Compressive Strength Comparison of Different Orthodontic Metal Bracket Systems
Abstract
:1. Introduction
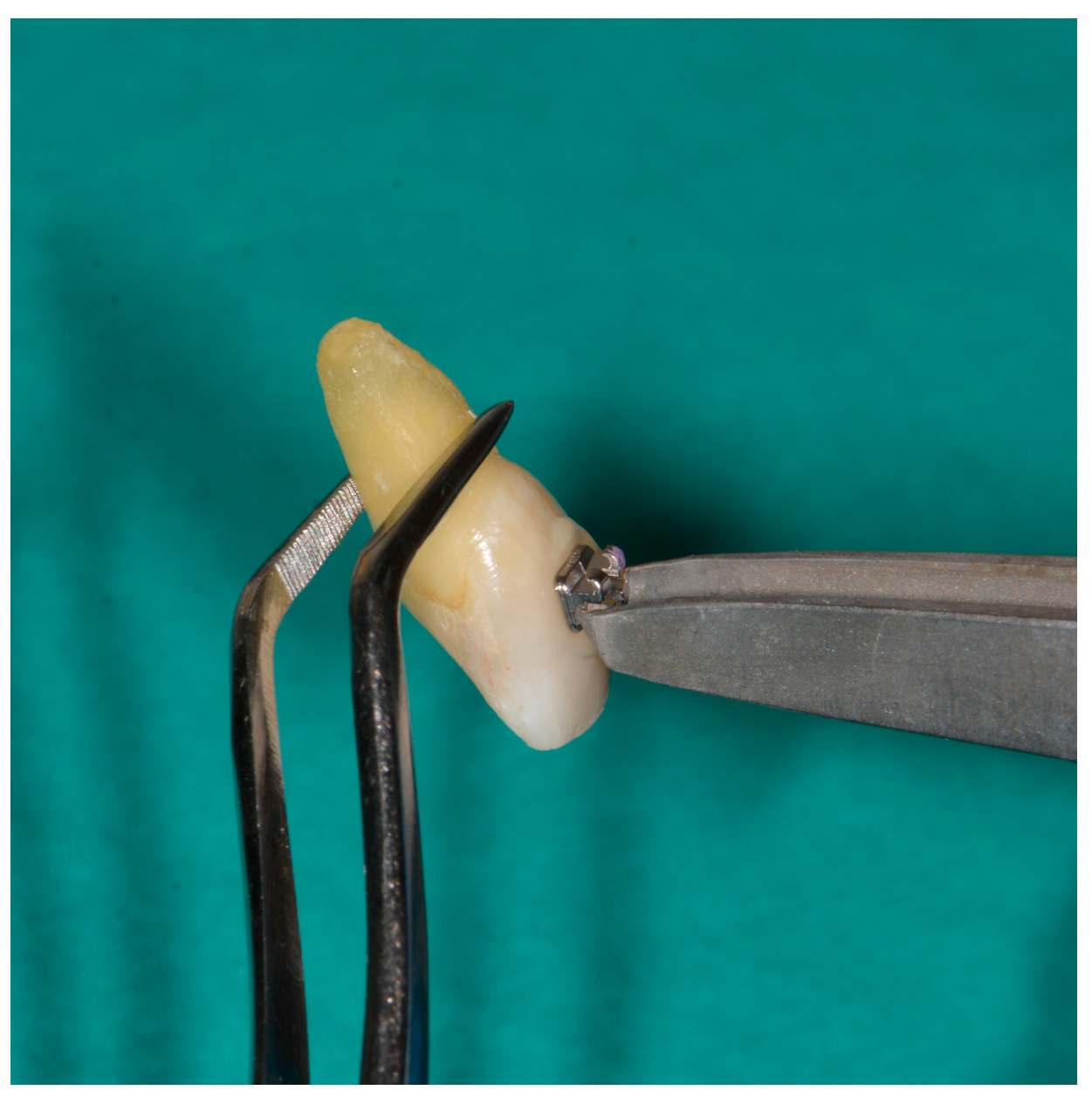
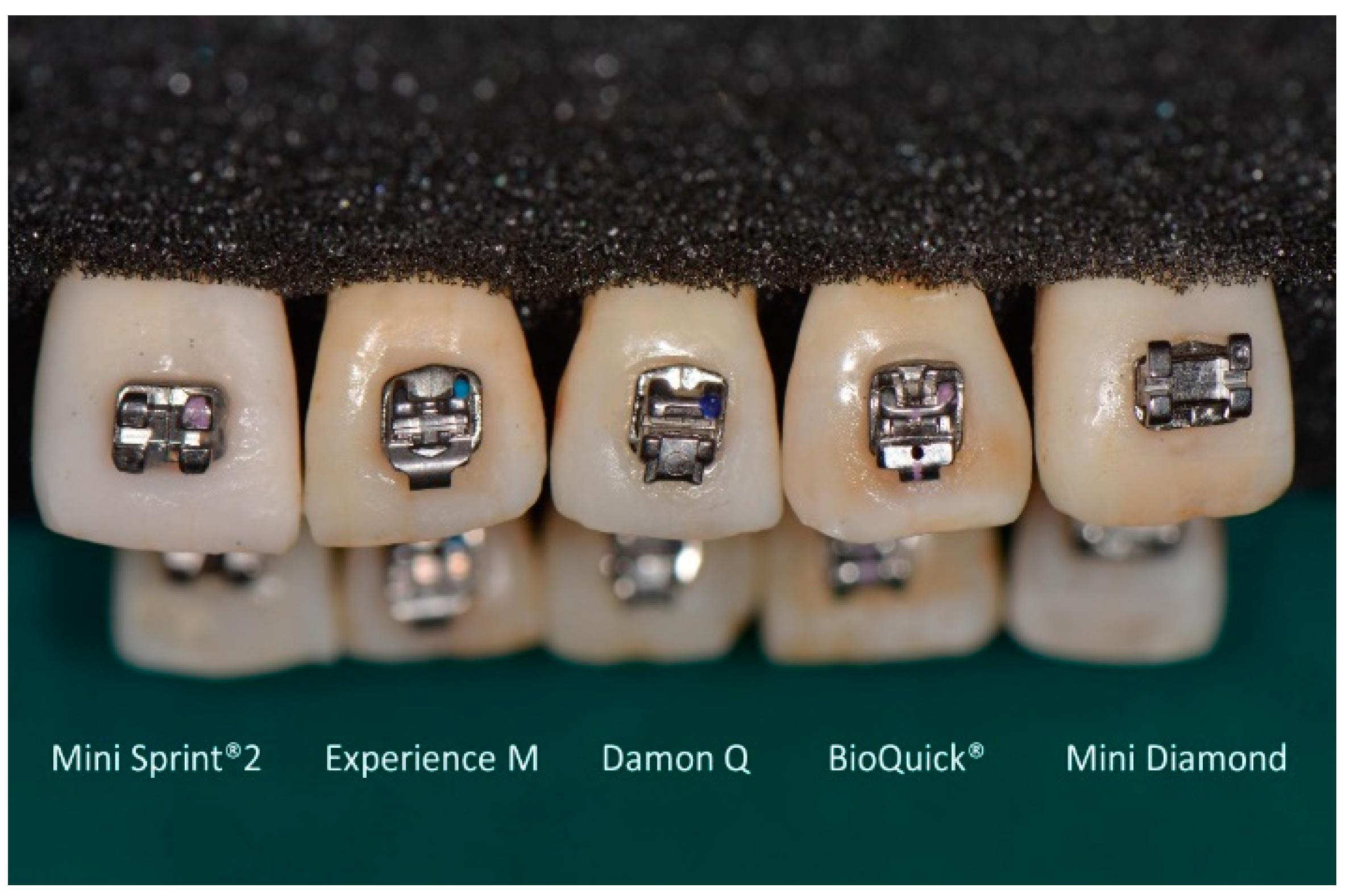
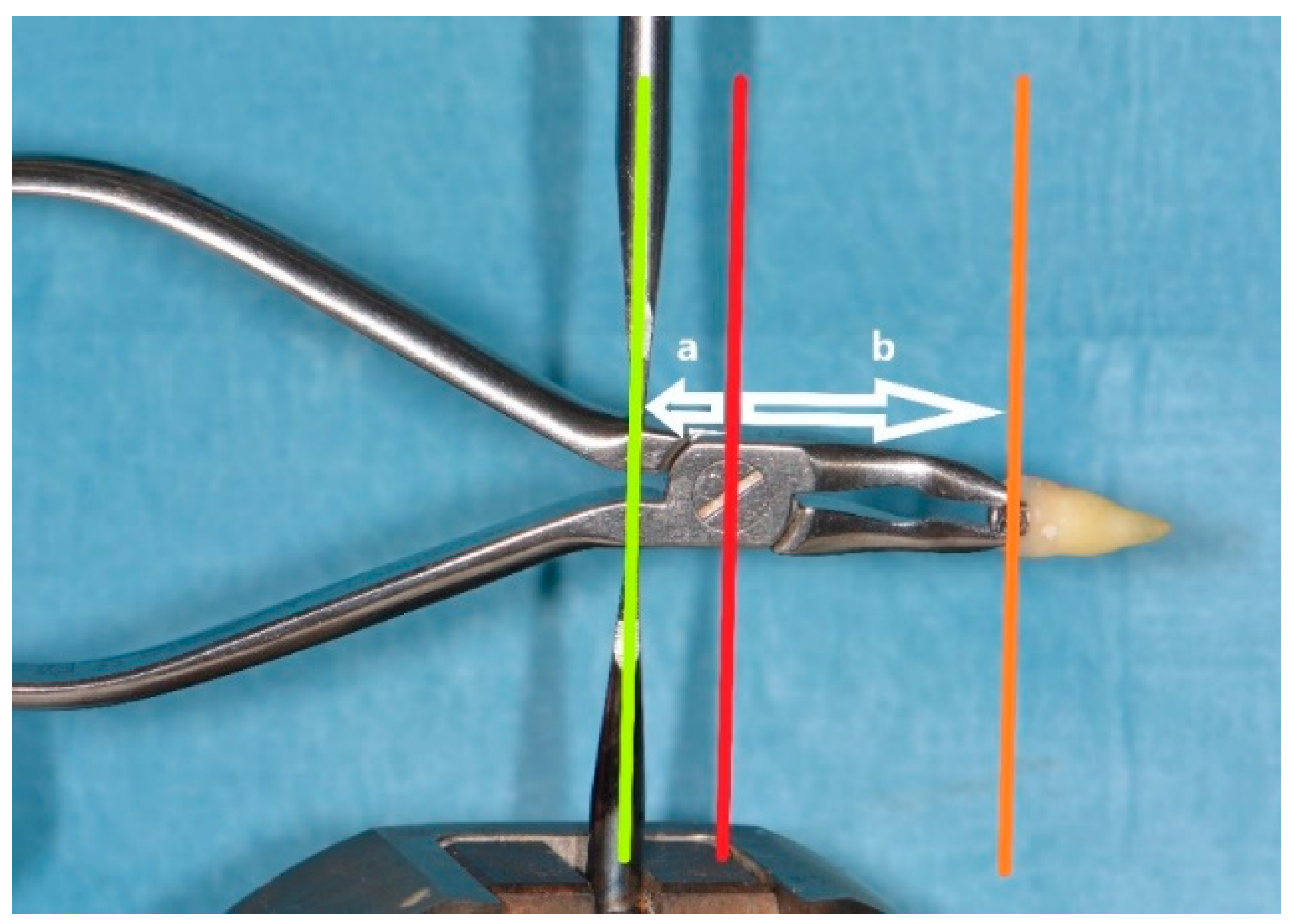
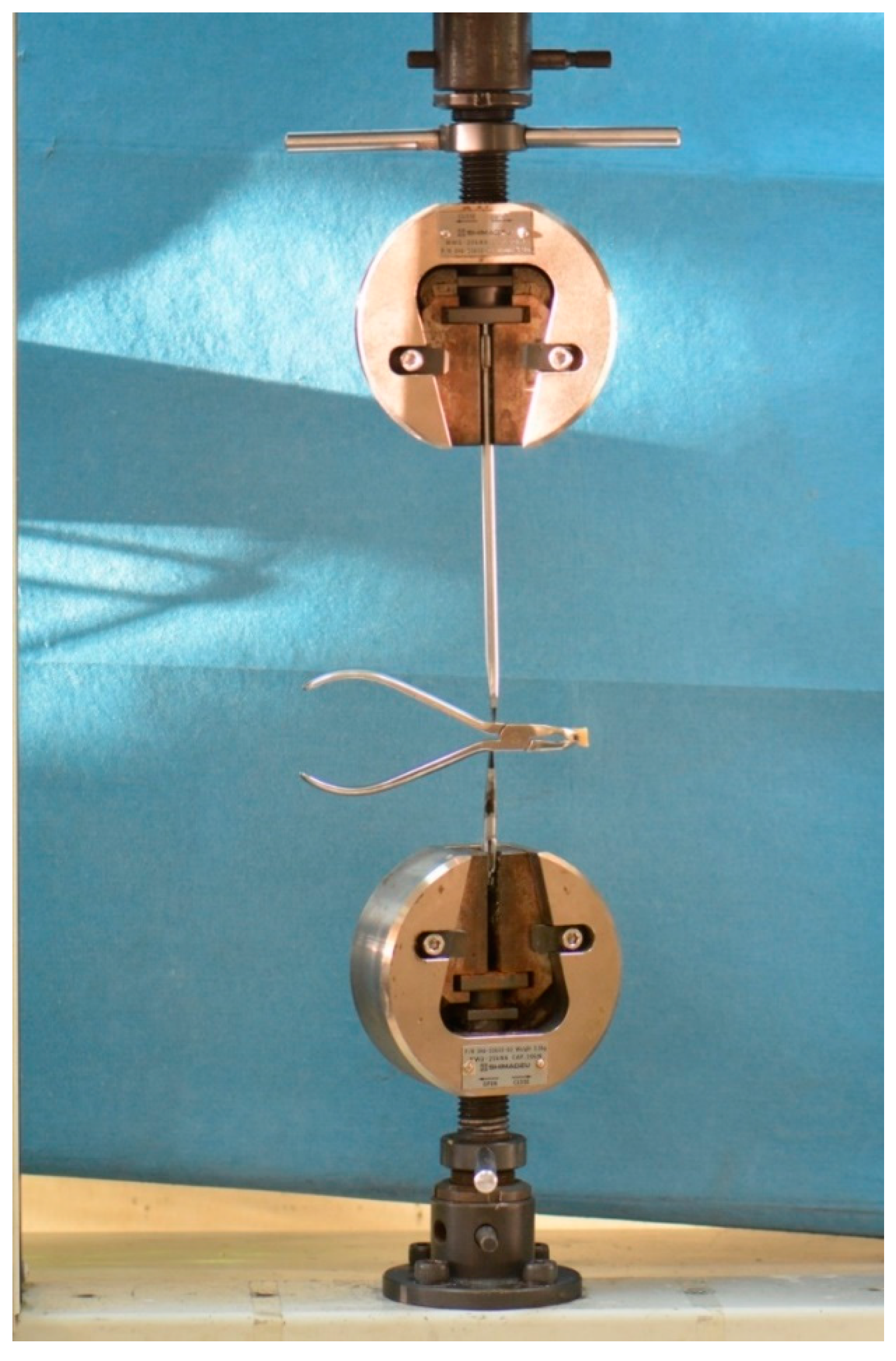
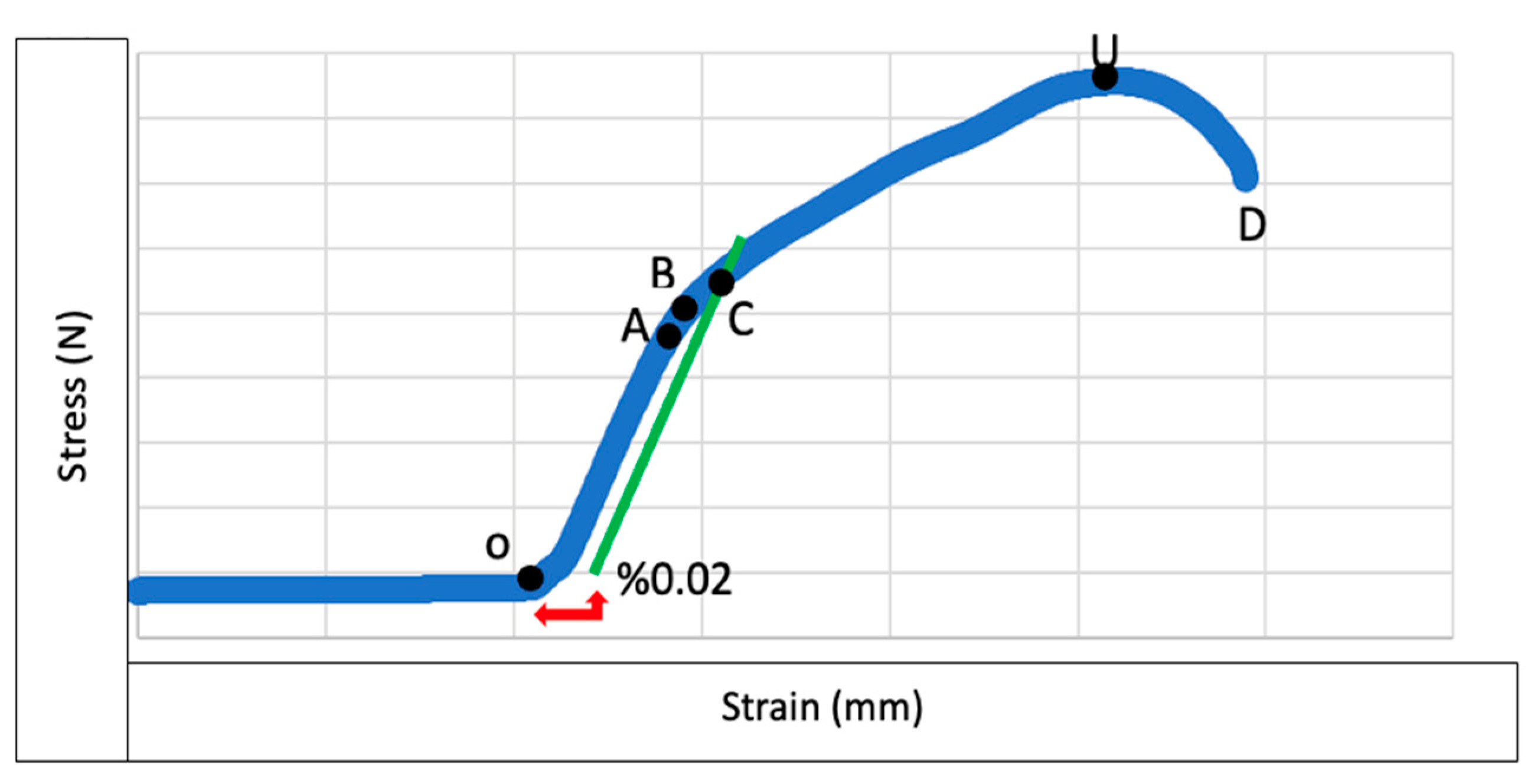
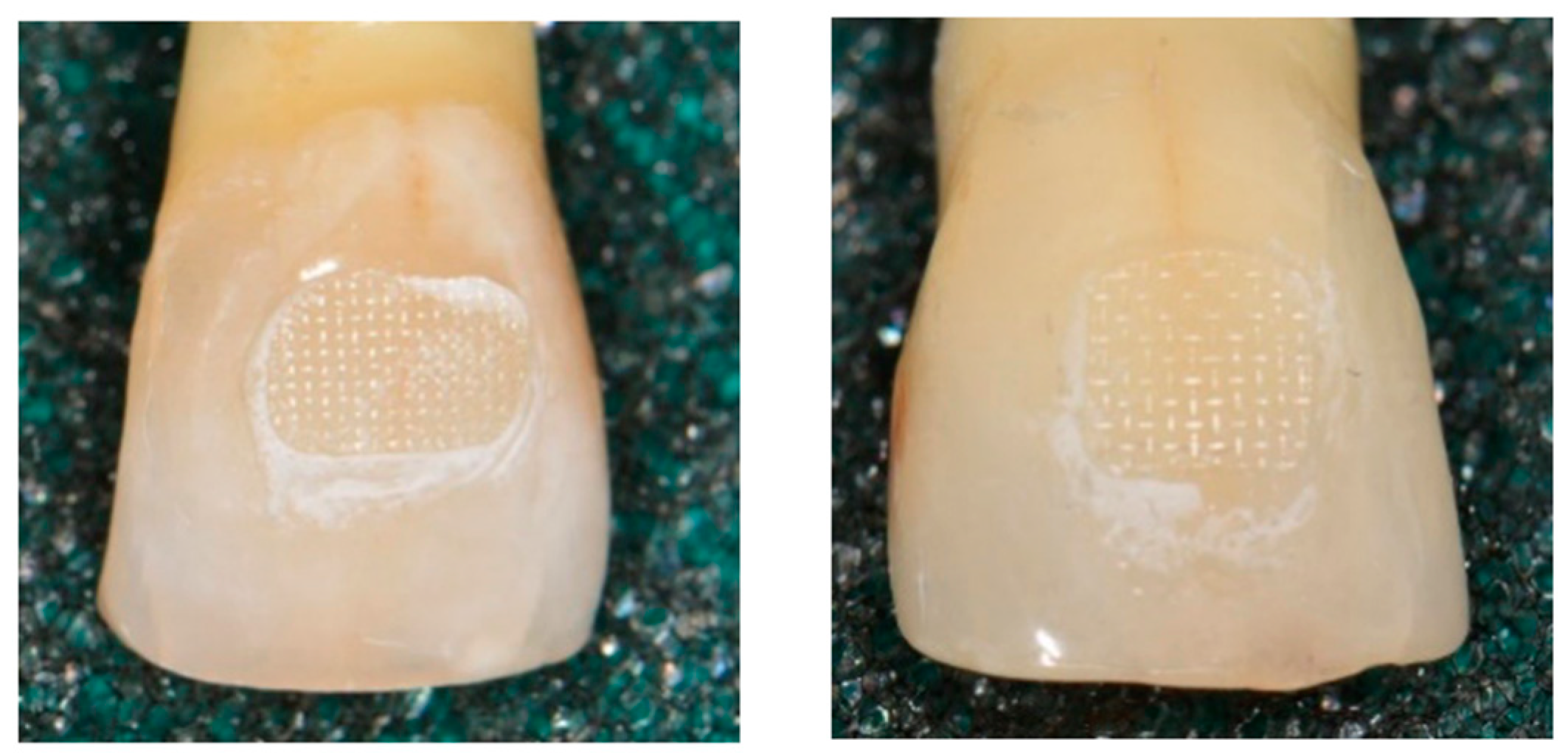
2. Materials and Methods
- No cracks or fractures in the enamel
- No fillings or restorations on the teeth
- Teeth should not have undergone root canal treatment
- No discoloration due to reasons such as medication usage
- Teeth should not exhibit major deformations
3. Results
4. Discussion
5. Conclusions
- Damon Q brackets are more resistant to plastic deformation compared to MiniDiamond, BioQuick, and Mini Sprint II brackets. Although Damon Q brackets exhibited the highest plastic deformation (yield) strength under compression forces, there was no significant difference compared to the Experience group.
- Damon Q and Experience brackets have higher ultimate strength values compared to Mini Diamond, BioQuick, and Mini Sprint II brackets. Damon Q brackets were the most successful group in terms of ultimate strength values with no significant difference found compared to the Experience group.
- There was no significant difference in ARI scores among the brackets used.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Koo, B.C.; Chung, C.-H.; Vanarsdall, R.L. Comparison of the Accuracy of Bracket Placement between Direct and Indirect Bonding Techniques. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 346–351. [Google Scholar] [CrossRef] [PubMed]
- Fan, X.-C.; Chen, L.; Huang, X.-F. Effects of Various Debonding and Adhesive Clearance Methods on Enamel Surface: An in Vitro Study. BMC Oral Health 2017, 17, 58. [Google Scholar] [CrossRef] [PubMed]
