Characterization of Pterygomaxillary Suture Morphology: A CBCT Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Sample
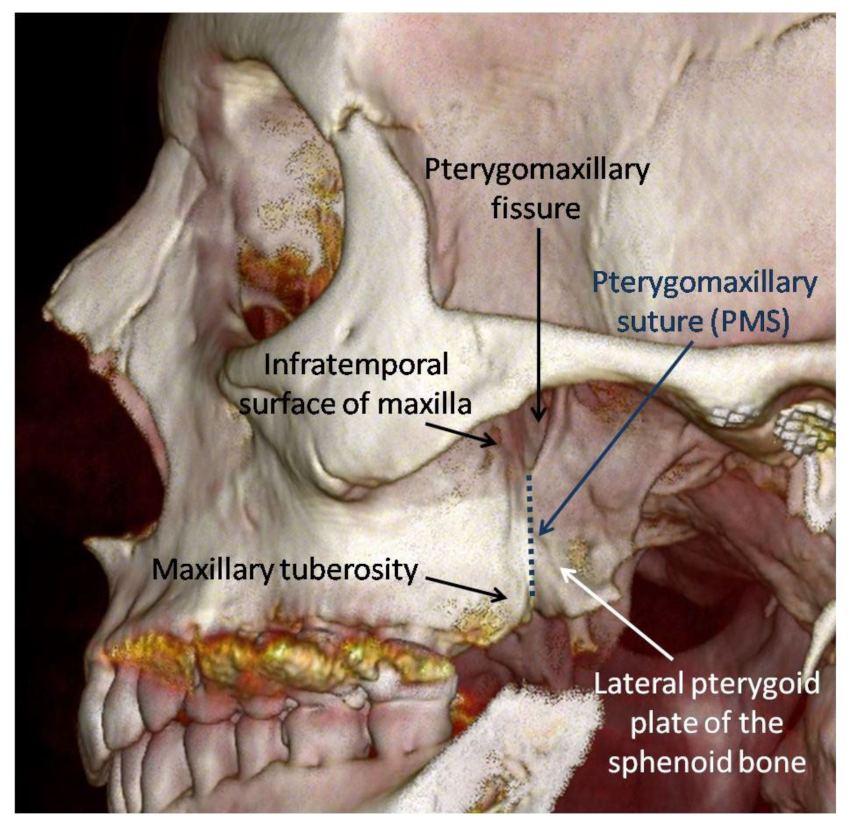
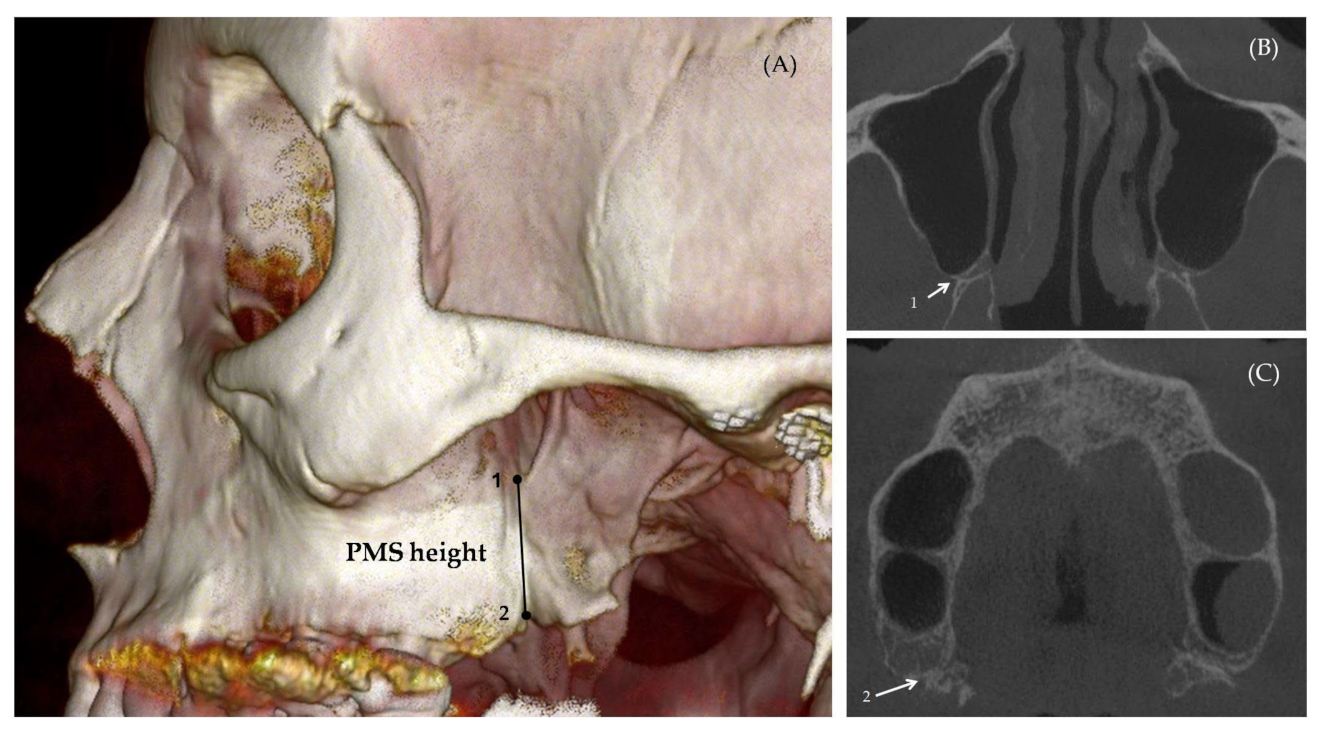
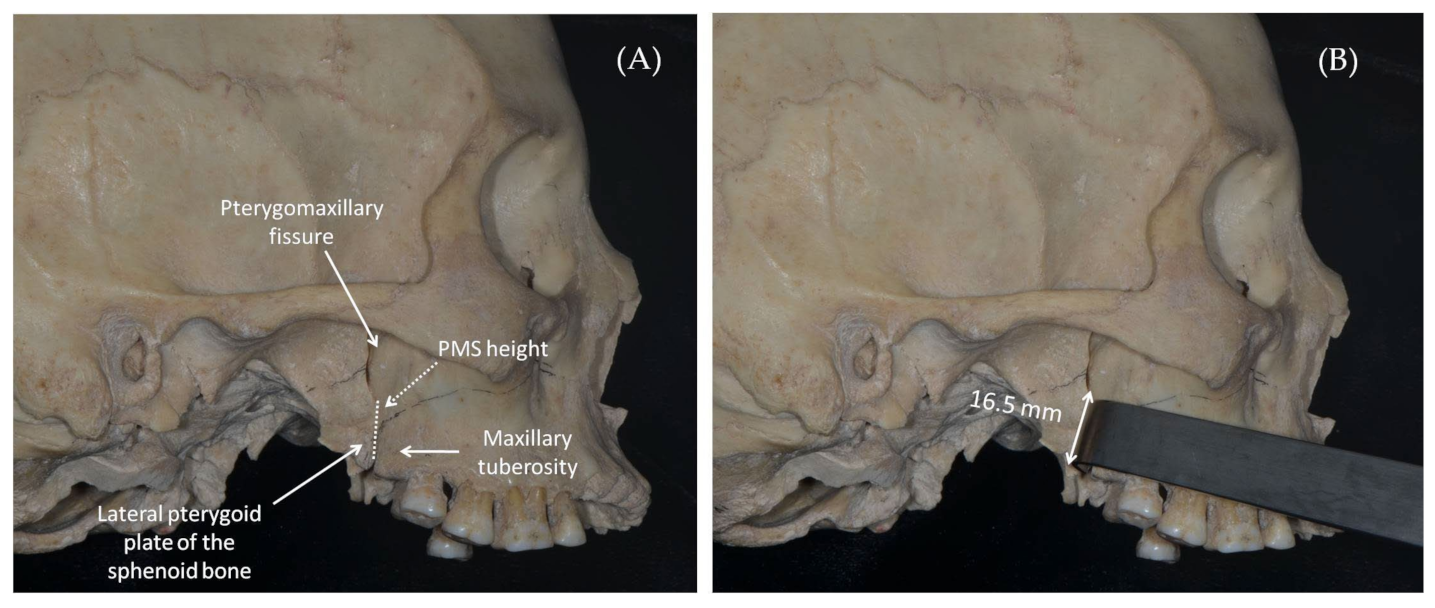
