings are unobtrusive.
7. Discussion
The main goal of the current work was to provide a roadmap for both the design and selection of exoskeletons for hand rehabilitation that can capture the peculiarities of soft, rigid, and hybrid devices with an impairment-oriented rationale for the final purpose of matching technical specifications and clinical needs.
Accordingly, the first part of the paper focused on the description of the strategies for the identification of the subject’s impairments (which define the clinical specifications) and the detection of the main characteristics of state-of-the-art hand exoskeletons (outlining the set of feasible technical features).
The PICO model allows for the careful recollection of the set of impairments, both functional and structural, that most likely may affect the end-user of a hand exoskeleton. Those impairments, reported in Table 1, can arise as consequences of very different pathologies, and often, the disease itself is used by the clinician as the first filter for the device selection. However, this approach is less efficient than tracing back the clinical picture to the impairments, since filtering by pathologies can cause the clinician to miss all of the devices compatible with the patient’s needs that were developed for a different purpose in the designer’s mind. In this context, the knowledgeability of the physician becomes fundamental in recognizing the impairments; actually, a first mapping between pathologies and impairments is outlined in Table 2, but a thorough analysis is still missing. Some investigations in this sense are currently under evaluation.
On the other hand, data are available in the literature regarding the technical features characterizing hand exoskeletons. The issues in this context refer to the wide variety of possible features and the peculiarities derived from the different architectures, i.e., rigid, soft, and hybrid devices.
The proposed design approach for robotic hand rehabilitative exoskeletons highlights the complexity of the design process, which evolves from an ideally linear procedure towards a set of interconnected iterative optimization phases. At each step of the process, new or updated technical requirements can emerge. The approach proposes a new classification strategy for the characteristics of the exoskeletons, i.e., functional and interactive experience features. The analysis of the devices, performed by the architectural class, allows those concepts to be elaborated in more detail: in fact, a set of features and feature details synthesized in Table 7 and Figure 6 has been identified.

Table 7.
Performance of soft, rigid, and hybrid soft/rigid hand exoskeletons in terms of design/selection features.
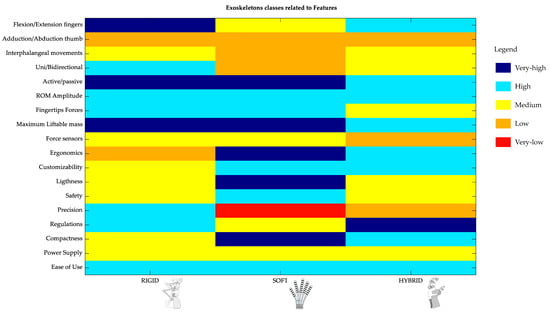
Figure 6.
Color-based representation of soft, rigid, and hybrid soft/rigid hand exoskeleton performance in terms of the design/selection features.
In particular, Table 7 enables a direct comparison of the technical requirements among rigid, soft, and hybrid hand exoskeletons for each feature. This kind of schematic is expected to be especially suitable for the designer of devices, who can make use of this matrix-based synthesis to promptly extract detailed technical information.
Figure 6 instead presents a qualitative evaluation of the performance assured by the three device families for each feature with a graphical approach. This synthesis is designed to be an immediate supportive tool for device selection, simplifying the interpretation of the technical characteristics, and helping the operator to identify the appropriateness of an architectural solution for specific purposes. For instance, the figure clarifies the tendency for the better performance of the rigid exoskeleton class in assuring the flexion/extension of fingers compared with soft-based devices, whereas better performances in terms of compactness tend to be provided by soft exoskeletons with respect to rigid-based systems. Exoskeletons of the hybrid class generally rank in between these extreme conditions. However, the schematic synthesized in Figure 6 has some limitations, primarily due to the quality of the available data: indeed, the literature presents little data, for some features especially, and there is a high variability for the results within the same class. The figure thus aims for synthesis, where possible, but the data should be analyzed with these limitations in mind.
Within this overall context, the relation between defined impairments and functional features can be finally investigated.
When comparing the two subsets of requirements, an immediate association emerges between n ROM limitation impairment and an ROM feature on one side, and between a strength reduction impairment and a force feature on the other. For all other impairments, intercorrelations can be identified with one or more features, but specific considerations must be regarded.
The ROM limitation impairment can be directly associated with the ROM feature. The distinction between uni- and bidirectional movements, as well as between active and passive motions, is likewise reported in both fields. A slightly different approach refers instead to the amplitude of the ROM feature: the designer focuses on providing maximum values of stroke allowed by the device, whereas the clinician aims to regain the ROM functionality of the subject’s hand, incrementally. Likewise, a direct relation can be identified between the strength reduction impairment and the force feature, especially if comparing motor control impairments on one side, particularly fine ones, and tip forces.
Nonetheless, both for ROM limitation and strength reduction, fundamental information for the clinician should be also expected from other elements, like the analysis of the actuated movements feature, which provides hints about the exercises allowed by the specific system. Actually, this feature relates very closely also to other additional impairments, such as coordination and sensory disorders, or tone alterations, since the actuation strategy in these conditions can enable or prevent the execution of some tasks (e.g., all fingers together simulating grasping, a precision pinch, or flexion/extension of one finger at a time).
According to this consideration, a first attempt to define the set of allowed exercises as an additional technical feature was initially evaluated, but this option was revealed to be impractical: papers focusing on the device design do not typically include this kind of information. On the contrary, literature that depicts details on this topic generally presents a strong clinical orientation, like clinical trials. These works, though, do not commonly provide technical details on the design of the used exoskeleton and often present protocols that are poorly comparable with each other. Nonetheless, the usefulness of this kind of feature is evident: for instance, cases of tone alteration can easily envisage rehabilitative treatments involving continuous passive motion strategies, which require exoskeletons with actuated joints to be performed. Similarly, coordination disorders reasonably require active-assistive exercises, and sensory disorder exercises demand haptic feedback and the assessment of the exerted forces: the selected exoskeleton should therefore allow integration with force sensors at least.
Similar relations can be identified for other motor disorders: pain, edema, and fatigue. Each of these impairments is reflected in the expected technical features of the device, although it is more difficult to delineate generally valid considerations in these cases.
In the same way, the characteristics classified as interactive experience features can provide interesting indications: the features wearability, control, and portability describe the expected inter-relation between the end-user and device.