- Pinho, M.; Manso, M.C.; Almeida, R.F.; Martin, C.; Carvalho, Ó.; Henriques, B.; Silva, F.; Pinhão Ferreira, A.; Souza, J.C.M. Bond Strength of Metallic or Ceramic Orthodontic Brackets to Enamel, Acrylic, or Porcelain Surfaces. Materials 2020, 13, 5197. [Google Scholar] [CrossRef] [PubMed]
- Paolone, G.; Mandurino, M.; Baldani, S.; Paolone, M.G.; Goracci, C.; Scolavino, S.; Gherlone, E.; Cantatore, G.; Gastaldi, G. Quantitative Volumetric Enamel Loss after Orthodontic Debracketing/Debonding and Clean-Up Procedures: A Systematic Review. Appl. Sci. 2023, 13, 5369. [Google Scholar] [CrossRef]
- Oliver, R.G. The Effect of Different Methods of Bracket Removal Onthe Amount of Residual Adhesive. Am. J. Orthod. Dentofac. Orthop. 1988, 93, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Brantley, W.A.; Eliades, T. Orthodontic Materials: Scientific and Clinical Aspects. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 672–673. [Google Scholar]
- Holberg, C.; Rudzki-Janson, I.; Wichelhaus, A.; Winterhalder, P. Periodontal Ligament Strain Induced by Different Orthodontic Bracket Removal Techniques. J. Orofac. Orthop. Fortschritte Kieferorthopädie 2014, 75, 287–298. [Google Scholar] [CrossRef] [PubMed]
- Holberg, C.; Winterhalder, P.; Holberg, N.; Wichelhaus, A.; Rudzki-Janson, I. Orthodontic Bracket Debonding: Risk of Enamel Fracture. Clin. Oral Investig. 2014, 18, 327–334. [Google Scholar] [CrossRef] [PubMed]
- Knösel, M.; Mattysek, S.; Jung, K.; Sadat-Khonsari, R.; Kubein-Meesenburg, D.; Bauss, O.; Ziebolz, D. Impulse Debracketing Compared to Conventional Debonding: Extent of Enamel Damage, Adhesive Residues and the Need for Postprocessing. Angle Orthod. 2010, 80, 1036–1044. [Google Scholar] [CrossRef]
