Abstract
Adjacent segment disease (ASD) is a prevalent complication following lumbar fusion surgery, representing a significant challenge in spinal surgery. This study aimed to assess the long-term outcomes of Nitinol spring rod semi-rigid fixation, a potential alternative to traditional rigid fixation, in reducing the incidence of ASD. This retrospective case study evaluated 89 patients who underwent lumbar or lumbosacral surgeries using a combination of Bioflex® (a Nitinol spring rod dynamic stabilization system) and an interbody cage over 10 years of follow-up. The fusion status, adjacent segment disc height, mechanical complications, and re-operation rates were analyzed. The cohort had a median follow-up duration of 13.0 years. All patients achieved solid fusion at the final follow-up visit. One patient underwent revision surgery for clinical ASD (1.1%), and no patients required revision surgery due to mechanical problems. Radiological evidence of ASD was observed in 16.9% of the patients. This study’s findings suggest that semi-rigid fixation using Bioflex with an interbody cage is a possibly effective treatment strategy to prevent ASD. The technique potentially reduces the risk of ASD by allowing a degree of movement at the surgical site.
1. Introduction
Lumbar surgery, primarily dominated by rigid fusion techniques, has been a cornerstone in treating degenerative spinal conditions [1]. However, this approach has been increasingly scrutinized due to the rising incidence of adjacent segment disease (ASD), a significant complication that compromises patients’ long-term outcomes [2,3,4,5,6,7,8,9,10]. In spine surgery, ASD is defined as degeneration occurring in the mobile segments above or below the fused spinal segment, and it can result in adjacent segment listhesis, instability, herniated nucleus pulposus, stenosis, hypertrophic facet arthritis, scoliosis, and vertebral compression fractures [11,12]. While rigid fusion provides stability, it often does so at the cost of increased mechanical stress on adjacent segments, leading to ASD, as revealed in some biomechanical studies [13,14]. Radiological ASD was reported to have an incidence rate of 42.6% beyond a five-year follow-up [15]. The incidence of clinically significant ASD, necessitating revision surgery, ranges from 4.7% to 27.4% [5]. This issue has prompted the exploration of motion-preserving fixation methods as alternatives. Dynamic stabilization methods, such as Dynesis, ISObar-TTL, and PEEK (polyetheretherketone) rods, which aim to preserve motion while offering stability, initially showed promise but faced setbacks mainly due to a high rate of mechanical complications [16,17]. Semi-rigid fixation techniques, although less explored, offer a potential compromise. These methods strive for a balance between the rigidity needed for effective stabilization and the flexibility that is necessary to mitigate the mechanical impact on adjacent segments. Our study aimed to evaluate the long-term outcomes of semi-rigid fixation in lumbar surgery with a Nitinol spring rod (Bioflex) and an interbody cage. Nitinol is an alloy of nickel and titanium that belongs to a class of materials called shape memory alloys. Nitinol implants have high elasticity, high tensile force, and flexibility (below 10 °C), but they have rigidity (above 30 °C) and biological compatibility. This system has been used to preserve motion at the area of implantation. However, the standalone use of Bioflex and e-pedicle screws is not widely adopted due to concerns about mechanical failure [18]. We specifically hypothesized that the use of posteriorly placed Nitinol spring rods combined with the stability provided by an anterior cage would not impede the achievement of fusion and would result in a lower incidence of adjacent segment disease (ASD) compared to fusion surgery using rigid rods based on the reported outcomes of fusion surgery using rigid rods. Through documenting and analyzing the long-term outcomes of using this method, our aim is to contribute to the ongoing discussion on spinal surgery techniques and potentially redefine surgical strategies to improve patient outcomes in treating lumbar degenerative diseases.
2. Materials and Methods
2.1. Patient Population
This retrospective study included 89 patients who underwent surgery for degenerative disorders of L2-S1 using the Bioflex system and an interbody cage. This study was approved by the institutional review board of our hospital and our Institutional Regional Board, and the requirement for informed consent was waived in view of the retrospective nature of this study. From 2006 to 2010, a total of 462 patients underwent surgery. Among them, 146 patients (31.6%) had clinical data available for more than 10 years, and 89 patients (19%) had radiologic data. The surgical indications are identical to those of lumbar fusion surgery in degenerative conditions: severe radiating pain that persists despite more than 3 months of conservative treatment and the corresponding evidence of degenerative stenosis, degenerative spondylolisthesis, or spondylolytic spondylolisthesis. Patients under 18 years of age, with less than 10 years of follow-up, or with conditions other than degenerative diseases, such as infection, tumor, trauma, or congenital anomalies, were excluded from this study. Patients diagnosed with severe coronal deformities or osteoporosis were also excluded from this study. The average age of the patients at the time of surgery was 53.5 years, with females comprising 67% of the cohort. The average number of surgical levels involved was 1.4 ± 0.6, the follow-up period averaged 13.3 years (ranging from 10 to 17.5 years), and the mean body mass index (BMI) was 25.0 ± 2.9 kg/m2. The distribution of conditions was as follows: 24 patients (27%) had degenerative stenosis, 21 (23.6%) had degenerative spondylolisthesis, and 44 (49.4%) had spondylolytic spondylolisthesis (Table 1). The post hoc power analysis indicated that with an effect size of 89, this study had a power of 91% to detect significant differences with an alpha level of 0.05. This suggests that the sample size of 89 patients was sufficient to achieve adequate statistical power for the primary outcome measures.

