Designing a Socially Assistive Robot to Assist Older Patients with Chronic Obstructive Pulmonary Disease in Managing Indoor Air Quality
Abstract
:1. Introduction
2. Materials and Methods
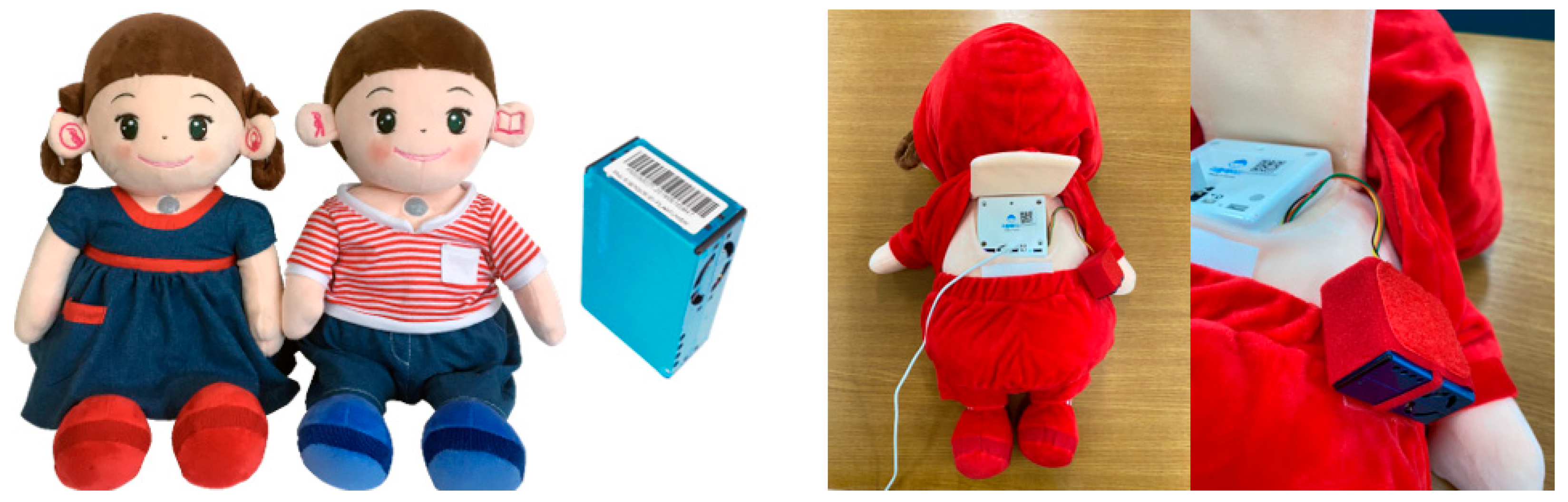
2.1. A Socially Assistive Robot with an Air Quality Sensor
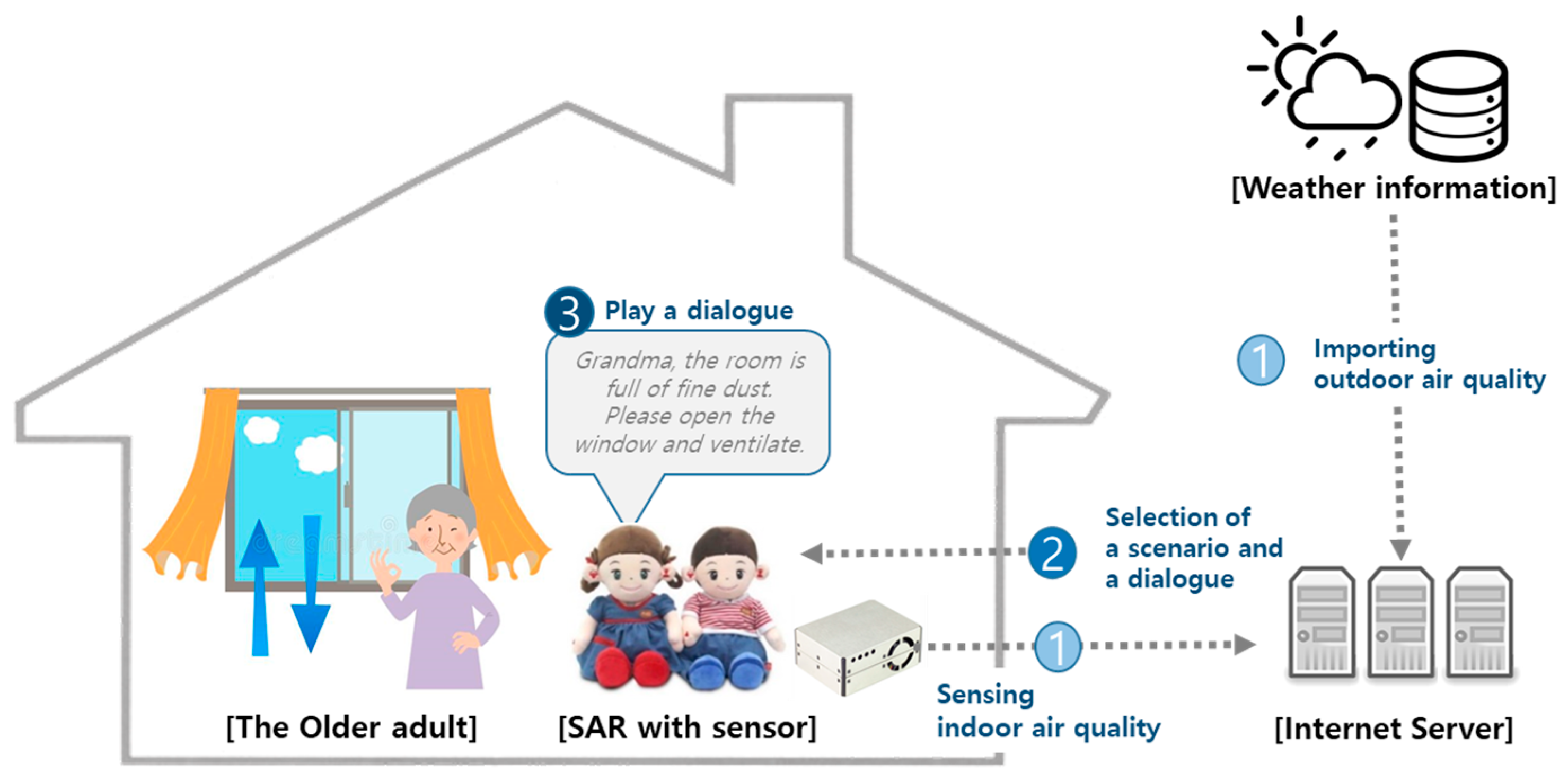
2.2. Collection of Weather (Atmosphere) Information
2.3. Scenarios and Intervention Stages
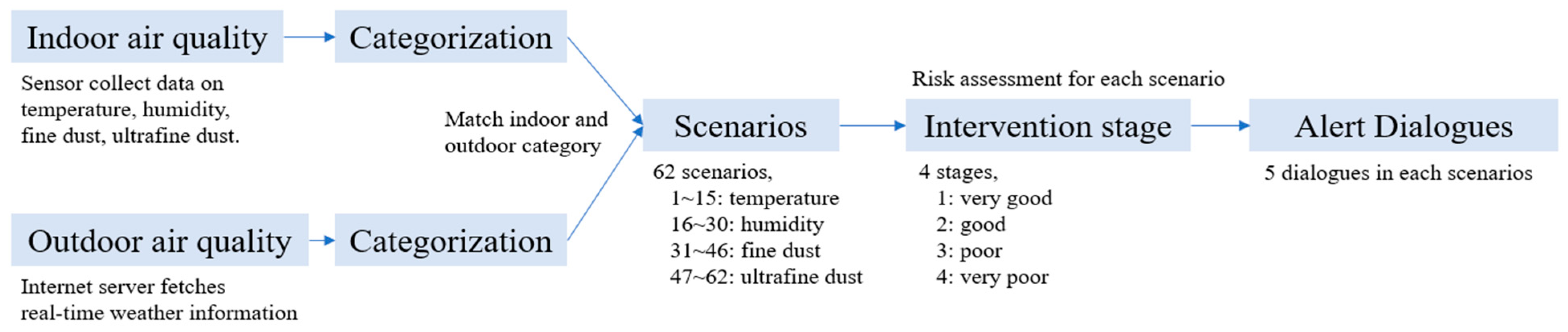
2.3.1. Combinations of Indoor and Outdoor Air Quality: Scenarios
2.3.2. Risk Assessment: Intervention Stages
2.3.3. Dialogues and Intervention Algorithm
2.4. Operating Mechanism
2.5. Participants
2.5.1. Inclusion and Exclusion Criteria
2.5.2. Participant Information
2.5.3. Research Process
2.6. Data Analysis
3. Results
3.1. Daily Trend of Air Quality Alert Occurrences per Hour
3.2. Prediction Analysis for Improvement in IAQ by Machine Learning
3.3. Summary of Interviews after Using SAR
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pauwels, R.A.; Rabe, K.F. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet 2004, 364, 613–620. [Google Scholar] [CrossRef] [PubMed]