- Sinha, P.K.; Nanda, R.S. The Effect of Different Bonding and Debonding Techniques on Debonding Ceramic Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 1997, 112, 132–137. [Google Scholar]
- Dalaie, K.; Fatemi, S.M.; Behnaz, M.; Ghaffari, S.; Hemmatian, S.; Soltani, A.D. Effect of Different Debonding Techniques on Shear Bond Strength and Enamel Cracks in Simulated Clinical Set-Ups. J. World Fed. Orthod. 2020, 9, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Ji, L.; Chen, Z.; Liao, C.-H.; Hu, S.-F.; Luo, Z.-X.; Lian, B.-W.; He, H. Effects of Customized Resin Base on Bonding Strength of Spherical Self-Ligating Brackets. J. Orofac. Orthop./Fortschritte Der Kieferorthopadie 2022, 83, 108–116. [Google Scholar] [CrossRef] [PubMed]
- Sfondrini, M.F.; Xheka, E.; Scribante, A.; Gandini, P.; Sfondrini, G. Reconditioning of Self-Ligating Brackets. Angle Orthod. 2012, 82, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; VonWald, L.; Laffoon, J.F.; Warren, J.J. Effect of a Self-Etch Primer/Adhesive on the Shear Bond Strength of Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 621–624. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Laffoon, J.F.; Vonwald, L.; Warren, J.J. The Effect of Repeated Bonding on the Shear Bond Strength of Different Orthodontic Adhesives. Am. J. Orthod. Dentofac. Orthop. 2002, 121, 521–525. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.L.; de Rijk, W.G.; Evans, C.A. Tensile and Shear Stresses in the Orthodontic Attachment Adhesive Layer with 3D Finite Element Analysis. Am. J. Orthod. Dentofac. Orthop. 1999, 116, 530–532. [Google Scholar] [CrossRef] [PubMed]
- Melenka, G.W.; Nobes, D.S.; Major, P.W.; Carey, J.P. Three-Dimensional Deformation of Orthodontic Brackets. J. Dent. Biomech. 2013, 4, 1758736013492529. [Google Scholar] [CrossRef] [PubMed]