Table 1.
The demographic and clinical characteristics of the patients.
2.2. Surgical Procedure
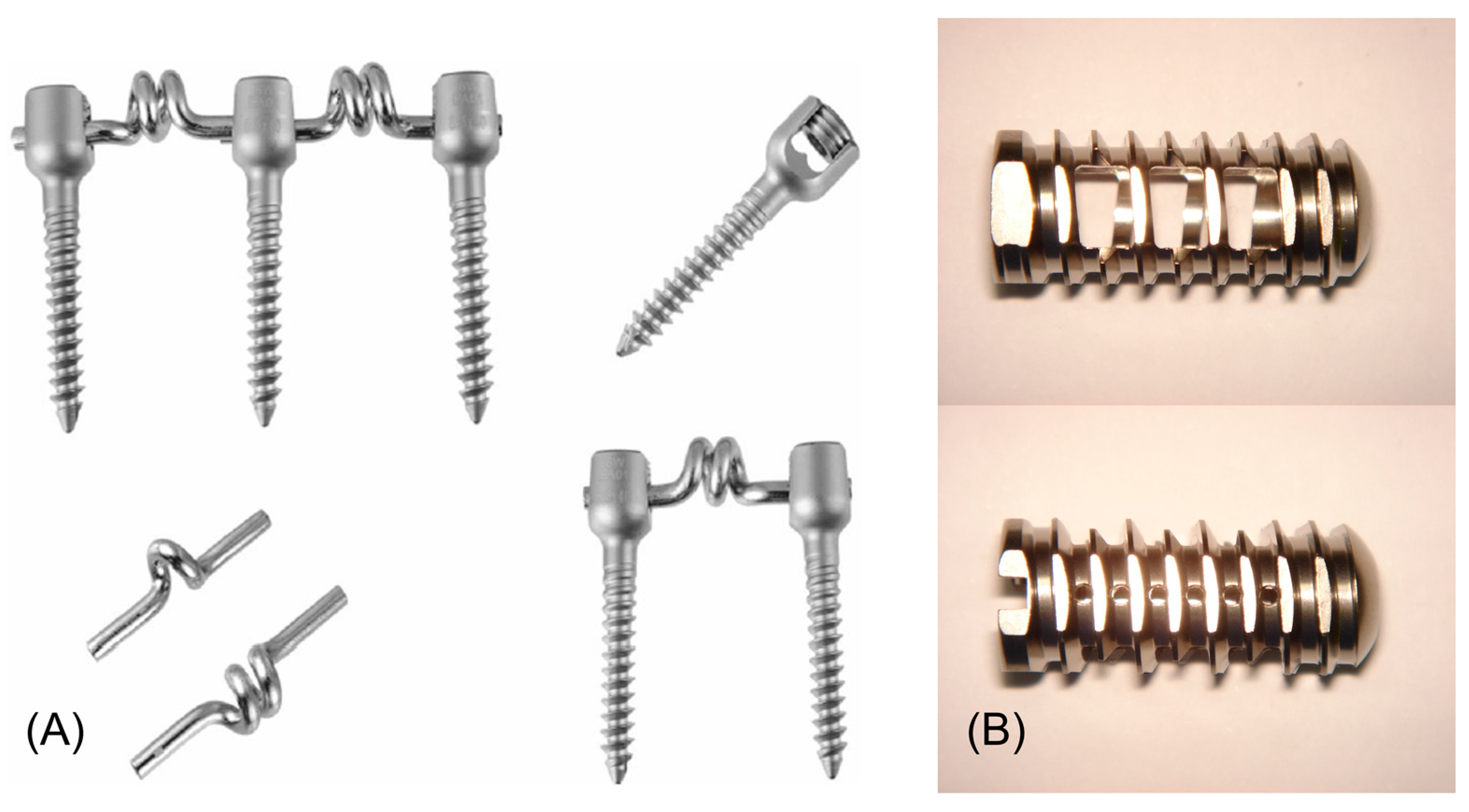
The posterior dynamic stabilization system used in this study (Bioflex System; Biospine Co., Ltd., Seoul, Republic of Korea) consisted of Ti6Al4V pedicle screws and a Nitinol spring rod. Nitinol is a nickel alloy, and Ti6Al4V is a shape memory alloy that was invented in 1962 by the US Naval Ordnance Laboratory. The diameter of the straight part in the Nitinol spring rod is 4 mm, featuring a coiled shape with 1 or 2 turns designed to provide physiological stability during flexion, extension, and lateral bending (Figure 1A, Supplement Video S1). The anterior fixation system used in this study comprised a threaded round cage made of Ti6Al4V (Figure 1B). The surgical procedure mirrored that of conventional posterior lumbar interbody fusion (PLIF) with a pedicle screw system. Under general endotracheal anesthesia, the patient was placed in a prone position. The procedure involved a midline incision, laminectomy at the target level, and discectomy. Pedicle screws were inserted into the pedicles bilaterally under fluoroscopic guidance. After meticulous preparation of the cartilaginous endplate, the cage was carefully inserted between the vertebral bodies by the threaded combination method without damaging the endplate. For the disc space, a threaded round titanium (Ti6Al4V) cage with a size that could reach as far forward into the disc space as possible, where cortical bone is more abundant, was chosen to prevent subsidence [19]. Finally, the Bioflex Nitinol spring rod and set screws were inserted. Appropriate positioning was confirmed by X-ray imaging before finishing surgery.