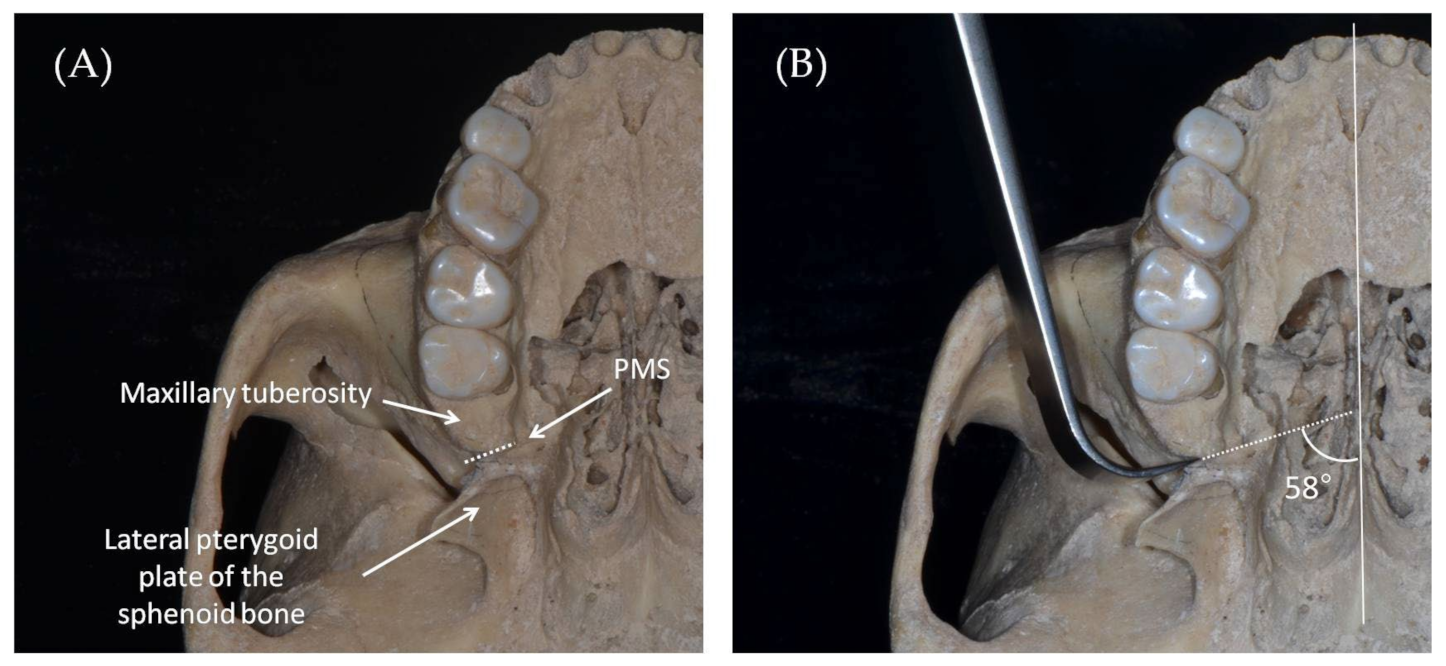
2.2. Measurement Method
- PMS thickness (mm): The maximal distance measured between the innermost points on the lateral concave and medial convex surfaces of the suture (Figure 3). The axial cross section in which the PMS thickness was greatest was evaluated separately for each side since the height of this section could vary slightly between the right and left sides of the same patient, depending on the anatomical differences between the sides.