- Lacoursiere, R.A.; Nobes, D.S.; Homeniuk, D.L.N.; Carey, J.P.; Badawi, H.H.; Major, P.W. Measurement of Orthodontic Bracket Tie Wing Elastic and Plastic Deformation by Arch Wire Torque Expression Utilizing an Optical Image Correlation Technique. J. Dent. Biomech. 2009, 2010, 397037. [Google Scholar] [CrossRef] [PubMed]
- Valletta, R.; Prisco, D.; De Santis, R.; Ambrosio, L.; Martina, R. Evaluation of the Debonding Strength of Orthodontic Brackets Using Three Different Bonding Systems. Eur. J. Orthod. 2007, 29, 571–577. [Google Scholar] [CrossRef]
- Ahmed, T.; Rahman, N.A.; Alam, M.K. Comparison of Orthodontic Bracket Debonding Force and Bracket Failure Pattern on Different Teeth In Vivo by a Prototype Debonding Device. BioMed. Res. Int. 2021, 2021, 6663683. [Google Scholar] [CrossRef]
- Linjawi, A.I.; Abbassy, M.A. Comparison of Shear Bond Strength to Clinically Simulated Debonding of Orthodontic Brackets: An in Vitro Study. J. Orthod. Sci. 2016, 5, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Olsen, M.E.; Bishara, S.E.; Damon, P.; Jakobsen, J.R. Evaluation of Scotchbond Multipurpose and Maleic Acid as Alternative Methods of Bonding Orthodontic Brackets. Am. J. Orthod. Dentofac. Orthop. 1997, 111, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Bishara, S.E.; Forrseca, J.M.; Fehr, D.E.; Boyer, D.B. Debonding Forces Applied to Ceramic Brackets Simulating Clinical Conditions. Angle Orthod. 1994, 64, 277–282. [Google Scholar] [CrossRef]
- Jonke, E.; Franz, A.; Freudenthaler, J.; König, F.; Bantleon, H.-P.; Schedle, A. Cytotoxicity and Shear Bond Strength of Four Orthodontic Adhesive Systems. Eur. J. Orthod. 2008, 30, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Cozza, P.; Martucci, L.; De Toffol, L.; Penco, S.I. Shear Bond Strength of Metal Brackets on Enamel. Angle Orthod. 2006, 76, 851–856. [Google Scholar] [CrossRef] [PubMed]