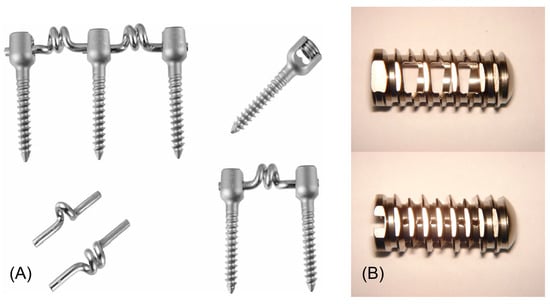
Figure 1.
(A) Photographs depicting the components of the BioFlex dynamic stabilization system consisting of titanium screws and Nitinol rods. There are 2 types of rods: 1 features a single-turn coil, and the other has a dual-turn coil. The photograph in the upper right corner illustrates the unique design of the BioFlex screw head. The design incorporates 2 grooves, allowing for the insertion of 2 rods per segment in instances where stabilization extends beyond a single segment (adapted with permission from Bio-Spine Corp, Seoul, Republic of Korea.). (B) Photographs of a threaded round cage made of Ti6Al4V.
2.3. Radiologic Outcome Measures
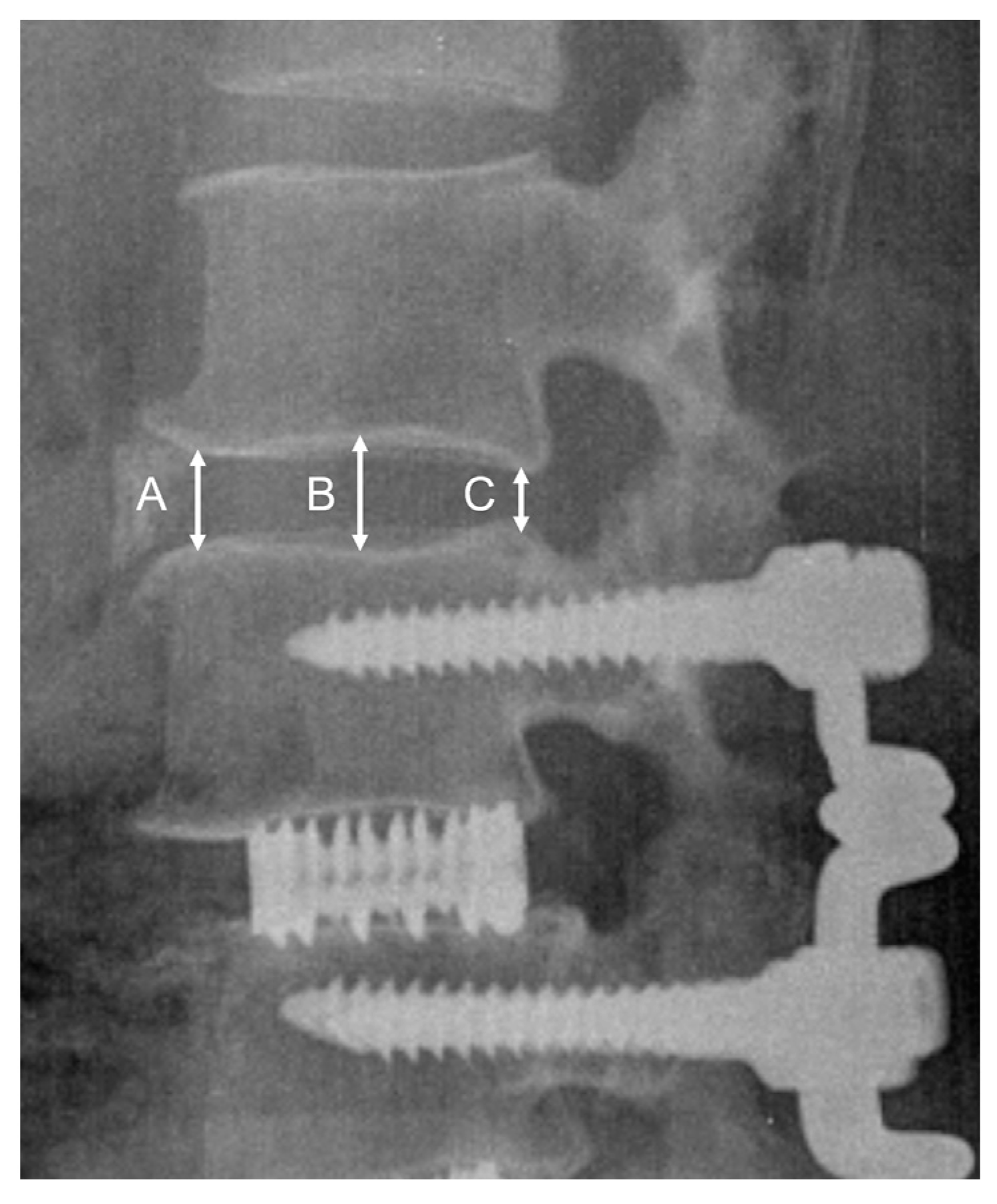
All radiographs were analyzed using validated software (Surgimap Version 2.3.2.1., Nemaris Inc., New York, NY, USA). Lumbar lordosis (LL; cobb’s angle from L1 upper endplate to S1 upper endplate) was measured in plain radiographs preoperatively, post-operatively, and at the final follow-up. The mean disc height (MDH) was calculated as the mean of the anterior, middle, and posterior disc heights (Figure 2) [20]. The reduction in the adjacent MDH was determined by comparing the final follow-up MDH to the preoperative MDH. Fusion was considered to be achieved when a clear bone bridging through the cages was detected on CT scan multiplanar reconstructions. The degeneration of adjacent discs was graded using the Weiner classification, which is based on the disc height and degenerative changes like osteophytes [21]. Radiographic ASD was defined as the development of spondylolisthesis > 4 mm, segmental kyphosis > 10°, the complete collapse of the disc space, or a deterioration in the Weiner classification of 2 or more grades [22].