In the choice of the optimal device, the possibility of independently donning the exoskeleton at home, the implementation in the device control of strategies to regulate the maximum exerted forces and ensure safety, as well as the level of customizability of the exoskeleton for the anthropometric variability of subjects represent examples of common scenarios used in everyday clinical practice. These aspects must be appropriately matched to the patient’s clinical picture, so in this case, it is difficult to identify guidelines for these features that are generally valid for specific impairments, whereas it becomes easier, on the contrary, to identify relations with the referring pathologies. Indeed, some disease types or stages introduce specific limitations to exoskeleton selection: for instance, exoskeletons are generally connected to the wearers’ hand by different design solutions, such as fabric rings, gloves, braces, or straps, but post-stroke patients with hand spasticity may likely need a device that leaves the hand palm-free, as much as possible, since the continuous stimulus provided by direct contact would instead accentuate the flexion reflex, risking a further increase in the spasticity itself. In these cases, the donning of the device could be especially delicate as well: exoskeletons presenting finger-stalls could be, for instance, preferred to full glove ones, for ease of wearing. In the same way, depending on the pathology, the presence of some sensors within the device could ease the measurement of specific outcomes, which are expected by the clinician to assess the state of the impairment and the evolution of the pathological condition of the patient: for example, integrated EMG probes could enable the measurement of the force outcome, which is useful in the evaluation of the strength reduction impairment. Similarly, flex or angular sensors could allow the assessment of outcomes related to the ROM limitation impairment. Besides, these aspects could be considered less relevant in cases requiring continuous passive motion (CPM) of the subject, since in this context, no force is required or expected by the subject themselves.
Finally, to select an exoskeleton for hand rehabilitation, moving from impairments to diseases, additional fundamental aspects that affect the overall quality of the treatment and are related to the device characteristics should be considered, but these rarely emerge from the analysis of the system technical features. Examples of these characteristics are, for instance, the possibility of integrating external multi-sensory stimuli to the device or enabling mirror therapy solutions, allowing the treatment of patients with neuro-cognitive deficits (e.g., post-stroke patients).
8. Conclusions
In this paper, we proposed a new roadmap (i) for both the design and selection of exoskeletons for hand rehabilitation, (ii) to discriminate among the peculiarities of soft, rigid, and hybrid devices, and (iii) with an impairment-oriented rationale.
To map the clinical specifications and technical features of hand exoskeletons, a PICO-inspired approach was applied, focused on impairments, to capture the clinical requirements, whereas the technical features were identified from the requirements extracted from the proposed exoskeleton design process and a narrative literature review. The technical features were reorganized into functional and interactive experience features, and the analysis was performed by investigating the three classes of rigid, soft, and hybrid architectures.
The performed cross-analyses between device families and features were synthesized in a table (Table 7) and a graphical matrix (Figure 6), which was intended to be a supporting tool for both the design and selection of hand exoskeletons within an impairment-oriented rationale. These tools provide a general overview of the main peculiarities of rigid, soft, and hybrid exoskeletons for hand rehabilitation, revealing direct relations between some impairments and technical features (e.g., ROM limitation–ROM feature, strength reduction–force feature) and more complex inter-dependencies of factors for others. Nonetheless, these indications shall be integrated with further considerations, i.e., including the additional aspects that could affect their correct interpretation. For instance, the clinical picture of the specific end-user could introduce additional requirements for the device or could evolve in time: in this case, the proposed tools can support the identification of the most proper device at the actual stage of the pathology, but cannot assure that the device will remain the optimal solution during the disease evolution. This consideration is especially true when the choice of an exoskeleton is performed with a patient-centered rationale and not a pathology-oriented approach. The former is the case of the end-user being willing to select a device; the latter is the most typical case in clinical environments, such as hospitals and rehabilitation centers, in which the selection of devices is constrained to the potential number of patients expected for a given pathology at a specific stage.
The awareness of a possible evolution in the clinical requirements needed by the end-user of a hand exoskeleton also suggests that the devices themselves could evolve with the patient’s needs: modular solutions, with interchangeable modules and sensor units could, in fact, offer an interesting option. Further evaluations are currently under investigation in this direction.
On the same note, further studies are currently ongoing to explore the feasibility of integrating the PICO model with both the traditional and the more innovative processes for the design of medical devices. The PICO model, as is, or adapted where needed, could help to elicit hidden requirements, reducing the resources (time, personnel, and costs) used during the product development and optimizing, in this way, the overall design process of devices.
Author Contributions