- Jabr, L.; Rossouw, P.E.; Michelogiannakis, D.; Malik, S.; Wheeler, T.T.; Barmak, A.B. A Comparative Assessment of the Bonding Characteristics of Three-Dimensional Custom-Printed Polycrystalline Alumina Brackets and Conventional Brackets. Appl. Sci. 2024, 14, 924. [Google Scholar] [CrossRef]
- Su, M.-Z.; Lai, E.H.-H.; Chang, J.Z.-C.; Chen, H.-J.; Chang, F.H.-F.; Chiang, Y.-C.; Lin, C.-P. Effect of Simulated Debracketing on Enamel Damage. J. Formos. Med. Assoc. 2012, 111, 560–566. [Google Scholar] [CrossRef]
- Jayakrishnan, U.; Sorake, A.; Rai, R.; Shetty, S. Assessment of Shear Bond Strength of Various Self Ligating Systems- An Evaluation of Bonding Efficiency. Saudi J. Oral Dent. Res. 2022, 7, 329–332. [Google Scholar] [CrossRef]
- Lo Giudice, G.; Lo Giudice, A.; Isola, G.; Fabiano, F.; Artemisia, A.; Fabiano, V.; Nucera, R.; Matarese, G. Evaluation of Bond Strength and Detachment Interface Distribution of Different Bracket Base Designs. Acta Med. Mediterr. 2015, 31, 585. [Google Scholar]
- Stanford, S.K.; Wozniak, W.T.; Fin, P.L. The Need for Standardization of Test Protocols. Semin. Orthod. 1997, 3, 206–209. [Google Scholar] [CrossRef]



| Model/Experiment Code | Max. | Min. | Mean | Standard Deviation | Median | |
|---|---|---|---|---|---|---|
| Experience M (E) | Yield Point (N) | 536.2 | 311.2 | 463.7918 | 56.72822 | 473.85 |
| MiniSprint II (MS) | 506.8 | 216.45 | 408.7529 | 89.48629 | 443.3 | |
| Mini Diamond (MD) | 295.05 | 95.68 | 211.7312 | 56.22774 | 217.1 | |
| BioQuick (BQ) | 527.85 | 108.86 | 280.6418 | 118.0751 | 289.8 | |