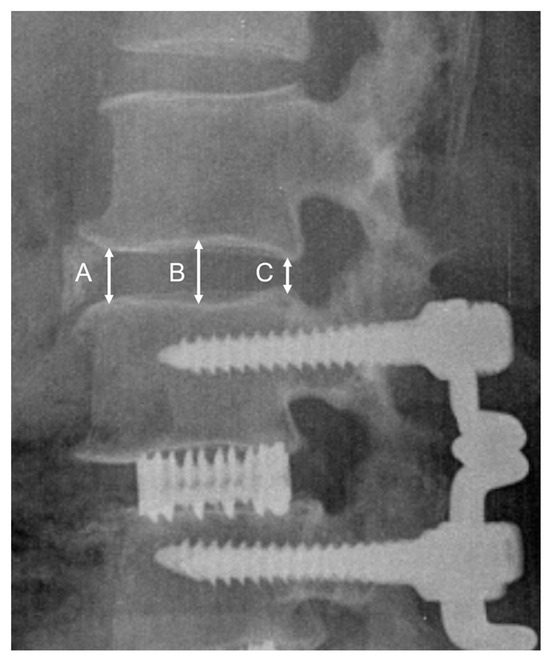
Figure 2.
Radiographic measurements of the lumbar disc height: A, anterior disc height; B, middle disc height; C, posterior disc height. Disc height = (A + B + C)/3 (mm).
2.4. Statistical Analysis
Numerical data are expressed as the mean ± standard deviation for parametric distributions and the median with an interquartile range for non-parametric distributions. Student’s t-test, a parametric test, was employed to compare the means between 2 groups when the data were normally distributed. For non-normally distributed data or when dealing with ordinal data or non-numeric outcomes, the non-parametric test known as the Wilcoxon signed-rank test was utilized. A p-value of less than 0.05 was set as the threshold for statistical significance to determine meaningful differences or changes. The choice of test was based on the Shapiro–Wilk test for normality and the presence of outliers, which was assessed prior to the main analysis. All statistical analyses were conducted using SPSS Ver. 26 (SPSS, Inc., Chicago, IL, USA).
3. Results
This study examined the preservation of the disc height in a total of 89 patients. The mean follow-up time was 159 months. Out of 146 patients, 89, along with an additional 58 who were not included in this study, demonstrated outcomes according to the Modified Odom’s Criteria: 30.8% were rated as good, 67.1% as better, and 2.1% as fair, and there were no poor outcomes [23]. The upper adjacent MDH was maintained at 84.6 ± 15.1% across all levels of surgery, without a significant difference being observed between the number of levels operated on (p = 0.12). The lower disc height was maintained at 89.4 ± 8.4% overall, and the level of surgery was not related to the MDH (p = 0.95). The occurrence of spondylolisthesis at the last follow-up was 5.7% (five patients) in the total population. Dividing by the number of levels operated revealed that 7% (four patients) had single-level surgeries, 3.8% (one patient) had two-level surgeries, and none had three-level surgeries, which was not statistically significant (p = 1).