- Adeloye, D.; Song, P.; Zhu, Y.; Campbell, H.; Sheikh, A.; Rudan, I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: A systematic review and modelling analysis. Lancet Respir. Med. 2022, 10, 447–458. [Google Scholar] [CrossRef] [PubMed]
- Cavaillès, A.; Brinchault-Rabin, G.; Dixmier, A.; Goupil, F.; Gut-Gobert, C.; Marchand-Adam, S.; Meurice, J.-C.; Morel, H.; Person-Tacnet, C.; Leroyer, C. Comorbidities of COPD. Eur. Respir. Rev. 2013, 22, 454–475. [Google Scholar] [CrossRef] [PubMed]
- Raherison, C.; Girodet, P.O. Epidemiology of COPD. Eur. Respir. Rev. 2009, 18, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Morley, J.E. Chronic obstructive pulmonary disease: A disease of older persons. J. Am. Med. Dir. Assoc. 2014, 15, 151–153. [Google Scholar] [CrossRef] [PubMed]
- Williams, V.; Bruton, A.; Ellis-Hill, C.; McPherson, K. The importance of movement for people living with chronic obstructive pulmonary disease. Qual. Health Res. 2011, 21, 1239–1248. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.; Shorter, C.; Kvalsvig, A.; Barnard, L.T.; Wilson, N.; Crane, J.; Douwes, J.; Cunningham, C.; Taptiklis, P.; Phipps, R. Indoor air quality, largely neglected and in urgent need of a refresh. New Zealand Med. J. 2022, 135, 136–139. [Google Scholar] [PubMed]
- Heseltine, E.; Rosen, J. WHO Guidelines for Indoor Air Quality: Dampness and Mould; World Health Organization: Geneva, Switzerland, 2009.
- Osman, L.M.; Douglas, J.G.; Garden, C.; Reglitz, K.; Lyon, J.; Gordon, S.; Ayres, J.G. Indoor air quality in homes of patients with chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2007, 176, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Shetty, B.S.P.; D’Souza, G.; Padukudru Anand, M. Effect of indoor air pollution on chronic obstructive pulmonary disease (COPD) deaths in Southern Asia—A systematic review and meta-analysis. Toxics 2021, 9, 85. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Sun, S.; Tang, R.; Qiu, H.; Huang, Q.; Mason, T.G.; Tian, L. Major air pollutants and risk of COPD exacerbations: A systematic review and meta-analysis. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 3079–3091. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines for Indoor Air Quality: Household Fuel Combustion; World Health Organization: Geneva, Switzerland, 2014.