| Damon Q (D) | 632.95 | 227.8 | 549.3529 | 108.969 | 588 | |
| Experience M (E) | Ultimate Strength (N) | 915.5 | 420.9 | 758.6542 | 146.3391 | 778.05 |
| MiniSprint II (MS) | 511.65 | 263.1 | 442.4618 | 63.90439 | 456.9 | |
| Mini Diamond (MD) | 301.4 | 97.82 | 224.0788 | 57.12496 | 240.8 | |
| BioQuick (BQ) | 554.65 | 114.57 | 313.2097 | 132.2631 | 296.3 | |
| Damon Q (D) | 1041.8 | 396.1 | 764.5051 | 178.1314 | 748.25 | |
| Experience M (E) | Failure/ DebondingPoint (N) | 777.98 | 383.15 | 591.8518 | 111.4679 | 584.95 |
| MiniSprint II (MS) | 412.6 | 234.34 | 312.1088 | 51.95756 | 306.04 | |
| Mini Diamond (MD) | 151.72 | 84.57 | 121.71 | 20.52432 | 127.05 | |
| BioQuick (BQ) | 513.25 | 104.68 | 204.2847 | 111.8101 | 156.05 | |
| Damon Q (D) | 1040.3 | 365.9 | 721.8912 | 163.7221 | 716.95 |
| Group | p Value | ||
|---|---|---|---|
| Yield Point (N) | Ultimate Strength Point (N) | Failure (Drop/Debond) (N) | |
| E | 0.013 | 0.031 | 0.831 |
| MS | 0.030 | 0.388 | 0.304 |
| MD | 0.436 | 0.276 | 0.300 |
| BQ | 0.637 | 0.486 | 0.002 |
| D | 0.001 | 0.720 | 0.815 |
| Total Sample Size | Test Statistic | Degrees of Freedom | Significance Value |
|---|---|---|---|
| 80 | 53.54 | 4 | 0.0001 |
| Groups | Median, (Minimum–Maximum) (N) | p | Significance (p) with Bonferroni Correction |
|---|---|---|---|
| Experience Mini Sprint II | 473.85 (311.2–536.2) 443.30 (216.45–506.80) | 0.188 | 1.000 |
| Mini Diamond Experience | 217.10 (95.68–295.05) 443.30 (216.45–506.80) | <0.001 | <0.001 |
| BioQuick Experience | 289.8 (108.86–527.85) 473.85 (311.2–536.2) | <0.001 | 0.004 |
| Damon Q Mini Sprint II | 748.25 (396.1–1041.8) 443.30 (216.45–506.80) | 0.002 | 0.019 |
| Mini Sprint II Mini Diamond | 443.30 (216.45–506.80) 217.10 (95.68–295.05) | 0.001 | 0.012 |