Conceptualization, G.M.A., C.A., M.D., M.G., S.L., M.M., M.T. and M.C.V.; methodology, G.M.A., C.A., M.D., M.G., S.L., M.M., M.T. and M.C.V.; formal analysis, G.M.A., M.D., M.G. and M.T.; investigation, G.M.A., C.A., M.D., M.G., S.L., M.M., M.T. and M.C.V.; writing—original draft preparation, G.M.A., C.A., M.D., M.G., S.L., M.M., M.T. and M.C.V.; writing—review and editing, C.A. and M.T.; supervision, M.T. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially funded by “Fondazione CARIT 2022”, grant “Progettazione e caratterizzazione sostenibile di materiali per applicazioni industriali, agroalimentari e biomediche”.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| ADL | Activity of Daily Living |
| CMC | Carpo-Metacarpal |
| CNS | Central Nervous System |
| CPM | Continuous Passive Motion |
| CT | Computed Tomography |
| DC motor | Direct Current |
| DIP | Distal Interphalangeal |
| DOF | Degree of Freedom |
| EBM | Evidence-Based Medicine |
| EEG | Electroencephalography |
| EMC | Electromagnetic Compatibility |
| EMG | Electromyography |
| EOG | Electrooculography |
| FEM | Finite Elements Method |
| FF | Finger Flexion |
| FPAs | Fabric-based PAs |
| HFFPAs | High-Force Fabric-based PAs |
| IFI | Inverse-Flow Injection |
| IMI | Intrinsic Motivation Inventory |
| IMU | Inertial Measurement Unit |
| IP | Inter Phalangeal |
| LVD | Low Voltage Directive |
| MCP | Metacarpo Phalangeal |
| MRC | Medical Research Council |
| MRI | Magnetic Resonance Imaging |
| PAs | Pneumatic Actuators |
| PICO | Population/Problem, Intervention, Comparison, Outcome |
| PIP | Proximal Interphalangeal |
| PNS | Peripheral Nervous System |
| PNSAs | Pneumatic Soft Actuators |
| RoHS | restriction of Hazardous Substances |
| ROM | Range of Motion |
| SEG | Soft Exo-Gloves |
| SEM | Soft Extra Muscle |
| SUS | System Usability Scale |
| TPE | Thermoplastic Elastomer |
| TPU | Thermoplastic Polyurethane |
| TF | Thumb Flexion |
| VAS | Visual Analog Scale |
| VR | Virtual Reality |
References
- Thimabut, W.; Terachinda, P.; Kitisomprayoonkul, W. Effectiveness of a Soft Robotic Glove to Assist Hand Function in Stroke Patients: A Cross-Sectional Pilot Study. Rehabil. Res. Pract. 2022, 2022, 3738219. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Nam, C.; Li, W.; Rong, W.; Xie, Y.; Liu, Y.; Qian, Q.; Hu, X. A comparison of the rehabilitation effectiveness of neuromuscular electrical stimulation robotic hand training and pure robotic hand training after stroke: A randomized controlled trial. Biomed. Signal Process. Control 2020, 56, 101723. [Google Scholar] [CrossRef]
- Chowdhury, A.; Meena, Y.K.; Raza, H.; Bhushan, B.; Uttam, A.K.; Pandey, N.; Hashmi, A.A.; Bajpai, A.; Dutta, A.; Prasad, G. Active Physical Practice Followed by Mental Practice Using BCI-Driven Hand Exoskeleton: A Pilot Trial for Clinical Effectiveness and Usability. IEEE J. Biomed. Health Inform. 2018, 22, 1786–1795. [Google Scholar] [CrossRef] [PubMed]
- Sale, P.; Lombardi, V.; Franceschini, M. Hand robotics rehabilitation: Feasibility and preliminary results of a robotic treatment in patients with hemiparesis. Stroke Res. Treat. 2012, 2012, 820931. [Google Scholar] [CrossRef] [PubMed]
- Du Plessis, T.; Djouani, K.; Oosthuizen, C. A Review of Active Hand Exoskeletons for Rehabilitation and Assistance. Robotics 2021, 10, 40. [Google Scholar] [CrossRef]
- Troncossi, M.; Mozaffari-Foumashi, M.; Parenti-Castelli, V. An Original Classification of Rehabilitation Hand Exoskeletons. J. Robot. Mech. Eng. Res. 2016, 1, 17–29. [Google Scholar] [CrossRef]
- Meng, Q.; Xiang, S.; Yu, H. Soft Robotic Hand Exoskeleton Systems: Review and Challenges Surrounding the Technology. In Proceedings of the 2017 2nd International Conference on Electrical, Automation and Mechanical Engineering (EAME 2017), Shanghai, China, 23–24 April 2017; Volume 86, pp. 186–190. [Google Scholar] [CrossRef]
- Shahid, T.; Gouwanda, D.; Nurzaman, S.G.; Gopalai, A.A. Moving toward Soft Robotics: A Decade Review of the Design of Hand Exoskeletons. Biomimetics 2018, 3, 17. [Google Scholar] [CrossRef]
- Chu, C.Y.; Patterson, R.M. Soft robotic devices for hand rehabilitation and assistance: A narrative review. J. Neuroeng. Rehabil. 2018, 15, 9. [Google Scholar] [CrossRef]
- Zhu, M.; Biswas, S.; Dinulescu, S.I.; Kastor, N.; Hawkes, E.W.; Visell, Y. Soft, Wearable Robotics and Haptics: Technologies, Trends, and Emerging Applications. Proc. IEEE 2022, 110, 246–272. [Google Scholar] [CrossRef]
- Sarac, M.; Solazzi, M.; Frisoli, A. Design Requirements of Generic Hand Exoskeletons and Survey of Hand Exoskeletons for Rehabilitation, Assistive or Haptic Use. IEEE Trans. Haptics 2019, 12, 400–413. [Google Scholar] [CrossRef]
- Boser, Q.A.; Dawson, M.R.; Schofield, J.S.; Dziwenko, G.Y.; Hebert, J.S. Defining the design requirements for an assistive powered hand exoskeleton: A pilot explorative interview study and case series. Prosthet. Orthot. Int. 2021, 45, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Eldawlatly, A.; Alshehri, H.; Alqahtani, A.; Ahmad, A.; Al-Dammas, F.; Marzouk, A. Appearance of Population, Intervention, Comparison, and Outcome as research question in the title of articles of three different anesthesia journals: A pilot study. Saudi J. Anaesth. 2018, 12, 283–286. [Google Scholar] [CrossRef] [PubMed]
- de la Tejera, J.A.; Bustamante-Bello, R.; Ramirez-Mendoza, R.A.; Izquierdo-Reyes, J. Systematic review of exoskeletons towards a general categorization model proposal. Appl. Sci. 2021, 11, 76. [Google Scholar] [CrossRef]
- Güçlü, H.; Cora, A. A survey on wearable hand robotics design for assistive, rehabilitative, and haptic applications. Int. J. Intell. Robot. Appl. 2023, 7, 227–252. [Google Scholar] [CrossRef]
- Lin, L.; Zhang, F.; Yang, L.; Fu, Y. Design and modeling of a hybrid soft-rigid hand exoskeleton for poststroke rehabilitation. Int. J. Mech. Sci. 2021, 212, 106831. [Google Scholar] [CrossRef]
- Haghshenas-Jaryani, M.; Patterson, R.M.; Bugnariu, N.; Wijesundara, M.B. A pilot study on the design and validation of a hybrid exoskeleton robotic device for hand rehabilitation. J. Hand Ther. 2020, 33, 198–208. [Google Scholar] [CrossRef]