- PMS angulation (°): The angle created between the PMS thickness line and the midsagittal plane (Figure 3).
- PMS height (mm): The suture height was calculated based on the number of axial sections counted from the suture initiation (the section where the maxillary lump connects to the pterygoid hamulus) and the suture termination (the last section before the suture is opened into a pterygomaxillary fissure) multiplied by the slice thickness (Figure 4).
2.3. Statistical Analysis
2.4. Reliability
3. Results
3.1. Reliability Test
3.2. Study Sample
3.3. PMS Morphology by the Right and Left Sides in Males and Females
3.4. Comparison of the PMS Morphology between the Sexes
3.5. PMS Morphology and Age by Sexes
4. Discussion
5. Limitations of the Study
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moore, U.J. Surgical Principles and Technique. In Principles of Oral and Maxillofacial Surgery, 6th ed.; John Wiley & Sons Ltd.: Hoboken, NJ, USA; Wiley-Blackwell: New York, NY, USA, 2011; pp. 87–105. [Google Scholar]
- Susarla, S.M.; Ettinger, R.E.; Egbert, M.A. Transmucosal pterygomaxillary separation in the Le Fort I osteotomy. Plast. Reconstr. Surg. 2020, 145, 1262–1265. [Google Scholar] [CrossRef] [PubMed]
- Naini, F.B.; Gill, D.S. Orthognathic Surgery Principles, Planning and Practice, 1st ed.; John Wiley & Sons Ltd.: West Sussex, UK, 2017. [Google Scholar]
- Fehrenbach, M.J.; Herring, S.W. Illustrated Anatomy of the Head and Neck-E-Book, 5th ed.; Elsevier Health Sciences: Amsterdam, The Netherlands, 2015. [Google Scholar]
- Osborn, A.G. Radiology of the pterygoid plates and pterygopalatine fossa. AJR Am. J. Roentgenol. 1979, 132, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Tashi, S.; Purohit, B.S.; Becker, M.; Mundada, P. The pterygopalatine fossa: Imaging anatomy, communications, and pathology revisited. Insights Imaging 2016, 7, 589–599. [Google Scholar] [CrossRef]
- Cheung, L.K.; Fung, S.C.; Li, T.; Samman, N. Posterior maxillary anatomy: Implications for Le Fort I osteotomy. Int. J. Oral Maxillofac. Surg. 1998, 27, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Odabaşı, O.; Erkmen, E.; Üçok, C.Ö.; Bakir, M.A.; Keriş, E.Y.; Şahin, O. Morphometric analysis of pterygomaxillary region by using cone beam computed tomography. J. Stomatol. Oral Maxillofac. Surg. 2021, 122, 273–277. [Google Scholar] [CrossRef]
- Turvey, T.A.; Fonseca, R.J. The anatomy of the internal maxillary artery in the pterygopalatine fossa: Its relationship to maxillary surgery. J. Oral Surg. 1980, 38, 92–95. [Google Scholar]
- Lanigan, D.T.; West, R.A. Management of postoperative hemorrhage following the Le Fort I maxillary osteotomy. J. Oral Maxillofac. Surg. 1984, 42, 367–375. [Google Scholar] [CrossRef]
- Lanigan, D.T.; Hey, J.H.; West, R.A. Major vascular complications of orthognathic surgery: Hemorrhage associated with Le Fort I osteotomies. J. Oral Maxillofac. Surg. 1990, 48, 561–573. [Google Scholar] [CrossRef]