- Liang, L.; Cai, Y.; Barratt, B.; Lyu, B.; Chan, Q.; Hansell, A.L.; Xie, W.; Zhang, D.; Kelly, F.J.; Tong, Z. Associations between daily air quality and hospitalisations for acute exacerbation of chronic obstructive pulmonary disease in Beijing, 2013–2017: An ecological analysis. Lancet Planet. Health 2019, 3, e270–e279. [Google Scholar] [CrossRef] [PubMed]
- Oh, J.S.; Park, S.H.; Kwak, M.K.; Pyo, C.H.; Park, K.H.; Kim, H.B.; Shin, S.Y.; Choi, H.J. Ambient particulate matter and emergency department visit for chronic obstructive pulmonary disease. J. Korean Soc. Emerg. Med. 2017, 28, 32–39. [Google Scholar]
- Meade, R.D.; Akerman, A.P.; Notley, S.R.; McGinn, R.; Poirier, P.; Gosselin, P.; Kenny, G.P. Physiological factors characterizing heat-vulnerable older adults: A narrative review. Environ. Int. 2020, 144, 105909. [Google Scholar] [CrossRef] [PubMed]
- Ailshire, J.; Brown, L.L. The importance of air quality policy for older adults and diverse communities. Public Policy Aging Rep. 2021, 31, 33–37. [Google Scholar] [CrossRef] [PubMed]
- McCormack, M.C.; Belli, A.J.; Waugh, D.; Matsui, E.C.; Peng, R.D.; Williams, D.A.L.; Paulin, L.; Saha, A.; Aloe, C.M.; Diette, G.B. Respiratory effects of indoor heat and the interaction with air pollution in chronic obstructive pulmonary disease. Ann. Am. Thorac. Soc. 2016, 13, 2125–2131. [Google Scholar] [CrossRef] [PubMed]
- Sebastião, B.F.; Hortelão, R.M.; Granadas, S.S.; Faria, J.M.; Pinto, J.R.; Henriques, H.R. Air quality self-management in asthmatic patients with COPD: An integrative review for developing nursing interventions to prevent exacerbations. Int. J. Nurs. Sci. 2023, 11, 46–56. [Google Scholar] [CrossRef] [PubMed]
- Pradhan, B.; Bharti, D.; Chakravarty, S.; Ray, S.S.; Voinova, V.V.; Bonartsev, A.P.; Pal, K. Internet of things and robotics in transforming current-day healthcare services. J. Healthc. Eng. 2021, 2021, 9999504. [Google Scholar] [CrossRef] [PubMed]
- Kodali, R.K.; Swamy, G.; Lakshmi, B. An implementation of IoT for healthcare. In Proceedings of the 2015 IEEE Recent Advances in Intelligent Computational Systems (RAICS), Trivandrum, India, 10–12 December 2015; pp. 411–416. [Google Scholar]
- Lee, H.; Park, Y.R.; Kim, H.-R.; Kang, N.Y.; Oh, G.; Jang, I.-Y.; Lee, E. Discrepancies in demand of internet of things services among older people and people with disabilities, their caregivers, and health care providers: Face-to-face survey study. J. Med. Internet Res. 2020, 22, e16614. [Google Scholar] [CrossRef]
- Jo, H.S.; Hwang, Y.S. Psychological factors that affect the acceptance and need for ICT services for older adults with chronic diseases. Gerontechnology 2021, 20, 1. [Google Scholar] [CrossRef]
- Pu, L.; Moyle, W.; Jones, C.; Todorovic, M. The effectiveness of social robots for older adults: A systematic review and meta-analysis of randomized controlled studies. Gerontologist 2019, 59, e37–e51. [Google Scholar] [CrossRef]
- Kim, E.-J.; Nam, I.-C.; Koo, Y.-R. Reframing patient experience approaches and methods to achieve patient-centeredness in healthcare: Scoping review. Int. J. Environ. Res. Public Health 2022, 19, 9163. [Google Scholar] [CrossRef] [PubMed]
- Abdi, J.; Al-Hindawi, A.; Ng, T.; Vizcaychipi, M.P. Scoping review on the use of socially assistive robot technology in elderly care. BMJ Open 2018, 8, e018815. [Google Scholar] [CrossRef] [PubMed]