- Richardson, W.S.; Wilson, M.C.; Nishikawa, J.; Hayward, R.S. The well-built clinical question: A key to evidence-based decisions. ACP J. Club 1995, 123, 6–8. [Google Scholar] [CrossRef]
- Formicola, R.; Amici, C.; Mor, M.; Bissolotti, L.; Borboni, A. Design of Medical Devices with Usability in Mind: A Theoretical Proposal and Experimental Case Study Using the LEPRE Device. Designs 2023, 7, 9. [Google Scholar] [CrossRef]
- Formicola, R.; Ragni, F.; Borboni, A.; Amici, C. Design Process of Medical Devices for Robotic Rehabilitation: An Open Innovation-Inspired Approach. In Robotics, Machinery and Engineering Technology for Precision Agriculture, Proceedings of XIV International Scientific Conference “INTERAGROMASH 2021”, Rostov-on-Don, Russia, 24–26 February 2021; Smart Innovation, Systems and Technologies; Springer: Berlin/Heidelberg, Germany, 2021; pp. 575–584. [Google Scholar] [CrossRef]
- Noronha, B.; Accoto, D. Exoskeletal Devices for Hand Assistance and Rehabilitation: A Comprehensive Analysis of State-of-the-Art Technologies. IEEE Trans. Med. Robot. Bionics 2021, 3, 525–538. [Google Scholar] [CrossRef]
- Tong, K.; Ho, S.; Pang, P.; Hu, X.; Tam, W.; Fung, K.; Wei, X.; Chen, P.; Chen, M. An intention driven hand functions task training robotic system. In Proceedings of the 2010 Annual International Conference of the IEEE Engineering in Medicine and Biology, Buenos Aires, Argentina, 31 August–4 September 2010; pp. 3406–3409. [Google Scholar]
- Cui, L.; Phan, A.; Allison, G. Design and fabrication of a three dimensional printable non-assembly articulated hand exoskeleton for rehabilitation. In Proceedings of the 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Milan, Italy, 25–29 August 2015; pp. 4627–4630. [Google Scholar]
- Iqbal, J.; Tsagarakis, N.G.; Caldwell, D.G. A multi-DOF robotic exoskeleton interface for hand motion assistance. In Proceedings of the 2011 Annual International Conference of the IEEE Engineering in Medicine and Biology Society, Boston, MA, USA, 30 August–3 September 2011; pp. 1575–1578. [Google Scholar]
- Rahman, M.A.; Al-Jumaily, A. Design and development of a hand exoskeleton for rehabilitation following stroke. Procedia Eng. 2012, 41, 1028–1034. [Google Scholar] [CrossRef]
- Heo, P.; Kim, J. Power-assistive finger exoskeleton with a palmar opening at the fingerpad. IEEE Trans. Biomed. Eng. 2014, 61, 2688–2697. [Google Scholar] [CrossRef] [PubMed]
- Jo, I.; Bae, J. Design and control of a wearable and force-controllable hand exoskeleton system. Mechatronics 2017, 41, 90–101. [Google Scholar] [CrossRef]
- Wang, D.; Meng, Q.; Meng, Q.; Li, X.; Yu, H. Design and development of a portable exoskeleton for hand rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 2376–2386. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; He, B.; Liang, Z.; Zhao, C.G.; Chen, J.; Zhuo, Y.; Xu, G.; Xie, J.; Althoefer, K. An attention-controlled hand exoskeleton for the rehabilitation of finger extension and flexion using a rigid-soft combined mechanism. Front. Neurorobotics 2019, 13, 34. [Google Scholar] [CrossRef] [PubMed]
- Sandison, M.; Phan, K.; Casas, R.; Nguyen, L.; Lum, M.; Pergami-Peries, M.; Lum, P.S. HandMATE: Wearable robotic hand exoskeleton and integrated android app for at home stroke rehabilitation. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020; pp. 4867–4872. [Google Scholar]
- Moreno-SanJuan, V.; Cisnal, A.; Fraile, J.C.; Pérez-Turiel, J.; de-la Fuente, E. Design and characterization of a lightweight underactuated RACA hand exoskeleton for neurorehabilitation. Robot. Auton. Syst. 2021, 143, 103828. [Google Scholar] [CrossRef]
- Dragusanu, M.; Iqbal, M.Z.; Baldi, T.L.; Prattichizzo, D.; Malvezzi, M. Design, development, and control of a hand/wrist exoskeleton for rehabilitation and training. IEEE Trans. Robot. 2022, 38, 1472–1488. [Google Scholar] [CrossRef]
- Tang, T.; Zhang, D.; Xie, T.; Zhu, X. An exoskeleton system for hand rehabilitation driven by shape memory alloy. In Proceedings of the 2013 IEEE International Conference on Robotics and Biomimetics (ROBIO), Shenzhen, China, 12–14 December 2013; pp. 756–761. [Google Scholar]
- Iqbal, J.; Khan, H.; Tsagarakis, N.G.; Caldwell, D.G. A novel exoskeleton robotic system for hand rehabilitation—Conceptualization to prototyping. Biocybern. Biomed. Eng. 2014, 34, 79–89. [Google Scholar] [CrossRef]
- Sandoval-Gonzalez, O.; Jacinto-Villegas, J.; Herrera-Aguilar, I.; Portillo-Rodiguez, O.; Tripicchio, P.; Hernandez-Ramos, M.; Flores-Cuautle, A.; Avizzano, C. Design and development of a hand exoskeleton robot for active and passive rehabilitation. Int. J. Adv. Robot. Syst. 2016, 13, 66. [Google Scholar] [CrossRef]
- Sarakoglou, I.; Brygo, A.; Mazzanti, D.; Hernandez, N.G.; Caldwell, D.G.; Tsagarakis, N.G. Hexotrac: A highly under-actuated hand exoskeleton for finger tracking and force feedback. In Proceedings of the 2016 IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS), Daejeon, Republic of Korea, 9–14 October 2016; pp. 1033–1040. [Google Scholar]
- Esposito, D.; Centracchio, J.; Andreozzi, E.; Savino, S.; Gargiulo, G.D.; Naik, G.R.; Bifulco, P. Design of a 3D-printed hand exoskeleton based on force-myography control for assistance and rehabilitation. Machines 2022, 10, 57. [Google Scholar] [CrossRef]
- De la Cruz-Sánchez, B.A.; Arias-Montiel, M.; Lugo-González, E. EMG-controlled hand exoskeleton for assisted bilateral rehabilitation. Biocybern. Biomed. Eng. 2022, 42, 596–614. [Google Scholar] [CrossRef]
- Tran, P.; Jeong, S.; Herrin, K.R.; Desai, J.P. Review: Hand Exoskeleton Systems, Clinical Rehabilitation Practices, and Future Prospects. IEEE Trans. Med. Robot. Bionics 2021, 3, 606–622. [Google Scholar] [CrossRef]
- Dragusanu, M.; Troisi, D.; Villani, A.; Prattichizzo, D.; Malvezzi, M. Design and Prototyping of an Underactuated Hand Exoskeleton With Fingers Coupled by a Gear-Based Differential. Front. Robot. AI 2022, 9, 862340. [Google Scholar] [CrossRef] [PubMed]