- Wikkeling, O.M.; Tacoma, J. Osteotomy of the pterygomaxillary junction. Int. J. Oral Surg. 1975, 4, 99–103. [Google Scholar] [CrossRef]
- Politis, C. Life-threatening haemorrhage after 750 Le Fort I osteotomies and 376 SARPE procedures. Int. J. Oral Maxillofac. Surg. 2012, 41, 702–708. [Google Scholar] [CrossRef]
- Zaroni, F.M.; Cavalcante, R.C.; da Costa, D.J.; Kluppel, L.E.; Scariot, R.; Rebellato, N.L.B. Complications associated with orthognathic surgery: A retrospective study of 485 cases. J. Maxillofac. Surg. 2019, 47, 1855–1860. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P.P.; Hendy, C.W. Pterygoid plate fractures caused by the Le Fort I osteotomy. Br. J. Oral Maxillofac. Surg. 1986, 24, 198–202. [Google Scholar] [CrossRef] [PubMed]
- Tung, T.C.; Chen, Y.R.; Bendor-Samuel, R. Surgical complications of the Le Fort I osteotomy-a retrospective review of 146 cases. Changgeng Yi Xue Za Zhi. 1995, 18, 102–107. [Google Scholar] [PubMed]
- Chin, Y.P.; Leno, M.B.; Dumrongwongsiri, S.; Chung, K.H.; Lin, H.H.; Lo, L.J. The pterygomaxillary junction: An imaging study for surgical information of Le Fort I osteotomy. Sci. Rep. 2017, 7, 9953. [Google Scholar] [CrossRef] [Green Version]
- Bilge, S.; Kaba, Y.N.; Demirbas, A.E.; Kütük, N.; Kiliç, E.; Alkan, A. Evaluation of the pterygomaxillary separation pattern in Le Fort I osteotomy using different cutting instruments. J. Oral Maxillofac. Surg. 2020, 78, 1820–1831. [Google Scholar] [CrossRef]
- Precious, D.S.; Morrison, A.; Ricard, D. Pterygomaxillary separation without the use of an osteotome. J. Oral Maxillofac. Surg. 1991, 49, 98–99. [Google Scholar] [CrossRef]
- Dupont, C.; Ciaburro, T.H.; Prévost, Y. Simplifying the Le Fort I type of maxillary osteotomy. Plast. Reconstr. Surg. 1974, 54, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Trimble, L.D.; Tideman, H.; Stoelinga, P.J. A modification of the pterygoid plate separation in low-level maxillary osteotomies. J. Oral Maxillofac. Surg. 1983, 41, 544–546. [Google Scholar] [CrossRef]
- O’Regan, B.; Bharadwaj, G. Pterygomaxillary separation in Le Fort I osteotomy UK OMFS consultant questionnaire survey. Br. J. Oral Maxillofac. Surg. 2006, 44, 20–23. [Google Scholar] [CrossRef]
- Breeze, J.; Verea Linares, C.; Stockton, P. Is an osteotome necessary for pterygomaxillary disjunction or disjunction through the tuberosity during Le Fort I osteotomy? A systematic review. Br. J. Oral Maxillofac. Surg. 2016, 54, 248–252. [Google Scholar] [CrossRef]
- Apinhasmit, W.; Chompoopong, S.; Methathrathip, D.; Sangvichien, S.; Karuwanarint, S. Clinical anatomy of the posterior maxilla pertaining to Le Fort I osteotomy in Thais. Clin. Anat. 2005, 18, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Kanazawa, T.; Kuroyanagi, N.; Miyachi, H.; Ochiai, S.; Kamiya, N.; Nagao, T.; Shimozato, K. Factors predictive of pterygoid process fractures after pterygomaxillary separation without using an osteotome in Le Fort I osteotomy. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Stajcić, Z. Altering the angulation of a curved osteotome-does it have effects on the type of pterygomaxillary disjunction in Le Fort I osteotomy? An experimental study. Int. J. Oral Maxillofac. Surg. 1991, 20, 301–303. [Google Scholar] [CrossRef] [PubMed]