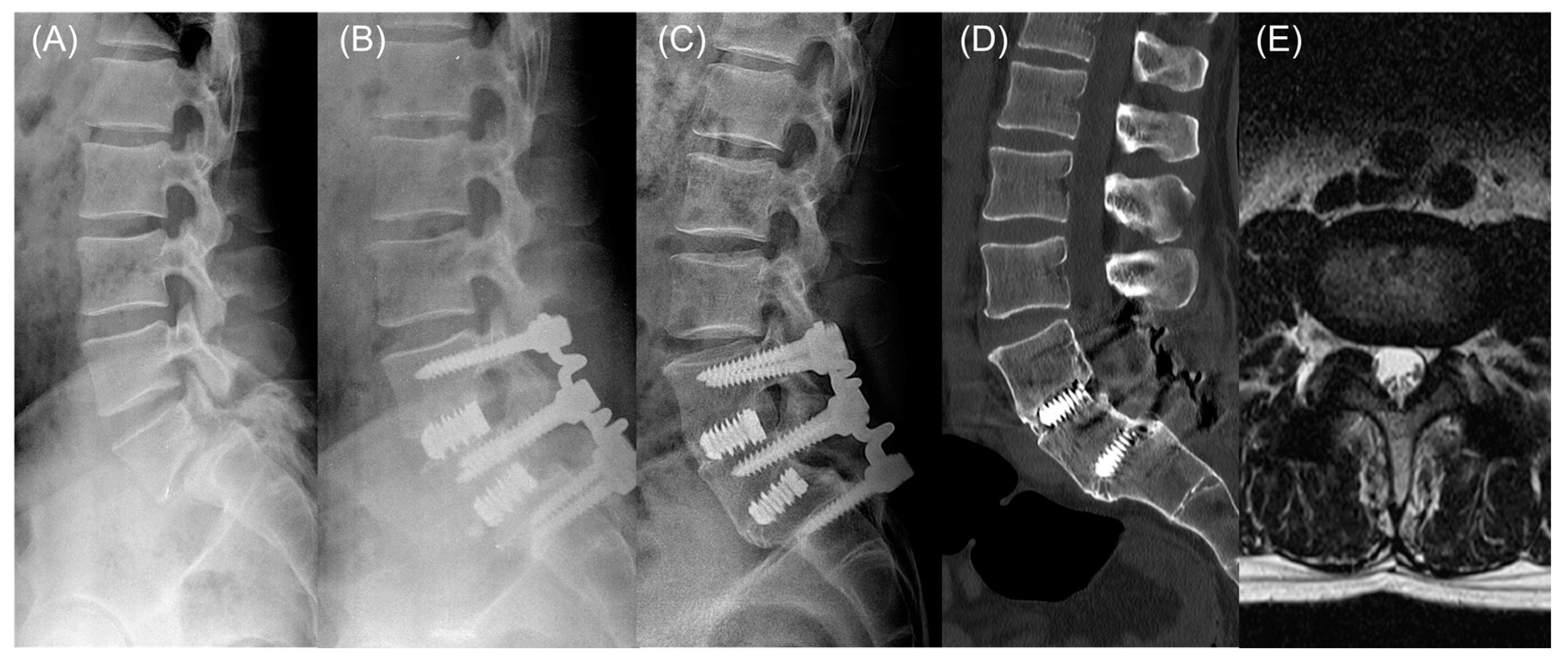
Fifteen (16.9%) of the total cohort developed ASD. There was a notable increase in ASD incidence with the number of levels operated: 13.8% (eight patients) had single-level surgeries, 15.4% (four patients) had two-level surgeries, and 60.0% (three patients) had three-level surgeries (p = 0.03). Five cases of rod fracture and one case of cage subsidence greater than 2 mm occurred, although there were no correlated symptoms (Table 2). One patient in her seventh year after L4–5 surgery underwent revision surgery for clinical ASD. Aside from this case, no other patients required revision surgery (illustrative case, Figure 3).

Table 2.
Surgical outcomes based on level of surgery.
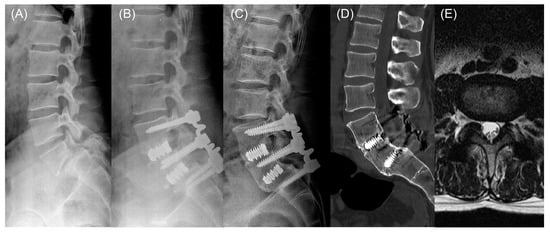
Figure 3.
Illustrative case. (A) A 48-year-old male patient underwent L4–5-S1 fusion surgery using a Nitinol spring rod due to severe lower back pain and bilateral radiculopathy stemming from L4–5 stenosis and L5-S1 spondylolytic spondylolisthesis. (A) A preoperative lateral radiograph. (B) A radiograph taken 1 year post-operation. (C) A radiograph taken 16 years post-operation. No mechanical failure is observed, and solid fusion is evident. (D) A sagittal view of the computer tomography 16 years post-operation showing solid fusion at both operated levels. (E) An axial MRI image of the adjacent level (L3–4) 16 years post-operation.
The preoperative LL was documented at 37.8 ± 10.9°. Immediately post-operatively, LL showed remarkable consistency with an immediate post-operative measurement of 37.9 ± 9.6°. The long-term follow-up revealed a slight non-significant reduction in LL to 36.5 ± 11.4°, suggesting the preservation of spinal curvature throughout the course of recovery and beyond (Table 3). At the final follow-up, it was confirmed that fusion had occurred at the site of the interbody cage in all cases in this study.

Table 3.
The lumbar lordosis measurement of the angle.
In the final follow-up, a significant difference was observed when comparing patients with ASD to those without ASD based on the number of surgery levels. The incidence of ASD was 13.8% for one level, 26.7% for two levels, and 60% for three levels (p = 0.03). However, there were no significant differences in age, gender, BMI, follow-up periods, or lumbar lordosis between the preoperative period and final follow-up (Table 4).

Table 4.
Comparison of demographic and clinical characteristics between patients with and without ASD at final follow-up.