- Conti, R.; Meli, E.; Ridolfi, A. A novel kinematic architecture for portable hand exoskeletons. Mechatronics 2016, 35, 192–207. [Google Scholar] [CrossRef]
- Abdallah, I.B.; Bouteraa, Y.; Rekik, C. Design and development of 3D printed myoelectric robotic exoskeleton for hand rehabilitation. Int. J. Smart Sens. Intell. Syst. 2017, 10, 341–366. [Google Scholar] [CrossRef]
- Jo, I.; Park, Y.; Lee, J.; Bae, J. A portable and spring-guided hand exoskeleton for exercising flexion/extension of the fingers. Mech. Mach. Theory 2019, 135, 176–191. [Google Scholar] [CrossRef]
- Secciani, N.; Brogi, C.; Pagliai, M.; Buonamici, F.; Gerli, F.; Vannetti, F.; Bianchini, M.; Volpe, Y.; Ridolfi, A. Wearable robots: An original mechatronic design of a hand exoskeleton for assistive and rehabilitative purposes. Front. Neurorobotics 2021, 15, 750385. [Google Scholar] [CrossRef]
- Bartalucci, L.; Secciani, N.; Brogi, C.; Topini, A.; Della Valle, A.; Ridolfi, A.; Allotta, B. An original mechatronic design of a kinaesthetic hand exoskeleton for virtual reality-based applications. Mechatronics 2023, 90, 102947. [Google Scholar] [CrossRef]
- Cempini, M.; Cortese, M.; Vitiello, N. A powered finger–thumb wearable hand exoskeleton with self-aligning joint axes. IEEE/ASME Trans. Mechatron. 2014, 20, 705–716. [Google Scholar] [CrossRef]
- Bataller, A.; Cabrera, J.; Clavijo, M.; Castillo, J. Evolutionary synthesis of mechanisms applied to the design of an exoskeleton for finger rehabilitation. Mech. Mach. Theory 2016, 105, 31–43. [Google Scholar] [CrossRef]
- Malvezzi, M.; Baldi, T.L.; Villani, A.; Ciccarese, F.; Prattichizzo, D. Design, development, and preliminary evaluation of a highly wearable exoskeleton. In Proceedings of the 2020 29th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN), Virtual, 31 August–4 September 2020; pp. 1055–1062. [Google Scholar]
- Schiele, A.; Van Der Helm, F.C. Kinematic design to improve ergonomics in human machine interaction. IEEE Trans. Neural Syst. Rehabil. Eng. 2006, 14, 456–469. [Google Scholar] [CrossRef]
- Marconi, D.; Baldoni, A.; McKinney, Z.; Cempini, M.; Crea, S.; Vitiello, N. A novel hand exoskeleton with series elastic actuation for modulated torque transfer. Mechatronics 2019, 61, 69–82. [Google Scholar] [CrossRef]
- Lambercy, O.; Schröder, D.; Zwicker, S.; Gassert, R. Design of a thumb exoskeleton for hand rehabilitation. In Proceedings of the 7th International Convention on Rehabilitation Engineering and Assistive Technology, Singapore, 29–31 August 2013; p. 41. [Google Scholar]
- Dragusanu, M.; Iqbal, Z.; Prattichizzo, D.; Malvezzi, M. Design of a modular hand exoskeleton for rehabilitation and training. In Proceedings of the ASME International Mechanical Engineering Congress and Exposition. American Society of Mechanical Engineers, Virtual, 1–5 November 2021; Volume 85598, p. V005T05A067. [Google Scholar]
- Schabowsky, C.N.; Godfrey, S.B.; Holley, R.J.; Lum, P.S. Development and pilot testing of HEXORR: Hand EXOskeleton rehabilitation robot. J. Neuroeng. Rehabil. 2010, 7, 1–16. [Google Scholar] [CrossRef] [PubMed]
- In, H.; Cho, K.J.; Kim, K.; Lee, B. Jointless structure and under-actuation mechanism for compact hand exoskeleton. In Proceedings of the 2011 IEEE International Conference on Rehabilitation Robotics, Zurich, Switzerland, 29 June–1 July 2011; pp. 1–6. [Google Scholar]
- Valero-Cuevas, F.J.; Johanson, M.E.; Towles, J.D. Towards a realistic biomechanical model of the thumb: The choice of kinematic description may be more critical than the solution method or the variability/uncertainty of musculoskeletal parameters. J. Biomech. 2003, 36, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Santello, M.; Flanders, M.; Soechting, J.F. Postural hand synergies for tool use. J. Neurosci. 1998, 18, 10105–10115. [Google Scholar] [CrossRef]
- Taylor-Schroeder, S.; LaBarbera, J.; McDowell, S.; Zanca, J.M.; Natale, A.; Mumma, S.; Gassaway, J.; Backus, D. Physical therapy treatment time during inpatient spinal cord injury rehabilitation. J. Spinal Cord Med. 2011, 34, 149–161. [Google Scholar] [CrossRef]
- Natale, A.; Taylor, S.; LaBarbera, J.; Bensimon, L.; McDowell, S.; Mumma, S.L.; Backus, D.; Zanca, J.M.; Gassaway, J. SCIRehab Project series: The physical therapy taxonomy. J. Spinal Cord Med. 2009, 32, 270–282. [Google Scholar] [CrossRef]
- Bosch, T.; van Eck, J.; Knitel, K.; de Looze, M. The effects of a passive exoskeleton on muscle activity, discomfort and endurance time in forward bending work. Appl. Ergon. 2016, 54, 212–217. [Google Scholar] [CrossRef]
- Pirondini, E.; Coscia, M.; Marcheschi, S.; Roas, G.; Salsedo, F.; Frisoli, A.; Bergamasco, M.; Micera, S. Evaluation of the effects of the Arm Light Exoskeleton on movement execution and muscle activities: A pilot study on healthy subjects. J. Neuroeng. Rehabil. 2016, 13, 9. [Google Scholar] [CrossRef]
- Topini, A.; Sansom, W.; Secciani, N.; Bartalucci, L.; Ridolfi, A.; Allotta, B. Variable admittance control of a hand exoskeleton for virtual reality-based rehabilitation tasks. Front. Neurorobotics 2022, 15, 789743. [Google Scholar] [CrossRef]
- Abras, C.; Maloney-Krichmar, D.; Preece, J. User-Centered Design; Sage Publications: Thousand Oaks, CA, USA, 2004; Volume 37, pp. 445–456. [Google Scholar]
- Lehoux, P.; Grimard, D. When robots care: Public deliberations on how technology and humans may support independent living for older adults. Soc. Sci. Med. 2018, 211, 330–337. [Google Scholar] [CrossRef]
- Östlund, B.; Malvezzi, M.; Frennert, S.; Funk, M.; Gonzalez-Vargas, J.; Baur, K.; Alimisis, D.; Thorsteinsson, F.; Alonso-Cepeda, A.; Fau, G.; et al. Interactive robots for health in Europe: Technology readiness and adoption potential. Front. Public Health 2023, 11, 979225. [Google Scholar] [CrossRef] [PubMed]
- Tiboni, M.; Amici, C. Soft Gloves: A Review on Recent Developments in Actuation, Sensing, Control, and Applications. Actuators 2022, 11, 232. [Google Scholar] [CrossRef]
- Tiboni, M.; Loda, D. Monolithic PneuNets Soft Actuators for Robotic Rehabilitation: Methodologies for Design, Production and Characterization. Actuators 2023, 12, 299. [Google Scholar] [CrossRef]