| Experience Damon Q | 473.85 (311.2–536.2) 748.25 (396.1–1041.8) | 0.073 | 0.726 |
| Mini Diamond Damon Q | 217.10 (95.68–295.05) 748.25 (396.1–1041.8) | <0.001 | <0.001 |
| BioQuick Mini Diamond | 289.8 (108.86–527.85) 217.10 (95.68–295.05) | 0.315 | 1.000 |
| Damon Q BioQuick | 748.25 (396.1–1041.8) 289.8 (108.86–527.85) | <0.001 | <0.001 |
| Mini Sprint II BioQuick | 443.30 (216.45–506.80) 289.8 (108.86–527.85) | 0.025 | 0.248 |
| Total Sample Size | Test Statistic | Degrees of Freedom | Significance Value |
|---|---|---|---|
| 80 | 60.43 | 4 | 0.0001 |
| Groups | Median, (Minimum–Maximum) (N) | p | Significance (p) with Bonferroni Correction |
|---|---|---|---|
| Experience Mini Sprint II | 778.05 (420.9–915.5) 456.9 (263.1–511.65) | 0.005 | 0.045 |
| Mini Diamond Experience | 240.8 (97.82–301.4) 778.05 (420.9–915.5) | <0.001 | <0.001 |
| BioQuick Experience | 296.3 (114.57–554.65) 778.05 (420.9–915.5) | <0.001 | <0.001 |
| Damon Q Mini Sprint II | 748.25 (396.1–1041.8) 456.9 (263.1–511.65) | 0.003 | 0.029 |
| Mini Sprint II Mini Diamond | 456.9 (263.1–511.65) 240.8 (97.82–301.4) | 0.002 | 0.017 |
| Experience Damon Q | 778.05 (420.9–915.5) 748.25 (396.1–1041.8) | 0.073 | 0.726 |
| Mini Diamond Damon Q | 240.8 (97.82–301.4) 748.25 (396.1–1041.8) | <0.001 | <0.001 |
| BioQuick Mini Diamond | 296.3 (114.57–554.65) 240.8 (97.82–301.4) | 0.207 | 1.000 |
| Damon Q BioQuick | 748.25 (396.1–1041.8) 296.3 (114.57–554.65) | <0.001 | <0.001 |
| Mini Sprint II BioQuick | 456.9 (263.1–511.65) 296.3 (114.57–554.65) | 0.060 | 0.602 |
| Total Sample Size | Test Statistic | Degrees of Freedom | Significance Value |
|---|---|---|---|
| 80 | 68.67 | 4 | 0.0001 |
| Groups | Median, (Minimum–Maximum) (N) | p | Significance (p) with Bonferroni Correction |