4. Discussion
In our study, the upper disc height and lower disc height were maintained at 84.6% and 89.2%, respectively, over the follow-up period. Radiological ASD was observed in 16.9% of the patients. According to a study by Schulte et al., there was an 18.9–22% reduction in the adjacent disc height at an average of 114 months post-posterolateral fusion (PLF), while our study showed a 15.4% reduction at an average of 159 months [24]. Harrop et al. reported that the annual risk of re-operation due to reported ASD was 2–14%, and Sears et al. reported a necessity for re-operation in 9% of cases at 5 years and 31% at 10 years [5,9]. A study by Kuo et al. reported radiologic ASD at 37% in solid fusion and 17% in Dynesys at 3 years [15]. Our study also showed a similar rate of 16.9 for radiologic ASD. However, considering that our average follow-up was 13 years, the risk of ASD might be lower. Furthermore, only a single patient in our study required re-operation due to ASD, suggesting that ensuring the stability of the surgical segments and potentially delaying adjacent segment disease could present an advantage over solid fusion. We used the Bioflex system, which has been used by Park et al. for dynamic stabilization and by Kim et al. in conjunction with PLIF, showing positive short-term outcomes [18,25]. An optimal system would include rods that are resistant to fatigue failure and that do not exhibit loosening at the device–bone interface. Because of these concerns, biomechanical tests were conducted using the BioFlex system [26]. The fatigue strength assessment, in accordance with the American Society for Testing and Materials F1717, involved a 9 mm displacement subject to 20 million cycles at 5 Hz, which did not subject the device to significant strains. The device maintained its structural integrity during the compression, torsion, and tension tests, indicating minimal strain transfer. Additionally, the biocompatibility of the Bioflex rod was examined. Over a period of 9 days, a nickel release test employing inductively coupled plasma–atomic emission spectroscopy did not show detectable nickel release, and a galvanic corrosion examination was conducted to determine the device’s performance in contact with other metals, which did not show any adverse interactions. While dynamic stabilization can be useful in certain indications, its inability to increase the disc height limits its applicability, and some studies have reported a mechanical failure risk exceeding 20% [16,17,27]. Convinced that dynamic stabilization lacking solid fusion could precipitate mechanical failure, our approach incorporated the use of an interbody cage. In our study, this strategy was shown to be effective through a 100% fusion rate over an average follow-up period of 13.0 years like that of a solid fusion surgery. Biomechanical studies suggest that semi-rigid fixation, particularly in long-level fusion surgery, enhances mobility at the UIV. This facilitates a more gradual transition of motion between the instrumented and the adjacent non-instrumented segments of the spine [17]. It also decreases screw loading at the UIV, which can reduce the occurrence of proximal junctional kyphosis. In the context of long-level fusion surgery, some surgeons have employed soft-landing techniques using hooks or bandages to prevent proximal junctional failure and similar issues [17,28,29,30]. We suggest that these mechanisms may have contributed to our study’s observation of a 16.9% incidence rate of radiologic ASD. In our study, the role of the cage in the anterior part of the spine was to reduce the load applied to the posterior spring rod, thus preventing fracture in the spring rod and maintaining the disc space interval, stabilizing the anterior column of the spine. Normal spinal load sharing has an anterior-to-posterior ratio of approximately 80:20. In biomechanical studies by Sengupta et al., rigid fixation altered this ratio to 59:41, whereas semi-rigid fixation showed a closer approximation to physiological load sharing at 75:25 and resulted in more uniform pressure distribution on the interbody cage compared to rigid rods [31]. Several limitations in this study should be pointed out, including its retrospective nature, the presence of selection bias due to a low follow-up rate, the small patient cohort, and the absence of a control group. Ideally, clinical outcomes should be quantitatively analyzed using health-related quality of life questionnaires. However, in this study, clinical outcomes could only be determined based on whether the patients underwent revision surgery for ASD. Additionally, there were no specific indications for whether surgeons should use rigid rods or Bioflex rods; the choices were made based on the surgeons’ preferences and discussions with the patients. Moreover, there was no consistent serial follow-up during the long-term follow-up period, leading to heterogeneous follow-up durations among patients. However, an ongoing discussion about alternatives to rigid fixation is crucial, and we believe that our study on long-term outcomes holds significant importance for future research directions in this field. Through this study, we confirmed that surgery using the Bioflex rod and cage could be a good alternative to lumbar fusion surgery with rigid rods by potentially lowering the ASD rate and demonstrating long-term stability. These findings suggest that further results could be developed through larger-scale and prospective studies.
5. Conclusions
This study assessed the long-term efficacy of semi-rigid fixation using the Bioflex Nitinol spring rod and interbody cage in lumbar surgery, suggesting it as a viable alternative to reduce ASD. The main conclusions can be summarized as follows:
- (1)
- Our findings indicate a lower incidence of ASD (16.9%) over a median follow-up of 13.0 years.
- (2)
- The adjacent disc height and motion were maintained compared to traditional rigid fixation.
- (3)
- There was a 5.6% incidence of mechanical complications due to rod fractures, but no patients required revision surgery due to symptoms.
- (4)
- As there were no cases of pseudarthrosis at the final follow-up in this case series, this surgical method can achieve a reasonable fusion rate.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/app14114574/s1, Video S1: A video demonstrating a Bioflex spring rod connected to a pedicle screw model repeatedly performing flexion and extension movements. The normal flexion and extension motion of the rod are facilitated by the structure of the spring rod.
Author Contributions
Conceptualization, D.-K.C.; methodology, D.-K.C.; validation, B.-J.M.; formal analysis, H.-J.J.; investigation, H.-J.J.; resources, D.-K.C.; data curation, H.-J.J.; writing—original draft preparation, H.-J.J.; writing—review and editing, H.-J.J., B.-J.M., and D.-K.C.; visualization, D.-K.C.; supervision, D.-K.C.; project administration, H.-J.J. and D.-K.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was a retrospective radiographic investigation approved by Gangnam Severance Hospital’s institutional review board (IRB No. 3-2023-0454).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of this study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to personal information.