- Cappello, L.; Meyer, J.T.; Galloway, K.C.; Peisner, J.D.; Granberry, R.; Wagner, D.A.; Engelhardt, S.; Paganoni, S.; Walsh, C.J. Assisting hand function after spinal cord injury with a fabric-based soft robotic glove. J. Neuroeng. Rehabil. 2018, 15, 59. [Google Scholar] [CrossRef] [PubMed]
- Elmoughni, H.M.; Yilmaz, A.F.; Ozlem, K.; Khalilbayli, F.; Cappello, L.; Tuncay Atalay, A.; Ince, G.; Atalay, O. Machine-Knitted Seamless Pneumatic Actuators for Soft Robotics: Design, Fabrication, and Characterization. Actuators 2021, 10, 94. [Google Scholar] [CrossRef]
- Polygerinos, P.; Wang, Z.; Galloway, K.C.; Wood, R.J.; Walsh, C.J. Soft robotic glove for combined assistance and at-home rehabilitation. Robot. Auton. Syst. 2015, 73, 135–143. [Google Scholar] [CrossRef]
- Tiboni, M.; Borboni, A.; Vérité, F.; Bregoli, C.; Amici, C. Sensors and Actuation Technologies in Exoskeletons: A Review. Sensors 2022, 22, 884. [Google Scholar] [CrossRef]
- Polygerinos, P.; Lyne, S.; Wang, Z.; Nicolini, L.F.; Mosadegh, B.; Whitesides, G.M.; Walsh, C.J. Towards a soft pneumatic glove for hand rehabilitation. In Proceedings of the 2013 IEEE/RSJ International Conference on Intelligent Robots and Systems, Tokyo, Japan, 3–7 November 2013; pp. 1512–1517. [Google Scholar] [CrossRef]
- Wang, X.; Cheng, Y.; Zheng, H.; Li, Y.; Wang, C. Design and optimization of actuator for multi-joint soft rehabilitation glove. Ind. Robot 2021, 48, 877–890. [Google Scholar] [CrossRef]
- Chen, Y.; Yang, Z.; Wen, Y. A soft exoskeleton glove for hand bilateral training via surface EMG. Sensors 2021, 21, 578. [Google Scholar] [CrossRef]
- Do, P.T.; Vo, D.T.; Le, H.P. A Soft Pneumatic Robotic Glove for Hand Rehabilitation after Stroke. In Proceedings of the 20th International Conference on Advanced Robotics (ICAR), Ljubljana, Slovenia, 6–10 December 2021; pp. 7–12. [Google Scholar] [CrossRef]
- Li, M.; Wang, T.; Zhuo, Y.; He, B.; Tao, T.; Xie, J.; Xu, G. A soft robotic glove for hand rehabilitation training controlled by movements of the healthy hand. In Proceedings of the 17th International Conference on Ubiquitous Robots (UR), Kyoto, Japan, 22–26 June 2020; pp. 62–67. [Google Scholar] [CrossRef]
- Souhail, A.; Vessakosol, P. Low cost soft robotic gloves for at-home rehabilitation and daily living activities. J. Autom. Mob. Robot. Intell. Syst. 2019, 13, 14–26. [Google Scholar] [CrossRef]
- Jiang, Y.; Chen, D.; Que, J.; Liu, Z.; Wang, Z.; Xu, Y. Soft robotic glove for hand rehabilitation based on a novel fabrication method. In Proceedings of the 2017 IEEE International Conference on Robotics and Biomimetics, ROBIO 2017, Macau, Macao, 5–8 December 2017; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2017; pp. 817–822. [Google Scholar] [CrossRef]
- Jadhav, S.; Kannanda, V.; Kang, B.; Tolley, M.T.; Schulze, J.P. Soft robotic glove for kinesthetic haptic feedback in virtual reality environments. Electron. Imaging 2017, 2017, 19–24. [Google Scholar] [CrossRef]
- Jiralerspong, T.; Heung, K.H.; Tong, R.K.; Li, Z. A Novel Soft Robotic Glove for Daily Life Assistance. In Proceedings of the 7th IEEE International Conference on Biomedical Robotics and Biomechatronics (Biorob), Enschede, The Netherlands, 26–29 August 2018; pp. 671–676. [Google Scholar] [CrossRef]
- Jumphoo, T.; Uthansakul, M.; Duangmanee, P.; Khan, N.; Uthansakul, P. Soft robotic glove controlling using brainwave detection for continuous rehabilitation at home. Comput. Mater. Contin. 2021, 66, 961–976. [Google Scholar] [CrossRef]
- Gerges, F.; Desai, J.; Watkins, J.; Burugupally, S.P. Master-Slave Control for a Pneumatically Actuated Low Pressure Soft Robotic Glove to Facilitate Bilateral Training for Stroke Patients. In Proceedings of the 2020 23rd IEEE International Symposium on Measurement and Control in Robotics, ISMCR 2020, Budapest, Hungary, 15–17 October 2020; Kiss, B., Harmati, I.T.Z., Eds.; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020; pp. 1–6. [Google Scholar] [CrossRef]
- Hu, D.; Zhang, J.; Yang, Y.; Li, Q.; Li, D.; Hong, J. A novel soft robotic glove with positive-negative pneumatic actuator for hand rehabilitation. In Proceedings of the 2020 IEEE/ASME International Conference on Advanced Intelligent Mechatronics (AIM), Virtual, 6–9 July 2020; pp. 1840–1847. [Google Scholar] [CrossRef]
- Guo, N.; Sun, Z.; Wang, X.; Yeung, E.H.K.; To, M.K.T.; Li, X.; Hu, Y. Simulation analysis for optimal design of pneumatic bellow actuators for soft-robotic glove. Biocybern. Biomed. Eng. 2020, 40, 1359–1368. [Google Scholar] [CrossRef]
- Ge, L.; Chen, F.; Wang, D.; Zhang, Y.; Han, D.; Wang, T.; Gu, G. Design, Modeling, and Evaluation of Fabric-Based Pneumatic Actuators for Soft Wearable Assistive Gloves. Soft Robot. 2020, 7, 583–596. [Google Scholar] [CrossRef]
- Feng, M.; Yang, D.; Gu, G. High-Force Fabric-Based Pneumatic Actuators with Asymmetric Chambers and Interference-Reinforced Structure for Soft Wearable Assistive Gloves. IEEE Robot. Autom. Lett. 2021, 6, 3105–3111. [Google Scholar] [CrossRef]
- Yap, H.K.; Khin, P.M.; Koh, T.H.; Sun, Y.; Liang, X.; Lim, J.H.; Yeow, C.H. A Fully Fabric-Based Bidirectional Soft Robotic Glove for Assistance and Rehabilitation of Hand Impaired Patients. IEEE Robot. Autom. Lett. 2017, 2, 1383–1390. [Google Scholar] [CrossRef]
- Koizumi, S.; Chang, T.H.; Nabae, H.; Endo, G.; Suzumori, K.; Mita, M.; Saitoh, K.; Hatakeyama, K.; Chida, S.; Shimada, Y. Soft Robotic Gloves with Thin McKibben Muscles for Hand Assist and Rehabilitation. In Proceedings of the 2020 IEEE/SICE International Symposium on System Integration (SII), Honolulu, HI, USA, 12–15 January 2020; pp. 93–98. [Google Scholar] [CrossRef]
- Cao, X.; Ma, K.; Jiang, Z.; Xu, F. A Soft Robotic Glove for Hand Rehabilitation using Pneumatic Actuators with Jamming Structure. In Proceedings of the 40th Chinese Control Conference (CCC), Shanghai, China, 26–28 July 2021; pp. 4120–4125. [Google Scholar] [CrossRef]