- Jo, H.; Kim, J.; Kim, S. Factors related to the effectiveness in the use of an ICT-based toy robot for the in-home care of community dwelling elderly. Korean J. Health Educ. Promot. 2019, 36, 43–51. [Google Scholar] [CrossRef]
- Cooper, S.; Di Fava, A.; Vivas, C.; Marchionni, L.; Ferro, F. ARI: The social assistive robot and companion. In Proceedings of the 2020 29th IEEE International Conference on Robot and Human Interactive Communication (RO-MAN), Naples, Italy, 31 August–4 September 2020; pp. 745–751. [Google Scholar]
- Yu, C.; Sommerlad, A.; Sakure, L.; Livingston, G. Socially assistive robots for people with dementia: Systematic review and meta-analysis of feasibility, acceptability and the effect on cognition, neuropsychiatric symptoms and quality of life. Ageing Res. Rev. 2022, 78, 101633. [Google Scholar] [CrossRef] [PubMed]
- Cano, S.; González, C.S.; Gil-Iranzo, R.M.; Albiol-Pérez, S. Affective communication for socially assistive robots (sars) for children with autism spectrum disorder: A systematic review. Sensors 2021, 21, 5166. [Google Scholar] [CrossRef] [PubMed]
- Getson, C.; Nejat, G. Socially assistive robots helping older adults through the pandemic and life after COVID-19. Robotics 2021, 10, 106. [Google Scholar] [CrossRef]
- Feil-Seifer, D.; Mataric, M.J. Defining socially assistive robotics. In Proceedings of the 9th International Conference on Rehabilitation Robotics (ICORR 2005), Chicago, IL, USA, 28 June–1 July 2005; pp. 465–468. [Google Scholar]
- Meinert, E.; Van Velthoven, M.; Brindley, D.; Alturkistani, A.; Foley, K.; Rees, S.; Wells, G.; de Pennington, N. The internet of things in health care in oxford: Protocol for proof-of-concept projects. JMIR Res. Protoc. 2018, 7, e12077. [Google Scholar] [CrossRef] [PubMed]
- Hyodol Co., Ltd. Hello, We Are HYODOL ‘How It Works?’. Available online: https://hyodol.oopy.io/ (accessed on 17 December 2022).
- Lee, O.E.; Lee, H.; Park, A.; Choi, N.G. My precious friend: Human-robot interactions in home care for socially isolated older adults. Clin. Gerontol. 2024, 47, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Od, S.; Huang, H.-H.; Wei, J.-B. Apply LoRa technology to construct an air quality monitoring IoT system. In Proceedings of the 2021 IEEE 3rd Eurasia Conference on Biomedical Engineering, Healthcare and Sustainability (ECBIOS), Tainan, Taiwan, 28–30 May 2021; pp. 88–91. [Google Scholar]
- Administration, K.M. Automatic Weather System (AWS) Database. Available online: https://data.kma.go.kr/data/rmt/rmtList.do?code=400&pgmNo=570 (accessed on 16 November 2022).
- Korea Environment Corporation. Air Pollution Information-Real-Time Measurement Information Station. Available online: https://www.airkorea.or.kr/web/khaiInfo?pMENU_NO=129 (accessed on 16 November 2020).
- Administration, K.M. Living Weather Index. Available online: https://www.weather.go.kr/w/theme/daily-life/life-weather-index.do (accessed on 10 February 2023).
- Tham, S.; Thompson, R.; Landeg, O.; Murray, K.; Waite, T. Indoor temperature and health: A global systematic review. Public Health 2020, 179, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Korea, A. Fine Dust Concentration Forecast—Forecast Grades and Action Guidelines. Available online: https://www.airkorea.or.kr/web/dustForecast?pMENU_NO=113 (accessed on 10 February 2023).