Acknowledgments
The patient data and radiologic data presented in this study were provided by Kwang-Hye Spine Hospital, Seoul, South Korea. The supplementary video was provided by Biospine, Co., Ltd., Seoul, Republic of Korea.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Harris, I.A.; Traeger, A.; Stanford, R.; Maher, C.G.; Buchbinder, R. Lumbar Spine Fusion: What Is the Evidence? Intern. Med. J. 2018, 12, 1430–1434. [Google Scholar] [CrossRef] [PubMed]
- Cheh, G.; Bridwell, K.H.; Lenke, L.G.; Buchowski, J.M.; Daubs, M.D.; Kim, Y.; Baldus, C. Adjacent Segment Disease Followinglumbar/Thoracolumbar Fusion with Pedicle Screw Instrumentation: A Minimum 5-Year Follow-Up. Spine 2007, 32, 2253–2257. [Google Scholar] [CrossRef] [PubMed]
- Ekman, P.; Möller, H.; Shalabi, A.; Yu, Y.X.; Hedlund, R. A Prospective Randomised Study on the Long-Term Effect of Lumbar Fusion on Adjacent Disc Degeneration. Eur. Spine J. 2009, 18, 1175–1186. [Google Scholar] [CrossRef] [PubMed]
- Ghiselli, G.; Wang, J.C.; Bhatia, N.N.; Hsu, W.K.; Dawson, E.G. Adjacent Segment Degeneration in the Lumbar Spine. JBJS 2004, 86, 1497–1503. [Google Scholar] [CrossRef] [PubMed]
- Harrop, J.S.; Youssef, J.A.; Maltenfort, M.; Vorwald, P.; Jabbour, P.; Bono, C.M.; Goldfarb, N.; Vaccaro, A.R.; Hilibrand, A.S. Lumbar Adjacent Segment Degeneration and Disease after Arthrodesis and Total Disc Arthroplasty. Spine 2008, 33, 1701–1707. [Google Scholar] [CrossRef]
- Helgeson, M.D.; Bevevino, A.J.; Hilibrand, A.S. Update on the Evidence for Adjacent Segment Degeneration and Disease. Spine J. 2013, 13, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Kumar, M.; Baklanov, A.; Chopin, D. Correlation between Sagittal Plane Changes and Adjacent Segment Degeneration Following Lumbar Spine Fusion. Eur. Spine J. 2001, 10, 314–319. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Villaescusa, J.; Hidalgo, J.L.-T.; Ruiz-Picazo, D.; Martín-Benlloch, A. A Descriptive Study on the Adjacent Segment Degeneration Related Signs Following a Lumbar Fusion Procedure. J. Spine Surg. 2021, 7, 354. [Google Scholar] [CrossRef] [PubMed]
- Sears, W.R.; Sergides, I.G.; Kazemi, N.; Smith, M.; White, G.J.; Osburg, B. Incidence and Prevalence of Surgery at Segments Adjacent to a Previous Posterior Lumbar Arthrodesis. Spine J. 2011, 11, 11–20. [Google Scholar] [CrossRef]
- Yoon, S.G.; Lee, H.C.; Lee, S.-M. Pelvic Incidence–Lumbar Lordosis Mismatch Is Predisposed to Adjacent Segment Degeneration after Single-Level Anterior Lumbar Interbody Fusion: A Retrospective Case-Control Study. Neurospine 2023, 20, 301. [Google Scholar] [CrossRef]
- Birjandi, A. Adjacent Segment Degeneration. J. Inj. Violence Res. 2012, 4 (Suppl. S1), 8. [Google Scholar]
- Virk, S.S.; Niedermeier, S.; Yu, E.; Khan, S.N. Adjacent Segment Disease. Orthopedics 2014, 37, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Li, H.-M.; Zhang, R.; Zhang, H.; Shen, C.-L. Biomechanical Changes of Adjacent and Fixed Segments through Cortical Bone Trajectory Screw Fixation Versus Traditional Trajectory Screw Fixation in the Lumbar Spine: A Finite Element Analysis. World Neurosurg. 2021, 151, e447–e456. [Google Scholar] [CrossRef] [PubMed]
- Cao, L.; Liu, Y.; Mei, W.; Xu, J.; Zhan, S. Biomechanical Changes of Degenerated Adjacent Segment and Intact Lumbar Spine after Lumbosacral Topping-Off Surgery: A Three-Dimensional Finite Element Analysis. BMC Musculoskelet. Disord. 2020, 21, 104. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.-H.; Huang, W.-C.; Wu, J.-C.; Tu, T.-H.; Fay, L.-Y.; Wu, C.-L.; Cheng, H. Radiological Adjacent-Segment Degeneration in L4–5 Spondylolisthesis: Comparison between Dynamic Stabilization and Minimally Invasive Transforaminal Lumbar Interbody Fusion. J. Neurosurg. Spine 2018, 29, 250–258. [Google Scholar] [CrossRef] [PubMed]