- Yap, H.K.; Kamaldin, N.; Lim, J.H.; Nasrallah, F.A.; Goh, J.C.H.; Yeow, C.H. A Magnetic Resonance Compatible Soft Wearable Robotic Glove for Hand Rehabilitation and Brain Imaging. IEEE Trans. Neural Syst. Rehabil. Eng. 2017, 25, 782–793. [Google Scholar] [CrossRef]
- Du, Q.; Zhao, W.; Cui, X.; Fei, Y. Design, control and testing of soft pneumatic rehabilitation glove. In Proceedings of the 2020 3rd World Conference on Mechanical Engineering and Intelligent Manufacturing, WCMEIM 2020, Shanghai, China, 4–6 December 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020; pp. 50–55. [Google Scholar] [CrossRef]
- Heung, K.H.L.; Tong, R.K.Y.; Lau, A.T.H.; Li, Z. Robotic Glove with Soft-Elastic Composite Actuators for Assisting Activities of Daily Living. Soft Robot. 2019, 6, 289–304. [Google Scholar] [CrossRef]
- Wang, J.; Liu, Z.; Fei, Y. Design and testing of a soft rehabilitation glove integrating finger and wrist function. J. Mech. Robot. 2019, 11, 011015. [Google Scholar] [CrossRef]
- Ang, B.W.K.; Yeow, C.H. Print-it-Yourself (PIY) glove: A fully 3D printed soft robotic hand rehabilitative and assistive exoskeleton for stroke patients. In Proceedings of the IEEE International Conference on Intelligent Robots and Systems, Vancouver, BC, Canada, 24–28 September 2017; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2017; pp. 1219–1223. [Google Scholar] [CrossRef]
- Yap, H.K.; Lim, J.H.; Nasrallah, F.; Yeow, C.H. Design and preliminary feasibility study of a soft robotic glove for hand function assistance in stroke survivors. Front. Neurosci. 2017, 11, 547. [Google Scholar] [CrossRef]
- Haghshenas-Jaryani, M.; Carrigan, W.; Nothnagle, C.; Wijesundara, M.B.J. Sensorized soft robotic glove for continuous passive motion therapy. In Proceedings of the IEEE RAS and EMBS International Conference on Biomedical Robotics and Biomechatronics, Singapore, 26–29 June 2016; IEEE Computer Society: Piscataway, NJ, USA, 2016; pp. 815–820. [Google Scholar] [CrossRef]
- Yap, H.K.; Ang, B.W.K.; Lim, J.H.; Goh, J.C.H.; Yeow, C.H. A fabric-regulated soft robotic glove with user intent detection using EMG and RFID for hand assistive application. In Proceedings of the IEEE International Conference on Robotics and Automation. Institute of Electrical and Electronics Engineers, Stockholm, Sweden, 16–21 May 2016; pp. 3537–3542. [Google Scholar] [CrossRef]
- Yap, H.K.; Lim, J.H.; Nasrallah, F.; Low, F.Z.; Goh, J.C.H.; Yeow, R.C.H. MRC-glove: A fMRI compatible soft robotic glove for hand rehabilitation application. In Proceedings of the IEEE International Conference on Rehabilitation Robotics, Singapore, 1–14 August 2015; Yu, H., Braun, D.C.D., Eds.; IEEE Computer Society: Piscataway, NJ, USA, 2015; pp. 735–740. [Google Scholar] [CrossRef]
- Wang, J.; Fei, Y.; Pang, W. Design, Modeling, and Testing of a Soft Pneumatic Glove with Segmented PneuNets Bending Actuators. IEEE/ASME Trans. Mechatron. 2019, 24, 990–1001. [Google Scholar] [CrossRef]
- Radder, B.; Prange-Lasonder, G.B.; Kottink, A.I.R.; Gaasbeek, L.; Holmberg, J.; Meyer, T.; Buurke, J.H.; Rietman, J.S. Preliminary findings of feasibility of a wearable soft-robotic glove supporting impaired hand function in daily life: A soft-robotic glove supporting adl of elderly people. In Proceedings of the ICT4AWE 2016—2nd International Conference on Information and Communication Technologies for Ageing Well and e-Health, Proceedings, Rome, Italy, 21–22 April 2016; Rocker, C., Ziefle, M., O’Donoghue, J., Helfert, M., Molloy, W., Eds.; SciTePress: Setúbal Municipality, Portugal, 2016; pp. 180–185. [Google Scholar] [CrossRef]
- Radder, B.; Prange-Lasonder, G.B.; Kottink, A.I.R.; Gaasbeek, L.; Sletta, K.; Holmberg, J.; Meyer, T.; Buurke, J.H.; Rietman, J.S. Preliminary Evaluation of a Wearable Soft-Robotic Glove Supporting Grip Strength in ADL. Biosyst. Biorobotics 2017, 15, 1245–1250. [Google Scholar] [CrossRef]
- Radder, B.; Prange-Lasonder, G.B.; Kottink, A.I.R.; Melendez-Calderon, A.; Buurke, J.H.; Rietman, J.S. Feasibility of a wearable soft-robotic glove to support impaired hand function in stroke patients. J. Rehabil. Med. 2018, 50, 598–606. [Google Scholar] [CrossRef] [PubMed]
- Amici, C.; Ragni, F.; Ghidoni, M.; Fausti, D.; Bissolotti, L.; Tiboni, M. Multi-sensor validation approach of an end-effector-based robot for the rehabilitation of the upper and lower limb. Electronics 2020, 9, 1751. [Google Scholar] [CrossRef]
- Palmcrantz, S.; Plantin, J.; Borg, J. Factors affecting the usability of an assistive soft robotic glove after stroke or multiple sclerosis. J. Rehabil. Med. 2020, 52, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Osuagwu, B.A.; Timms, S.; Peachment, R.; Dowie, S.; Thrussell, H.; Cross, S.; Heywood, T.; Shirley, R.; Taylor, J. Clinical trial of the soft extra muscle glove to assess orthotic and long-term functional gain following chronic incomplete tetraplegia: Preliminary functional results. Biosyst. Biorobotics 2019, 21, 385–389. [Google Scholar] [CrossRef]
- Osuagwu, B.A.C.; Timms, S.; Peachment, R.; Dowie, S.; Thrussell, H.; Cross, S.; Shirley, R.; Segura-Fragoso, A.; Taylor, J. Home-based rehabilitation using a soft robotic hand glove device leads to improvement in hand function in people with chronic spinal cord injury:a pilot study. J. Neuroeng. Rehabil. 2020, 17, 40. [Google Scholar] [CrossRef]
- Nilsson, M.; Ingvast, J.; Wikander, J.; von Holst, H. The Soft Extra Muscle system for improving the grasping capability in neurological rehabilitation. In Proceedings of the 2012 IEEE-EMBS Conference on Biomedical Engineering and Sciences, Langkawi, Malaysia, 17–19 December 2012; pp. 412–417. [Google Scholar] [CrossRef]
- Takahashi, N.; Takahashi, H.; Koike, H. Soft Exoskeleton Glove Enabling Force Feedback for Human-Like Finger Posture Control with 20 Degrees of Freedom. In Proceedings of the 2019 IEEE World Haptics Conference (WHC), Tokyo, Japan, 9–12 July 2019; pp. 217–222. [Google Scholar] [CrossRef]
- Tiboni, M.; Legnani, G.; Lancini, M.; Serpelloni, M.; Gobbo, M.; Fausti, D. ERRSE: Elbow robotic rehabilitation system with an EMG-based force control. Mech. Mach. Sci. 2018, 49, 892–900. [Google Scholar] [CrossRef]