- Etikan, I.; Musa, S.A.; Alkassim, R.S. Comparison of convenience sampling and purposive sampling. Am. J. Theor. Appl. Stat. 2016, 5, 1–4. [Google Scholar] [CrossRef]
- Tanaka, M.; Ishii, A.; Yamano, E.; Ogikubo, H.; Okazaki, M.; Kamimura, K.; Konishi, Y.; Emoto, S.; Watanabe, Y. Effect of a human-type communication robot on cognitive function in elderly women living alone. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2012, 18, CR550. [Google Scholar] [CrossRef]
- Liang, A.; Piroth, I.; Robinson, H.; MacDonald, B.; Fisher, M.; Nater, U.M.; Skoluda, N.; Broadbent, E. A pilot randomized trial of a companion robot for people with dementia living in the community. J. Am. Med. Dir. Assoc. 2017, 18, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Nasteski, V. An overview of the supervised machine learning methods. Horizons. B 2017, 4, 56. [Google Scholar] [CrossRef]
- Kim, J.-h.; Song, D. Analysis of fine dust generation by indoor activities in residential building. In Proceedings of the Society of Airconditioning and Refrigerating Engineers of Korea, Seoul, Republic of Korea, 25 November 2016; pp. 261–264. [Google Scholar]
- Won, S.R.; Ji, H.A.; Kwon, M.; Hwang, E.S.; Lee, J.-S.; Shim, I.-K. Characteristics of particles and gaseous pollutants generated from roasting fish and meat in kitchens. J. Environ. Anal. Health Toxicol. 2019, 22, 224–229. [Google Scholar] [CrossRef]
- Jones, P.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.; Leidy, N.K. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Bestall, J.; Paul, E.; Garrod, R.; Garnham, R.; Jones, P.; Wedzicha, J. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999, 54, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Leidy, N.K.; Rennard, S.I.; Schmier, J.; Jones, M.K.C.; Goldman, M. The breathlessness, cough, and sputum scale: The development of empirically based guidelines for interpretation. Chest 2003, 124, 2182–2191. [Google Scholar] [CrossRef] [PubMed]
- Plaza, V.; Fernández-Rodríguez, C.; Melero, C.; Cosío, B.G.; Entrenas, L.M.; De Llano, L.P.; Gutiérrez-Pereyra, F.; Tarragona, E.; Palomino, R.; López-Viña, A. Validation of the ‘Test of the Adherence to Inhalers’(TAI) for asthma and COPD patients. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 142–152. [Google Scholar] [CrossRef] [PubMed]
- Löwe, B.; Unützer, J.; Callahan, C.M.; Perkins, A.J.; Kroenke, K. Monitoring depression treatment outcomes with the patient health questionnaire-9. Med. Care 2004, 42, 1194–1201. [Google Scholar] [CrossRef] [PubMed]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- Caruana, R.; Niculescu-Mizil, A. An empirical comparison of supervised learning algorithms. In Proceedings of the 23rd International Conference on Machine Learning, Pittsburgh, PA, USA, 25–29 June 2006; pp. 161–168. [Google Scholar]
- Gockley, R.; Bruce, A.; Forlizzi, J.; Michalowski, M.; Mundell, A.; Rosenthal, S.; Sellner, B.; Simmons, R.; Snipes, K.; Schultz, A.C. Designing robots for long-term social interaction. In Proceedings of the 2005 IEEE/RSJ International Conference on Intelligent Robots and Systems, Edmonton, AB, Canada, 2–6 August 2005; pp. 1338–1343. [Google Scholar]
- Michalski, R.S.; Carbonell, J.G.; Mitchell, T.M. Machine Learning: An Artificial Intelligence Approach; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2013. [Google Scholar]