- Barrey, C.Y.; Ponnappan, R.K.; Song, J.; Vaccaro, A.R. Biomechanical Evaluation of Pedicle Screw-Based Dynamic Stabilization Devices for the Lumbar Spine: A Systematic Review. SAS J. 2008, 2, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Liu, L.; Shi, J.-Y.; Yan, K.-Z.; Shen, W.-Z.; Yang, Z.-R. Clinical and Biomechanical Researches of Polyetheretherketone (Peek) Rods for Semi-Rigid Lumbar Fusion: A Systematic Review. Neurosurg. Rev. 2018, 41, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.Y.; Park, J.Y.; Cho, B.Y. The Bioflex System as a Dynamic Stabilization Device: Does It Preserve Lumbar Motion? J. Korean Neurosurg. Soc. 2009, 46, 431. [Google Scholar] [CrossRef]
- Ritzel, H.; Amling, M.; Pösl, M.; Hahn, M.; Delling, G. The Thickness of Human Vertebral Cortical Bone and Its Changes in Aging and Osteoporosis: A Histomorphometric Analysis of the Complete Spinal Column from Thirty-Seven Autopsy Specimens. J. Bone Miner. Res. 1997, 12, 89–95. [Google Scholar] [CrossRef]
- Lin, B.; Yu, H.; Chen, Z.; Huang, Z.; Zhang, W. Comparison of the Peek Cage and an Autologous Cage Made from the Lumbar Spinous Process and Laminae in Posterior Lumbar Interbody Fusion. BMC Musculoskelet. Disord. 2016, 17, 374. [Google Scholar] [CrossRef]
- Weiner, D.K.; Distell, B.; Studenski, S.; Martinez, S.; Lomasney, L.; Bongiorni, D. Does Radiographic Osteoarthritis Correlate with Flexibility of the Lumbar Spine? J. Am. Geriatr. Soc. 1994, 42, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Röllinghoff, M.; Schlüter-Brust, K.; Groos, D.; Sobottke, R.; Michael, J.W.-P.; Eysel, P.; Delank, K.S. Mid-Range Outcomes in 64 Consecutive Cases of Multilevel Fusion for Degenerative Diseases of the Lumbar Spine. Orthop. Rev. 2010, 2, e3. [Google Scholar] [CrossRef] [PubMed]
- Luo, C.-A.; Lim, A.S.; Lu, M.-L.; Chiu, P.-Y.; Lai, P.-L.; Niu, C.-C. The Surgical Outcome of Multilevel Anterior Cervical Discectomy and Fusion in Myelopathic Elderly and Younger Patients. Sci. Rep. 2022, 12, 4495. [Google Scholar] [CrossRef] [PubMed]
- Schulte, T.L.; Leistra, F.; Bullmann, V.; Osada, N.; Vieth, V.; Marquardt, B.; Lerner, T.; Liljenqvist, U.; Hackenberg, L. Disc Height Reduction in Adjacent Segments and Clinical Outcome 10 Years after Lumbar 360 Fusion. Eur. Spine J. 2007, 16, 2152–2158. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.-S.; Zhang, H.-Y.; Moon, B.-J.; Park, K.-W.; Ji, K.-Y.; Lee, W.-C.; Oh, K.-S.; Ryu, G.-U.; Kim, D.H. Nitinol Spring Rod Dynamic Stabilization System and Nitinol Memory Loops in Surgical Treatment for Lumbar Disc Disorders: Short-Term Follow Up. Neurosurg. Focus. 2007, 22, 1–9. [Google Scholar] [CrossRef]
- Massey, P.A.; Hoge, S.; Nelson, B.G.; Ogden, A.L.; Mody, M.G.; Myers, M.; Bilderback, K.; Solitro, G.; Barton, R.S. Nitinol Memory Rods Versus Titanium Rods: A Biomechanical Comparison of Posterior Spinal Instrumentation in a Synthetic Corpectomy Model. Glob. Spine J. 2021, 11, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Akgün, M.; Ateş, Ö.; Günerbüyük, C.; Karadağ, M.; Özer, A. Long-Term Failure of Dynamic Rods Used in Full Dynamic Stabilization. J. Turk. Spinal Surg. 2023, 34, 137–142. [Google Scholar] [CrossRef]
- Lee, B.-J.; Bae, S.S.; Choi, H.Y.; Park, J.H.; Hyun, S.-J.; Jo, D.J.; Cho, Y.; Korean Spinal Deformity Society. Proximal Junctional Kyphosis or Failure after Adult Spinal Deformity Surgery-Review of Risk Factors and Its Prevention. Neurospine 2023, 20, 863. [Google Scholar] [CrossRef] [PubMed]
- Cazzulino, A.; Gandhi, R.; Woodard, T.; Ackshota, N.; Janjua, M.B.; Arlet, V.; Saifi, C. Soft Landing Technique as a Possible Prevention Strategy for Proximal Junctional Failure Following Adult Spinal Deformity Surgery. J. Spine Surg. 2021, 7, 26. [Google Scholar] [CrossRef] [PubMed]
- Rodnoi, P.; Le, H.; Hiatt, L.; Wick, J.; Barber, J.; Javidan, Y.; Roberto, R.; Klineberg, E.O. Ligament Augmentation with Mersilene Tape Reduces the Rates of Proximal Junctional Kyphosis and Failure in Adult Spinal Deformity. Neurospine 2021, 18, 580. [Google Scholar] [CrossRef]
- Sengupta, D.K.; Bucklen, B.; McAfee, P.C.; Nichols, J.; Angara, R.; Khalil, S. The Comprehensive Biomechanics and Load-Sharing of Semirigid Peek and Semirigid Posterior Dynamic Stabilization Systems. Adv. Orthop. 2013, 2013, 745610. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).