- Sierotowicz, M.; Lotti, N.; Nell, L.; Missiroli, F.; Alicea, R.; Zhang, X.; Xiloyannis, M.; Rupp, R.; Papp, E.; Krzywinski, J.; et al. EMG-Driven Machine Learning Control of a Soft Glove for Grasping Assistance and Rehabilitation. IEEE Robot. Autom. Lett. 2022, 7, 1566–1573. [Google Scholar] [CrossRef]
- Serpelloni, M.; Tiboni, M.; Lancini, M.; Pasinetti, S.; Vertuan, A.; Gobbo, M.; Meccanica, I.; Brescia, U. Preliminary Study of a Robotic Rehabilitation System Driven by EMG for Hand Mirroring. In Proceedings of the 2016 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Benevento, Italy, 15–18 May 2016; pp. 1–5. [Google Scholar]
- Zhu, Y.; Gong, W.; Chu, K.; Wang, X.; Hu, Z.; Su, H. A Novel Wearable Soft Glove for Hand Rehabilitation and Assistive Grasping. Sensors 2022, 22, 6294. [Google Scholar] [CrossRef]
- Demolder, C.; Molina, A.; Hammond, F.L.; Yeo, W.H. Recent advances in wearable biosensing gloves and sensory feedback biosystems for enhancing rehabilitation, prostheses, healthcare, and virtual reality. Biosens. Bioelectron. 2021, 190, 113443. [Google Scholar] [CrossRef] [PubMed]
- Burns, M.K.; Vinjamuri, R. Design of a Soft Glove-Based Robotic Hand Exoskeleton with Embedded Synergies; Springer International Publishing: Berlin/Heidelberg, Germany, 2020; pp. 71–87. [Google Scholar] [CrossRef]
- Yavuzer, G.; Selles, R.; Sezer, N.; Sütbeyaz, S.; Bussmann, J.B.; Köseoǧlu, F.; Atay, M.B.; Stam, H.J. Mirror Therapy Improves Hand Function in Subacute Stroke: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2008, 89, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Chun Li, Y.; Chung Lin, K.; ling Chen, C.; Yao, G.; Ya-ju, C.; yun Lee, Y.; ting Liu, C.; Chen, W.S. Three Ways to Improve Arm Function in the Chronic Phase After Stroke by Robotic Priming Combined With Mirror Therapy, Arm Training, and Movement-Oriented Therapy. Arch. Phys. Med. Rehabil. 2023, 104, 1195–1202. [Google Scholar] [CrossRef]
- Chen, X.; Gong, L.; Zheng, L.; Zou, Z. Soft Exoskeleton Glove for Hand Assistance Based on Human-machine Interaction and Machine Learning. In Proceedings of the 2020 IEEE International Conference on Human-Machine Systems, ICHMS 2020, Rome, Italy, 7–9 September 2020; Institute of Electrical and Electronics Engineers Inc.: Piscataway, NJ, USA, 2020. [Google Scholar] [CrossRef]
- Yun, S.S.; Kang, B.B.; Cho, K.J. Exo-glove PM: An easily customizable modularized pneumatic assistive glove. IEEE Robot. Autom. Lett. 2017, 2, 1725–1732. [Google Scholar] [CrossRef]
- Connelly, L.; Jia, Y.; Toro, M.L.; Stoykov, M.E.; Kenyon, R.V.; Kamper, D.G. A pneumatic glove and immersive virtual reality environment for hand rehabilitative training after stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 551–559. [Google Scholar] [CrossRef]
- Polygerinos, P.; Galloway, K.C.; Sanan, S.; Herman, M.; Walsh, C.J. EMG controlled soft robotic glove for assistance during activities of daily living. In Proceedings of the IEEE International Conference on Rehabilitation Robotics, Singapore, 11–14 August 2015; Yu, H., Braun, D.C.D., Eds.; IEEE Computer Society: Piscataway, NJ, USA, 2015; pp. 55–60. [Google Scholar] [CrossRef]
- Arata, J.; Ohmoto, K.; Gassert, R.; Lambercy, O.; Fujimoto, H.; Wada, I. A new hand exoskeleton device for rehabilitation using a three-layered sliding spring mechanism. In Proceedings of the 2013 IEEE International Conference on Robotics and Automation, Karlsruhe, Germany, 6–10 May 2013; pp. 3902–3907. [Google Scholar]
- Kladovasilakis, N.; Kostavelis, I.; Sideridis, P.; Koltzi, E.; Piliounis, K.; Tzetzis, D.; Tzovaras, D. A Novel Soft Robotic Exoskeleton System for Hand Rehabilitation and Assistance Purposes. Appl. Sci. 2022, 13, 553. [Google Scholar] [CrossRef]
- Achilli, G.M.; Logozzo, S.; Valigi, M.C.; Dragusanu, M.; Malvezzi, M. Theoretical and experimental characterization of a new robotic gripper’s joint. In Advances in Italian Mechanism Science, Proceedings of the 4th International Conference of IFToMM Italy, Napoli, Italy, 7–9 September 2022; Springer: Berlin/Heidelberg, Germany, 2022; pp. 738–745. [Google Scholar]
- Serbest, K.; Eldoğan, O. Design, development and evaluation of a new hand exoskeleton for stroke rehabilitation at home. Politek. Derg. 2020, 24, 305–314. [Google Scholar] [CrossRef]
- Li, G.; Cheng, L.; Sun, N. Design, manipulability analysis and optimization of an index finger exoskeleton for stroke rehabilitation. Mech. Mach. Theory 2022, 167, 104526. [Google Scholar] [CrossRef]
- Achilli, G.M.; Logozzo, S.; Malvezzi, M.; Prattichizzo, D.; Salvietti, G.; Valigi, M. Characterization of finger joints with underactuated modular structure. Theor. Appl. Mech. AIMETA 2022 2023, 26, 201. [Google Scholar]
- Bützer, T.; Lambercy, O.; Arata, J.; Gassert, R. Fully wearable actuated soft exoskeleton for grasping assistance in everyday activities. Soft Robot. 2021, 8, 128–143. [Google Scholar] [CrossRef]
- Vertongen, J.; Kamper, D. Design of a 3D printed hybrid mechanical structure for a hand exoskeleton. Curr. Dir. Biomed. Eng. 2020, 6, 20202003. [Google Scholar] [CrossRef]
- Wang, Z.; Wang, D.; Zhang, Y.; Liu, J.; Wen, L.; Xu, W.; Zhang, Y. A three-fingered force feedback glove using fiber-reinforced soft bending actuators. IEEE Trans. Ind. Electron. 2019, 67, 7681–7690. [Google Scholar] [CrossRef]
- Rose, C.G.; O’Malley, M.K. Hybrid rigid-soft hand exoskeleton to assist functional dexterity. IEEE Robot. Autom. Lett. 2018, 4, 73–80. [Google Scholar] [CrossRef]
- Randazzo, L.; Iturrate, I.; Perdikis, S.; Millán, J.d.R. mano: A wearable hand exoskeleton for activities of daily living and neurorehabilitation. IEEE Robot. Autom. Lett. 2017, 3, 500–507. [Google Scholar] [CrossRef]
- Logozzo, S.; Valigi, M.C.; Malvezzi, M. Modelling the human touch: A basic study for haptic technology. Tribol. Int. 2022, 166, 107352. [Google Scholar] [CrossRef]
- Achilli, G.M.; Logozzo, S.; Malvezzi, M.; Valigi, M.C. Contact mechanics analysis of a soft robotic fingerpad. Front. Mech. Eng. 2022, 8, 966335. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).