- Sahin, E.K.; Colkesen, I.; Acmali, S.S.; Akgun, A.; Aydinoglu, A.C. Developing comprehensive geocomputation tools for landslide susceptibility mapping: LSM tool pack. Comput. Geosci. 2020, 144, 104592. [Google Scholar] [CrossRef]
- Winkle, K.; McMillan, D.; Arnelid, M.; Harrison, K.; Balaam, M.; Johnson, E.; Leite, I. Feminist human-robot interaction: Disentangling power, principles and practice for better, more ethical HRI. In Proceedings of the 2023 ACM/IEEE International Conference on Human-Robot Interaction, Stockholm, Sweden, 13–16 March 2023; pp. 72–82. [Google Scholar]
- Yu, S.-H.; Guo, A.-M.; Zhang, X.-J. Effects of self-management education on quality of life of patients with chronic obstructive pulmonary disease. Int. J. Nurs. Sci. 2014, 1, 53–57. [Google Scholar] [CrossRef]
- Simoni-Wastila, L.; Wei, Y.-J.; Qian, J.; Zuckerman, I.H.; Stuart, B.; Shaffer, T.; Dalal, A.A.; Bryant-Comstock, L. Association of chronic obstructive pulmonary disease maintenance medication adherence with all-cause hospitalization and spending in a Medicare population. Am. J. Geriatr. Pharmacother. 2012, 10, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Gasteiger, N.; Loveys, K.; Law, M.; Broadbent, E. Friends from the future: A scoping review of research into robots and computer agents to combat loneliness in older people. Clin. Interv. Aging 2021, 16, 941–971. [Google Scholar] [CrossRef] [PubMed]
- Lazar, A.; Thompson, H.J.; Piper, A.M.; Demiris, G. Rethinking the design of robotic pets for older adults. In Proceedings of the 2016 ACM Conference on Designing Interactive Systems, Brisbane, QLD, Australia, 4–8 June 2016; pp. 1034–1046. [Google Scholar]
- Zhu, H.; Wu, C.K.; Koo, C.H.; Tsang, Y.T.; Liu, Y.; Chi, H.R.; Tsang, K.-F. Smart healthcare in the era of internet-of-things. IEEE Consum. Electron. Mag. 2019, 8, 26–30. [Google Scholar] [CrossRef]



| Measurement | Temperature | Humidity | Fine Dust | Ultrafine Dust |
|---|---|---|---|---|
| Range | −20–99 °C | 0–99% | 2.5–10 µm | 1.0–2.5 µm |
| Accuracy | 0.1 °C | 0.1% | 1 µg/m3 | 1 µg/m3 |
| Indoor Air Quality | Outdoor Atmosphere | |||||
|---|---|---|---|---|---|---|
| Standards | Spring and Fall | Summer | Winter | Standards | Four Seasons | |
| Temperature | Very hot | >32 °C | Hot | >32 °C | ||
| Hot | 28–32 °C | Good | 10–32 °C | |||
| Good | 22–28 °C | Cold | 10 °C | |||
| Cold | 18–22 °C | |||||
| Very cold | <18 °C | |||||
| Humidity | Very humid | >80% | >90% | >70% | Humid | >80% |
| Humid | 60–80% | 70–90% | 50–70% | Good | 20–80% | |
| Good | 40–60% | 50–70% | 30–50% | Dry | <20% | |
| Dry | 20–40% | 30–50% | 10–30% | |||
| Very dry | <20% | <30% | <10% | |||
| PM10 | Good | 0–30 μg/m3 | Good | 0–30 μg/m3 | ||
| Normal | 31–80 μg/m3 | Normal | 31–80 μg/m3 | |||
| Poor | 81–150 μg/m3 | Poor | 81–150 μg/m3 | |||
| Very poor | >151 μg/m3 | Very poor | >151 μg/m3 | |||
| PM2.5 | Good | 0–15 μg/m3 | Good | 0–15 μg/m3 | ||
| Normal | 16–35 μg/m3 | Normal | 16–35 μg/m3 | |||
| Poor | 36–75 μg/m3 | Poor | 36–75 μg/m3 | |||
| Very poor | >76 μg/m3 | Very poor | >76 μg/m3 | |||
| Week 1 | Week 2 | Week 3 | Week 4 | |
|---|---|---|---|---|
| Good (Stage 1 or 2) | 1.121 | 1.262 | 1.260 | 1.121 |
| Bad (Stage 3 or 4) | 0.580 | 0.509 | 0.464 | 0.298 |
| Features | Sum | Not Improved/Worsened (Stage 3 or 4) | Improved/Remain Good (Stage 1 or 2) | ||
|---|---|---|---|---|---|
| N | (%) | N | (%) | ||
| Intervention Stage 2 Alert | 3800 | 329 | (8.7) | 3471 | (91.3) |