| Sex | n (%) | Mean Age (Years) | ± SD | Min | Max | p-Value * |
|---|---|---|---|---|---|---|
| Males | 27 (54) | 51.04 | 16.211 | 20 | 79 | 0.048 |
| Females | 23 (46) | 41.88 | 15.742 | 19 | 74 | |
| Total | 50 (100) | 46.46 | 16.411 | 19 | 79 |
| PMS Measurement | Side | Mean | ± SD | Min | Max | p-Value * |
|---|---|---|---|---|---|---|
| Thickness (mm) | Right | 1.02 | 0.139 | 0.75 | 1.25 | 0.225 |
| Left | 0.98 | 0.144 | 0.70 | 1.25 | ||
| Height (mm) | Right | 16.67 | 2.569 | 11.40 | 22.50 | 0.392 |
| Left | 17.10 | 2.744 | 12.80 | 22.90 | ||
| Angulation (°) | Right | 57.86 | 5.212 | 67.20 | 49.10 | 0.380 |
| Left | 58.74 | 5.259 | 66.70 | 49.20 |
| PMS Measurement | Side | Mean | ± SD | Min | Max | p-Value * |
|---|---|---|---|---|---|---|
| Thickness (mm) | Right | 0.91 | 0.178 | 0.51 | 1.18 | 0.738 |
| Left | 0.90 | 0.179 | 0.57 | 1.36 | ||
| Height (mm) | Right | 16.35 | 2.748 | 11.40 | 22.50 | 0.973 |
| Left | 16.37 | 3.467 | 12.50 | 24.20 | ||
| Angulation (°) | Right | 58.42 | 6.210 | 67.60 | 47.90 | 0.975 |
| Left | 58.46 | 5.305 | 69.90 | 49.20 |
| PMS Measurement | Sex | Mean | ± SD | Min | Max | p-Value * |
|---|---|---|---|---|---|---|
| Thickness (mm) | Male | 1.00 | 0.130 | 0.76 | 1.22 | 0.029 |
| Female | 0.90 | 0.170 | 0.54 | 1.27 | ||
| Height (mm) | Male | 16.89 | 2.322 | 12.85 | 22.45 | 0.486 |
| Female | 16.36 | 2.994 | 12.05 | 23.35 | ||
| Angulation (°) | Male | 58.30 | 4.557 | 66.85 | 50.35 | 0.915 |
| Female | 58.44 | 4.755 | 67.35 | 49.95 |
| PMS Measurement | Sex | r | p-Value * |
|---|---|---|---|
| Thickness (mm) | Male | 0.17 | 0.400 |
| Female | 0.04 | 0.858 | |
| Height (mm) | Male | −0.16 | 0.411 |
| Female | 0.13 | 0.558 | |
| Angulation (°) | Male | 0.16 | 0.439 |
| Female | 0.14 | 0.516 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tunis, T.S.; Dratler, S.; Kats, L.; Allon, D.M. Characterization of Pterygomaxillary Suture Morphology: A CBCT Study. Appl. Sci. 2023, 13, 3825. https://doi.org/10.3390/app13063825
Tunis TS, Dratler S, Kats L, Allon DM. Characterization of Pterygomaxillary Suture Morphology: A CBCT Study. Applied Sciences. 2023; 13(6):3825. https://doi.org/10.3390/app13063825
Chicago/Turabian StyleTunis, Tatiana Sella, Shaked Dratler, Lazar Kats, and Dror Michael Allon. 2023. "Characterization of Pterygomaxillary Suture Morphology: A CBCT Study" Applied Sciences 13, no. 6: 3825. https://doi.org/10.3390/app13063825
APA StyleTunis, T. S., Dratler, S., Kats, L., & Allon, D. M. (2023). Characterization of Pterygomaxillary Suture Morphology: A CBCT Study. Applied Sciences, 13(6), 3825. https://doi.org/10.3390/app13063825