|---|---|---|---|
| Experience Mini Sprint II | 584.95 (383.15–777.98) 306.04 (234.34–412.6) | 0.012 | 0.123 |
| Mini Diamond Experience | 127.05 (84.57–151.72) 584.95 (383.15–777.98) | <0.001 | <0.001 |
| BioQuick Experience | 156.05 (104.68–513.25) 584.95 (383.15–777.98) | <0.001 | <0.001 |
| Damon Q Mini Sprint II | 716.95 (365.9–1040.3) 306.04 (234.34–412.6) | <0.001 | 0.005 |
| Mini Sprint II Mini Diamond | 306.04 (234.34–412.6) 127.05 (84.57–151.72) | 0.001 | 0.006 |
| Experience Damon Q | 584.95 (383.15–777.98) 716.95 (365.9–1040.3) | 0.323 | 1.000 |
| Mini Diamond Damon Q | 127.05 (84.57–151.72) 716.95 (365.9–1040.3) | <0.001 | <0.001 |
| BioQuick Mini Diamond | 156.05 (104.68–513.25) 127.05 (84.57–151.72) | 0.153 | 1.000 |
| Damon Q BioQuick | 716.95 (365.9–1040.3) 156.05 (104.68–513.25) | <0.001 | <0.001 |
| Mini Sprint II BioQuick | 306.04 (234.34–412.6) 156.05 (104.68–513.25) | 0.044 | 0.438 |
| Group | Debonded Sample/Total Sample | Average (MPa) |
|---|---|---|
| Experience | 7/17 | 56.84 |
| Mini Sprint II | 2/17 | 33.18 |
| Mini Diamond | 5/17 | 10.93 |
| BioQuick | 1/17 | 20.01 |
| Damon Q | 1/17 | 68.21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Şaylan, Ç.E.; Özel, M.B. Compressive Strength Comparison of Different Orthodontic Metal Bracket Systems. Appl. Sci. 2024, 14, 6692. https://doi.org/10.3390/app14156692
Şaylan ÇE, Özel MB. Compressive Strength Comparison of Different Orthodontic Metal Bracket Systems. Applied Sciences. 2024; 14(15):6692. https://doi.org/10.3390/app14156692
Chicago/Turabian StyleŞaylan, Çağan Erkman, and Mehmet Birol Özel. 2024. "Compressive Strength Comparison of Different Orthodontic Metal Bracket Systems" Applied Sciences 14, no. 15: 6692. https://doi.org/10.3390/app14156692