| Intervention Stage 3 Alert | 818 | 531 | (64.9) | 287 | (35.1) |
| Intervention Stage 4 Alert | 71 | 54 | (76.1) | 17 | (23.9) |
| Week 1 to 2 | 1300 | 238 | (18.3) | 1062 | (81.7) |
| Week 3 to 4 | 1100 | 192 | (17.5) | 908 | (82.2) |
| Week 5 to 6 | 1107 | 225 | (20.3) | 882 | (79.7) |
| Week 7 to 8 | 1182 | 259 | (21.9) | 923 | (78.1) |
| Alert time AM 0 to 6 ’o clock | 508 | 106 | (20.9) | 402 | (79.1) |
| Alert time AM 7 to 12 ’o clock | 1823 | 386 | (21.2) | 1437 | (78.8) |
| Alert time PM 12 to 6 ’o clock | 1379 | 208 | (15.1) | 1171 | (84.9) |
| Alert time PM 7 to 12 ’o clock | 979 | 214 | (21.9) | 765 | (78.1) |
| Aged over 75 | 2346 | 531 | (22.6) | 1815 | (77.4) |
| Living Alone | 2309 | 499 | (21.6) | 1810 | (78.4) |
| CAT high (baseline) | 1431 | 299 | (20.9) | 1132 | (79.1) |
| CAT mid (baseline) | 1142 | 210 | (18.4) | 932 | (81.6) |
| CAT low (baseline) | 2116 | 405 | (19.1) | 1711 | (80.9) |
| CAT high (end point) | 1431 | 299 | (20.9) | 1132 | (79.1) |
| CAT mid (end point) | 1791 | 279 | (15.6) | 1512 | (84.4) |
| CAT low (end point) | 1467 | 336 | (22.9) | 1131 | (77.1) |
| MRC 0 to 1 (baseline) | 2980 | 582 | (19.5) | 2398 | (80.5) |
| MRC 2 to 3 (baseline) | 2833 | 566 | (20.0) | 2267 | (80.0) |
| BSCC 0 to 2 (baseline) | 3465 | 660 | (19.0) | 2805 | (81.0) |
| BSCC 0 to 2 (end point) | 1924 | 392 | (20.4) | 1532 | (79.6) |
| TAI good (end point) | 3326 | 664 | (20.0) | 2662 | (80.0) |
| TAI intermediate (end point) | 1170 | 213 | (18.2) | 957 | (81.8) |
| TAI poor (end point) | 193 | 37 | (19.2) | 156 | (80.8) |
| PHQ-9 none (baseline) | 4086 | 780 | (19.1) | 3306 | (80.9) |
| PHQ-9 none (end point) | 2733 | 434 | (15.9) | 2299 | (84.1) |
| EQ-5D perfect (baseline) | 1914 | 382 | (20.0) | 1532 | (80.0) |
| EQ-5D perfect (end point) | 1461 | 288 | (19.7) | 1173 | (80.3) |
| Evaluation Index | Naïve Bayes Classification | Neural Networks | Logistic Regression | Support Vector Machines | Random Forests | Decision Trees |
|---|---|---|---|---|---|---|
| Accuracy | 86.2 | 86.0 | 86.4 | 86.7 | 87.1 | 85.6 |
| Sensitivity | 92.1 | 94.7 | 93.3 | 92.6 | 94.1 | 90.8 |
| Specificity | 61.7 | 51.4 | 60.1 | 60.6 | 58.2 | 60.3 |
| Precision | 90.8 | 88.6 | 90.0 | 91.3 | 90.3 | 91.7 |
| AUC 1 | 0.83 | 0.83 | 0.83 | 0.82 | 0.85 | 0.84 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hwang, Y.-S.; Lee, O.E.-K.; Kim, W.-J.; Jo, H.-S. Designing a Socially Assistive Robot to Assist Older Patients with Chronic Obstructive Pulmonary Disease in Managing Indoor Air Quality. Appl. Sci. 2024, 14, 5647. https://doi.org/10.3390/app14135647
Hwang Y-S, Lee OE-K, Kim W-J, Jo H-S. Designing a Socially Assistive Robot to Assist Older Patients with Chronic Obstructive Pulmonary Disease in Managing Indoor Air Quality. Applied Sciences. 2024; 14(13):5647. https://doi.org/10.3390/app14135647
Chicago/Turabian StyleHwang, Yu-Seong, Othelia Eun-Kyoung Lee, Woo-Jin Kim, and Heui-Sug Jo. 2024. "Designing a Socially Assistive Robot to Assist Older Patients with Chronic Obstructive Pulmonary Disease in Managing Indoor Air Quality" Applied Sciences 14, no. 13: 5647. https://doi.org/10.3390/app14135647
APA StyleHwang, Y.-S., Lee, O. E.-K., Kim, W.-J., & Jo, H.-S. (2024). Designing a Socially Assistive Robot to Assist Older Patients with Chronic Obstructive Pulmonary Disease in Managing Indoor Air Quality. Applied Sciences, 14(13), 5647. https://doi.org/10.3390/app14135647






